Abstract
Background: Robotic systems have the potential to significantly enhance the accuracy and outcomes of spinal surgery. Adopting this new technology requires an examination of its learning curve and influencing factors. This study analyzes the learning curve associated with using the Mazor X Stealth Edition system for pedicle screw placement and performs a matched-pair analysis to compare operative durations between robot-assisted and navigation-based surgeries, evaluating the efficiency of the robotic system. Methods: We collected retrospective operative data from patients who underwent robot-assisted pedicle screw placements between December 2020 and June 2024 and conducted a cumulative sum (CuSUM) analysis to assess the learning curve, focusing on the robotic system’s setup duration. Additionally, we compared a group of patients who underwent robot-assisted pedicle screw placements with a pair-matched group who underwent O-arm-based navigation-assisted pedicle screw placements. Results: There was a notable decrease in the robotic setup duration, with a significant shift in trend observed after the first 20 cases. While the initial setup time was 24 minutes, it reduced to 17 minutes in later cases, reflecting a marked improvement in efficiency as the surgeon gained more experience with the robot. Conclusion: Our findings indicate there were no added difficulties using the robotic system compared to the navigation system. Moreover, the learning curve for the robotic system can be quickly surmounted, and it offers clear advantages over previous systems, making it a valuable tool for pedicle screw application.
1. Introduction
In the rapidly advancing field of surgical technology, robotic systems have become increasingly significant, revolutionizing how surgeries are performed and markedly improving patient outcomes [1,2,3]. This is especially true in the realm of spinal surgery, in which these innovative systems are proving to be exceptionally beneficial. Robotic systems in spinal surgery represent a major leap forward in terms of precision and control [4,5]. By integrating robotic guidance with real-time navigation technologies, these systems enable surgeons to execute complex procedures with enhanced precision [6,7,8]. This capability is crucial in spinal surgery, in which even minor errors can lead to significant complications or suboptimal results.
The first robotic system for spinal surgery, SpineAssist (Mazor Robotics Ltd., Caesarea, Israel), received FDA approval in 2004, marking a significant milestone in the adoption of robotics within spinal surgery [9]. Today, the advanced third-generation Mazor X Stealth Edition from Medtronic (Medtronic Inc., Dublin, Ireland) integrates the features of Mazor X with Medtronic’s Stealth intraoperative navigation system [9]. In addition to this system, several other robotic systems are currently being used in spinal surgery. These include the ROSA Surgical Robot (Medtech, Zimmer-Biomet, Warsaw, IN, USA), the ExcelsiusGPS Robotic Guidance and Navigation System (Globus Medical Inc., Audubon, PA, USA), the CUVIS Spine (Curexo Inc., Seoul, Korea), the CirQ Robotic Arm (BrainLAB AG, Munich, Germany), and the TIVAVI system, co-designed by Beijing Jishuitan Hospital and Beijing Tinavi Medical Technologies Co., Ltd. (Beijing, China) [9].
The introduction of these new technologies necessitates a thorough evaluation of both their efficiency and the learning curve associated with their adoption. The learning curve in robotic spinal surgery reflects the journey from a novice to an expert level of proficiency. This progression includes the acquisition of essential technical skills, development of surgical judgment, and the capability to troubleshoot and adapt to complex clinical scenarios. Exploring the learning curve involves analyzing how quickly and effectively surgeons can master the use of robotic systems and what factors may influence this process.
This study aims to evaluate the learning curve associated with adopting the Mazor X Stealth Edition robotic system (Medtronic Inc., Dublin, Ireland) for pedicle screw application in spinal surgery, providing insights into the practical challenges and training period required for surgeons to achieve proficiency. By analyzing the speed at which surgeons become adept with this technology, this study offers valuable information on the effectiveness of current training protocols and the potential need for additional resources. Additionally, we conduct a comparative analysis of surgical outcomes between robot-assisted procedures and traditional navigation-based surgeries, focusing on metrics such as operative duration to assess whether the robotic system offers significant advantages in terms of efficiency and overall patient outcomes. This specific evaluation aims to inform training programs, enhance surgical practices, and influence decisions regarding the broader adoption of robotic systems in spinal surgery.
2. Materials and Methods
2.1. Patients
After approval from the National Healthcare Group, Domain Specific Review Board, Singapore, we conducted a retrospective study (Ref. No. 2024-3041) that included all patients who received robot-assisted pedicle screws placed by a fellowship-trained spinal surgeon using the Mazor X Stealth Edition system at our institution from December 2020 to June 2024. The focus of our study was specifically on surgeries performed with the merged CT-fluoro modality provided by the robotic system, while we excluded surgeries conducted using the scan-and-plan modality. Additionally, cases in which the robotic system was aborted due to technical issues were not included in the analysis.
To further assess the effectiveness and outcomes of the robot-assisted surgeries, we performed a matched-pair analysis. This required assessment of a subset of patients who underwent pedicle screw placements with the assistance of the O-arm-based intraoperative navigation system between January 2022 and December 2023. This comparison aimed to evaluate the relative performance and outcomes of the Mazor X Stealth Edition system against the O-arm navigation-based system which we previously used at our institution.
The data collected for analysis included a range of patient and surgical characteristics. Patient demographics such as age, gender, and primary diagnosis were documented to provide context for the outcomes. Surgical characteristics recorded included the specific spinal levels treated, the surgical approach employed, the time required to set up the robotic system, and the total duration of the operative procedure. These data were crucial for understanding the efficiency, accuracy, and overall effectiveness of robot-assisted pedicle screw placements in comparison to the O-arm navigation-based method.
2.2. Robotic Workflow
The robotic system can be utilized in two ways: the merged CT-fluoro method or scan-and-plan method [10,11,12]. The merged CT-fluoro method is a multi-step process that begins with comprehensive pre-operative planning using high-resolution CT imaging. This imaging provides detailed anatomical data and allows for precise planning of screw placements before the actual surgery. Once the patient is in the operating room, the CT images are integrated with real-time fluoroscopic imaging to guide the surgical process. The fluoroscopic images, taken during the surgery, are merged with the pre-operative CT scans to provide a dynamic, real-time view of the patient’s anatomy. This integration ensures a high degree of accuracy in screw placement and can enhance the overall precision of the surgical procedure. In contrast, the scan-and-plan method is another process which relies solely on intra-operative fluoroscopic imaging for both planning and guidance. This approach eliminates the need for pre-operative CT scans. Instead, the robotic system utilizes real-time fluoroscopic images to plan and execute the screw placements during the surgery. However, we prefer the merged CT-fluoro modality, and this study specifically examines its learning curve.
The process of using the robotic system with the merged CT-fluoro modality consists of six steps (Table 1). The first two steps are pre-operative: (1) obtaining CT imaging; and (2) planning screw placement. Here, the optimal diameter, size, and trajectory of the screw in all three planes are determined. The four intra-operative steps are (3) mounting the robotic system, (4) performing a topographical scan of the surgical field, (5) using C-arm imaging to merge with the pre-operative CT images, and (6) inserting the screws.

Table 1.
Robotic system workflow.
To mount the robotic system, the robot arm needs to be secured to the Jackson table using a specific mount located near the end of the table (Figure 1A). A sterile drape is placed over the robotic arm (Figure 1B), followed by the attachment of the robotic reference frame and arm guide. A single posterior superior iliac spine (PSIS) Schanz screw is then inserted as a reference point to anchor the robot to the patient (Figure 1C). A topographical scan of the surgical field is conducted to allow the robotic arm to execute efficient maneuvers (Figure 1D,E). The C-arm captures anteroposterior (AP) and lateral X-ray images of the targeted spinal levels (Figure 1F). These X-ray images are then merged with pre-operative CT images. This merging process is critical for aligning the robotic system’s guidance with the actual anatomy, ensuring that the planned screw placement can be executed precisely (Figure 1G,H). The pedicle preparation and screw insertion are then carried out with real-time robotic guidance, in which the robotic arm moves precisely along the predetermined trajectory to facilitate this process. Navigational tools are then inserted through the robotic arm into the pedicle to prepare it for screw application. While the robotic arm maintains a steady trajectory, screws are inserted, ensuring that each screw is placed in the exact intended position (Figure 1I–K).

Figure 1.
Robotic workflow. (A) Mounting of the robotic arm; (B) Sterile draping; (C) Posterior superior iliac spine (PSIS) Schanz screw anchor; (D,E) Topographical scan of the surgical field; (F) C-arm capturing anteroposterior (AP) and lateral X-ray images of the targeted spinal levels; (G,H) Toggle between CT and fluoro images of the same area, representing a precise merge of CT-fluoro modalities for execution of screw trajectory as planned; (I–K) Placement of screws; (J) Axial view as visualized in the display monitor; (H) Sagittal view as visualized in the display monitor.
2.3. Data Analysis
A CuSUM analysis was performed using “R” statistical analysis software (version 4.3.1) to evaluate the learning curve of robot-assisted spinal surgery. CuSUM analysis is a statistical method employed to monitor and evaluate the learning process in various fields, including surgery. It is particularly useful for tracking improvements in performance over time and identifying trends in learning curves [13,14]. In this study, the CuSUM analysis utilized the recorded robotic system setup times from a cohort of surgical cases. The robotic system setup time was specifically defined as the interval between the percutaneous insertion of the Schanz screw and the completion of the merged CT-fluoro method, which marks the point when the surgeon is prepared to begin pedicle screw insertion. By analyzing these setup times cumulatively, the CuSUM method provides insights into how the efficiency of the robotic setup evolves with increased experience and practice, highlighting any significant improvements or changes in performance over the course of the surgical cases.
In addition, a comparison of operative durations between robot-assisted and navigation-assisted pedicle screw placements, performed by the same surgeon and matched for surgical characteristics (such as levels of surgery, surgical approach, and type of decompression), was conducted to assess any differences in time taken between the two modalities. The robot-assisted cases for the comparative analysis were selected after the learning phase of the learning curve, specifically during the proficiency and competency phases. This ensures an accurate reflection of the robot’s use and benefits in surgery. For comparing continuous variables, the Shapiro–Wilk test was first applied to check for normality, and based on that, an unpaired t-test was used to determine if there were statistically significant differences between the procedures, with a significance level set at p < 0.05.
3. Results
Between December 2020 and June 2024, our institution conducted a total of 110 surgeries in which robotic assistance was utilized for the placement of pedicle screws. After applying the exclusion criteria, 100 cases were included in the analysis (Table 2). The study cohort consisted of 40 males and 60 females, with a mean age of 69.6 years, ranging from 34 to 81 years. The primary diagnoses were degenerative lumbar spinal stenosis in 99 cases and trauma in one case. Among these surgeries, 12 were performed using an open approach, while 88 were carried out with a minimally invasive approach.

Table 2.
Patient demographics.
The CuSUM curve reveals an initial upward trend throughout the first 20 surgeries, indicating a learning phase during which the surgeons’ skills were developed and their familiarity with the procedure increased (Figure 2). Following this period, the curve stabilized, suggesting a level of proficiency was reached. In the subsequent phase, the curve declined, reflecting a significant reduction in the duration of the robot’s setup as the efficiency improved. This trend indicates an enhancement in overall performance, suggesting increasing competence in executing these procedures effectively. Based on this, the first 20 cases were classified as the “early group”, representing the learning phase for the surgeon. The subsequent 80 cases were classified as the “late group”, reflecting the surgeon’s progression to proficiency and competency. The mean setup time for the early group was 24 min, while the mean setup time for the late group was reduced to 17 min. This difference in setup time was statistically significant (p < 0.001), indicating a substantial improvement in efficiency as the surgeon gained experience with the robotic system.
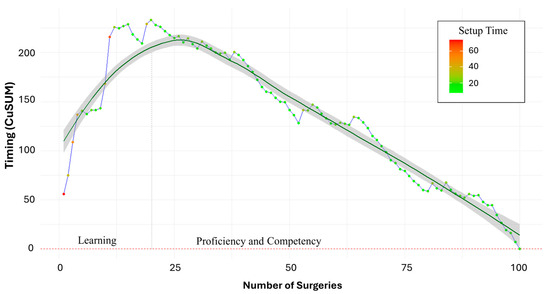
Figure 2.
CuSUM analysis of learning curve. A notable change in trend can be observed after the 20-case mark, signifying the transition from the learning phase to the proficiency phase. These first 20 cases were classified as the “early group”, and the subsequent 80 cases were classified as the “late group”.
The operative durations for the final 10 surgeries performed using the robotic system were compared with those of a matched set of 10 recent surgeries that utilized intra-operative O-arm navigation (Table 3). The analysis found no statistically significant difference in operative duration between the robotic and navigation systems, with a p-value of 0.21, indicating that the time required for surgery was similar for both systems. Importantly, the study found no occurrences of screw-related complications in any of the surgeries reviewed and the implants remained stable throughout the follow-up period (Figure 3). This suggests that the robotic system did not introduce additional risks related to screw placement, while providing enhanced accuracy and increased ease of implantation.

Table 3.
Matched-pair analysis of operative duration between robot-assisted and navigated spinal surgery.
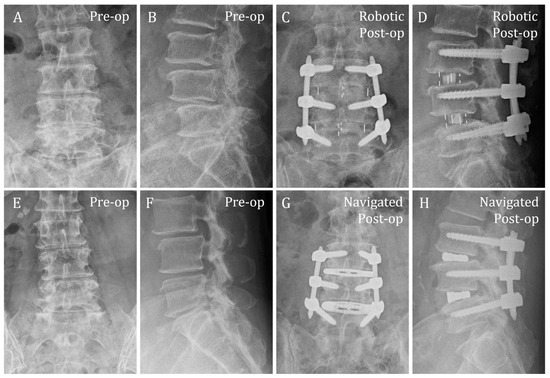
Figure 3.
Representative pre- and post-operative radiographs of patients who underwent two-level OLIF (L3–L5) and posterior stabilization, with pedicle screws placed using robotic and navigation assistance. (A–D) Robotic group; (E–H) Navigation group; (A,C,E,G) Antero-posterior views; (B,D,F,H) Lateral views.
4. Discussion
The advantage of robotic pedicle screw placement during spinal stabilization lies in its ability to seamlessly translate pre-operative surgical planning into highly precise intra-operative screw placement. This technology enables surgeons to create comprehensive and detailed surgical plans using CT scans before the procedure and execute them with remarkable accuracy during surgery. By leveraging robotic systems, the precision of screw placement is significantly enhanced, resulting in several key benefits [9,15,16]. Firstly, the meticulous planning facilitated by robotic assistance streamlines the surgical process. Surgeons can follow their planned approach with greater accuracy, leading to a reduction in operating room time. The robotic system’s advanced guidance and real-time feedback ensure that each step adheres closely to the pre-established plan, minimizing deviations that could affect the procedure’s success. This efficiency not only optimizes the surgical workflow but also improves patient outcomes by reducing the duration of anesthesia and surgical intervention. It also decreases the potential for serious injuries due to screw misplacement and improves overall patient safety.
Exploring straightforward comparisons between robot-assisted and navigation-assisted pedicle screw placement in the literature revealed that there are only a few studies making direct one-to-one comparisons. These studies are primarily focused on accuracy as highlighted below (Table 4). They indicate either an increased accuracy with robotic systems or a comparable accuracy to navigation systems. Additionally, comparisons between older and newer robotic systems demonstrate significantly less radiation exposure, lower robot abandonment rates, and reduced blood transfusion rates when using advanced systems, such as the Mazor X Stealth Edition [17].

Table 4.
One-to-one comparisons of robot-assisted and navigation-assisted pedicle screw placements.
The introduction of new technologies and techniques in surgery often raises concerns regarding their suitability and ease of adoption. This is particularly true when utilizing robotic assistance during spinal surgery, which, despite offering a superior level of precision compared to traditional methods, requires a careful evaluation of the learning curve associated with its implementation. Studying the learning curve is essential for understanding how readily surgeons can incorporate these new technologies into their practice. This involves assessing how quickly and effectively surgeons can adapt to robotic systems and integrate them into their procedures. Although robotic spinal surgery promises an enhanced accuracy and better surgical outcomes [19,23,24,25,26,27,28], the effective utilization of this technology necessitates both training and hands-on experience. Surgeons must become familiar with the robotic system’s interface, techniques, and workflow, which can differ significantly from traditional surgical methods.
Analyzing the learning curve provides valuable insights into how many cases a surgeon typically needs to perform before achieving proficiency in robot-assisted spinal surgery. This analysis also helps identify specific challenges and obstacles that may arise during the initial adoption phase. Understanding these challenges allows surgeons and healthcare institutions to develop strategies to overcome them. Moreover, this knowledge is crucial for making informed decisions about adopting robotic systems. It helps healthcare institutions plan and allocate resources effectively, including budgeting for training programs and support systems. Such programs can focus on common pitfalls, enhance hands-on training, and provide ongoing support to ease the transition for surgeons.
Several studies have explored the learning curve associated with robotic spinal surgery, revealing insights into how quickly surgeons can adapt to this advanced technology. For instance, Yu et al. evaluated robot-assisted pedicle screw application by two surgeons and found that the learning curve could be effectively navigated after approximately 17–18 cases, with their assessment primarily focusing on operation time [29]. By categorizing the cases into early and late phases, as in this study, they observed notable improvements in screw accuracy: from 87.50% to 96.30% for one surgeon and from 91.18% to 96.15% for the other. This indicates that, as surgeons gain experience with the robotic system, their accuracy in screw placement significantly improves, underscoring the potential for enhanced precision with continued use. Similarly, Torii et al. observed that screw insertion time, robot setting time, and registration time decreased as the number of surgical cases increased [30]. Surgeons typically master the learning curve after approximately 23 cases, as evidenced by a reduction in the screw insertion time. Specifically, the mean screw insertion time decreased from 3.2 min in the early cases to 2.7 min in the later cases, highlighting the efficiency achieved with increased experience in using the robotic system.
Our study builds upon this existing body of research by focusing on the setup time and further clarifying the learning curve for robotic spinal surgery. We found that the learning curve can be overcome after the first 20 cases, with notable improvements in setup efficiency. Initially, the setup time for the robotic system averaged between 37 and 44 min for early cases. However, this time significantly decreased to between 8 and 15 min as the number of cases increased. This reduction in setup time is attributed to the growing familiarity of the surgeon and operating room staff with the robotic technology, as well as the optimization of the system’s placement and workflow. As experience with the robotic system grows, the team becomes more adept at streamlining the setup process, which helps to minimize disruptions and prevent the unnecessary prolongation of the surgical procedure.
Efficient use of surgical technology is vital, as prolonged procedures can impact patient safety, increase anesthesia time, and potentially lead to higher rates of complications. Hence, it is crucial to ensure that new technologies in surgery are used efficiently and do not lead to extended operative times. Our pilot study investigated whether the robotic system, despite its advanced capabilities and additional setup requirements, affects the duration of spine surgeries compared to procedures performed with the O-arm navigation-based system that we previously used. The results of our study revealed no significant difference in the operative duration between the two methods. This finding is particularly encouraging as it indicates that the robotic system, while requiring some time for the initial setup, does not adversely affect the overall efficiency of the surgical procedure.
The lack of a significant difference in operative times suggests that the robotic system enables the effective use of its advanced features without compromising the overall efficiency of the surgical process. This indicates that surgeons can leverage the enhanced accuracy and reliability provided by the robotic system to perform their planned procedures with greater confidence and precision, all while avoiding the unnecessary prolongation of the surgery, creating a balance between efficiency and precision. Our findings also suggest that surgical efficiency is notably enhanced, especially in multi-level cases. In these scenarios, while the setup time for the robotic system remains consistent, time is saved with each additional screw inserted using the robot, thereby contributing to overall efficiency.
As a retrospective study, this research has limitations inherent to its design. Specifically, we did not evaluate surgeries utilizing the scan-and-plan method, and only focused on the merged CT-fluoro modality, as this method is predominantly used in our institution. Moreover, the comparison between robot-assisted and O-arm navigation-assisted pedicle screw placements was based on a limited number of cases. This sample size may not represent the broader population of patients undergoing these procedures, though our findings do suggest the most likely trend. Furthermore, all surgeries were performed by a single surgeon, which implies that the results may have been influenced by the experience of the surgeon and could vary with other surgeons. Our study did not examine postoperative recovery, complications, or functional or radiological outcomes, as there were no deviations from the normal course. These factors could have provided additional context to the learning curve and the overall effectiveness of the procedures.
5. Conclusions
Robot-assisted spinal surgery represents a significant advancement by enabling the precise translation of pre-operative plans for pedicle screw placements into accurate intra-operative execution. One of the key advantages of this technology is that its learning curve can be overcome relatively easily, allowing surgeons to achieve proficiency after initial training. This is supported by our CuSUM analysis, which demonstrates how quickly surgeons can become skilled in using the robotic system following their initial experience. This analysis highlighted a notable improvement in the setup time required for the robotic system, with a significant shift in the trend observed after the first 20 cases. While the initial setup time was 24 min, it decreased to 17 min in the later cases, reflecting a significant improvement in efficiency as the surgeon gained more experience with the robot. This reduction in setup time not only underscores the efficiency achieved by the surgeon but also reflects the broader impact on the overall operating room efficiency. Overall, beyond enhancing surgical precision, robotic systems streamline procedures and adapt quickly to the needs of the surgeon. These benefits make the robotic system a versatile and essential tool in modern spinal surgery, highlighting its value in enhancing accuracy, improving efficiency, and meeting the dynamic demands of surgical practice.
Author Contributions
Conceptualization, P.P.M.S., M.C.L., A.-K.K.-P., and J.Y.-L.O.; methodology, P.P.M.S., M.C.L., and J.Y.-L.O.; formal analysis, P.P.M.S. and M.C.L.; investigation, P.P.M.S., M.C.L., and A.-K.K.-P.; resources, J.Y.-L.O.; data curation, P.P.M.S. and M.C.L.; writing—original draft preparation, P.P.M.S. and M.C.L.; writing—review and editing, A.-K.K.-P. and J.Y.-L.O.; supervision, J.Y.-L.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study (Ref. No. 2024-3041) was conducted in accordance with the Declaration of Helsinki and was exempted from full review by the National Healthcare Group, Domain Specific Review Board, Singapore.
Informed Consent Statement
The requirement of informed consent was waived due to the retrospective nature of the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to ongoing studies utilizing the dataset.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Fairag, M.; Almahdi, R.H.; Siddiqi, A.A.; Alharthi, F.K.; Alqurashi, B.S.; Alzahrani, N.G.; Alsulami, A.; Alshehri, R. Robotic Revolution in Surgery: Diverse Applications Across Specialties and Future Prospects Review Article. Cureus 2024, 16, e52148. [Google Scholar] [CrossRef]
- Reddy, K.; Gharde, P.; Tayade, H.; Patil, M.; Reddy, L.S.; Surya, D. Advancements in Robotic Surgery: A Comprehensive Overview of Current Utilizations and Upcoming Frontiers. Cureus 2023, 15, e50415. [Google Scholar] [CrossRef]
- Rivero-Moreno, Y.; Echevarria, S.; Vidal-Valderrama, C.; Pianetti, L.; Cordova-Guilarte, J.; Navarro-Gonzalez, J.; Acevedo-Rodriguez, J.; Dorado-Avila, G.; Osorio-Romero, L.; Chavez-Campos, C.; et al. Robotic Surgery: A Comprehensive Review of the Literature and Current Trends. Cureus 2023, 15, e42370. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Fang, Y.; Jin, Z.; Wang, Y.; Yu, M. The impact of robot-assisted spine surgeries on clinical outcomes: A systemic review and meta-analysis. Int. J. Med. Robot. 2020, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Ong, V.; Swan, A.R.; Sheppard, J.P.; Ng, E.; Faung, B.; Diaz-Aguilar, L.D.; Pham, M.H. A Comparison of Spinal Robotic Systems and Pedicle Screw Accuracy Rates: Review of Literature and Meta-Analysis. Asian J. Neurosurg. 2022, 17, 547–556. [Google Scholar] [CrossRef]
- Benech, C.A.; Perez, R.; Benech, F.; Shirk, T.; Bucklen, B.S. A quantitative accuracy assessment of the use of a rigid robotic arm in navigated placement of 726 pedicle screws. BMC Surg. 2022, 22, 385. [Google Scholar] [CrossRef]
- Wallace, D.J.; Vardiman, A.B.; Booher, G.A.; Crawford, N.R.; Riggleman, J.R.; Greeley, S.L.; Ledonio, C.G. Navigated robotic assistance improves pedicle screw accuracy in minimally invasive surgery of the lumbosacral spine: 600 pedicle screws in a single institution. Int. J. Med. Robot. 2020, 16, e2054. [Google Scholar] [CrossRef] [PubMed]
- Garg, B.; Mehta, N.; Malhotra, R. Robotic spine surgery: Ushering in a new era. J. Clin. Orthop. Trauma. 2020, 11, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Cho, D.C.; Kim, K.T. Navigation-Guided/Robot-Assisted Spinal Surgery: A Review Article. Neurospine 2024, 21, 8–17. [Google Scholar] [CrossRef]
- Medtronic Spine & Orthopaedic Products—Mazor, X. Available online: https://www.medtronic.com/us-en/healthcare-professionals/therapies-procedures/spinal-orthopaedic/spine-robotics.html (accessed on 22 August 2024).
- Khan, A.; Soliman, M.A.R.; Lee, N.J.; Waqas, M.; Lombardi, J.M.; Boddapati, V.; Levy, L.C.; Mao, J.Z.; Park, P.J.; Mathew, J.; et al. CT-to-fluoroscopy registration versus scan-and-plan registration for robot-assisted insertion of lumbar pedicle screws. Neurosurg. Focus. 2022, 52, E8. [Google Scholar] [CrossRef] [PubMed]
- Avrumova, F.; Sivaganesan, A.; Alluri, R.K.; Vaishnav, A.; Qureshi, S.; Lebl, D.R. Workflow and Efficiency of Robotic-Assisted Navigation in Spine Surgery. HSS J. 2021, 17, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.L.; Zheng, F.; Shin, M.; Liu, X.; Oh, D.; D’Attilio, D. CUSUM learning curves: What they can and can’t tell us. Surg. Endosc. 2023, 37, 7991–7999. [Google Scholar] [CrossRef] [PubMed]
- Woodall, W.H.; Rakovich, G.; Steiner, S.H. An overview and critique of the use of cumulative sum methods with surgical learning curve data. Stat. Med. 2021, 40, 1400–1413. [Google Scholar] [CrossRef]
- Volk, V.L.; Steele, K.A.; Cinello-Smith, M.; Chua, R.V.; Pollina, J.; Poulter, G.; Shafa, E.; Busselberg, P.; Fitzpatrick, C.K. Pedicle Screw Placement Accuracy in Robot-Assisted Spinal Fusion in a Multicenter Study. Ann. Biomed. Eng. 2023, 51, 2518–2527. [Google Scholar] [CrossRef]
- Antonacci, C.L.; Zeng, F.; Block, A.; Davey, A.; Makanji, H. Robotic-assisted spine surgery-a narrative review. J. Spine Surg. 2024, 10, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.J.; Zuckerman, S.L.; Buchanan, I.; Boddapati, V.; Park, P.; Leung, E.; Mathew, J.; Buchholz, A.L.; Pollina, J.; Khan, A.; et al. P132. How does the Mazor X stealth edition compare with the Mazor X for robot-assisted spine surgery? A multicenter, propensity matched analysis of 2,800 screws and 372 patients. Spine J. 2021, 21, S205–S206. [Google Scholar] [CrossRef]
- Asada, T.; Subramanian, T.; Simon, C.Z.; Singh, N.; Hirase, T.; Araghi, K.; Lu, A.Z.; Mai, E.; Kim, Y.E.; Tuma, O.; et al. Level-specific comparison of 3D navigated and robotic arm-guided screw placement: An accuracy assessment of 1210 pedicle screws in lumbar surgery. Spine J. 2024, 24, 1872–1880. [Google Scholar] [CrossRef]
- Yu, T.; Jiao, J.H.; Wang, Y.; Wang, Q.Y.; Jiang, W.B.; Wang, Z.H.; Wu, M.F. Robot-assisted versus navigation-assisted screw placement in spinal vertebrae. Int. Orthop. 2023, 47, 527–532. [Google Scholar] [CrossRef]
- Shafi, K.A.; Pompeu, Y.A.; Vaishnav, A.S.; Mai, E.; Sivaganesan, A.; Shahi, P.; Qureshi, S.A. Does robot-assisted navigation influence pedicle screw selection and accuracy in minimally invasive spine surgery? Neurosurg. Focus. 2022, 52, E4. [Google Scholar] [CrossRef] [PubMed]
- Shahi, P.; Vaishnav, A.; Araghi, K.; Shinn, D.; Song, J.; Dalal, S.; Melissaridou, D.; Mai, E.; Dupont, M.; Sheha, E.; et al. Robotics Reduces Radiation Exposure in Minimally Invasive Lumbar Fusion Compared With Navigation. Spine 2022, 47, 1279–1286. [Google Scholar] [CrossRef]
- Khan, A.; Meyers, J.E.; Yavorek, S.; O’Connor, T.E.; Siasios, I.; Mullin, J.P.; Pollina, J. Comparing Next-Generation Robotic Technology with 3-Dimensional Computed Tomography Navigation Technology for the Insertion of Posterior Pedicle Screws. World Neurosurg. 2019, 123, e474–e481. [Google Scholar] [CrossRef] [PubMed]
- Al-Naseem, A.O.; Al-Muhannadi, A.; Ramadhan, M.; Alfadhli, A.; Marwan, Y.; Shafafy, R.; Abd-El-Barr, M.M. Robot-assisted pedicle screw insertion versus navigation-based and freehand techniques for posterior spinal fusion in scoliosis: A systematic review and meta-analysis. Spine Deform. 2024, 12, 1203–1215. [Google Scholar] [CrossRef] [PubMed]
- Jung, B.; Han, J.; Shahsavarani, S.; Abbas, A.M.; Echevarria, A.C.; Carrier, R.E.; Ngan, A.; Katz, A.D.; Essig, D.; Verma, R. Robotic-Assisted Versus Fluoroscopic-Guided Surgery on the Accuracy of Spine Pedicle Screw Placement: A Systematic Review and Meta-Analysis. Cureus 2024, 16, e54969. [Google Scholar] [CrossRef]
- Su, X.J.; Lv, Z.D.; Chen, Z.; Wang, K.; Zhu, C.; Chen, H.; Han, Y.C.; Song, Q.X.; Lao, L.F.; Zhang, Y.H.; et al. Comparison of Accuracy and Clinical Outcomes of Robot-Assisted Versus Fluoroscopy-Guided Pedicle Screw Placement in Posterior Cervical Surgery. Glob. Spine J. 2022, 12, 620–626. [Google Scholar] [CrossRef]
- Li, C.; Li, W.; Gao, S.; Cao, C.; Li, C.; He, L.; Ma, X.; Li, M. Comparison of accuracy and safety between robot-assisted and conventional fluoroscope assisted placement of pedicle screws in thoracolumbar spine: A meta-analysis. Medicine 2021, 100, e27282. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Wang, Z.; Li, D.; Tian, Y.; Yuan, S.; Wang, L.; Liu, X. Safety and accuracy of cannulated pedicle screw placement in scoliosis surgery: A comparison of robotic-navigation, O-arm-based navigation, and freehand techniques. Eur. Spine J. 2023, 32, 3094–3104. [Google Scholar] [CrossRef]
- Li, C.; Li, H.; Su, J.; Wang, Z.; Li, D.; Tian, Y.; Yuan, S.; Wang, L.; Liu, X. Comparison of the Accuracy of Pedicle Screw Placement Using a Fluoroscopy-Assisted Free-Hand Technique with Robotic-Assisted Navigation Using an O-Arm or 3D C-Arm in Scoliosis Surgery. Glob. Spine J. 2024, 14, 1337–1346. [Google Scholar] [CrossRef]
- Yu, J.; Zhang, Q.; Fan, M.X.; Han, X.G.; Liu, B.; Tian, W. Learning curves of robot-assisted pedicle screw fixations based on the cumulative sum test. World J. Clin. Cases 2021, 9, 10134–10142. [Google Scholar] [CrossRef] [PubMed]
- Torii, Y.; Ueno, J.; Iinuma, M.; Yoshida, A.; Niki, H.; Akazawa, T. The Learning Curve of Robotic-Assisted Pedicle Screw Placements Using the Cumulative Sum Analysis: A Study of the First 50 Cases at a Single Center. Spine Surg. Relat. Res. 2022, 6, 589–595. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).