1. Definition
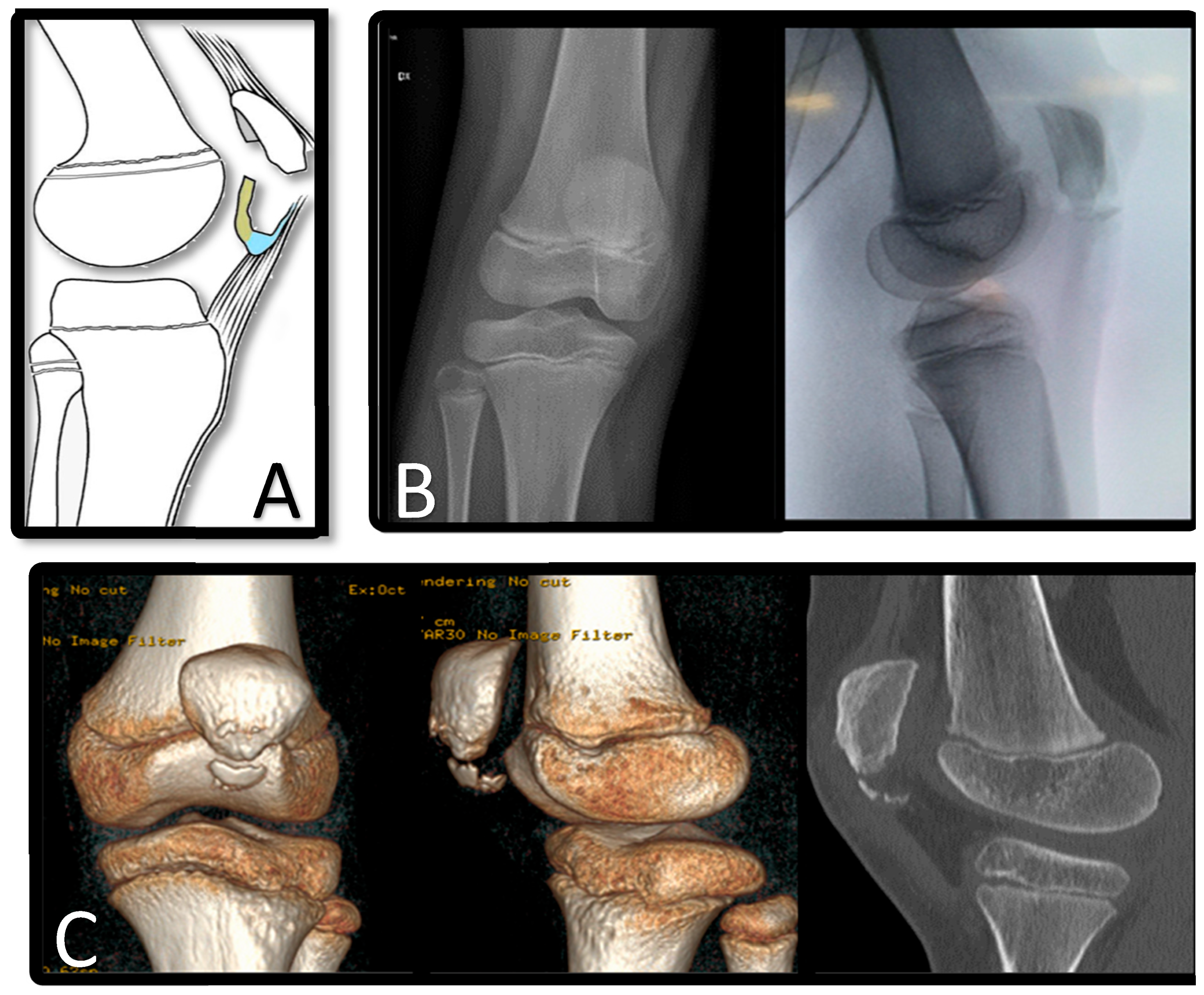
Patellar sleeve avulsion fractures are rare injuries seen in children between 8 and 12 years of age and are characterized by the separation of the cartilage “sleeve” from the ossified patella (
Figure 1).
2. Epidemiology
Although relatively uncommon, patellar sleeve fractures represent a significant subset of pediatric fractures, accounting for approximately 1% of all fractures in this population. Within the pediatric population, however, they represent a significant proportion, accounting for approximately 50% of all patellar fractures [
1].
The peak incidence of patellar sleeve fractures occurs around 12.7 years of age, with cases typically observed within a range spanning from 8 to 16 years. Notably, this injury has a higher prevalence in boys, with the male-to-female ratio ranging from 3:1 to 5:1 [
2].
Adolescents are particularly susceptible to patellar sleeve fractures, likely due to a combination of factors. Intense participation in sporting activities during this developmental period, coupled with rapid skeletal growth, may contribute to an increased risk. In addition, the ongoing process of osteochondral transformation at the periphery of the patella, along with relative patellar instability during growth spurts, may predispose individuals to such injuries [
3].
In children, sleeve fractures of the patella predominantly occur in the inferior pole, although occurrences in the superior pole are exceedingly rare [
4,
5,
6,
7]. Conversely, in adults, sleeve fractures involving the superior pole are exceptionally uncommon, with a higher predilection observed in males. This rarity in adults is attributed to the characteristics of the enthesis, which becomes more resistant to tensile force injuries as the patella fully ossifies [
8]. Therefore, while patellar sleeve fractures are relatively common in the pediatric population, they represent an extremely rare condition in adults due to the biomechanical properties of the fully ossified patella.
3. Etiopathogenesis
Patellar sleeve fractures typically result from distal or proximal avulsions, which can be thought of as bony tears of the quadriceps or patellar tendon. These avulsions occur due to a sudden contraction of the quadriceps muscle during knee flexion. The exact mechanism of this injury is thought to involve a large eccentric contraction of the quadriceps muscle while the knee is in flexion [
9].
This forceful contraction of the quadriceps results in the separation of the inferior pole of the immature patella from the rest of the patella. The fragile nature of the immature patella, with its developing ossification centers and cartilaginous structure, predisposes it to such injuries, especially during periods of rapid growth and increased physical activity.
Patella fractures are common in individuals who participate in activities that require explosive acceleration, such as jumping or sudden changes in direction, which are common in sports such as basketball, soccer, and volleyball. In addition, high-energy sports that place repetitive stress on the knee joint, such as running and gymnastics, may also contribute to the development of these fractures [
10].
The repetitive and forceful nature of these activities can place significant stress on the patellar tendon and its insertion point on the immature patella, leading to avulsion injuries. In addition, the biomechanical forces generated during these activities could exceed the tensile strength of the patellar tendon, resulting in the separation of the inferior pole of the patella.
While the exact etiology of patellar sleeve fractures may vary depending on individual circumstances and biomechanical factors, the common denominator is the excessive stress placed on the patellar tendon and its attachment to the developing patella. Understanding these mechanisms is crucial for both prevention and effective management of this injury.
4. Anatomy and Embryology
The patella is the largest sesamoid bone in the human body. Deep to the fascia lata and rectus femoris tendon, it attaches anteriorly to the quadriceps [
11]. The origin of the patellar tendon is on the inferior pole of the patella, passing on the articular cartilage on the deep side and becoming confluent with the periosteum of the patella anteriorly [
12].
By the ninth week of gestation, following the chondrification of the distal femur and proximal tibia, a continuous band of connective tissue forms. This band represents three structures: quadriceps tendon, patellar ligament, and patella. Patellar precursor cells form a hyaline cartilage mass that divides the band already formed, leaving a thin communication of the fibers anterior to the chondrified patella [
13,
14]. There are multiple small ossification centers in the middle of the patella, possibly as many as six, and ossification progresses peripherally with growth [
15]. This leaves a rim of soft, intense osseo-chondrous transformation all around the growing patella [
1]. The patella is completely cartilaginous by 14 weeks of gestation. Between 5 and 6 years of age, primary ossification of the patella occurs, but it can be evident on plain film radiographs as early as 2 to 3 years. Before ossification, the patella can be assessed with ultrasound [
16].
5. Biomechanics
The extensor mechanism of the knee consists of static and dynamic stabilizers that converge on the centrally located patella. The extensor mechanism of the knee acts as a lever arm, participating in both extension and flexion movements.
The knee is capable of maintaining an upright position and walking unassisted through the process of extension. The patella plays a role in the flexion and gliding movements of the knee and enhances the strength of the quadriceps in extension. It acts as a link between the proximal tibia and the quadriceps during flexion. Between 45 and 60 degrees of flexion, the patella must withstand the greatest amount of pressure. During flexion, the patella must withstand high forces to fulfill its function. In fact, it has been observed that the patella can withstand forces more than 3200 N, converting tensile forces into compressive forces during movement.
6. Classification
Patellar fractures have traditionally been classified using various systems, each with its own advantages and limitations. Grogan et al. [
17] provided a classification system in which they described 47 patella fractures and categorized them all as avulsion fractures. However, this classification did not specifically include sleeve fractures as a separate category. In addition, the AO-OTA classification system, which is commonly used for orthopedic fractures, does not adequately address the nuances of sleeve fractures [
18].
In recent years, there has been a growing recognition of the need for more nuanced classifications, particularly with regard to lower pole patella fractures. A notable advance in this regard is the proposed classification based on CT imaging, which provides a comprehensive approach to categorizing fractures of the lower pole of the patella. Although this classification system was not developed specifically for pediatric cases, it provides valuable insight into the diverse patterns of lower pole patellar fracture. The proposed classification system delineates five distinct types of lower pole patella fractures:
Type I: Simple inferior patellar fracture pattern (IPFP)—Characterized by a straightforward fracture pattern without comminution;
Type II: Comminuted IPFP—Involves fragmentation of the inferior patellar pole with multiple fracture fragments;
Type III: Simple IPFP with additional patellar body fracture—Subdivided into two subtypes:
- -
Type A: Transverse patellar fracture;
- -
Type B: Longitudinal patellar fracture.
Type IV: Comminuted patellar fracture involving the inferior pole—Represents a more severe form of comminution involving the entire patellar bone, particularly the inferior pole.
This classification system provides a comprehensive framework for understanding the diverse spectrum of lower pole patella fractures, allowing for more accurate diagnosis and tailored treatment strategies. However, further validation and refinement of this classification is warranted, particularly with regard to its applicability to pediatric populations and its potential to guide surgical management and prognosis [
19]. It would have been interesting if the classification also aimed to better understand the percentage of each type of fracture, but unfortunately, that was not the primary aim of the study, so certainly more research needs to be conducted.
7. Diagnosis
7.1. Clinical Presentation
Patellar sleeve fractures typically present with distinct clinical features, although the diagnosis can sometimes be difficult due to overlapping symptoms with other knee pathologies. Presentation often begins with a sudden onset of severe pain, often precipitated by explosive activities such as jumping rather than a fall. Patients commonly report pain and swelling in the affected knee, accompanied by difficulty raising the leg straight due to pain and mechanical obstruction.
A key clinical indicator of a suspected patellar sleeve fracture is the presence of a palpable gap at the inferior pole of the patella. This palpable gap indicates separation of the patellar sleeve from the ossified patella and may aid in diagnosis. In addition, assessment for patella alta may provide further diagnostic clues, as the affected patella may be palpated more proximally compared to the contralateral side.
However, diagnosing patellar sleeve fractures based on clinical examination alone can be challenging, especially when disruption is minimal or when alternative muscle groups compensate for the injury, resulting in preserved function. Therefore, clinicians must maintain a high index of suspicion and carefully consider the differential diagnosis. Recent studies have highlighted important differences in the clinical presentation of patellar sleeve fractures and other knee pathologies. Patellar sleeve fractures and inferior pole fractures are commonly associated with acute trauma, whereas Sinding–Larsen–Johansson (SLJS) disease typically presents with chronic overuse. Patients with patellar sleeve fractures often present with an inability to perform intact straight leg raises, distinguishing them from those with inferior pole fractures or SLJS. In addition, knee swelling and effusion are common in patellar sleeve fractures, further aiding in differentiation from other pathologies. Of note, patients with SLJS may still be able to bear weight, unlike those with patellar sleeve fractures, who often have significant functional limitations [
20].
7.2. Differential Diagnosis
To correctly differentiate between fractures and anatomical variants, the normal ossification sequence should be known. Children presenting with anterior knee pain may often have a bipartite patella or inferior patellar pole fragmentation. A bipartite patella should be considered when evaluating radiographs of the patella [
21]. Commonly due to an unfused superolateral ossification center or fragment, it is seen in 3% of adults and is symptomatic in <2% of cases [
16,
22]. It needs to be mentioned also the avascular osteonecrosis of the inferior patella pole, known as Sinding–Larsen–Johansson disease [
23], and the other inferior pole fractures [
18]. The inferior patellar pole may also have a fragmented pattern of ossification during the first decade of life in up to 25% of patients presenting with knee pain [
24]. It could be a normal variant or otherwise an avulsion injury [
7,
24].
Acute inferior patellar avulsion or sleeve injuries can often be distinguished from normal variation based on clinical presentation and the presence of incompletely corticated, sharply defined linear or curvilinear osteochondral fragments on radiographs [
10,
25,
26,
27], increased prepatellar swelling, patella alta with higher mean Insall Salvati (IS) ratio [
20].
8. Imaging
Imaging plays a crucial role in the diagnosis and management of patellar sleeve fractures, helping to accurately characterize the extent and nature of the injury. While plain radiographs are often the initial imaging modality used, they may not always reveal bony damage associated with patellar sleeve fractures. In addition, joint effusion, a common feature of these injuries, may not be visible on radiographs. However, lateral knee radiographs can provide valuable information by demonstrating swelling at the inferior pole of the patella, a characteristic finding in patellar sleeve fractures. Of particular importance is the identification of the patella alta, which serves as a key diagnostic clue on radiographs.
Ultrasound imaging provides a cost-effective alternative for the diagnosis of patellar sleeve fractures, especially in the absence of radiographically visible fracture fragments. Ultrasound can effectively detect the presence of a patellar sleeve avulsion, aiding in prompt diagnosis and appropriate management [
28].
Computed tomography (CT) imaging offers high sensitivity in the detection of inferior pole patellar fractures (IPFP), with studies reporting detection rates of up to 88%. Compared to radiographs, which only can identify 44% [
19]. CT imaging provides superior visualization of bony structures, facilitating accurate diagnosis and classification of patellar sleeve fractures.
Magnetic resonance imaging (MRI) is a valuable tool for further characterization of suspected patellar avulsion fractures, especially in pediatric patients. MRI can provide detailed information regarding the extent of the injury, including the presence of bone marrow edema-like signal characteristics at the inferior patellar pole and adjacent soft tissue edema. In addition, MRI can help identify loose bodies in the joint space that may contribute to mechanical symptoms such as locking. By providing a comprehensive view of the injury, MRI assists clinicians in formulating optimal management strategies for patellar sleeve fractures, ensuring appropriate treatment, and facilitating the early return to function [
16].
9. Treatment
9.1. Conservative Treatment
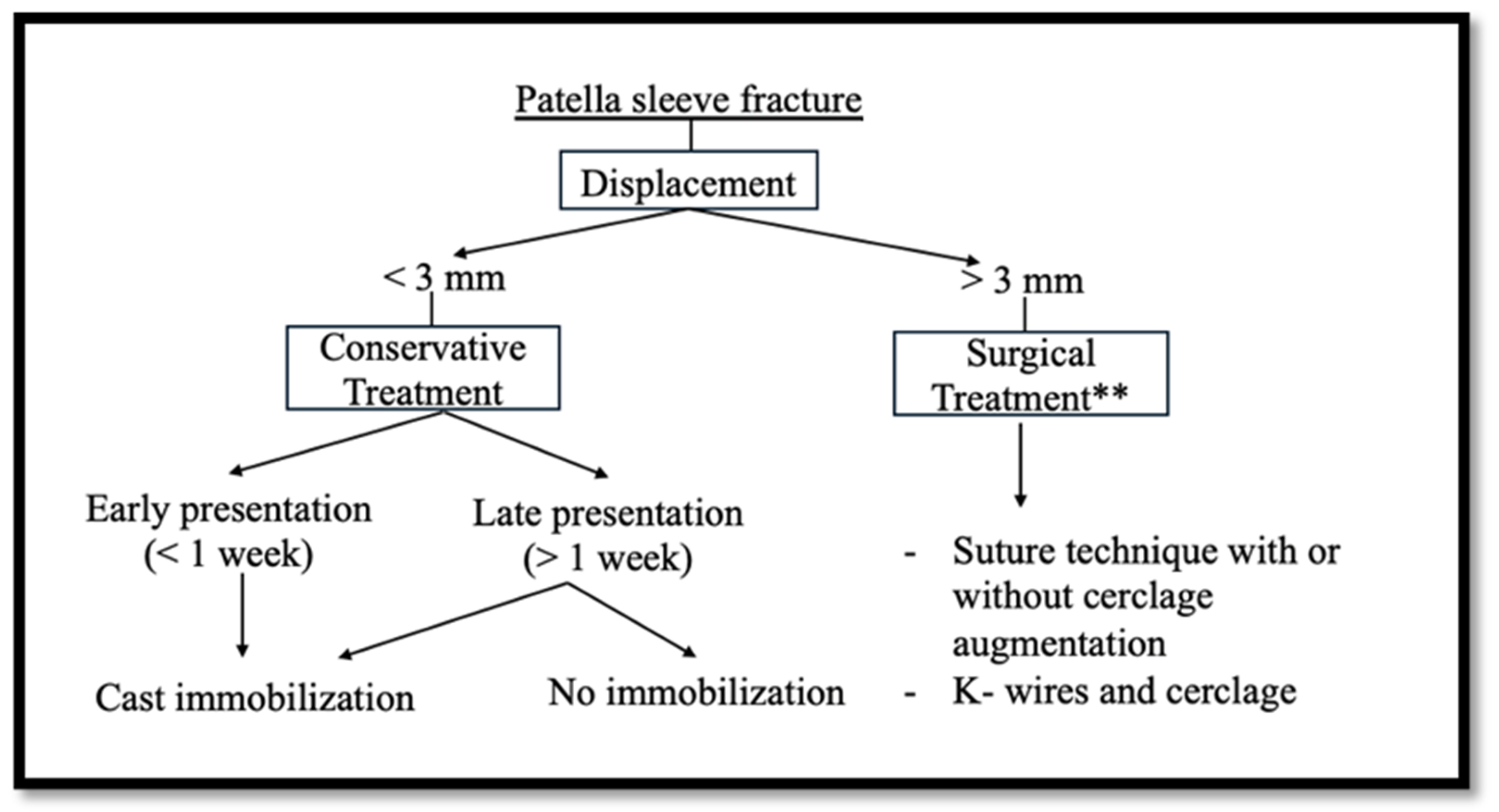
There is a lack of literature on the nonoperative management of these injuries, and few studies have focused on the management of minimally displaced fractures. It is believed that <2 or 3 mm is the limit to encourage conservative treatment.
Gao et al. [
27] reported on a case series of eleven patients with patellar sleeve fractures, six of whom were minimally displaced (<2 mm) and were treated with a femoro-podalic cast for 4 to 6 weeks. All patients achieved full knee extension and were pain-free at ten months. Unfortunately, it was not possible to understand the type of rehabilitation program and physical and medical protocol. No clinical outcome was reported also.
Sousa et al. [
29] reported a retrospective analysis of twenty patients treated for patellar sleeve fracture. Two of them had a displacement >4 mm, and the other 18 included in the study were categorized as minimally displaced (<3 mm). Five patients had advanced imaging, and they were studied as a reference group. Patients with acute presentation were treated with immobilization in a cast or knee brace for a minimum of 4 weeks. Patients with a delayed presentation (>1 week) were treated with activity modification and physical therapy and were not immobilized. Delayed presentation may place patients with non-displaced or minimally displaced fractures at higher risk for surgery. No patient had an extensor lag at the time of final follow-up. No patient reported limitations in sports activities (mean follow-up 7.8 years). The authors strongly believe that nonoperative treatment of minimally displaced patellar sleeve fractures (≤3 mm) results in excellent outcomes. It is of fundamental importance to diagnose the condition promptly. Delays in diagnosis and treatment may be associated with worse outcomes.
When a bony fragment is visible on radiographs and the displacement is less than 2 mm, closed reduction and casting in extension is plausible, but the results of conservative treatment are unsatisfactory [
30], leaving possible sequelae such as nonunion, heterotopic ossification, decreased range of motion of the knee, and delayed mobilization [
31]. Despite reports that nonoperative intervention, even in minimally displaced cases, may lead to chronic patella alta or patellar tendon ossification, Yellin et al. [
32] analyzed a group of 64 patients (71%) who underwent nonoperative treatment. None of these patients had patellar tendon ossification on final radiographs, and only one patient had patella alta. The results are summarized in
Table 1.
9.2. Surgical Treatment
Operative management is encouraged for all sleeve fractures with displacement >3 mm [
10].
Patellar fractures (PFs) have traditionally been treated with metallic tension-band fixation, a method associated with a significant complication rate. It is believed that non-metallic tension-band fixation may be a safe and effective alternative to traditional metallic tension-band fixation for patellar fractures in general [
32].
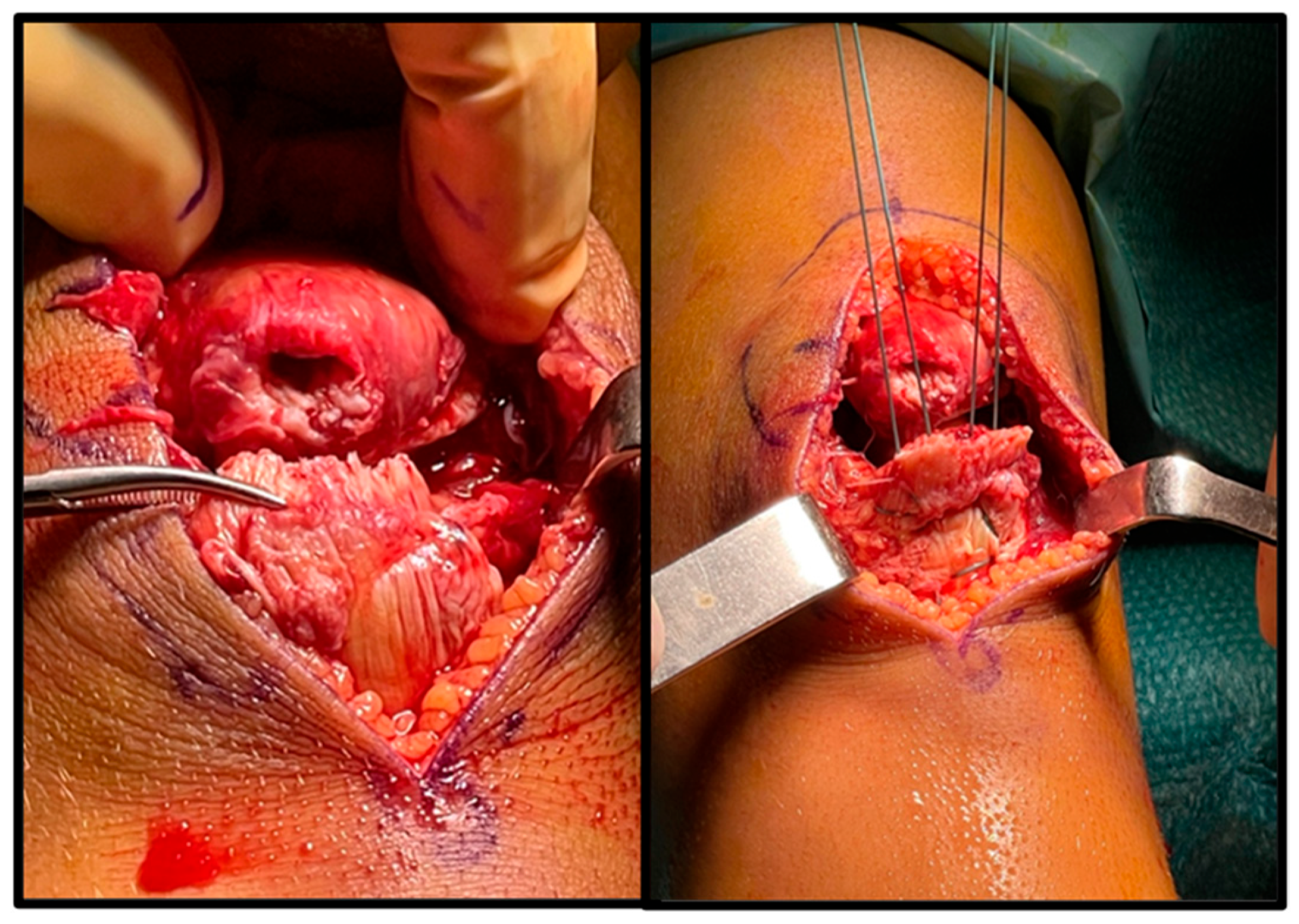
Large transosseous sutures are simple and efficient [
33,
34]. Intraosseous anchors or tension-band wire systems could be used [
34] (
Figure 2).
Various techniques have been described in the literature for the treatment of PF: hook plate, hammock plate technique, cerclage wire, and sutures with anchor or bone tunnel fixation technique. Different options have been presented; from literature analysis, to our knowledge, the plate technique has only been described in the adult population [
35,
36]. Although partial patellectomy was described, its indications and possible complications were not discussed.
Shea et al. [
37] compared the efficacy of three main methods of patellar fracture fixation (suture technique, hybrid fixation, and wire cerclage) in a cohort of patients aged 10 to 60 years. In terms of reoperation rates and complications associated with the treatments, they agreed that sutures alone were preferable to hybrid fixation for patella fractures involving the distal pole. Although the use of a supportive metal tension-band loop in addition to transosseous sutures may provide additional stability, this technique should be used with caution because of the increased incidence of soft tissue impingement and reoperation.
In general, various techniques using transosseous suture fixation keep patients in strict immobilization in extension for 4 to 6 weeks with varying weight-bearing restrictions [
38]. Hebbel et al. [
39] immobilized with a locked knee brace in full extension with weight-bearing restriction for 6 weeks. Physical therapy was started immediately with a full passive range of motion. After seven weeks, the patient began an active range of motion and partial weight bearing with 20 kg increments per week. Full strength and no limitation in sports activities were reported at 2-year follow-up. Tsubosaka et al. [
40] used a wiring cerclage of the soft tissues around the patella and the tendon. Immobilization in a cast for 4 weeks was suggested. At 9 months after surgery, there was no extension lag, and the active range of motion of the injured knee was 0–140° of flexion. The patient did not report any limitations in sports activities. Similar results were reported by Li et al. [
41], with a postoperative extension cast for four weeks followed by a hinger cast applied for four weeks with gradual weight bearing. K-wires and cerclage were removed at the ten-month follow-up. The patient’s outcome was excellent, with no complaints or symptoms of patellar instability and with normal muscle strength and a full range of motion in daily activities.
Perkins et al. [
35] considered in their studies the fact that preoperative immobilization may be a limitation. The duration of initial immobilization was found to be the only variable strongly associated with final postoperative ROM. Gaining full ROM (>130 degrees in flexion) was found to be faster in the group with less than 22 days of postoperative immobilization.
Meiming Xie et al. [
42] described the results of their experience with multidirectional three-dimensional steel wire ring sleeve fixation, pointing out the advantages of reliable fixation, early functional recovery, and fewer complications of the technique. However, the technique was described in a population aged 20 years and older. Intermittent ice application on the first day after surgery was suggested, followed by active knee and ankle training and straight leg elevation. Four weeks after the surgery, the weight-bearing part of the ground walking was suggested to avoid accidental falls. The follow-up period for the inferior pole patella fracture was from 15 months to 5 years.
Shimasaki et al. [
43] recently described their experience with the pull-out technique with transosseous sutures. Krackow sutures were used with a continuous locking loop technique for tendon repair. A 10° flexion brace was applied after surgery. Physical therapy was started gradually, allowing full weight bearing depending on his pain. Radiographically, there was no difference from the contralateral side at the 10-month follow-up. Clinically, the patient was able to resume full range of motion with no extension lag. Nowel et al. described their technique using intraosseous suture anchors with suture cerclage augmentation. They added a suture cerclage technique to resist dislocation forces and allow early mobilization. The authors’ protocol was an immediate range of motion and weight bearing, allowing for a faster rehabilitation program [
44]. Range of motion from 0 to 30° in the brace is allowed for the first 2 weeks and then sequentially increased by 30° every 2 weeks. The brace is removed after 6 weeks. Follow-up results were not described.
A similar all-suture technique was described by Bhumiwat et al. [
45]. Internal fixation was performed using a transosseous suture technique with two Krackow sutures on the patellar tendon, and then the sutures were passed back proximally to the fracture site. Finally, a cerclage augmentation was performed. In this case, the author immobilized the knee with a knee brace in 0° of flexion for the first 2 weeks and in 90° of flexion for 2–4 weeks postoperatively. Passive ROM exercise was started as soon as tolerated by the patient. The patient was able to walk with crutches (protected weight bearing) for the first 2 weeks and then with full weight bearing after 2 weeks. The authors believe that the strong fixation technique allows for early ROM and weight bearing postoperatively. No follow-up data were presented. Due to its small size, irregular geometry, and minimal operative space, the inferior pole fracture of the patella is challenging to treat in the adult population, and no single surgical method can consistently produce positive results. Liu et al. [
19], in their review, attempted to provide a complete overview of the different treatment options and the appropriateness of each in the treatment of adult patellar fractures. In patellar sleeve fractures, the lack of literature could be a challenge in the intent to provide a precise, appropriate surgical treatment for each fracture type. Most authors often do not only consider the treatment in the pediatric population but also generalize the treatment results. Therefore, it is not possible to evaluate in the same studies which specific treatment suggestions were adopted in the pediatric population and which were adopted in the adult population.
In children, due to the lack of literature and the limited cohorts, it could be challenging to represent the best option for each type of fracture. Therefore, we have tried to summarize all the surgical options presented in the literature related specifically to a pediatric population, evaluating all the complications, the postoperative protocol, and the return to sports activities. The results are shown in
Table 2.
In order to facilitate the decision-making process in the treatment of patellar sleeve fractures, we have attempted to propose a treatment flowchart. It should be noted that there is a paucity of literature analyzing the treatments with their outcomes, and it could be challenging (
Figure 3).
Considering the pediatric population, we believe that the exposed suture technique could be a good option. In fact, they have a low percentage of complications, no need for reintervention for hardware removal, and good outcomes at long-term follow-up. The majority of authors consider a postoperative immobilization of 4–6 weeks. On the contrary, Perkins suggests reducing the immobilization period to 21 days. This could be a valid option, but a larger sample could be evaluated. So far, we believe that 4 weeks could be a good alternative.
10. Complications
The blood supply of the young patella is derived from the anterior surface of the distal pole, with minimal contribution from the medial margins. Injury to the anterior and distal poles can result in avascular necrosis of the proximal pole [
46].
Wound infection, ischemic necrosis of the patella, limited flexion, and ectopic ossifications have also been described [
47]. Nonunion degenerative hypertrophic changes have also been described [
48].
Malalignment, quadriceps atrophy, heterotopic ossification, and extensor lag have been reported in significantly displaced fractures treated nonoperatively [
47]. A recent retrospective study selected a cohort of 38 patients with 16 years of activity. Despite various rehabilitation programs, the operative management was to restore the extensor mechanism. In their experience, only 8% of patients had complications requiring unplanned surgery [
48].
11. Rehabilitation
The treatment of patients involves the selection of different techniques according to their specific needs in order to facilitate the return to optimal function and sports activities.
The use of physical therapy has been the subject of considerable debate, and a number of different physical therapy techniques have been proposed. Some authors argue that immobilization and prevention of knee flexion for a period of three to six weeks postoperatively is necessary, while others argue that this is an unnecessary limitation [
49].
The goal of physical therapy is to prevent and restore motion and strength. It is critical to the healing process to maintain strength through a combination of isometric, isotonic, and isokinetic exercises. This will increase flexibility and strength, reduce discomfort, and increase the range of motion in the lower leg [
50,
51].
The rehabilitation program should restore full ROM and function and reduce pain. Initially, ROM exercises may include passive ROM, isometric contraction of the quadriceps, and heel side. Manual and active stretching of the lower leg muscles may be useful [
52].
12. Conclusions
Patellar sleeve fractures, although rare in children, pose significant challenges both in terms of treatment and return to sports activity. The paucity of literature on this topic may be due to the low percentage of cases encountered. In our institution, only two cases of patellar sleeve fractures have been encountered, which underscores the rarity of this injury. It is imperative that physicians be familiar with this condition and be able to make an accurate diagnosis.
Several surgical options have been shown to reduce immobilization time and speed rehabilitation. Evidence suggests that minimizing immobilization may play a critical role in achieving early and complete recovery of range of motion. However, further research is warranted to comprehensively evaluate the benefits and limitations of different surgical techniques.
Future studies should focus on refining diagnostic algorithms, optimizing surgical interventions, and standardizing rehabilitation protocols to improve patient outcomes and facilitate a rapid return to pre-injury activity levels. Collaborative efforts within the medical community are essential to expand the body of knowledge regarding patellar sleeve fractures and improve the management of this challenging orthopedic condition.
Author Contributions
Conceptualization, G.P.; methodology, F.M.C.P.; software, R.O.; validation, G.C.S.; formal analysis, C.P.; investigation, M.G.; resources, F.C.; data curation, S.C.; writing—original draft preparation, G.P.; writing—review and editing, M.G.; visualization, K.S.; supervision, G.L.; project administration, G.P.; funding acquisition, A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to its retrospective nature.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in the text and tables.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hunt, D.M.; Somashekar, N. A review of sleeve fractures of the patella in children. Knee 2005, 12, 3–7. [Google Scholar] [CrossRef]
- Georgiadis, A.G.; Comadoll, S.M. Patellar sleeve fracture: Open reduction and internal fixation. J. Pediatr. Orthop. Soc. N. Am. 2021, 3, 367. [Google Scholar] [CrossRef]
- Ray, J.M.; Hendrix, J. Incidence, mechanism of injury, and treatment of fractures of the patella in children. J. Trauma 1992, 32, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Ro, K.-H.; Park, J.-H.; Kim, M.-J.; Lee, D.-H. Rare sleeve fracture of the superior patella pole in an adult due to forceful passive physiotherapy following cast immobilization. Knee 2014, 21, 600–604. [Google Scholar] [CrossRef]
- Teixeira, P.; Lecocq, S.; Moisei, A.; Chanson, A.; Louis, M.; Blum, A. Sleeve-like avulsion fracture of the superior pole of the patella in a healthy adult. Diagn. Interv. Imaging 2013, 94, 108–111. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kakazu, T.; Tatemoto, H.; Kawamura, M.; Sugita, T. Sleeve fracture of the upper pole of the patella in an adult with osteogenesis imperfecta. Injury 2003, 34, 793–794. [Google Scholar] [CrossRef]
- Xie, L.; Xu, H.; Zhang, L.; Xu, R.; Guo, Y. Sleeve fracture of the adult patella: Case report and review of the literature. Medicine 2017, 96, e7096. [Google Scholar] [CrossRef]
- Gettys, F.K.; Morgan, R.J.; Fleischli, J.E. Superior pole sleeve fracture of the patella: A case report and review of the literature. Am. J. Sports Med. 2010, 38, 2331–2336. [Google Scholar] [CrossRef]
- Schmal, H.; Strohm, P.C.; Niemeyer, P.; Reising, K.; Kuminack, K.; Sudkamp, N.P. Fractures of the patella in children and adolescents. Acta Orthop. Belg. 2010, 76, 644–650. [Google Scholar]
- Houghton, G.; Ackroyd, C. Sleeve fractures of the patella in children. J. Bone Jt. Surgery. Br. Vol. 1979, 61, 165–168. [Google Scholar] [CrossRef]
- Cox, C.F.; Sinkler, M.A.; Black, A.C.; Launico, M.V.; Hubbard, J.B. Anatomy, Bony Pelvis and Lower Limb, Knee Patella; Stat Pearls: Treasure Island, FL, USA, 2023; Bookshelf, ID: NBK519534. [Google Scholar]
- Hsu, H.; Siwiec, R.M. Patellar Tendon Rupture; StatPearls: Treasure Island, FL, USA, 2023; Bookshelf, ID: NBK513275. [Google Scholar]
- Mérida-Velasco, J.A.; Sánchez-Montesinos, I.; Espín-Ferra, J.; Mérida-Velasco, J.R.; Rodríguez-Vázquez, J.F.; Jiménez-Collado, J. Develomment of the human knee joint ligaments. Anat. Rec. 1997, 248, 259–268. [Google Scholar] [CrossRef]
- Gardner, E.; O’Rahilly, R. The early development of the knee joint in staged human embryos. J. Anat. 1968, 102, 289–299. [Google Scholar] [PubMed] [PubMed Central]
- Sponseller, P.; Stanitsk, C. Fractures in Children; Lippincott, Williams and Wilkins: Philadelphia, PA, USA, 2001; p. 1029. [Google Scholar]
- Maloney, E.; Stanescu, A.L.; Ngo, A.-V.; Parisi, M.T.; Iyer, R.S. The Pediatric Patella: Normal Development, Anatomical Variants and Malformations, Stability, Imaging, and Injury Patterns. Semin. Musculoskelet. Radiol. 2018, 22, 081–094. [Google Scholar] [CrossRef]
- Grogan, D.P.; Carey, T.P.; Leffers, D.; Ogden, J.A. Avulsion fractures of the patella. J. Pediatr. Orthop. 1990, 10, 721–730. [Google Scholar] [CrossRef]
- Gwinner, S.C.; Märdian Schwabe, P.; Schaser, K.D.; Krapohl, B.D.; Jung, T.M. Current Concepts Review: Fractures of the Patella; GMS Interdisciplinary Plastic and Reconstructive Surgery DGPW: Bergen, Germany, 2016. [Google Scholar] [CrossRef]
- Liu, C.-D.; Hu, S.-J.; Chang, S.-M.; Du, S.-C.; Chu, Y.-Q. Morphological characteristics and a new classification system of the inferior pole fracture of the patella: A computer-tomography–based study. Injury 2024, 55, 111256. [Google Scholar] [CrossRef] [PubMed]
- Devana, S.K.; Trivellas, A.; Bennett, A.; Jackson, N.; Beck, J.J. Clinical and Radiographic Differentiation of Pediatric Patellar Sleeve Fractures and Other Inferior Pole Pathologies. Am. J. Sports Med. 2022, 50, 977–983. [Google Scholar] [CrossRef]
- Soini, V.; Raitio, A.; Virkki, E.; Syvänen, J. Treatment of congenital bipartite patella in pediatric population—A systematic review of the published studies. Acta Orthop. Belg. 2022, 88, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Koshino, T.; Oohashi, Y. Clinical features and classification of bipartite or tripartite patella. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1465–1469. [Google Scholar] [CrossRef]
- Negrão, E.; van den Eede, E.; Kyriazopoulos, A.; Romijn, M.G. Sinding–Larsen–Johansson syndrome with minimally displaced patellar sleeve avulsion fracture: A case report with multimodality approach and literature review. Skelet. Radiol. 2023, 52, 1403–1407. [Google Scholar] [CrossRef]
- Kan, J.H.; Vogelius, E.S.; Orth, R.C.; Guillerman, R.P.; Jadhav, S.P. Inferior patellar pole fragmentation in children: Just a normal variant? Pediatr. Radiol. 2014, 45, 882–887. [Google Scholar] [CrossRef]
- Keats, T.E. Atlas of Normal Roentgen Variants That May Simulate Disease, 5th ed.; Mosby Yearbook: St. Louis, MO, USA, 1992. [Google Scholar] [CrossRef]
- Ogden, J.A. Radiology of postnatal skeletal development. X. Patella and tibial tuberosity. Skelet. Radiol. 1984, 11, 246–257. [Google Scholar] [CrossRef]
- Gao, G.; Mahadev, A.; Lee, E. Sleeve fracture of the patella in children. J. Orthop. Surg. 2008, 16, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Ditchfield, A.; Sampson, M.; Taylor, G. Case reports. Ultrasound diagnosis of sleeve fractures of the patella. Clin. Radiol. 2000, 55, 721–722. [Google Scholar] [CrossRef] [PubMed]
- Sousa, P.L.; Stuart, M.J.; Prince, M.R.; Dahm, D.L. Nonoperative Management of Minimally Displaced Patellar Sleeve Fractures. J. Knee Surg. 2020, 34, 242–246. [Google Scholar] [CrossRef]
- Ishikawa, H.; Sakurai, A.; Hirata, S.; Ohno, O.; Kita, K.; Sato, T.; Kashiwagi, D. Painful bipartite patella in young athletes: The diagnostic value of skyline views taken in the squatting position and the results of surgical excision. Clin. Orthop. Relat. Res. 1994, 305, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Ansari, S.; Barman, S.; Raja, B.S.; Kurmi, A.C.; Yadav, R.; Bansal, S.; Regmi, A.; Singh, V. Pediatric Patella fractures—A Systematic review. J. Orthop. 2023, 49, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Yellin, J.L.; Feroe, A.G.; Watkins, I.T.; Franco, H.; Guevel, B.; Haber, D.B.; Kocher, M.S. Management and subsequent outcomes of patellar sleeve injuries: A retrospective case series of 90 pediatric and adolescent patients. J. Child. Orthop. 2024, 18, 208–215. [Google Scholar] [CrossRef]
- Giuseppe, R.; Michele, R.; Luca, F.; Michele, G.; Giuseppe, G.; Valentina, M.; Giustra, F.; Bosco, F.; Camarda, L. Nonmetallic tension band fixation is a viable and low-complication surgical technique in patellar fractures: A five-year retrospective study. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 2065–2071. [Google Scholar] [CrossRef]
- Kaar, T.K.; Murray, P.; Cashman, W.F. Transosseous suturing for sleeve fracture of the patella: A Case report. Ir. J. Med. Sci. 1993, 162, 148–149. [Google Scholar] [CrossRef]
- Perkins, C.A.; Egger, A.C.; Willimon, S.C. Transosseous Repair of Patellar Sleeve Fractures: A Case Series and Surgical Technique Guide. J. Knee Surg. 2022, 35, 1326–1332. [Google Scholar] [CrossRef]
- Springorum, H.-P.; Siewe, J.; Dargel, J.; Schiffer, G.; Michael, J.; Eysel, P. Einteilung und Therapie der Patellafraktur [Classification and treatment of patella fractures]. Orthopade 2011, 40, 877–884. [Google Scholar] [CrossRef]
- Shea, G.K.-H.; So, K.H.-T.; Tam, K.-W.; Yee, D.K.-H.; Fang, C.; Leung, F. Comparing 3 Different Techniques of Patella Fracture Fixation and Their Complications. Geriatr. Orthop. Surg. Rehabil. 2019, 10, 2151459319827143. [Google Scholar] [CrossRef]
- Jang, J.H.; Cho, Y.J.; Choi, Y.Y.; Rhee, S.J. Hammock plating for comminuted inferior sleeve avulsion fractures of the patella: A surgical technique and clinical results. Orthop. Traumatol. Surg. Res. 2021, 107, 102866. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Hebbel, A.; Eggers, F.; Schütte, V.; Achtnich, A.; Imhoff, A.B. Patellar sleeve avulsion fracture in a patient with Sinding-Larsen-Johansson syndrome: A case report. BMC Musculoskelet. Disord. 2020, 21, 267. [Google Scholar] [CrossRef] [PubMed]
- Tsubosaka, M.; Makino, T.; Kishimoto, S.I.; Yamaura, K. A case report of sleeve fracture of the patella in a shield. J. Orthop. Case Rep. 2016, 6, 24–27. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Xiang, M.; Lv, X.; Gan, Y.; Yu, S. Bilateral sleeve fracture of the inferior pole of the patella in children: A case report. Front. Surg. 2022, 9, 970802. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Liao, D.; Gong, K.; Huang, C.; Chen, S.; Ren, Y.; Zheng, W. Effectiveness of multidirectionally three-dimensional steel wire ring sleeve fixation in treatment of inferior patellar pole avulsion fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2021, 35, 183–187. [Google Scholar] [CrossRef]
- Shimasaki, K.; Uesugi, M.; Kobayashi, T.; Tanaka, H.; Ichimura, H. Inferior Pole Sleeve Fracture of the Patella in an Adolescent: A Case Report. Cureus 2023, 15, e33494. [Google Scholar] [CrossRef]
- Nowell, J.A.; Niu, E.L. Patellar Sleeve Avulsion Fracture Repair: Suture Anchor Technique with Suture Cerclage Augmentation. Arthrosc. Tech. 2023, 12, e2197–e2202. [Google Scholar] [CrossRef]
- Bhumiwat, P.; Fossum, B.W.; Hazra, R.-O.D.; Ganokroj, P. Treatment of Unfixable Inferior Pole Fractures of the Patella Using an All-Suture Internal Fixation Technique. Clin. Orthop. Surg. 2024, 16, 168–172. [Google Scholar] [CrossRef]
- Lin, S.-Y.; Lin, W.-C.; Wang, J.-W. Inferior sleeve fracture of the patella. J. Chin. Med. Assoc. 2011, 74, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.Y.; Zhang, W.M. Fractures of the patella in children. Knee Surg. Sports Traumatol. Arthrosc. 1999, 7, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Desai, V.M.B.; DeFrancesco, C.J.; Yellin, J.L.; Nguyen, J.C.; Williams, B.A. Patient Characteristics and Postoperative Outcomes of Surgically Treated Inferior Pole Patellar Sleeve Fractures. J. Pediatr. Orthop. 2024, 44, 483–488. [Google Scholar] [CrossRef]
- Harna, B.; Gupta, P.; Singh, J.; Rousa, S.; Gupta, A. Surgical management of non-union patella fracture: A case series and review of the literature. Arch. Bone Jt. Surg. 2021, 9, 554–558. [Google Scholar] [CrossRef]
- Mirapurkar, T.S.; Boob, M.A.; Bhoge, S.S.; Phansopkar, P. A Comprehensive Physiotherapeutic Rehabilitation Protocol for Malunited Post-operative Patellar Fractures: A Case Report. Cureus 2023, 15, e51252. [Google Scholar] [CrossRef]
- Coco, M.; Ramaci, T.; Sagone, E.; Sardo, M.G.; Brachina, P.; Buscemi, B.; Coco, L.S.G.; Papotto, G.; Papotto, G.M.F.; Di Gregorio, G.; et al. Brain and memory: A pilot study on the experience of rebirth and the present life quality of adult subjects. Acta Medica Mediterr. 2017, 33, 901–904. [Google Scholar] [CrossRef]
- Henry, P.; Panwitz, B.; Wilson, J.K. Rehabilitation of a Post-surgical Patella Fracture: A Case report. Physiotherapy 2000, 86, 139–142. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).