A Five-Year Review of Temporal Bone Fractures at a Level One Trauma Center and Examination of the Impact of the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Recommendations
6. Study Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| COVID-19 | Coronavirus 2019 |
| ICD-10 | International Classification of Diseases, Tenth Revision |
| ICU | Intensive Care Unit |
| CSF | Cerebrospinal Fluid |
| SNHL | Sensorineural Hearing Loss |
References
- Ahmed, F.; Zviedrite, N.; Uzicanin, A. Effectiveness of workplace social distancing measures in reducing influenza transmission: A systematic review. BMC Public Health 2018, 18, 518. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.; Wong, J.Y.; Cowling, B.J. Nonpharmaceutical interventions for managing SARS-CoV-2. Curr. Opin. Pulm. Med. 2023, 29, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, G.D.; Jacobsen, K.H. Statewide COVID-19 Stay-at-Home Orders and Population Mobility in the United States. World Med. Health Policy 2020, 12, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.C.; Nelson, J.L.; Burke, A.B.; Lang, M.S.; Dillon, J.K. What Is the Effect of COVID-19-Related Social Distancing on Oral and Maxillofacial Trauma? J. Oral Maxillofac. Surg. 2021, 79, 1091–1097. [Google Scholar] [CrossRef] [PubMed]
- Hasso, A.N.; Ledington, J.A. Traumatic injuries of the temporal bone. Otolaryngol. Clin. N. Am. 1988, 21, 295–316. [Google Scholar] [CrossRef]
- Wiet, R.J.; Valvassori, G.E.; Kotsanis, C.A.; Parahy, C. Temporal bone fractures. State of the art review. Am. J. Otol. 1985, 6, 207–215. [Google Scholar] [PubMed]
- Dahiya, R.; Keller, J.D.; Litofsky, N.S.; Bankey, P.E.; Bonassar, L.J.; Megerian, C.A. Temporal bone fractures: Otic capsule sparing versus otic capsule violating clinical and radiographic considerations. J. Trauma Acute Care Surg. 1999, 47, 1079–1083. [Google Scholar] [CrossRef] [PubMed]
- Little, S.C.; Kesser, B.W. Radiographic classification of temporal bone fractures: Clinical predictability using a new system. Arch. Otolaryngol. Head Neck Surg. 2006, 132, 1300–1304. [Google Scholar] [CrossRef] [PubMed]
- Ishman, S.L.; Friedland, D.R. Temporal bone fractures: Traditional classification and clinical relevance. Laryngoscope 2004, 114, 1734–1741. [Google Scholar] [CrossRef] [PubMed]
- Yanagihara, N.; Murakami, S.; Nishihara, S. Temporal bone fractures inducing facial nerve paralysis: A new classification and its clinical significance. Ear Nose Throat J. 1997, 76, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Brodie, H.A.; Thompson, T.C. Management of complications from 820 temporal bone fractures. Am. J. Otol. 1997, 18, 188–197. [Google Scholar] [PubMed]
- Kanona, H.; Anderson, C.; Lambert, A.; Al-Abdulwahed, R.; O’Byrne, L.; Vakharia, N.; Motter, D.; Offiah, C.; Adams, A.; Seymour, K.; et al. A large case series of temporal bone fractures at a UK major trauma centre with an evidence-based management protocol. J. Laryngol. Otol. 2020, 134, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.; Arango, M.; Balica, L.; Cottingham, R.; El-Sayed, H.; Farrell, B.; Fernandes, J.; Tamar, G.; Golden, N.; Hartzenberg, H.B.; et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury—Outcomes at 6 months. Lancet 2005, 365, 1957–1959. [Google Scholar] [PubMed]
- Alderson, P.; Roberts, I. Corticosteroids for acute traumatic brain injury. Cochrane Database Syst. Rev. 2005, CD000196. [Google Scholar] [CrossRef] [PubMed]
- Gantz, B.J.; Rubinstein, J.T.; Gidley, P.; Woodworth, G.G. Surgical management of Bell’s palsy. Laryngoscope 1999, 109, 1177–1188. [Google Scholar] [CrossRef] [PubMed]
- Mannarelli, G.; Griffin, G.R.; Kileny, P.; Edwards, B. Electrophysiological measures in facial paresis and paralysis. Oper. Tech. Otolaryngol. Head Neck Surg. 2012, 23, 236–247. [Google Scholar] [CrossRef]
- Mehta, R.P. Surgical treatment of facial paralysis. Clin. Exp. Otorhinolaryngol. 2009, 2, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Sofferman, R.A. Facial nerve injury and decompression. In Surgery of the Ear and Temporal Bone; Nadol, J.B., Jr., Mckenna, M.J., Eds.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2005; pp. 435–450. [Google Scholar]
| Race | Before (n = 136) | During (n = 32) | After (n = 196) | |
|---|---|---|---|---|
| White | 107 (78.7%) | 24 (75.0%) | 137 (69.9%) | |
| Black | 4 (2.9%) | 1 (3.1%) | 18 (9.2%) | |
| Other | 20 (14.7%) | 3 (9.4%) | 28 (14.3%) | |
| Unknown | 1 (0.7%) | 4 (12.5%) | 12 (6.1%) | |
| Asian | 4 (2.9%) | 0 (0.0%) | 0 (0.0%) | |
| American Indian | 0 (0%) | 0 (0.0%) | 1 (0.5%) | |
| Ethnicity | ||||
| Not Hispanic or Latino | 114 (83.8%) | 25 (78.1%) | 151 (77.0%) | |
| Hispanic | 21 (15.4%) | 3 (9.4%) | 31 (15.8%) | |
| Unknown | 1 (0.7%) | 4 (12.5%) | 14 (7.1%) | |
| Gender | ||||
| Male | 96 (70.6%) | 25 (78.1%) | 155 (79.1%) | |
| Female | 40 (29.4%) | 7 (21.9%) | 41 (20.9%) | |
| Age | ||||
| Median | 50.0 | 53.5 | 44.5 | |
| Mean | 49.0 (SD 20.3) | 50.6 (SD 21.2) | 45.6 (SD 19.3) | |
| Injury Location | Before (n = 136) | During (n = 32) | After (n = 196) | |
|---|---|---|---|---|
| Street/highway | 56 (41.2%) | 12 (37.5%) | 70 (35.7%) | |
| Private residence | 41 (30.1%) | 9 (28.1%) | 63 (32.1%) | |
| Public location | 17 (12.5%) | 6 (18.8%) | 20 (10.2%) | |
| Unknown | 13 (9.6%) | 5 (15.6%) | 30 (15.3%) | |
| Pedestrian/walkway | 4 (2.9%) | 0 (0.0%) | 9 (4.6%) | |
| Hospital | 2 (1.5%) | 0 (0.0%) | 1 (0.5%) | |
| Construction site | 3 (2.2%) | 0 (0.0%) | 3 (1.5%) | |
| Mechanism of injury | ||||
| Motor vehicle collision | 23 (16.9%) | 6 (18.8%) | 32 (16.3%) | |
| Fall | 54 (39.7%) | 15 (46.9%) | 60 (30.6%) | |
| Motorcycle collision | 20 (14.7%) | 3 (9.4%) | 52 (26.5%) | |
| Bicycle | 3 (2.2%) | 1 (3.1%) | 6 (3.1%) | |
| Pedestrian | 11 (8.1%) | 4 (12.5%) | 13 (6.6%) | |
| Gun | 3 (2.2%) | 1 (3.1%) | 5 (2.6%) | |
| Assault | 10 (7.4%) | 1 (3.1%) | 7 (3.6%) | |
| Unknown | 2 (1.5%) | 0 (0.0%) | 11 (5.6%) | |
| Other blunt mechanism | 9 (6.6%) | 1 (3.1%) | 10 (5.1%) | |
| Injury type | ||||
| Blunt | 131 (96.3%) | 30 (93.8%) | 188 (95.9%) | |
| Penetrating | 5 (3.7%) | 2 (6.3%) | 8 (4.1%) | |
| Fracture laterality | ||||
| Right | 60 (44.1%) | 15 (46.9%) | 78 (39.8%) | |
| Left | 64 (47.1%) | 13 (40.6%) | 92 (46.9%) | |
| Bilateral | 12 (8.8%) | 4 (12.5%) | 26 (13.3%) | |
| Involvement of facial nerve | ||||
| No | 130 (95.6%) | 29 (90.6%) | 183 (93.4%) | |
| Yes | 6 (4.4%) | 3 (9.4%) | 13 (6.6%) | |
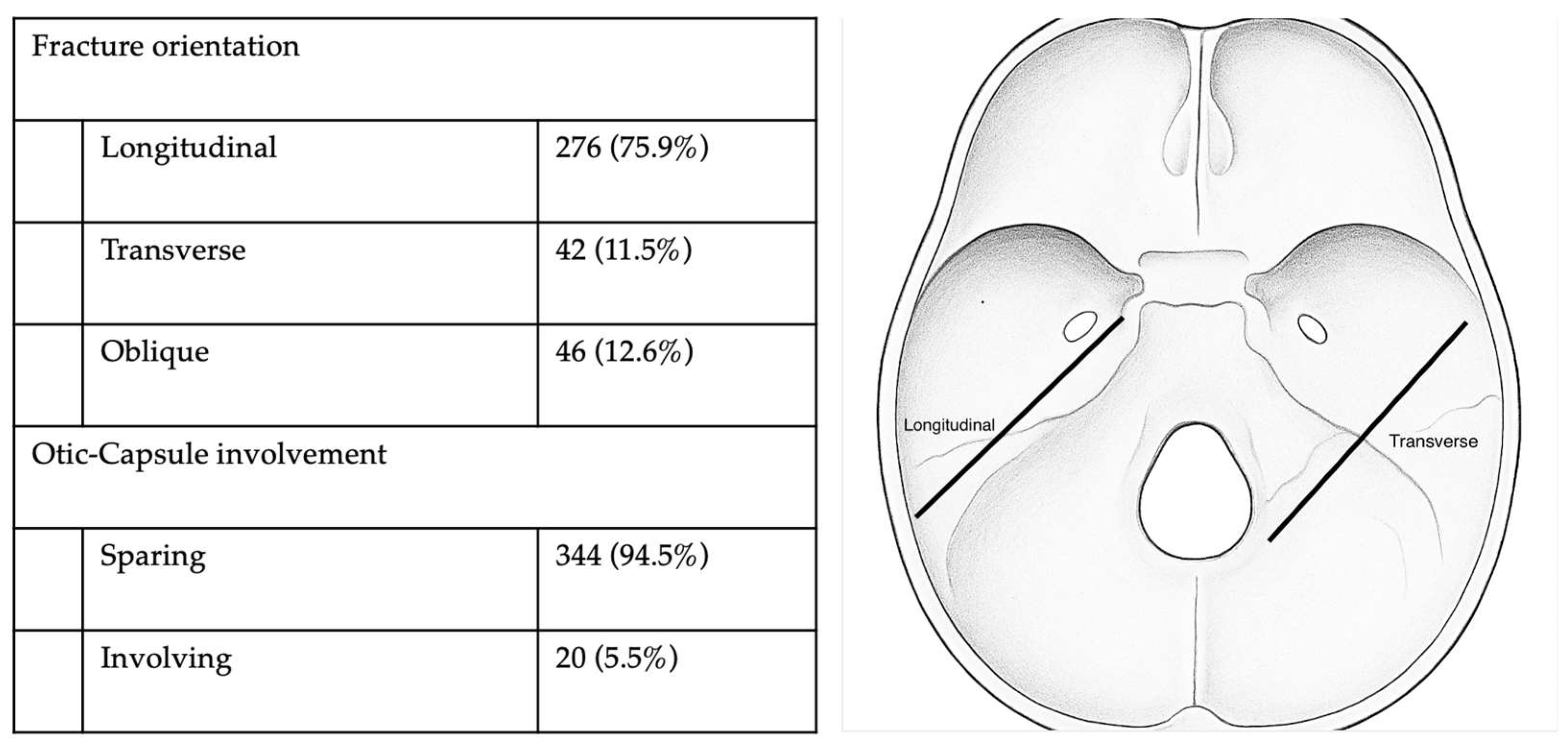
| Fracture orientation | ||||
| Longitudinal | 99 (72.8%) | 22 (68.8%) | 155 (79.1%) | |
| Transverse | 14 (10.3%) | 6 (18.8%) | 22 (11.2%) | |
| Oblique | 23 (16.9%) | 4 (12.5%) | 19 (9.7%) | |
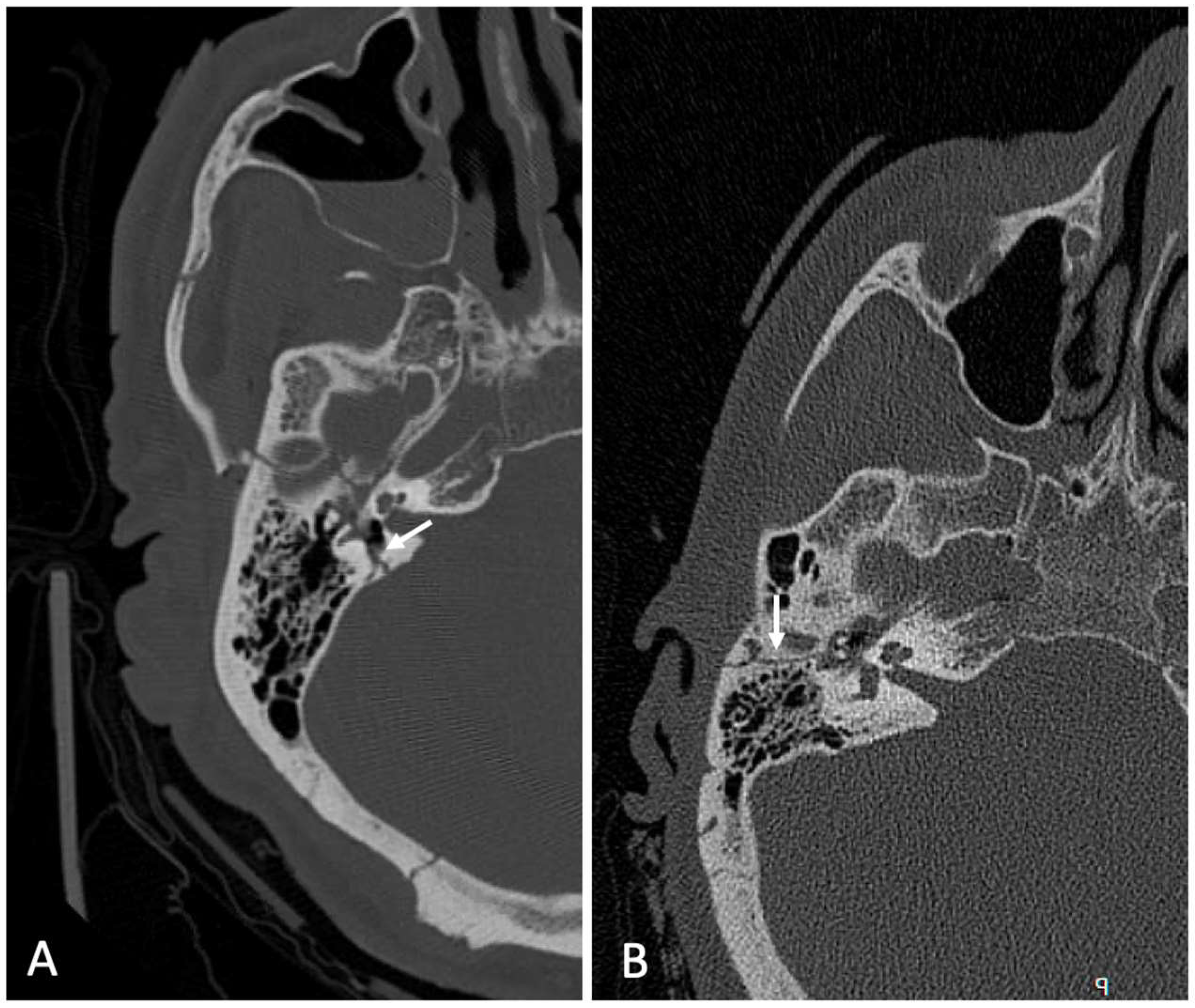
| Otic capsule involvement | ||||
| Sparing | 129 (94.9%) | 30 (93.8%) | 185 (94.4%) | |
| Involving | 7 (5.1%) | 2 (6.3%) | 11 (5.6%) | |
| Presence of Alcohol | Before (n = 136) | During (n = 32) | After (n = 196) | p-Value | |
|---|---|---|---|---|---|
| No | 87 (64.0%) | 21 (65.6%) | 136 (69.4%) | 0.562 | |
| Yes | 49 (36.0%) | 11 (34.4%) | 60 (30.6%) | ||
| Hospital length of stay (days) | |||||
| Median (IQR) | 130.5 (45.8, 306.8) | 59.0 (20.3, 180.5) | 164.0 (58.5, 413.5) | 0.011 | |
| Mean (SD) | 213.6 (238.5) | 183.1 (277.3) | 300.6 (321.7) | ||
| Days in intensive care unit | |||||
| Median (IQR) | 3.0 (0.0, 7.3) | 0.5 (0.0, 4.0) | 3.0 (0.0, 9.0) | 0.035 | |
| Mean (SD) | 6.1 (11.8) | 3.9 (6.8) | 7.8 (11.7) | ||
| Days on ventilator | |||||
| Median (IQR) | 1.0 (0.0, 5.0) | 1.0 (0.0, 2.0) | 2.0 (0.0, 6.0) | 0.241 | |
| Mean (SD) | 4.7 (8.8) | 3.3 (6.5) | 7.1 (15.7) | ||
| Mortality status | |||||
| Alive | 108 (79.4%) | 23 (71.9%) | 158 (80.6%) | 0.500 | |
| Dead | 28 (20.6%) | 9 (28.1%) | 38 (19.4%) | ||
| Injury Location | Injury to Facial Nerve (n = 22) | No Injury to Facial Nerve (n = 342) | p-Value | |
|---|---|---|---|---|
| Street/highway | 11 (50.0%) | 127 (37.1%) | 0.868 | |
| Private residence | 7 (31.8%) | 106 (31.0%) | ||
| Public location | 1 (4.5%) | 42 (12.3%) | ||
| Unknown | 3 (13.6%) | 45 (13.2%) | ||
| Pedestrian/walkway | 0 (0.0%) | 13 (3.8%) | ||
| Hospital | 0 (0.0%) | 3 (0.9%) | ||
| Construction site | 0 (0.0%) | 6 (1.8%) | ||
| Mechanism of injury | ||||
| Motor vehicle collision | 5 (22.7%) | 56 (16.4%) | 0.739 | |
| Fall | 8 (36.4%) | 121 (35.4%) | ||
| Motorcycle collision | 4 (18.2%) | 71 (20.8%) | ||
| Bicycle | 0 (0.0%) | 10 (2.9%) | ||
| Pedestrian | 1 (4.5%) | 27 (7.9%) | ||
| Gun | 2 (9.1%) | 7 (2.0%) | ||
| Assault | 1 (4.5%) | 17 (5.0%) | ||
| Unknown | 0 (0.0%) | 13 (3.8%) | ||
| Other blunt mechanism | 1 (4.5%) | 19 (5.6%) | ||
| Injury type | ||||
| Blunt | 20 (90.9%) | 329 (96.2%) | 0.227 | |
| Penetrating | 2 (9.1%) | 13 (3.8%) | ||
| Fracture orientation | ||||
| Longitudinal | 8 (36.4%) | 268 (78.4%) | <0.001 | |
| Transverse | 9 (40.9%) | 33 (9.6%) | ||
| Oblique | 5 (22.7%) | 41 (12.0%) | ||
| Otic capsule involvement | ||||
| Sparing | 11 (50.0%) | 333 (97.4%) | <0.001 | |
| Involving | 11 (50.0%) | 9 (2.6%) | ||
| Characteristics | n (%) |
|---|---|
| Partial/incomplete paralysis | 10 (45.5%) |
| Complete paralysis | 6 (27.3%) |
| Delayed weakness | 4 (18.2%); average time was 6.5 days (range: 3–9 days) |
| Cerebrospinal fluid (CSF) leak | 4 (18.2%) |
| High-dose steroids | 11 (50%) |
| Surgical decompression | 3 (13.6%); one regained function, two did not |
| Eye precautions (taping, lubricating eye drops) | 10 (45.5%); all with incomplete eye closure |
| Deceased before formal evaluation | 6 (27.3%) |
| Dexamethasone 8 mg every 8 h × 7 days, followed by Prednisone 80 mg once daily × 1 day, 70 mg × 1 day, 60 mg × 1 day, 50 mg × 1 day, 40 mg × 1 day, 30 mg × 1 day, 20 mg × 1 day, 10 mg × 1 day |
| Prednisone 60 mg once daily × 7 days, 40 mg × 3 days, 20 mg × 3 days, 10 mg × 2 days |
| Prednisone 60 mg once daily × 5 days, 40 mg × 2 days, 30 mg × 2 days, 20 mg × 2 days, 10 mg × 1 day |
| Prednisone 60 mg once daily × 3 days, 50 mg × 3 days, 40 mg × 2 days, 30 mg × 2 days, 10 mg × 2 days |
| Prednisone 40 mg once daily × 5 days, 60 mg × 2 days, 40 mg × 2 days, 20 mg × 2 days, 20 mg × 2 days 10 mg × 2 days |
| Dexamethasone 8 mg every 8 h × 7 days |
| Dexamethasone 8 mg every 8 h × 3 doses |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jongbloed, W.M.; Campbell, D.; Kuo, C.-L.; Zhong, K.; Cavanagh, N.J. A Five-Year Review of Temporal Bone Fractures at a Level One Trauma Center and Examination of the Impact of the COVID-19 Pandemic. Surgeries 2025, 6, 33. https://doi.org/10.3390/surgeries6020033
Jongbloed WM, Campbell D, Kuo C-L, Zhong K, Cavanagh NJ. A Five-Year Review of Temporal Bone Fractures at a Level One Trauma Center and Examination of the Impact of the COVID-19 Pandemic. Surgeries. 2025; 6(2):33. https://doi.org/10.3390/surgeries6020033
Chicago/Turabian StyleJongbloed, Walter M., Desiree Campbell, Chia-Ling Kuo, Kelin Zhong, and Norman J. Cavanagh. 2025. "A Five-Year Review of Temporal Bone Fractures at a Level One Trauma Center and Examination of the Impact of the COVID-19 Pandemic" Surgeries 6, no. 2: 33. https://doi.org/10.3390/surgeries6020033
APA StyleJongbloed, W. M., Campbell, D., Kuo, C.-L., Zhong, K., & Cavanagh, N. J. (2025). A Five-Year Review of Temporal Bone Fractures at a Level One Trauma Center and Examination of the Impact of the COVID-19 Pandemic. Surgeries, 6(2), 33. https://doi.org/10.3390/surgeries6020033






