Comparative Analysis of Open Transforaminal Lumbar Interbody Fusion and Wiltse Transforaminal Lumbar Interbody Fusion Approaches for Treating Single-Level Lumbar Spondylolisthesis: A Single-Center Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Conservative Treatment Prior to Surgery
2.2. Indications for Selection of Open TLIF vs. Wiltse TLIF Approach
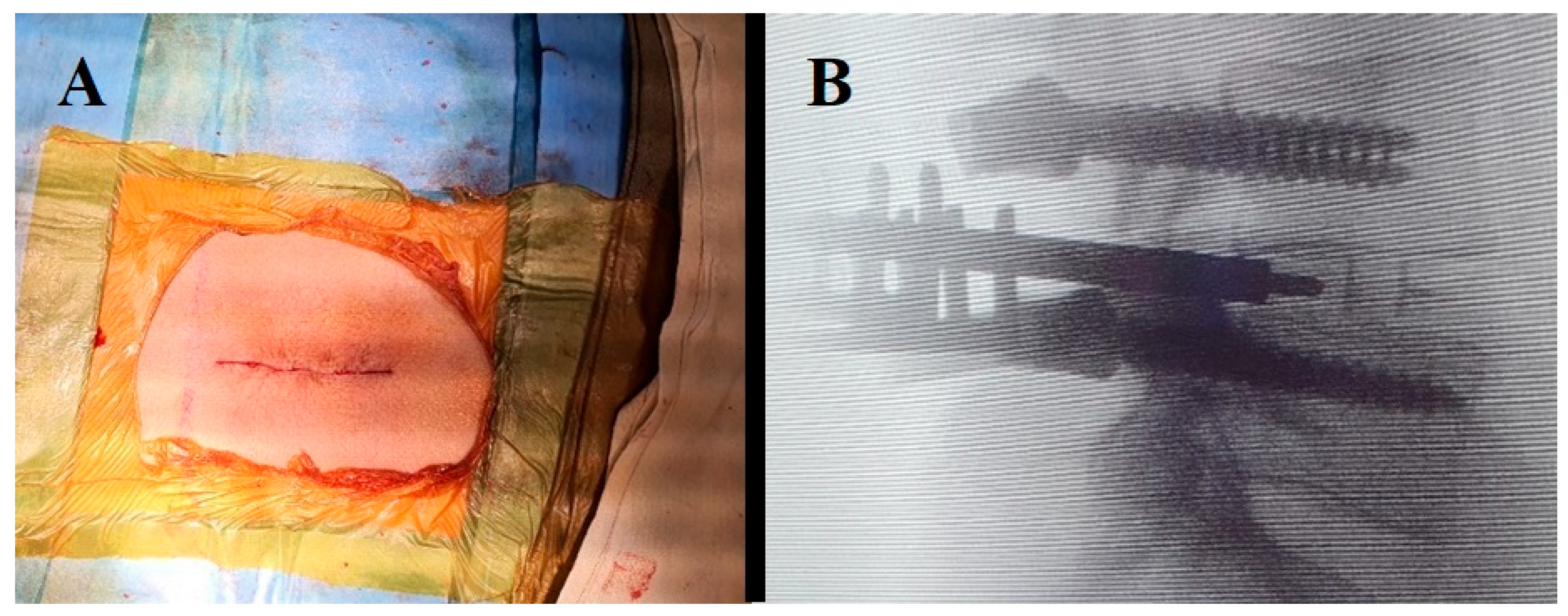
2.3. Surgical Technique in Open TLIF
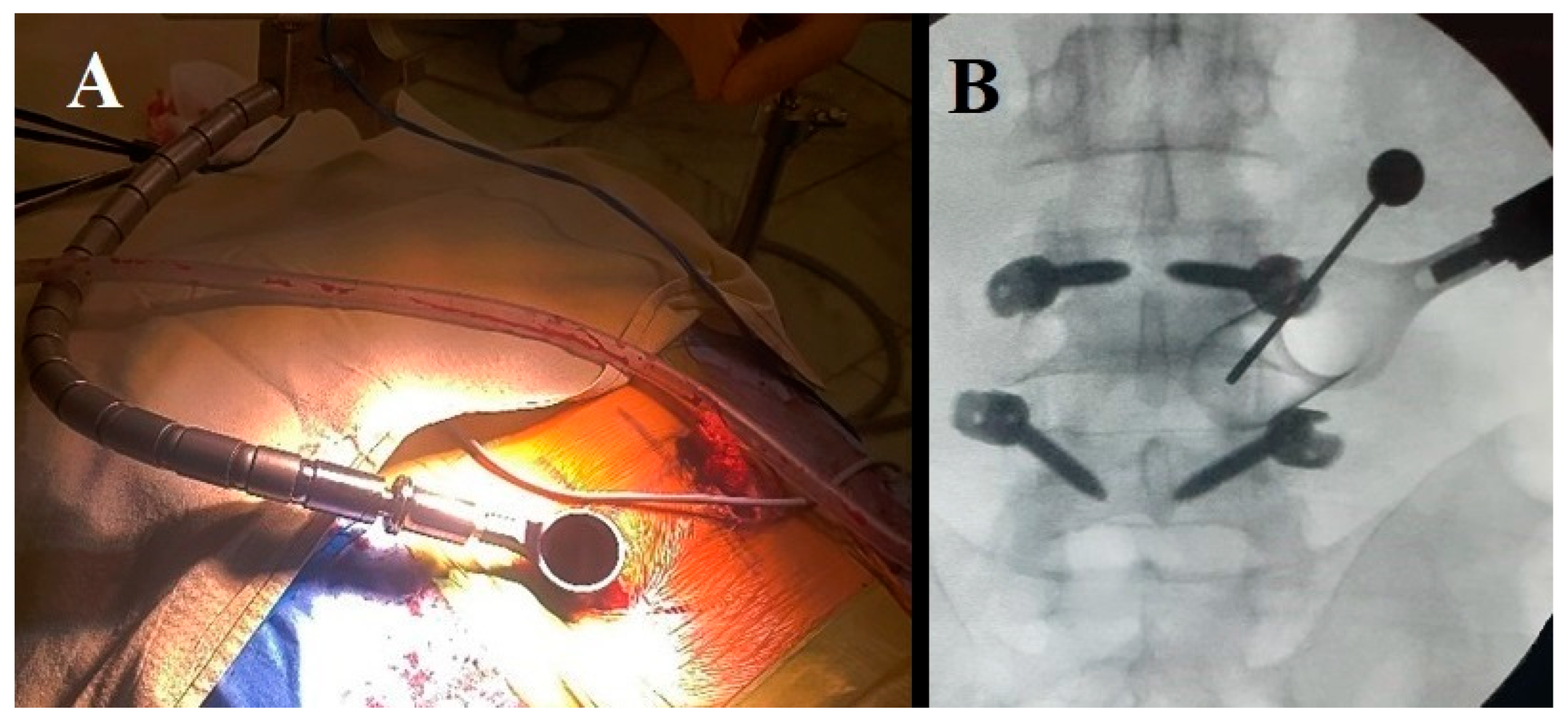
2.4. Bilateral Wiltse TLIF Approach
2.5. Data Presentation
2.6. Comparison of Group Means
2.7. Statistical Analysis and Significance Level
3. Results
4. Discussion
Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spiker, W.R.; Goz, V.; Brodke, D.S. Lumbar Interbody Fusions for Degenerative Spondylolisthesis: Review of Techniques, Indications, and Outcomes. Glob. Spine J. 2019, 9, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.; Gu, G.; Zhu, Y.; Guan, X.; Hu, A.; Wu, X.; Zhang, H.; He, S. Minimally Invasive Transforaminal Lumbar Interbody Fusion for Isthmic Spondylolisthesis: In Situ Versus Reduction. World Neurosurg. 2016, 90, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Sivaraman, A.; Altaf, F.; Jalgaonkar, A.; Kakkar, R.; Sirigiri, P.B.; Howieson, A.; Crawford, R.J. Prospective study of posterior lumbar interbody fusion with either interbody graft or interbody cage in the treatment of degenerative spondylolisthesis. J. Spinal Disord. Tech. 2015, 28, E467–E471. [Google Scholar] [CrossRef] [PubMed]
- Ha, K.Y.; Na, K.H.; Shin, J.H.; Kim, K.W. Comparison of posterolateral fusion with and without additional posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis. J. Spinal Disord. Tech. 2008, 21, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Momin, A.A.; Steinmetz, M.P. Evolution of Minimally Invasive Lumbar Spine Surgery. World Neurosurg. 2020, 140, 622–626. [Google Scholar] [CrossRef]
- Cutler, A.R.; Siddiqui, S.; Mohan, A.L.; Hillard, V.H.; Cerabona, F.; Das, K. Comparison of polyetheretherketone cages with femoral cortical bone allograft as a single-piece interbody spacer in transforaminal lumbar interbody fusion. J. Neurosurg. Spine 2006, 5, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Houten, J.K.; Post, N.H.; Dryer, J.W.; Errico, T.J. Clinical and radiographically/neuroimaging documented outcome in transforaminal lumbar interbody fusion. Neurosurg. Focus 2006, 20, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Potter, B.K.; Freedman, B.A.; Verwiebe, E.G.; Hall, J.M.; Polly, D.W., Jr.; Kuklo, T.R. Transforaminal lumbar interbody fusion: Clinical and radiographic results and complications in 100 consecutive patients. J. Spinal Disord. Tech. 2005, 18, 337–346. [Google Scholar] [CrossRef]
- Liang, Y.; Shi, W.; Jiang, C.; Chen, Z.; Liu, F.; Feng, Z.; Jiang, X. Clinical outcomes and sagittal alignment of single-level unilateral instrumented transforaminal lumbar interbody fusion with a 4 to 5-year follow-up. Eur. Spine J. 2015, 24, 2560–2566. [Google Scholar] [CrossRef]
- Nurmukhametov, R.; Dosanov, M.; Encarnacion, M.D.; Barrientos, R.; Matos, Y.; Alyokhin, A.I.; Baez, I.P.; Efe, I.E.; Restrepo, M.; Chavda, V.; et al. Transforaminal Fusion Using Physiologically Integrated Titanium Cages with a Novel Design in Patients with Degenerative Spinal Disorders: A Pilot Study. Surgeries 2022, 3, 175–184. [Google Scholar] [CrossRef]
- Foley, K.T.; Holly, L.T.; Schwender, J.D. Minimally Invasive Lumbar Fusion. Spine 2003, 28, S26–S35. [Google Scholar] [CrossRef]
- Styf, J.R.; Willén, J. The Effects of External Compression by Three Different Retractors on Pressure in the Erector Spine Muscles During and After Posterior Lumbar Spine Surgery in Humans. Spine 1998, 23, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Tian, N.-F.; Wu, Y.-S.; Zhang, X.-L.; Xu, H.-Z.; Chi, Y.-L.; Mao, F.-M. Minimally invasive versus open transforaminal lumbar interbody fusion: A meta-analysis based on the current evidence. Eur. Spine J. 2013, 22, 1741–1749. [Google Scholar] [CrossRef] [PubMed]
- Adogwa, O.; Parker, S.L.; Bydon, A.; Cheng, J.; Mcgirt, M.J. Comparative Effectiveness of Minimally Invasive Versus Open Transforaminal Lumbar Interbody Fusion: 2-year Assessment of Narcotic Use, Return to Work, Disability, and Quality of Life. Clin. Spine Surg. 2011, 24, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.; Zhao, X.; Zhao, F.; Xiangqian, F. Minimally Invasive Transforaminal Lumbar Interbody Fusion for the Treatment of Degenerative Lumbar Diseases. Spine 2010, 35, 1615–1620. [Google Scholar]
- Musa, G.; Barrientos Castillo, R.E.; Slabov, M.V.; Chirwa, K.; Chmutin, G.E.; Ramirez, M.d.J.E.; Nurmukhametov, R. Degenerative Grade 3 Spondylolisthesis Management: A Case Report and Literature Review. Cureus 2022, 14, e29374. [Google Scholar] [CrossRef]
- Ramirez, M.E.; Peralta, I.; Nurmukhametov, R.; Castillo, R.E.; Castro, J.S.; Volovich, A.; Dosanov, M.; Efe, I.E. Expanding access to microneurosurgery in low-resource settings: Feasibility of a low-cost exoscope in transforaminal lumbar interbody fusion. J. Neurosci. Rural Pract. 2023, 14, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Ahsan, K.; Khan, S.I.; Zaman, N.; Ahmed, N.; Montemurro, N.; Chaurasia, B. Fusion versus nonfusion treatment for recurrent lumbar disc herniation. J. Craniovertebral Junction Spine 2021, 12, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Liu, X. Clinical outcomes of two minimally invasive transforaminal lumbar interbody fusion (TLIF) for lumbar degenerative diseases. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhang, W.; Zhang, F.; Li, J.; Guo, L. Study of single-level lumbar degenerative diseases treated by unilateral wiltse access with unilateral nail rod fixation assisted by a new automatic retraction device. J. Orthop. Surg. Res. 2023, 18, 66. [Google Scholar] [CrossRef]
- Kim, S.H.; Hahn, B.S.; Park, J.Y. What Affects Segmental Lordosis of the Surgical Site after Minimally Invasive Transforaminal Lumbar Interbody Fusion? Yonsei Med. J. 2022, 63, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Li, J.; Sun, Y.; Wang, X.; Wang, W.; Guo, L.; Zhang, F.; Zhang, P.; Zhang, W. A Comparative Study of a New Retractor-Assisted WILTSE TLIF, MIS-TLIF, and Traditional PLIF for Treatment of Single-Level Lumbar Degenerative Diseases. Orthop. Surg. 2022, 14, 1317–1330. [Google Scholar] [CrossRef]
- Wang, S.; Duan, C.; Yang, H.; Kang, J.; Wang, Q. Wiltse Approach Versus Conventional Transforaminal Interbody Fusion for Unstable Thoracolumbar Fracture with Intervertebral Disc Lesions. Orthop. Surg. 2022, 14, 694–703. [Google Scholar] [CrossRef] [PubMed]
- Pull ter Gunne, A.F.; Cohen, D.B. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine 2009, 34, 1422–1428. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, A.J.; Ochoa, L.M.; Bader, J.O.; Belmont, P.J., Jr. Risk factors for immediate postoperative complications and mortality following spine surgery: A study of 3475 patients from the National Surgical Quality Improvement Program. J. Bone Jt. Surg. 2011, 93, 1577–1582. [Google Scholar] [CrossRef] [PubMed]
- Parker, S.L.; Adogwa, O.; Witham, T.F.; Aaronson, O.S.; Cheng, J.; McGirt, M.J. Post-Operative Infection after Minimally Invasive versus Open Transforaminal Lumbar Interbody Fusion (TLIF): Literature Review and Cost Analysis. Minim. Invasive Neurosurg. 2011, 54, 33–37. [Google Scholar] [CrossRef]
- Williams, B.J.; Sansur, C.A.; Smith, J.S.; Berven, S.H.; Broadstone, P.A.; Choma, T.J.; Goytan, M.J.; Noordeen, H.H.; Knapp, D.R.; Hart, R.A.; et al. Incidence of unintended durotomy in spine surgery based on 108,478 cases. Neurosurgery 2011, 68, 117–123. [Google Scholar] [CrossRef]
- Nandyala, S.V.; Fineberg, S.J.; Pelton, M.; Singh, K. Minimally invasive transforaminal lumbar interbody fusion: One surgeon’s learning curve. Spine J. 2014, 14, 1460–1465. [Google Scholar] [CrossRef]
- Patel, J.; Kundnani, V.; Raut, S.; Meena, M.; Ruparel, S. Perioperative Complications of Minimally Invasive Transforaminal Lumbar Interbody Fusion (MI-TLIF): 10 Years of Experience With MI-TLIF. Glob. Spine J. 2021, 11, 733–739. [Google Scholar] [CrossRef]
- Kanna, R.M.; Renjith, K.R.; Shetty, A.P.; Rajasekaran, S. Classification and Management Algorithm for Postoperative Wound Complications Following Transforaminal Lumbar Interbody Fusion. Asian Spine J. 2020, 14, 673–681. [Google Scholar] [CrossRef]
- Sclafani, J.A.; Raiszadeh, K.; Raiszadeh, R.; Kim, P.; Doerr, T.; Siddiqi, F.; LaMotta, I.; Park, P.; Templin, C.; Gill, S.; et al. Validation and analysis of a multi-site MIS Prospective Registry through sub-analysis of an MIS TLIF Subgroup. Int. J. Spine Surg. 2014, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.; Rao, P.J.; Kam, A.C.; Mobbs, R.J. Minimally invasive versus open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: Systematic review and meta-analysis. Eur. Spine J. 2015, 24, 1017–1030. [Google Scholar] [CrossRef]
- Chan, A.K.; Bisson, E.F.; Bydon, M.; Glassman, S.D.; Foley, K.T.; Potts, E.A.; Shaffrey, C.I.; Shaffrey, M.E.; Coric, D.; Knightly, J.J.; et al. A comparison of minimally invasive transforaminal lumbar interbody fusion and decompression alone for degenerative lumbar spondylolisthesis. Neurosurg. Focus 2019, 46, E13. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.K.; Bydon, M.; Bisson, E.F.; Glassman, S.D.; Foley, K.T.; Shaffrey, C.I.; Potts, E.A.; Shaffrey, M.E.; Coric, D.; Knightly, J.J.; et al. Minimally invasive versus open transforaminal lumbar interbody fusion for grade I lumbar spondylolisthesis: 5-year follow-up from the prospective multicenter Quality Outcomes Database registry. Neurosurg. Focus 2023, 54, E2. [Google Scholar] [CrossRef]
- Mummaneni, P.V.; Bisson, E.F.; Kerezoudis, P.; Glassman, S.; Foley, K.; Slotkin, J.R.; Potts, E.; Shaffrey, M.; Shaffrey, C.I.; Coric, D.; et al. Minimally invasive versus open fusion for Grade I degenerative lumbar spondylolisthesis: Analysis of the Quality Outcomes Database. Neurosurg. Focus 2017, 43, E11. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, C.L.; Macwan, K.; Sundararajan, K.; Rampersaud, R.Y. Comparative Outcomes of Minimally Invasive Surgery for Posterior Lumbar Fusion: A Systematic Review. Clin. Orthop. Relat. Res. 2014, 472, 1727–1737. [Google Scholar] [CrossRef]
- Lee, K.H.; Yeo, W.; Soeharno, H.; Yue, W.M. Learning Curve of a Complex Surgical Technique: Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF). Clin. Spine Surg. 2014, 27, E234–E240. [Google Scholar] [CrossRef]
- Jin-Tao, Q.; Yu, T.; Mei, W.; Xu-Dong, T.; Tian-Jian, Z.; Guo-Hua, S.; Lei, C.; Yue, H.; Zi-Tian, W.; Yue, Z. Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: A meta-analysis. Eur. Spine J. 2015, 24, 1058–1065. [Google Scholar] [CrossRef]
- Ahsan, M.K.; Hossain, M.R.; Khan, M.S.I.; Zaman, N.; Ahmed, N.; Montemurro, N.; Chaurasia, B. Lumbar revision microdiscectomy in patients with recurrent lumbar disc herniation: A single-center prospective series. Surg. Neurol. Int. 2020, 11, 404. [Google Scholar] [CrossRef]
- Perrini, P.; Pieri, F.; Montemurro, N.; Tiezzi, G.; Parenti, G.F. Thoracic extradural haematoma after epidural anaesthesia. Neurol. Sci. 2010, 31, 87–88. [Google Scholar] [CrossRef]
- Patel, K.; Harikar, M.M.; Venkataram, T.; Chavda, V.; Montemurro, N.; Assefi, M.; Hussain, N.; Yamamoto, V.; Kateb, B.; Lewandrowski, K.-U.; et al. Is Minimally Invasive Spinal Surgery Superior to Endoscopic Spine Surgery in Postoperative Radiologic Outcomes of Lumbar Spine Degenerative Disease? A Systematic Review. J. Neurol. Surg. Part A Central Eur. Neurosurg. 2023, 8, 1. [Google Scholar] [CrossRef] [PubMed]
- Lei, F.; Li, Z.; He, W.; Tian, X.; Zheng, L.; Kang, J.; Feng, D. Total and hidden blood loss between open posterior lumbar interbody fusion and transforaminal lumbar interbody fusion by Wiltse approach. Medicine 2020, 99, e19864. [Google Scholar] [CrossRef] [PubMed]
- Kovari, V.Z.; Kuti, A.; Konya, K.; Szel, I.; Szekely, A.K.; Szalay, K. Comparison of Single-Level Open and Minimally Invasive Transforaminal Lumbar Interbody Fusions Presenting a Learning Curve. BioMed Res. Int. 2020, 2020, 3798537. [Google Scholar] [CrossRef] [PubMed]
- Sharif, S.; Afsar, A. Learning Curve and Minimally Invasive Spine Surgery. World Neurosurg. 2018, 119, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Chen, Q.; Chen, C.; Lyu, J.; Shi, B.; Yang, C.; Xia, C. Clinical Research and Technique Note of TLIF by Wiltse Approach for the Treatment of Degenerative Lumbar. Orthop. Surg. 2021, 13, 1628–1638. [Google Scholar] [CrossRef]
- Heo, D.H.; Hong, Y.H.; Lee, D.C.; Chung, H.J.; Park, C.K. Technique of Biportal Endoscopic Transforaminal Lumbar Interbody Fusion. Neurospine 2020, 17, S129–S137. [Google Scholar] [CrossRef]
- Lee, J.C.; Jang, H.D.; Shin, B.J. Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: Our experience in 86 consecutive cases. Spine 2012, 37, 1548–1557. [Google Scholar] [CrossRef]
- Montemurro, N. Telemedicine: Could it represent a new problem for spine surgeons to solve? Glob. Spine J. 2022, 12, 1306–1307. [Google Scholar] [CrossRef]
- Silva, P.S.; Pereira, P.; Monteiro, P.; Silva, P.A.; Vaz, R. Learning curve and complications of minimally invasive transforaminal lumbar interbody fusion. Neurosurg. Focus 2013, 35, E7. [Google Scholar] [CrossRef]
| Open TLIF Technique | Wiltse TLIF Technique | p-Value | |
|---|---|---|---|
| Number of patients | 300 | 300 | - |
| Age (years, mean ± SD) | 56.1 ± 7.9 | 50.3 ± 8.6 | 0.23 |
| Sex (M/F) | 160/140 | 155/145 | 0.78 |
| Time of surgery (min) | 136.2 ± 24.3 | 117.8 ± 19.6 | <0.01 |
| Time of fluoroscopy (s) | 18. ± 3 | 24.6 ± 6.4 | <0.05 |
| Blood loss (mL) | 467.8 ± 104.9 | 226.4 ± 56.5 | <0.01 |
| Outcome Measure | Open TLIF Technique | Wiltse TLIF Technique |
|---|---|---|
| VAS pre-op | 7.2 ± 1.1 | 7.4 ± 1.2 |
| VAS post-op | 2.0 ± 1.2 | 2.1 ± 1.4 |
| p-value | <0.05 | <0.05 |
| ODI pre-op | 61.7 ± 9.5 | 60.3 ± 8.9 |
| ODI post-op | 23.9 ± 5.9 | 25.1 ± 6.2 |
| p-value | <0.05 | <0.05 |
| Complications | Open TLIF Technique (Patient n° (%)) | Wiltse TLIF Technique (Patient n° (%)) | p-Value |
|---|---|---|---|
| Infection | 3 (1) | 1 (0.3) | 0.616 |
| Nerve damage | 2 (0.7) | 2 (0.7) | 1.000 |
| Dural tear | 3 (1) | 3 (1) | 1.000 |
| Implant malposition or failure | 1 (0.3) | - | 1.000 |
| Persistent pain | 1 (0.3) | - | 1.000 |
| Wound dehiscence | 3 (1) | - | 0.247 |
| Overall complications | 13 (4.3) | 7 (2.3) | 0.255 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nurmukhametov, R.; Dosanov, M.; Medetbek, A.; Encarnacion Ramirez, M.D.J.; Chavda, V.; Chmutin, G.; Montemurro, N. Comparative Analysis of Open Transforaminal Lumbar Interbody Fusion and Wiltse Transforaminal Lumbar Interbody Fusion Approaches for Treating Single-Level Lumbar Spondylolisthesis: A Single-Center Retrospective Study. Surgeries 2023, 4, 623-634. https://doi.org/10.3390/surgeries4040060
Nurmukhametov R, Dosanov M, Medetbek A, Encarnacion Ramirez MDJ, Chavda V, Chmutin G, Montemurro N. Comparative Analysis of Open Transforaminal Lumbar Interbody Fusion and Wiltse Transforaminal Lumbar Interbody Fusion Approaches for Treating Single-Level Lumbar Spondylolisthesis: A Single-Center Retrospective Study. Surgeries. 2023; 4(4):623-634. https://doi.org/10.3390/surgeries4040060
Chicago/Turabian StyleNurmukhametov, Renat, Medet Dosanov, Abakirov Medetbek, Manuel De Jesus Encarnacion Ramirez, Vishal Chavda, Gennady Chmutin, and Nicola Montemurro. 2023. "Comparative Analysis of Open Transforaminal Lumbar Interbody Fusion and Wiltse Transforaminal Lumbar Interbody Fusion Approaches for Treating Single-Level Lumbar Spondylolisthesis: A Single-Center Retrospective Study" Surgeries 4, no. 4: 623-634. https://doi.org/10.3390/surgeries4040060
APA StyleNurmukhametov, R., Dosanov, M., Medetbek, A., Encarnacion Ramirez, M. D. J., Chavda, V., Chmutin, G., & Montemurro, N. (2023). Comparative Analysis of Open Transforaminal Lumbar Interbody Fusion and Wiltse Transforaminal Lumbar Interbody Fusion Approaches for Treating Single-Level Lumbar Spondylolisthesis: A Single-Center Retrospective Study. Surgeries, 4(4), 623-634. https://doi.org/10.3390/surgeries4040060









