Balancing Stability and Recovery: A Scoping Review on Conservative vs. Surgical Management of Acute Posterior Cruciate Ligament Injuries
Abstract
1. Introduction
2. Methods
2.1. Review Question
2.2. Eligibility Criteria
- Conservative treatment, which typically involves bracing, physiotherapy, quadriceps strengthening, and proprioceptive exercises.
- Surgical reconstruction, which includes techniques such as single-bundle or double-bundle reconstruction using autografts, allografts, or synthetic materials.
2.3. Exclusion Criteria
2.4. Search Strategy
- MEDLINE(PubMed):(“Posterior Cruciate Ligament”[MeSH Terms] OR “Posterior Cruciate Ligament Injury”[All Fields]) AND (“Conservative Treatment”[All Fields] OR “Rehabilitation”[All Fields]) AND (“Surgical Reconstruction”[All Fields] OR “Posterior Cruciate Ligament Reconstruction”[All Fields]) AND (“Function”[All Fields] OR “Return to Function”[All Fields]);
- Cochrane Central:1 “Posterior Cruciate Ligament” #2 “Rehabilitation” OR “Conservative Treatment” #3 “Surgical Reconstruction” OR “Reconstruction Surgery” #4 “Function” OR “Functional Recovery” #5 #1 AND (#2 OR #3) AND #4;
- Scopus:(TITLE-ABS-KEY(“Posterior Cruciate Ligament”) AND TITLE-ABS-KEY(“Conservative Treatment” OR “Rehabilitation”) AND TITLE-ABS-KEY(“Surgical Reconstruction” OR “Reconstructive Surgery”) AND TITLE-ABS-KEY(“Function” OR “Return to Function”));
- PEDro:“Posterior Cruciate Ligament” AND “Rehabilitation” AND “Reconstruction” AND “Function”;
- Web of Science:TS=(“Posterior Cruciate Ligament” AND (“Conservative Treatment” OR “Rehabilitation”) AND (“Surgical Reconstruction” OR “Reconstructive Surgery”) AND (“Function” OR “Return to Function”)).
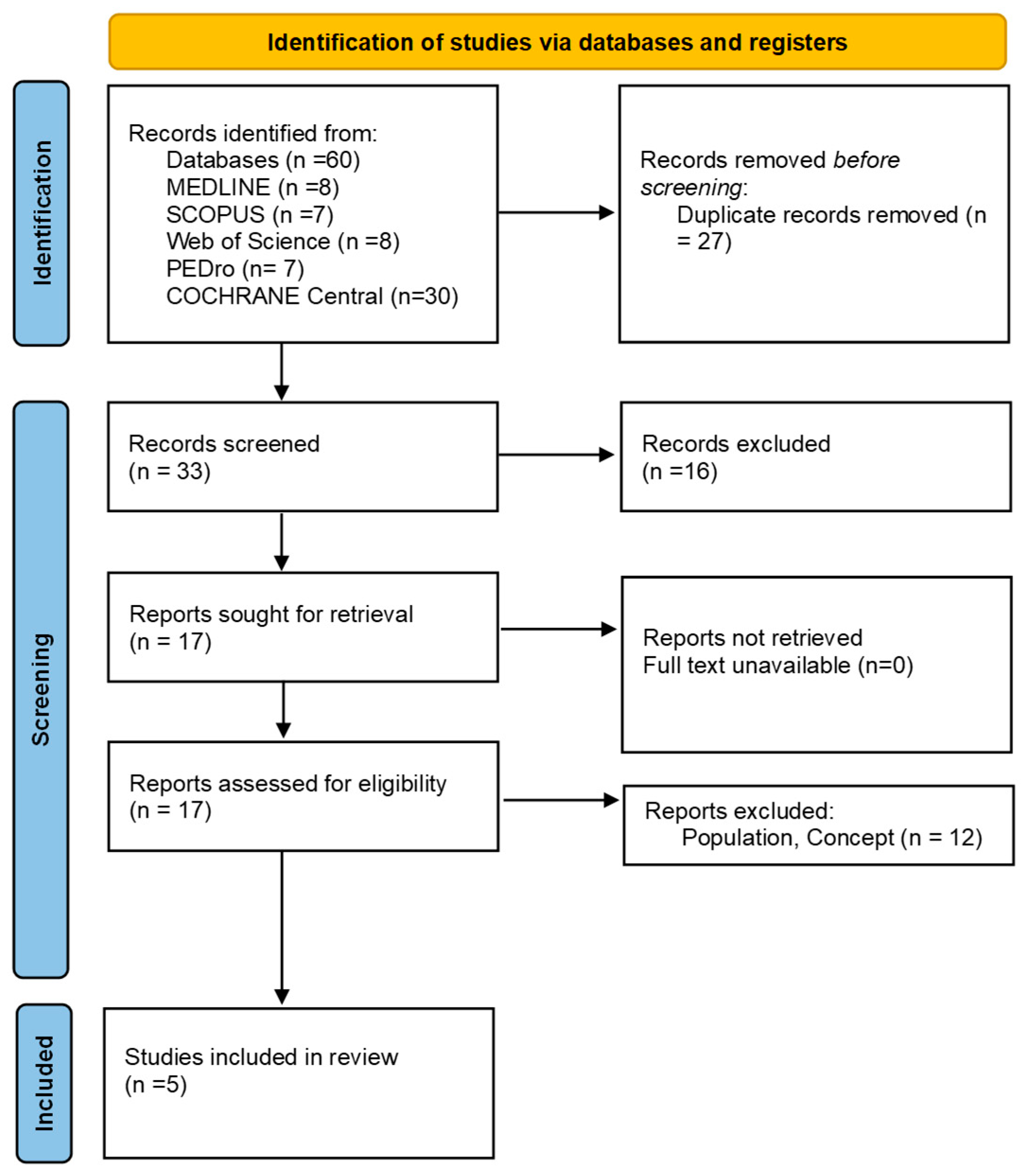
2.5. Study Selection
2.6. Data Extraction and Data Synthesis
3. Results
3.1. Functional Recovery
3.2. Stability
3.3. Long-Term Outcomes
3.4. Pain and Patient Satisfaction
4. Discussion
4.1. Limitations
4.2. Clinical Practice Implications
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Sanders, T.L.; Pareek, A.; Barrett, I.J.; Kremers, H.M.; Bryan, A.J.; Stuart, M.J.; Levy, B.A.; Krych, A.J. Incidence and Long-Term Follow-up of Isolated Posterior Cruciate Ligament Tears. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3017–3023. [Google Scholar] [CrossRef] [PubMed]
- Arthur, J.R.; Haglin, J.M.; Makovicka, J.L.; Chhabra, A. Anatomy and Biomechanics of the Posterior Cruciate Ligament and Their Surgical Implications. Sports Med. Arthrosc. Rev. 2020, 28, e1–e10. [Google Scholar] [CrossRef] [PubMed]
- Piskin, D.; Cobani, G.; Lehmann, T.; Büchel, D.; Baumeister, J. Cortical Changes Associated with an Anterior Cruciate Ligament Injury May Retrograde Skilled Kicking in Football: Preliminary EEG Findings. Sci. Rep. 2025, 15, 2208. [Google Scholar] [CrossRef]
- Zsidai, B.; Winkler, P.W.; Naarup, E.; Olsson, E.; Horvath, A.; Moatshe, G.; Lind, M.; Musahl, V.; Hamrin Senorski, E.; Samuelsson, K. Evaluation of Factors Associated with Short-Term Failure After Primary Isolated PCL Reconstruction: A Study of Patients From the Swedish and Norwegian Knee Ligament Registries. Orthop. J. Sports Med. 2025, 13, 23259671241305191. [Google Scholar] [CrossRef]
- Ricci, V.; Mezian, K.; Cocco, G.; Donati, D.; Naňka, O.; Farì, G.; Özçakar, L. Anatomy and Ultrasound Imaging of the Tibial Collateral Ligament: A Narrative Review. Clin. Anat. 2022, 35, 571–579. [Google Scholar] [CrossRef]
- Kew, M.E.; Cavanaugh, J.T.; Elnemer, W.G.; Marx, R.G. Return to Play after Posterior Cruciate Ligament Injuries. Curr. Rev. Musculoskelet. Med. 2022, 15, 606–615. [Google Scholar] [CrossRef]
- Fanelli, G.C.; Edson, C.J. Combined Posterior Cruciate Ligament-Posterolateral Reconstructions with Achilles Tendon Allograft and Biceps Femoris Tendon Tenodesis: 2- to 10-Year Follow-Up. Arthroscopy 2004, 20, 339–345. [Google Scholar] [CrossRef]
- Swenson, D.M.; Collins, C.L.; Best, T.M.; Flanigan, D.C.; Fields, S.K.; Comstock, R.D. Epidemiology of Knee Injuries among U.S. High School Athletes, 2005/2006–2010/2011. Med. Sci. Sports Exerc. 2013, 45, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Shelbourne, K.D.; Davis, T.J.; Patel, D.V. The Natural History of Acute, Isolated, Nonoperatively Treated Posterior Cruciate Ligament Injuries. A Prospective Study. Am. J. Sports Med. 1999, 27, 276–283. [Google Scholar] [CrossRef]
- Tucker, C.J.; Cotter, E.J.; Waterman, B.R.; Kilcoyne, K.G.; Cameron, K.L.; Owens, B.D. Functional Outcomes After Isolated and Combined Posterior Cruciate Ligament Reconstruction in a Military Population. Orthop. J. Sports Med. 2019, 7, 2325967119875139. [Google Scholar] [CrossRef]
- Vaquero-Picado, A.; Rodríguez-Merchán, E.C. Isolated Posterior Cruciate Ligament Tears: An Update of Management. EFORT Open Rev. 2017, 2, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Fanelli, G.C.; Beck, J.D.; Edson, C.J. Current Concepts Review: The Posterior Cruciate Ligament. J. Knee Surg. 2010, 23, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Tedeschi, R. Adapting RegentK Principles for Nonsurgical Meniscal Tear Management: An Innovative Case Report. Man. Med. 2024, 1–6. [Google Scholar] [CrossRef]
- Tedeschi, R.; Giorgi, F. What Is Known about the RegentK Regenerative Treatment for Ruptured Anterior Cruciate Ligament? A Scoping Review. Man. Med. 2023, 61, 181–187. [Google Scholar] [CrossRef]
- Schroven, W.; Vles, G.; Verhaegen, J.; Roussot, M.; Bellemans, J.; Konan, S. Operative Management of Isolated Posterior Cruciate Ligament Injuries Improves Stability and Reduces the Incidence of Secondary Osteoarthritis: A Systematic Review. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1733–1743. [Google Scholar] [CrossRef]
- Hooper, P.O.; Silko, C.; Malcolm, T.L.; Farrow, L.D. Management of Posterior Cruciate Ligament Tibial Avulsion Injuries: A Systematic Review. Am. J. Sports Med. 2018, 46, 734–742. [Google Scholar] [CrossRef]
- Simhal, R.K.; Bovich, M.; Bahrun, E.A.; Dreese, J.C. Postoperative Rehabilitation of Posterior Cruciate Ligament Surgery: A Systematic Review. Sports Med. Arthrosc. Rev. 2021, 29, 81–87. [Google Scholar] [CrossRef]
- Rochecongar, G.; Plaweski, S.; Azar, M.; Demey, G.; Arndt, J.; Louis, M.-L.; Limozin, R.; Djian, P.; Sonnery-Cottet, B.; Bousquet, V.; et al. Management of Combined Anterior or Posterior Cruciate Ligament and Posterolateral Corner Injuries: A Systematic Review. Orthop. Traumatol. Surg. Res. 2014, 100, S371–S378. [Google Scholar] [CrossRef]
- Tedeschi, R.; Platano, D.; Giorgi, F.; Donati, D. To Operate or Not? Evaluating the Best Approach for First-Time Patellar Dislocations: A Review. J. Clin. Med. 2024, 13, 5434. [Google Scholar] [CrossRef]
- Wind, W.M.; Bergfeld, J.A.; Parker, R.D. Evaluation and Treatment of Posterior Cruciate Ligament Injuries: Revisited. Am. J. Sports Med. 2004, 32, 1765–1775. [Google Scholar] [CrossRef]
- Ahn, S.; Lee, Y.S.; Song, Y.D.; Chang, C.B.; Kang, S.B.; Choi, Y.S. Does Surgical Reconstruction Produce Better Stability than Conservative Treatment in the Isolated PCL Injuries? Arch. Orthop. Trauma. Surg. 2016, 136, 811–819. [Google Scholar] [CrossRef]
- Boynton, M.D.; Tietjens, B.R. Long-Term Followup of the Untreated Isolated Posterior Cruciate Ligament-Deficient Knee. Am. J. Sports Med. 1996, 24, 306–310. [Google Scholar] [CrossRef]
- Hughston, J.C.; Andrews, J.R.; Cross, M.J.; Moschi, A. Classification of Knee Ligament Instabilities. Part I. The Medial Compartment and Cruciate Ligaments. J. Bone Jt. Surg. Am. 1976, 58, 159–172. [Google Scholar] [CrossRef]
- Panchal, H.B.; Sekiya, J.K. Open Tibial Inlay versus Arthroscopic Transtibial Posterior Cruciate Ligament Reconstructions. Arthroscopy 2011, 27, 1289–1295. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-M.; Lee, C.A.; Matava, M.J. Clinical Results of Arthroscopic Single-Bundle Transtibial Posterior Cruciate Ligament Reconstruction: A Systematic Review. Am. J. Sports Med. 2011, 39, 425–434. [Google Scholar] [CrossRef]
- Farì, G.; Mancini, R.; Dell’Anna, L.; Ricci, V.; Della Tommasa, S.; Bianchi, F.P.; Ladisa, I.; De Serio, C.; Fiore, S.; Donati, D.; et al. Medial or Lateral, That Is the Question: A Retrospective Study to Compare Two Injection Techniques in the Treatment of Knee Osteoarthritis Pain with Hyaluronic Acid. J. Clin. Med. 2024, 13, 1141. [Google Scholar] [CrossRef]
- Voos, J.E.; Mauro, C.S.; Wente, T.; Warren, R.F.; Wickiewicz, T.L. Posterior Cruciate Ligament: Anatomy, Biomechanics, and Outcomes. Am. J. Sports Med. 2012, 40, 222–231. [Google Scholar] [CrossRef]
- Spiridonov, S.I.; Slinkard, N.J.; LaPrade, R.F. Isolated and Combined Grade-III Posterior Cruciate Ligament Tears Treated with Double-Bundle Reconstruction with Use of Endoscopically Placed Femoral Tunnels and Grafts: Operative Technique and Clinical Outcomes. J. Bone Jt. Surg. Am. 2011, 93, 1773–1780. [Google Scholar] [CrossRef] [PubMed]
- Garofalo, R.; Jolles, B.M.; Moretti, B.; Siegrist, O. Double-Bundle Transtibial Posterior Cruciate Ligament Reconstruction with a Tendon-Patellar Bone-Semitendinosus Tendon Autograft: Clinical Results with a Minimum of 2 Years’ Follow-Up. Arthroscopy 2006, 22, 1331–1338.e1. [Google Scholar] [CrossRef]
- Winkler, P.W.; Zsidai, B.; Wagala, N.N.; Hughes, J.D.; Horvath, A.; Senorski, E.H.; Samuelsson, K.; Musahl, V. Evolving Evidence in the Treatment of Primary and Recurrent Posterior Cruciate Ligament Injuries, Part 1: Anatomy, Biomechanics and Diagnostics. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Forster, I.W.; Warren-Smith, C.D.; Tew, M. Is the KT1000 Knee Ligament Arthrometer Reliable? J. Bone Jt. Surg. Br. 1989, 71, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Gross, M.L.; Grover, J.S.; Bassett, L.W.; Seeger, L.L.; Finerman, G.A. Magnetic Resonance Imaging of the Posterior Cruciate Ligament. Clinical Use to Improve Diagnostic Accuracy. Am. J. Sports Med. 1992, 20, 732–737. [Google Scholar] [CrossRef] [PubMed]
- MacGillivray, J.D.; Stein, B.E.S.; Park, M.; Allen, A.A.; Wickiewicz, T.L.; Warren, R.F. Comparison of Tibial Inlay versus Transtibial Techniques for Isolated Posterior Cruciate Ligament Reconstruction: Minimum 2-Year Follow-Up. Arthroscopy 2006, 22, 320–328. [Google Scholar] [CrossRef]
- Rasmussen, R.G.; Jacobsen, J.S.; Blaabjerg, B.; Nielsen, T.G.; Miller, L.L.; Lind, M. Patient-Reported Outcomes and Muscle Strength after a Physiotherapy-Led Exercise and Support Brace Intervention in Patients with Acute Injury of the Posterior Cruciate Ligament: A Two-Year Follow-up Study. Int. J. Sports Phys. Ther. 2023, 18, 807–819. [Google Scholar] [CrossRef]
- Shelbourne, K.D.; Clark, M.; Gray, T. Minimum 10-Year Follow-up of Patients after an Acute, Isolated Posterior Cruciate Ligament Injury Treated Nonoperatively. Am. J. Sports Med. 2013, 41, 1526–1533. [Google Scholar] [CrossRef]
- Jung, Y.B.; Tae, S.K.; Lee, Y.S.; Jung, H.J.; Nam, C.H.; Park, S.J. Active Non-Operative Treatment of Acute Isolated Posterior Cruciate Ligament Injury with Cylinder Cast Immobilization. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 729–733. [Google Scholar] [CrossRef]
- Lien, O.A.; Aas, E.J.-L.; Johansen, S.; Ludvigsen, T.C.; Figved, W.; Engebretsen, L. Clinical Outcome after Reconstruction for Isolated Posterior Cruciate Ligament Injury. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1568–1572. [Google Scholar] [CrossRef] [PubMed]
- Peters: Joanna Briggs Institute Reviewer’s Manual, JBI. Available online: https://scholar-google-com.ezproxy.unibo.it/scholar_lookup?hl=en&publication_year=2020&author=MDJ+Peters&author=C+Godfrey&author=P+McInerney&author=Z+Munn&author=AC+Tricco&author=H+Khalil&title=Joanna+Briggs+Institute+Reviewer%27s+Manual%2C+JBI (accessed on 9 June 2022).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Jung, Y.-B.; Jung, H.-J.; Song, K.-S.; Kim, J.Y.; Lee, H.J.; Lee, J.-S. Remnant Posterior Cruciate Ligament-Augmenting Stent Procedure for Injuries in the Acute or Subacute Stage. Arthroscopy 2010, 26, 223–229. [Google Scholar] [CrossRef]

| Author, Year, and Study Type | Methods | Results | Outcomes Achieved |
|---|---|---|---|
| Rasmussen et al., 2023 (Case Series) [34] | Evaluated 50 patients with acute isolated PCL injury using supervised physiotherapy and bracing over 2 years. Assessed IKDC, STSD, and muscle strength. | Significant improvement in IKDC score (35 to 67, p < 0.001). Minimal change in STSD. Muscle strength increased by 16% for knee flexors. | Functional improvement with low risk of surgical intervention. Moderate persistence of posterior instability. |
| Shelbourne et al., 2013 (Case Series) [35] | Long-term follow-up (10+ years) of 133 patients treated conservatively for acute isolated PCL injury. Evaluated ROM, STSD, and subjective scales. | Minimal loss of ROM; stable STSD measures. Osteoarthritis observed in 11.4%. IKDC scores averaged 73.4/100 after 10 years. | Sustained functional recovery with moderate long-term risks of osteoarthritis and instability. |
| Jung et al., 2008 (Prospective Study) [36] | Investigated immobilisation with a cylinder cast and brace in 17 patients with acute isolated PCL injuries. Measured STSD, IKDC, and CKRS over 6 months. | STSD decreased significantly from 6.2 mm to 2.97 mm (p < 0.05). IKDC scores showed 35.3% of patients as normal and 64.7% as nearly normal. | High satisfaction with conservative treatment. Reduction in instability and functional improvement. |
| Lien et al., 2010 (Retrospective) [37] | Evaluated 43 patients undergoing surgical PCL reconstruction with a 4-year follow-up. Measured ROM, STSD, IKDC, and Tegner scores. | Mean IKDC score at follow-up was 63/100. Tegner Activity Scale score decreased from 7 (pre-injury) to 6. Persistent instability in some cases. | Moderate functional recovery with persistent posterior instability. |
| Jung et al., 2010 (Case Series) [40] | Investigated augmented stent procedure in 20 patients with acute/subacute PCL injuries. Evaluated STSD and IKDC. | Significant reduction in STSD (8.2 mm to 2.7 mm, p < 0.001). IKDC scores: 85% normal or nearly normal after 3 years. | High stability and functional outcomes post-surgery. |
| Kew et al., 2022 (Narrative Review) [6] | Summarised evidence on conservative vs. surgical PCL treatments, including rehabilitation protocols and return-to-play criteria. | Greater posterior laxity in conservatively treated patients (8 mm vs. 1.4 mm). Similar IKDC and Tegner scores between groups. | Both treatments enable return to function, with reduced degenerative changes in surgical cases. |
| Study | Age (years) | Sex (M/F) | BMI (kg/m²) | Conservative Treatment Type | Follow-up Time | Surgical Technique | Graft Type | IKDC Score (avg.) | STSD Reduction (mm) | Long-Term OA (%) | Functional Recovery | Patient Satisfaction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rasmussen et al., 2023 [34] | 32 | M 70%, F 30% | 24.5 | Bracing, physiotherapy | 24 months | - | - | 67 | 0 | - | Significant | High |
| Shelbourne et al., 2013 [35] | 30 | M 75%, F 25% | 25.2 | Rehabilitation program | 10+ years | - | - | 73.4 | - | 11.4 | Sustained | Moderate |
| Jung et al., 2008 [36] | 28 | M 80%, F 20% | 23.9 | Cylinder cast immobilization | 6 months | - | - | 90.3 | 3.23 | - | High | High |
| Lien et al., 2010 [37] | 29 | M 85%, F 15% | 26.1 | - | 48 months | Single-bundle reconstruction | Autograft | 63 | - | - | Moderate | Moderate |
| Jung et al., 2010 [40] | 31 | M 78%, F 22% | 24.8 | - | 36 months | Double-bundle reconstruction | Allograft | 85.4 | 5.5 | - | High | High |
| Kew et al., 2022 [6] | - | - | - | Both approaches analysed | Review | - | - | - | 1.4 (Surg)/8 (Cons) | - | Comparable | Comparable |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tedeschi, R.; Giorgi, F.; Platano, D.; Berti, L.; Vita, F.; Donati, D. Balancing Stability and Recovery: A Scoping Review on Conservative vs. Surgical Management of Acute Posterior Cruciate Ligament Injuries. Surgeries 2025, 6, 24. https://doi.org/10.3390/surgeries6010024
Tedeschi R, Giorgi F, Platano D, Berti L, Vita F, Donati D. Balancing Stability and Recovery: A Scoping Review on Conservative vs. Surgical Management of Acute Posterior Cruciate Ligament Injuries. Surgeries. 2025; 6(1):24. https://doi.org/10.3390/surgeries6010024
Chicago/Turabian StyleTedeschi, Roberto, Federica Giorgi, Daniela Platano, Lisa Berti, Fabio Vita, and Danilo Donati. 2025. "Balancing Stability and Recovery: A Scoping Review on Conservative vs. Surgical Management of Acute Posterior Cruciate Ligament Injuries" Surgeries 6, no. 1: 24. https://doi.org/10.3390/surgeries6010024
APA StyleTedeschi, R., Giorgi, F., Platano, D., Berti, L., Vita, F., & Donati, D. (2025). Balancing Stability and Recovery: A Scoping Review on Conservative vs. Surgical Management of Acute Posterior Cruciate Ligament Injuries. Surgeries, 6(1), 24. https://doi.org/10.3390/surgeries6010024






