Abstract
Ostomy formation is a vital component in the treatment of advanced gastrointestinal diseases, including colorectal cancer and inflammatory bowel disease. It usually involves externalizing a part of the colon or small bowel to the skin surface. Thus, the creation of an ostomy can often have a major negative impact on quality of life. This study aimed to evaluate whether the use of an ostomy belt could improve quality of life measures in stoma patients through a prospective interventional open-label study of 17–80-year-old English- and Spanish-speaking patients with stomas who were using an ostomy belt for 8 weeks. Changes in quality of life were assessed using the Stoma Quality of Life Scale questionnaire at baseline, at 4 weeks, and at 8 weeks post ostomy belt use. A total of 45 patients enrolled (20 female, mean age 48) in the study. The ostomy belt significantly improved quality of life scores from baseline to 4 weeks regarding overall life satisfaction (F(2, 76) = 14.77, p < 0.001) and in the domains of work/social function (F(2, 72) = 30.32, p < 0.001), sexuality/body image (F(2, 68) = 3.34, p = 0.04), and stoma function (F(2, 72) = 8.72, p < 0.001). These improvements were sustained at the 8-week follow-up. No significant differences were observed in the domains of financial impact and skin irritation. This study represents the first prospective interventional study that provides evidence for the simple low-cost intervention of ostomy support belt use in improving quality of life in patients with a stoma.
1. Introduction
Ostomy formation is a vital component in the treatment of advanced gastrointestinal diseases, including colorectal cancer and inflammatory bowel disease (IBD), among others. This typically involves externalizing part of the colon or small bowel to the skin surface [1]. Stoma management includes using a pouch to collect stool with the objective of avoiding leakage to maintain peristomal skin integrity [2]. The literature shows that stoma formation negatively affects patients’ physical, psychological, social, and sexual health when compared to the general population [3,4,5,6,7,8]. Specifically, psychosocial challenges such as feeling a loss of control over body function, physical aspects that affect quality of life (QOL), and acceptance and adaptation to living with a stoma are common [9]. Additionally, problems with pouch leakage are common and negatively affect QOL both psychologically and physically through the limitation of activities [10,11,12,13,14,15,16,17].
QOL in ostomy patients has been linked to factors such as duration of stoma implantation, education, gender, and concurrent chronic disease [13,14]. The prior literature has reported that interventions such as preoperative skin site marking, stoma care education, and involvement of certified ostomy nursing support can help QOL in stoma patients [10,11,12]. However, there are very few interventions that have been studied over time in stoma patients. Ostomy support belts provide a potential solution to issues that affect QOL. The goal of ostomy support belts is to prevent the appliance from shifting around, disconnecting from the flange, or falling off accidentally, and to help promote self-confidence when returning to daily activities after surgery. Anecdotally, stoma belts have been reported by patients to improve confidence and the ability to participate in desired activities. However, to our knowledge, no formal prospective interventional studies exist on the influence of stoma belt use and changes in QOL in those with an ostomy.
To close this gap, we conducted a prospective cohort study of QOL in stoma patients who were provided with an ostomy support belt to use over an 8-week intervention period. Changes in QOL during the study were measured using a stoma-specific QOL questionnaire. We hypothesized that stoma belts would increase QOL over an 8-week period.
2. Materials and Methods
2.1. Study Population
This was a prospective interventional IRB-approved open-label study of 45 patients with stomas who were provided with an ostomy belt (Stealth belt®, Johnson City, TN, USA) to use during the study. Participants over 18 years old with a stoma who were willing and able to use an ostomy belt were identified from the University of Miami (UMH) stoma patient clinic in the years 2021–2023. Study recruitment was limited to English- and Spanish-speaking patients, as QOL surveys were available in these languages. Patients without a stoma, those unwilling to wear an ostomy belt, or who did not speak English or Spanish fluently were excluded. Additionally, patients with a condition that, in the opinion of the investigator, would compromise the well-being of the patient or the study or prevent the patient from meeting or performing study requirements were excluded. This study was approved by the University of Miami. Patients signed a written consent form. This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of University of Miami (protocol code 20201333 20 January 2021).
Consenting volunteers with stomas were provided with an ostomy belt (Stealth belt brand) to use during the study (Figure 1 and Figure 2). Ostomy belts were provided free of cost to the patient. The goal of ostomy support belts is to prevent the appliance from shifting around, disconnecting from the flange, or falling off accidentally, and to help promote self-confidence when returning to daily activities after surgery. The ostomy belt is positioned either horizontally or vertically depending on style. The appliance is then inserted through the flange hole in the belt and Velcro is attached with adjustment for a comfortable fit. The zipper is then closed on the bottom of the belt, enclosing the appliance in the pouch of the belt. Patients were instructed to wear the belt for the 2-month study duration and were instructed that the belt can be worn comfortably 24 h a day through daily activities including sleep, sport, and intimacy.

Figure 1.
Stealth Belt Pro Horizontal ostomy support belt.

Figure 2.
Stealth Belt Pro Vertical ostomy support belt.
2.2. Measures
A baseline demographic survey was administered, and QOL was assessed using the Stoma Quality of Life Scale questionnaire (SQOLS) at baseline and at 4 weeks and 8 weeks post ostomy belt use. Data collected in the demographic survey included age, gender, language, educational level, waist circumference, BMI, ostomy type, reason for ostomy, and time from surgery. The SQOLS is a 21-item questionnaire that measures QOL in several domains: overall satisfaction (2 items), work/social function (6 items), sexuality/body image (5 items), stoma function (6 items), financial impact (1 item), and skin irritation (1 item). Nineteen (19) items are scored using a Likert-type, 5-point scale (1 = never, 2 = seldom, 3 = occasionally, 4 = frequently, 5 = always), and 2 items measure overall life satisfaction from 0 to 100. Each domain of QOL on the SQOLS ranges from 0 to 100 (0 is the worst, and 100 indicates the best QOL) for each item. Scores were calculated according to formulas detailed by Baxter et al. [18]. The SQOL questionnaire demonstrates good convergent validity with the 12-Item Short Form Health Survey when measuring QOL and is a commonly used instrument in patients with a stoma [18,19,20,21]. SQOLS was scored from 0 to 100 in overall satisfaction in life with a higher score indicating higher satisfaction.
2.3. Statistical Analysis
The analyses included all participants from whom baseline and 4- and 8-week follow-up surveys were available. Group differences in demographic characteristics and medical factors were assessed with chi-square tests and 1-way analyses of variance. Data were examined for skewness and kurtosis. An analysis of variance was used to assess differences in QOL domain scores (work/social function, sexuality/body image, stoma function, financial impact, and skin irritation) over the three time points (baseline, 4 weeks, 8 weeks). We conducted additional subgroup analyses for patients based on ostomy permanence (temporary versus permanent ostomy) as well as ostomy type (ileostomy versus colostomy). These additional analyses were conducted, as these factors may affect QOL survey scoring between patients. A minimum sample size of 34 patients was determined for this study, using a statistical power of 80% and an alpha level of 5%. Data were analyzed using the Statistical Package for the Social Sciences (SPSS)-version 28 (IBM SPSS Inc.; IBM Corporation, Armonk, NY, USA).
3. Results
3.1. Patient Characteristics
Of the 50 patients recruited, 45 patients completed the demographic survey (Table 1). The study population was characterized by a mean age of 48 years with a standard deviation (SD) of 10 years. Of the participants, 40.0% (n = 20) were female, 50.0% (n = 25) were male, and there were 10.0% (n = 5) with missing gender data. The majority spoke English (90.0%, n = 45) while 10.0% (n = 5) reported speaking Spanish. When considering educational attainment, the largest group had completed their undergraduate studies (44.0%, n = 22), followed by those who had completed high school (28.0%, n = 14). Smaller proportions had a master’s degree (8.0%, n = 4), a Doctorate (6.0%, n = 3), or had only completed some high school (4.0%, n = 2). There were 10.0% (n = 5) of participants with missing education data. The mean waist circumference was 38 inches (SD = 5), and the mean body mass index (BMI) was 25 (SD = 5). In terms of ostomy type, 42.0% (n = 21) had a colostomy, 48.0% (n = 24) had an ileostomy, with 10.0% (n = 5) missing this information. The majority of patients (n = 28) had temporary ostomies as opposed to permanent (n = 12), with 20.0% (n = 10) missing this information. For underlying illnesses, 50.0% (n = 22) had colorectal or other gastrointestinal (GI) malignancies, 25.0% (n = 11) had inflammatory bowel disease, 20.5% (n = 9) had non-GI malignancies, and 4.5% (n = 2) had other types of illnesses, which included hidradenitis and unspecified condyloma. Regarding the time elapsed since surgery, 33.3% (n = 15) had their operation less than 1 month ago, 46.7% (n = 21) underwent surgery 1–3 months prior, and 20.0% (n = 9) had their surgery more than 3 months ago.

Table 1.
Patient characteristics.
3.2. Ostomy Belt Survey Results over Time
Overall, 37 patients completed the pre-belt survey, 4-week survey, and 8-week survey and were included in the repeated measures ANOVA analysis. Mean scores for QOL measures at each time point can be visualized in Table 2 and Figure 3. On repeated measures ANOVA, a significant increase in QOL scores was seen between the time points on overall life satisfaction (F(2, 76) = 14.77, p < 0.001) and in the domains of work/social function (F(2, 72) = 30.32, p < 0.001), sexuality/body image (F(2, 68) = 3.34, p = 0.04), and stoma function (F(2, 72) = 8.72, p < 0.001). No significant differences between time points were observed in the domains of financial impact (F (2, 72) = 0.52, p = 0.60) and skin irritation (F(2, 74) = 2.37, p = 0.10). Mauchly’s Test of Sphericity indicated that the assumption of sphericity had not been violated for any of the measures.

Table 2.
Mean Stoma Quality of Life Scale questionnaire (SQOLS) scores at baseline, 4 weeks, and 8 weeks post ostomy support belt use.
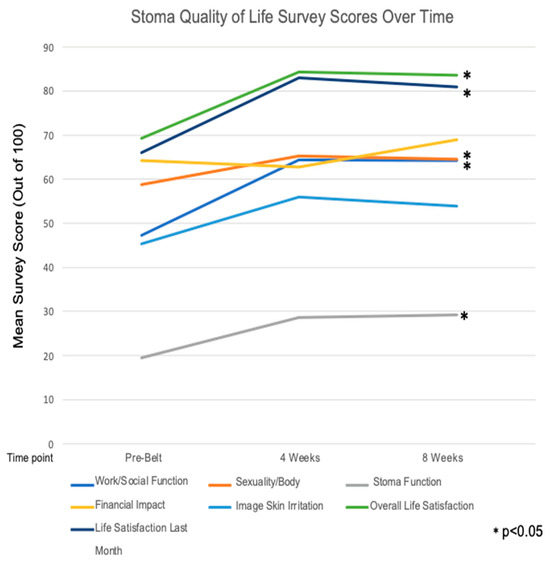
Figure 3.
Stoma Quality of Life Mean Survey Scores over time. * p-values reflect the between-group differences over all three time points, as noted in Table 2.
Post hoc pairwise comparisons with least significant difference adjustment indicated that from pre-belt to 4 weeks post belt and pre-belt to 8 weeks post belt, scores were significantly higher for the work/social function domain (pre-belt to 4 weeks, p < 0.001; pre-belt to 8 weeks, p < 0.001), stoma function (pre-belt to 4 weeks, p = 0.001; pre-belt to 8 weeks, p = 0.002), life satisfaction over the last month (pre-belt to 4 weeks, p < 0.001; pre-belt to 8 weeks, p = 0.004), and life satisfaction overall (pre-belt to 4 weeks, p < 0.001; pre-belt to 8 weeks, p < 0.001). On the sexuality and body image domain, there was a significant increase in scores from pre-belt to 4 weeks (p = 0.03), but the scores were not significantly different from pre-belt to 8 weeks (p = 0.084). The 4-week to 8-week scores were not significantly different for the domains of work/social function (4-week to 8-week scores: p= 0.917), sexuality and body image (p = 0.727), stoma function (p = 0.768), life satisfaction in the last month (4-week to 8-week scores: p= 0.485), or life satisfaction overall (4-week to 8-week scores: p= 0.744). Although the financial and skin irritation domain scores were not significantly different over time, the pre-belt to 4-week skin irritation score did increase and was trending towards significant (p = 0.062).
3.3. Subgroup Analyses
To determine if there were differences in scoring between patients with temporary versus permanent stoma placement, we conducted a subgroup analysis of pre-belt, 4-week, and 8-week survey scores across groups (Table 3). At baseline (pre-belt), there were no statistically significant differences between the temporary and permanent ostomy groups across all QOL domains, including overall life satisfaction (t(38) = −0.618, p = 0.541), life satisfaction over the last month (t(38) = −1.125, p = 0.268), work (t(38) = −0.901, p = 0.373), sexuality and body image (t(37) = −1.440, p = 0.158), stoma function (t(38) = −1.445, p = 0.157), financial concerns (t(38) = 0.857, p = 0.397), and skin irritation (t(38) = 0.373, p = 0.711).

Table 3.
Mean Stoma Quality of Life Scale questionnaire (SQOLS) scores at pre-belt, 4-week, and 8-week post ostomy support belt use stratified by temporary versus permanent ostomy type. * p < 0.05.
At 4 weeks of using the belt, permanent ostomy patients had significantly higher mean scores compared to temporary ostomy patients in overall life satisfaction (t(37) = −2.394, p = 0.022), life satisfaction over the last month (t(37) = −2.893, p = 0.006), and work (t(35) = −2.046, p = 0.048). By 8 weeks of using the belt, the permanent ostomy group continued to show statistically significantly higher QOL scores compared to the temporary group. There were significant differences in overall life satisfaction (t (37) = −2.547, p = 0.015), life satisfaction over the last month (t(36) = −3.677, p < 0.001), work (t(37) = −2.896, p = 0.006), sexuality and body image (t(37) = −2.594, p = 0.014), and stoma function (t(37) = −3.383, p = 0.002). There were no significant differences noted in financial concerns (t (37) = −0.750, p = 0.458) or skin irritation (t(37) = −1.009, p = 0.320).
Additionally, we conducted an analysis between ostomy types, ileostomy, and colostomy at each survey time point for survey scores (Table 4). In the pre-belt survey time point, there was a significant difference in mean financial concerns scores between groups with ileostomy scores (M = 78, SD = 30) being higher than colostomy scores (M = 52, SD = 40); (t(36) = −2.411, p = 0.021). No other scale significantly differed between groups in the pre-belt time point. There was no significant difference in survey scores between ostomy type groups in the 4-week survey time point. At the 8-week study time point, there were significant differences in skin irritation scores between ileostomy (M = 45, SD = 32) and colostomy (M = 65, SD = 19) patients; t(30) = 2.383, p = 0.024). No other scale significantly differed between groups in the 8-week time point.

Table 4.
Mean Stoma Quality of Life Scale questionnaire (SQOLS) scores at pre-belt, 4-week, and 8-week post ostomy support belt use, stratified by ostomy type. * p < 0.05.
4. Discussion
To our knowledge, this is the first prospective interventional study to assess the impact of ostomy belts on QOL for stoma patients. We found that the QOL domains of overall and recent life satisfaction, work/social function, sexuality/body image, and stoma function all improved with use of an ostomy support belt. This improvement was seen at the 4-week follow-up and was maintained at the 8-week follow-up. Our study findings support the use of ostomy support belts as a simple intervention to improve QOL in stoma patients.
Only one other recent study has examined the effect of ostomy support belt use on QOL. This non-interventional descriptive study found a decrease in leakage and peristomal irritation with ostomy belt use with corresponding improvement in mean QOL scores, which were postulated to be clinically significant, although the improvement in QOL scores did not reach statistical significance [17]. The study authors compared their QOL survey scores in ostomy support belt wearers to a separate cohort from another study using the same QOL survey and found that QOL mean scores in those who wore an ostomy support belt were significantly higher in the physical (p < 0.0001), social (p < 0.0001), and spiritual (p < 0.0001) well-being domains and the total mean score (p < 0.0001) [17]. Based on these findings, the authors concluded that the use of an ostomy support belt may offer an intervention to decrease the frequency of leakage and peristomal skin irritation and improve QOL. While our study used a different validated, ostomy-specific QOL survey, we also found an improvement in stoma function with support belt wear, although no significant change was noted in the level of skin irritation.
In our subgroup analysis comparing groups by temporary versus permanent stoma, we found that those with permanent ostomies had significantly higher 4-week and 8-week QOL scores compared to temporary ostomy patients with higher scores in life satisfaction and the domains of work and social function by 4 weeks, and additionally higher sexuality and body image and stoma function scores by 8 weeks. Adjusting to the physical changes of an ostomy can have severe psychological consequences that affect QOL, and this can differ between temporary and permanent ostomy patients [22,23]. Adjustment to the stoma, which is individualized and influenced by multiple pre- and post-operative factors, is essential for predicting patient QOL [24]. Multiple studies on adjustment after stoma have shown that permanent ostomates have better adjustment than temporary ostomates [22]. Our findings align with these studies, as permanent ostomates in our cohort had higher QOL scores after 4- and 8-weeks use of the belt. Combined, our studies provide promising evidence on the use of ostomy belts to help in multiple domains of QOL as well as adjustment to ostomy use and may provide especially positive benefits for permanent ostomy patients.
The literature has shown that ostomy use and associated peristomal leakage affects many aspects of QOL, including psychological, social, and sexual health through stigma and embarrassment and limitations to social and physical activities [3,4,5,6,25,26,27,28]. The QOL measures in our study that had significant improvements were life satisfaction overall and over the last month, work/social function, sexuality/body image, and stoma function. The ostomy support belts help prevent the ostomy bag from shifting around and leaking, helping to conceal and support the weight of the pouch. This promotes self-confidence when returning to daily activities with a stoma, making patients feel more comfortable psychologically and physically. If patients are less bothered by their pouch and more able to participate in physical activity, which is generally reduced in patients with stoma, and return to participation in previously enjoyed activities, this is expected to improve QOL and life satisfaction [15,16]. Exercise has already demonstrated improvement in QOL in numerous populations, including cancer and IBD, which are most relevant to our cohort [29,30], and has also been associated with lower rates of parastomal hernia [31]. Thus, our observed improvement in QOL using a stoma support belt may be mediated by increased participation in activities including exercise. It is not surprising that there were no differences in financial concerns over the 8-week period, as this dimension primarily addressed the cost of stoma supplies, and this would not likely change with the use of an ostomy belt. In our subgroup analysis between ileostomy and colostomy patients, there was an initial pre-belt difference in financial concerns amongst groups, with colostomy patients expressing more financial concerns with a lower score in this QOL domain. However, the scores were not significantly different at the 4-week and 8-week time periods. This may have been due to unaccounted-for patient factors, such as insurance coverage, that we were not able to include in our analysis. Additionally with skin irritation around the stoma, while the ostomy belt may help, this is also a difference seen between colostomy and ileostomy patients that may be contributing more to this dimension than the ostomy belt. In this subgroup analysis, we found that the ileostomy group had significantly lower satisfaction scores in the skin irritation domain than colostomy patients at the 8-week time point. Interestingly, while it did not reach statistical significance, the skin irritation QOL scores at pre-belt and 4-week time points for ileostomy patients were lower (less satisfaction) than colostomy patients. This aligns with the current literature, as up to 80% of patients with an ostomy experience skin-related complications, which are frequently caused by pouch leakage, and this is often worse in ileostomy patients due to the more caustic nature of ileostomy output [13,17,32,33].
Given that cost is of concern both to patients and the healthcare system, use of ostomy support belts can provide a simple low-cost intervention to improve QOL. Currently, most ostomy support belt prices range from under the 10s to mid-100s in USD, depending on the manufacturer of the appliance and associated features, and are recommended to be replaced about twice per year [34]. Many of these belts are currently covered by insurance in the US. Besides offering a low-cost intervention to improve QOL, ostomy support belts can also lead to potential significant cost savings by preventing complications of skin breakdown caused by leakage and by preventing the formation of parastomal hernias, which are a common complication after stoma formation. Furthermore, our results suggest ostomy support belt use may prevent the negative interference with work and school that is often reported by patients with stomas.
The strengths of our study include its prospective, interventional design and use of a validated stoma-specific QOL questionnaire that addresses multiple domains of QOL. We were also able to capture a population with a relatively even representation of men and women as well as colostomies and ileostomies. While the pre-belt survey time point essentially served as a control, this study could have benefited from a separate control group. Our study has several other important limitations. Notably, our methodology did not capture a comprehensive socioeconomic profile of the participants, including economic situation and marital status, both before and after ostomy formation. These factors can significantly influence an individual’s quality of life and their adaptation to living with a stoma. The study’s patient population, while ethnically diverse, is lacking in racial diversity and therefore lacks generalizability in more racially diverse populations. It is imperative for future research to validate the suitability of the ostomy support belt across diverse demographic and cultural contexts to ensure the generalizability of the results. The lack of homogeneity of our patient population is another limitation. Our study cohort included a mix of ileostomies and colostomies, which differ significantly in their physiological and practical management challenges, such as flow rate, skin consequences, and appliance issues. Additionally, the intervention was implemented at varying stages of post-stoma creation, which could influence outcomes due to differences in patient education, adjustment to stoma care, and the implementation of hygieno-dietary and medicinal measures for flow rate control. However, these variances underscore the need for a standardized approach in timing the intervention to better isolate the effects of the ostomy belt. Finally, our approach was limited by the absence of a control group and the presence of missing data in approximately 10% of cases, which introduces potential biases. Future studies should employ larger, randomized control trials with a homogenized population to minimize these biases and enhance the robustness of the findings. Additionally, more longitudinal data on the durability of the intervention would further support the utility of ostomy belts as an intervention to improve QOL.
5. Conclusions
In conclusion, this study represents the first prospective interventional study that provides evidence for the simple low-cost intervention of ostomy support belt use in improving QOL in patients with a stoma, a population that is known to have reduced QOL over a variety of domains, including psychological, social, and physical health. Currently, there is a need for additional studies examining interventions to improve QOL in this population, but our study results suggest that ostomy support belts should be considered by clinicians to improve patients’ QOL. Larger long-term interventional studies are warranted to confirm these findings and assess the durability of response over time.
Author Contributions
Conception and design: E.K.K., A.M.R., and V.W.H.; Acquisition of data: E.K.K., A.M.R., and V.W.H.; Analysis and interpretation of data: E.K.K., A.E.H., and V.W.H.; Drafting the manuscript: E.K.K., A.E.H. and V.W.H.; Revising it for intellectual content: E.K.K., A.E.H., and V.W.H.; Final approval of the completed manuscript: E.K.K., A.E.H., A.M.R., and V.W.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of University of Miami (protocol code 20201333 20 January 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author [V.W.H.], upon reasonable request.
Acknowledgments
We would like to thank Maky Suarez for her valuable contributions in the recruitment of study participants, survey administration, and ostomy support belt coordination. We would also like to thank Stealth Belt for their donation of ostomy support belts for use during our study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ambe, P.C.; Kurz, N.R.; Nitschke, C.; Odeh, S.F.; Möslein, G.; Zirngibl, H. Intestinal Ostomy. Dtsch. Arztebl. Int. 2018, 115, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Colwell, J.C.; Bain, K.A.; Hansen, A.S.; Droste, W.; Vendelbo, G.; James-Reid, S. International Consensus Results: Development of Practice Guidelines for Assessment of Peristomal Body and Stoma Profiles, Patient Engagement, and Patient Follow-up. J. Wound Ostomy Cont. Nurs. 2019, 46, 497–504. [Google Scholar] [CrossRef]
- Ang, S.G.; Chen, H.C.; Siah, R.J.; He, H.G.; Klainin-Yobas, P. Stressors relating to patient psychological health following stoma surgery: An integrated literature review. Oncol. Nurs. Forum 2013, 40, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Vonk-Klaassen, S.M.; de Vocht, H.M.; den Ouden, M.E.; Eddes, E.H.; Schuurmans, M.J. Ostomy-related problems and their impact on quality of life of colorectal cancer ostomates: A systematic review. Qual. Life Res. 2016, 25, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Schiergens, T.S.; Hoffmann, V.; Schobel, T.N.; Englert, G.H.; Kreis, M.E.; Thasler, W.E.; Werner, J.; Kasparek, M.S. Long-term Quality of Life of Patients With Permanent End Ileostomy: Results of a Nationwide Cross-Sectional Survey. Dis. Colon. Rectum 2017, 60, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Zewude, W.C.; Derese, T.; Suga, Y.; Teklewold, B. Quality of Life in Patients Living with Stoma. Ethiop. J. Health Sci. 2021, 31, 993–1000. [Google Scholar] [CrossRef] [PubMed]
- Santos, V.L.; Augusto, F.S.; Gomboski, G. Health-Related Quality of Life in Persons with Ostomies Managed in an Outpatient Care Setting. J. Wound Ostomy Cont. Nurs. 2016, 43, 158–164. [Google Scholar] [CrossRef]
- Alenezi, A.; McGrath, I.; Kimpton, A.; Livesay, K. Quality of life among ostomy patients: A narrative literature review. J. Clin. Nurs. 2021, 30, 3111–3123. [Google Scholar] [CrossRef]
- Ayaz-Alkaya, S. Overview of psychosocial problems in individuals with stoma: A review of literature. Int. Wound J. 2019, 16, 243–249. [Google Scholar] [CrossRef]
- Cakir, S.K.; Ozbayir, T. The effect of preoperative stoma site marking on quality of life. Pak. J. Med. Sci. 2018, 34, 149–153. [Google Scholar] [CrossRef]
- Goldstine, J.; van Hees, R.; van de Vorst, D.; Skountrianos, G.; Nichols, T. Factors influencing health-related quality of life of those in the Netherlands living with an ostomy. Br. J. Nurs. 2019, 28, S10–S17. [Google Scholar] [CrossRef] [PubMed]
- Khalilzadeh Ganjalikhani, M.; Tirgari, B.; Roudi Rashtabadi, O.; Shahesmaeili, A. Studying the effect of structured ostomy care training on quality of life and anxiety of patients with permanent ostomy. Int. Wound J. 2019, 16, 1383–1390. [Google Scholar] [CrossRef] [PubMed]
- Pittman, J.; Rawl, S.M.; Schmidt, C.M.; Grant, M.; Ko, C.Y.; Wendel, C.; Krouse, R.S. Demographic and clinical factors related to ostomy complications and quality of life in veterans with an ostomy. J. Wound Ostomy Cont. Nurs. 2008, 35, 493–503. [Google Scholar] [CrossRef]
- Chunli Liao, Y.Q. Factors associated with stoma quality of life among stoma patients. Int. J. Nurs. Sci. 2014, 1, 196–201. [Google Scholar] [CrossRef]
- Russell, S. Physical activity and exercise after stoma surgery: Overcoming the barriers. Br. J. Nurs. 2017, 26, S20–S26. [Google Scholar] [CrossRef] [PubMed]
- Eyl, R.E.; Koch-Gallenkamp, L.; Jansen, L.; Walter, V.; Carr, P.; Hoffmeister, M.; Chang-Claude, J.; Brenner, H.; Arndt, V. Potential determinants of physical inactivity among long-term colorectal cancer survivors. J. Cancer Surviv. 2018, 12, 679–690. [Google Scholar] [CrossRef] [PubMed]
- Pittman, J.; Colwell, J.; Mulekar, M.S. Ostomy Complications and Quality of Life of Ostomy Support Belt/Garment Wearers: A Web-Based Survey. J. Wound Ostomy Cont. Nurs. 2022, 49, 60–68. [Google Scholar] [CrossRef]
- Baxter, N.N.; Novotny, P.J.; Jacobson, T.; Maidl, L.J.; Sloan, J.; Young-Fadok, T.M. A stoma quality of life scale. Dis. Colon. Rectum 2006, 49, 205–212. [Google Scholar] [CrossRef]
- Kuruvilla, K.; Osler, T.; Hyman, N.H. A comparison of the quality of life of ulcerative colitis patients after IPAA vs ileostomy. Dis. Colon. Rectum 2012, 55, 1131–1137. [Google Scholar] [CrossRef]
- Neuman, H.B.; Patil, S.; Fuzesi, S.; Wong, W.D.; Weiser, M.R.; Guillem, J.G.; Paty, P.B.; Nash, G.M.; Temple, L.K. Impact of a temporary stoma on the quality of life of rectal cancer patients undergoing treatment. Ann. Surg. Oncol. 2011, 18, 1397–1403. [Google Scholar] [CrossRef]
- Knowles, S.R.; Wilson, J.; Wilkinson, A.; Connell, W.; Salzberg, M.; Castle, D.; Desmond, P.; Kamm, M.A. Psychological well-being and quality of life in Crohn’s disease patients with an ostomy: A preliminary investigation. J. Wound Ostomy Cont. Nurs. 2013, 40, 623–629. [Google Scholar] [CrossRef]
- Kittscha, J.; Fairbrother, G.; Bliokas, V.; Wilson, V. Adjustment to an Ostomy: An Integrative Literature Review. J. Wound Ostomy Cont. Nurs. 2022, 49, 439–448. [Google Scholar] [CrossRef]
- de Gouveia Santos, V.L.; Chaves, E.C.; Kimura, M. Quality of life and coping of persons with temporary and permanent stomas. J. Wound Ostomy Cont. Nurs. 2006, 33, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Whiteley, I.; Randall, S.; Stanaway, F.F. Comparison of Adjustment or Adaptation to the Formation of a Temporary versus a Permanent Ostomy: A Systematic Review. J. Wound Ostomy Cont. Nurs. 2024, 51, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Annells, M. The experience of flatus incontinence from a bowel ostomy: A hermeneutic phenomenology. J. Wound Ostomy Cont. Nurs. 2006, 33, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Sun, V.; Grant, M.; McMullen, C.K.; Altschuler, A.; Mohler, M.J.; Hornbrook, M.C.; Herrinton, L.J.; Baldwin, C.M.; Krouse, R.S. Surviving colorectal cancer: Long-term, persistent ostomy-specific concerns and adaptations. J. Wound Ostomy Cont. Nurs. 2013, 40, 61–72. [Google Scholar] [CrossRef]
- Torquato Lopes, A.P.; Decesaro, M. The adjustments experienced by persons with an ostomy: An integrative review of the literature. Ostomy Wound Manag. 2014, 60, 34–42. [Google Scholar]
- Manderson, L. Boundary breaches: The body, sex and sexuality after stoma surgery. Soc. Sci. Med. 2005, 61, 405–415. [Google Scholar] [CrossRef]
- Mishra, S.I.; Scherer, R.W.; Snyder, C.; Geigle, P.M.; Berlanstein, D.R.; Topaloglu, O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst. Rev. 2012, 2012, Cd008465. [Google Scholar] [CrossRef]
- Packer, N.; Hoffman-Goetz, L.; Ward, G. Does physical activity affect quality of life, disease symptoms and immune measures in patients with inflammatory bowel disease? A systematic review. J. Sports Med. Phys. Fit. 2010, 50, 1–18. [Google Scholar]
- Park, J.; Rivard, S.J.; Maguire, L.; Varlamos, C.; Duby, A.; Hendren, S. Parastomal Hernia Rates and Exercise after Ostomy Surgery. Dis. Colon. Rectum 2023, 66, 823–830. [Google Scholar] [CrossRef]
- Richbourg, L.; Thorpe, J.M.; Rapp, C.G. Difficulties experienced by the ostomate after hospital discharge. J. Wound Ostomy Cont. Nurs. 2007, 34, 70–79. [Google Scholar] [CrossRef]
- Salvadalena, G.D. The incidence of stoma and peristomal complications during the first 3 months after ostomy creation. J. Wound Ostomy Cont. Nurs. 2013, 40, 400–406. [Google Scholar] [CrossRef]
- Hoeflok, J. Ostomy Belts. Available online: https://badgut.org/information-centre/ostomies/ostomy-belts/ (accessed on 6 September 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).