Head Regional Differences in Thermal Comfort: Evaluating a Novel Surgical Helmet Cooling Method with Phase Change Material
Abstract
:1. Introduction
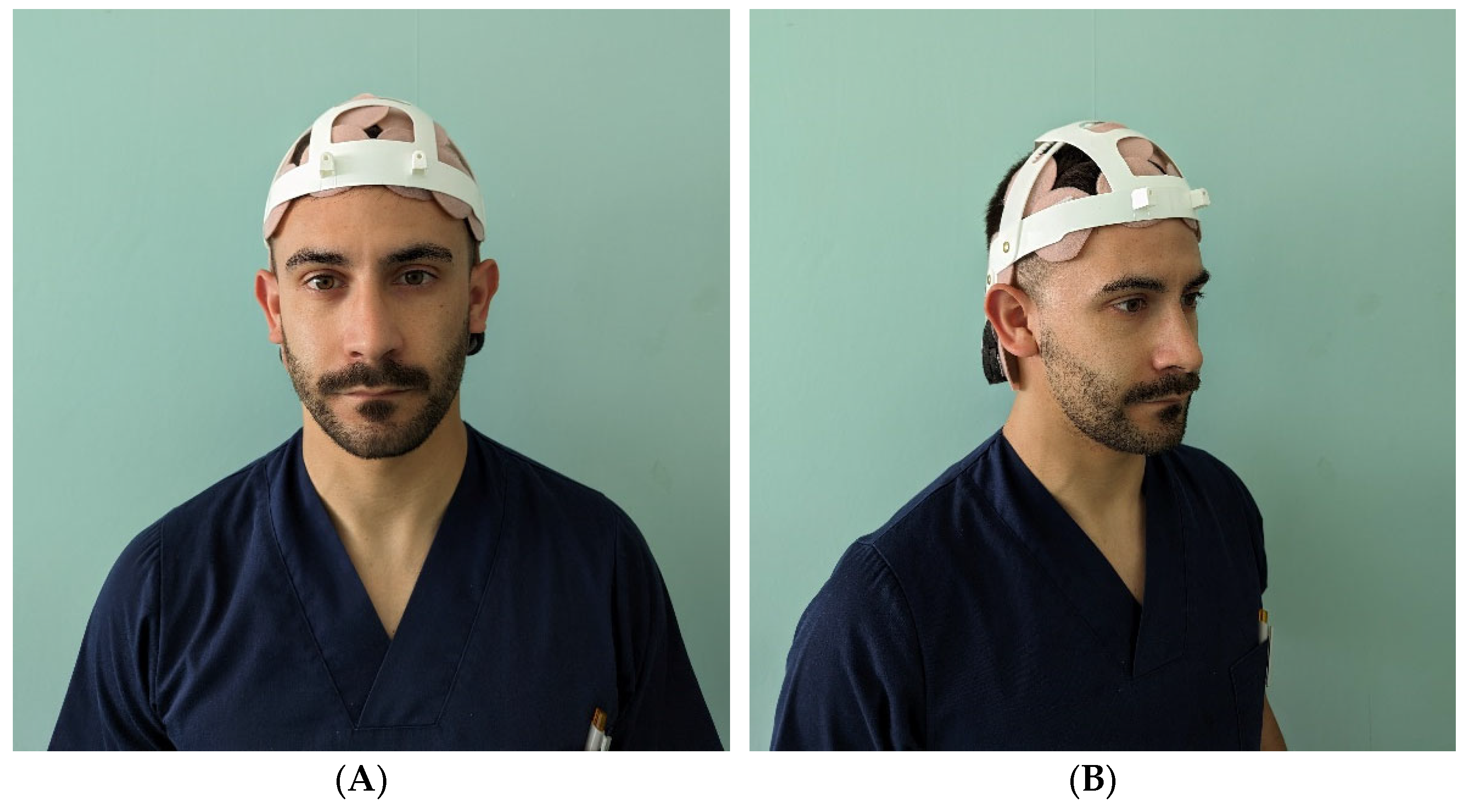
2. Materials and Methods
2.1. Participants
2.2. Test Procedure
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gasparini, G.; Castioni, D.; Spina, G.; Familiari, F.; Galasso, O.; Mercurio, M. The use of a surgical helmet system with a high-efficiency particulate air filter as possible protection equipment during the coronavirus disease 2019 pandemic: A double-blinded randomized control study. Int. Orthop. 2022, 46, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, J.; Gehrke, T.; Krueger, C.A.; Chisari, E.; Citak, M.; Van Onsem, S.; Walter, W.L. Resuming Elective Orthopaedic Surgery During the COVID-19 Pandemic. J. Bone Jt. Surg. 2020, 102, 1205–1212. [Google Scholar] [CrossRef]
- Rahardja, R.; Morris, A.J.; Hooper, G.J.; Grae, N.; Frampton, C.M.; Young, S.W. Surgical Helmet Systems Are Associated With a Lower Rate of Prosthetic Joint Infection After Total Knee Arthroplasty: Combined Results From the New Zealand Joint Registry and Surgical Site Infection Improvement Programme. J. Arthroplast. 2022, 37, 930–935.e1. [Google Scholar] [CrossRef]
- Castioni, D.; Galasso, O.; Rava, A.; Massè, A.; Gasparini, G.; Mercurio, M. Has the COVID-19 Pandemic Changed the Daily Practices and Psychological State of Orthopaedic Residents? Clin. Orthop. Relat. Res. 2021, 479, 1947–1954. [Google Scholar] [CrossRef]
- Nakamura, M.; Yoda, T.; Crawshaw, L.I.; Kasuga, M.; Uchida, Y.; Tokizawa, K.; Nagashima, K.; Kanosue, K. Relative importance of different surface regions for thermal comfort in humans. Eur. J. Appl. Physiol. 2013, 113, 63–76. [Google Scholar] [CrossRef]
- Nakamura, M.; Yoda, T.; Crawshaw, L.I.; Yasuhara, S.; Saito, Y.; Kasuga, M.; Nagashima, K.; Kanosue, K. Regional differences in temperature sensation and thermal comfort in humans. J. Appl. Physiol. 2008, 105, 1897–1906. [Google Scholar] [CrossRef]
- Arens, E.; Zhang, H.; Huizenga, C. Partial- and whole-body thermal sensation and comfort—Part I: Uniform environmental conditions. J. Therm. Biol. 2006, 31, 53–59. [Google Scholar] [CrossRef]
- Deiana, G.; Arghittu, A.; Dettori, M.; Deriu, M.G.; Palmieri, A.; Azara, A.; Castiglia, P.; Masia, M.D. Ten-Year Evaluation of Thermal Comfort in Operating Rooms. Healthcare 2022, 10, 307. [Google Scholar] [CrossRef]
- Cotter, J.D.; Taylor, N.A.S. The distribution of cutaneous sudomotor and alliesthesial thermosensitivity in mildly heat-stressed humans: An open-loop approach. J. Physiol. 2005, 565, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Nunneley, S.A.; Reader, D.C.; Maldonado, R.J. Head-temperature effects on physiology, comfort, and performance during hyperthermia. Aviat. Space. Environ. Med. 1982, 53, 623–628. [Google Scholar] [PubMed]
- Hong, J.M.; Choi, E.S.; Park, S.Y. Selective Brain Cooling: A New Horizon of Neuroprotection. Front. Neurol. 2022, 13, 873165. [Google Scholar] [CrossRef] [PubMed]
- Galvin, I.M.; Levy, R.; Boyd, J.G.; Day, A.G.; Wallace, M.C. Cooling for cerebral protection during brain surgery. Cochrane Database Syst. Rev. 2015, 1, CD006638. [Google Scholar] [CrossRef]
- Sherman, A.L.; Wang, M.Y. Hypothermia as a Clinical Neuroprotectant. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 519–529. [Google Scholar] [CrossRef]
- Mattingly, T.; Lownie, S. Cold blood perfusion for selective hypothermia in acute ischemic stroke. Brain Circ. 2019, 5, 187. [Google Scholar] [CrossRef]
- Baraka, A.A.E.; Hassan, E.A.; El-Soussi, A.H.; Mohamed, H.E. Effect of selective brain cooling versus core cooling on achieving target temperature among patients with severe traumatic brain injury. Int. J. Africa Nurs. Sci. 2020, 13, 100209. [Google Scholar] [CrossRef]
- Bernard, S.; Buist, M.; Monteiro, O.; Smith, K. Induced hypothermia using large volume, ice-cold intravenous fluid in comatose survivors of out-of-hospital cardiac arrest. Resuscitation 2003, 56, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Hypothermia after Cardiac Arrest Study Group. Mild Therapeutic Hypothermia to Improve the Neurologic Outcome after Cardiac Arrest. N. Engl. J. Med. 2002, 346, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Lei, T.-H.; Wang, F.; Yang, B.; Mündel, T. Head, Face and Neck Cooling as Per-cooling (Cooling During Exercise) Modalities to Improve Exercise Performance in the Heat: A Narrative Review and Practical Applications. Sports Med. Open 2022, 8, 16. [Google Scholar] [CrossRef]
- Douzi, W.; Dugué, B.; Vinches, L.; Al Sayed, C.; Hallé, S.; Bosquet, L.; Dupuy, O. Cooling during exercise enhances performances, but the cooled body areas matter: A systematic review with meta-analyses. Scand. J. Med. Sci. Sports 2019, 29, 1660–1676. [Google Scholar] [CrossRef]
- Hamanishi, S.; Eguchi, E.; Ito, T.; Nagaoka, K.; Ogino, K. Head cooling during sleep improves sleep quality in the luteal phase in female university students: A randomized crossover-controlled pilot study. PLoS ONE 2019, 14, e0213706. [Google Scholar] [CrossRef] [PubMed]
- Byrne, J.; Ludington-Hoe, S.M.; Voss, J.G. Occupational Heat Stress, Thermal Comfort, and Cognitive Performance in the OR: An Integrative Review. AORN J. 2020, 111, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Tripathy, S.; Mahapatra, A. Targeted temperature management in brain protection: An evidence-based review. Indian J. Anaesth. 2015, 59, 9. [Google Scholar] [CrossRef] [PubMed]
- Kramer, C.; Freeman, W.D.; Larson, J.S.; Hoffman-Snyder, C.; Wellik, K.E.; Demaerschalk, B.M.; Wingerchuk, D.M. Therapeutic Hypothermia for Severe Traumatic Brain Injury. Neurologist 2012, 18, 173–177. [Google Scholar] [CrossRef]
- Pereira, P.F.d.C.; Broday, E.E.; Xavier, A.A.d.P. Thermal Comfort Applied in Hospital Environments: A Literature Review. Appl. Sci. 2020, 10, 7030. [Google Scholar] [CrossRef]
- Alaqeel, M.; Tanzer, M. Improving ergonomics in the operating room for orthopaedic surgeons in order to reduce work-related musculoskeletal injuries. Ann. Med. Surg. 2020, 56, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Gaoua, N.; Grantham, J.; Racinais, S.; El Massioui, F. Sensory displeasure reduces complex cognitive performance in the heat. J. Environ. Psychol. 2012, 32, 158–163. [Google Scholar] [CrossRef]
- Byrne, J.E.; Rodriguez-Patarroyo, F.A.; Mascha, E.J.; Han, Y.; Bravo, M.; Bloomfield, M.R.; Rao, S.M.; Sessler, D.I. Cooling vest improves surgeons’ thermal comfort without affecting cognitive performance: A randomised cross-over trial. Occup. Environ. Med. 2023, 80, 339–345. [Google Scholar] [CrossRef]
- Van Gaever, R.; Jacobs, V.A.; Diltoer, M.; Peeters, L.; Vanlanduit, S. Thermal comfort of the surgical staff in the operating room. Build. Environ. 2014, 81, 37–41. [Google Scholar] [CrossRef]
- Yang, B.; Lei, T.-H.; Wang, F.; Yang, P. On the use of facial and neck cooling to improve indoor occupant thermal comfort in warm conditions. bioRxiv 2021. [Google Scholar] [CrossRef]
- Assis, F.; Narasimhan, B.; Ziai, W.; Tandri, H. From systemic to selective brain cooling—Methods in review. Brain Circ. 2019, 5, 179. [Google Scholar] [CrossRef] [PubMed]
- Harris, B.; Andrews, P.; Murray, G.; Forbes, J.; Moseley, O. Systematic review of head cooling in adults after traumatic brain injury and stroke. Health Technol. Assess. 2012, 16, 1–175. [Google Scholar] [CrossRef]
- Zwolińska, M.; Bogdan, A. Thermal Sensations of Surgeons During Work in Surgical Gowns. Int. J. Occup. Saf. Ergon. 2013, 19, 443–453. [Google Scholar] [CrossRef]
- Langø, T.; Nesbakken, R.; Færevik, H.; Holbø, K.; Reitan, J.; Yavuz, Y.; Mårvik, R. Cooling vest for improving surgeons’ thermal comfort: A multidisciplinary design project. Minim. Invasive Ther. Allied Technol. 2009, 18, 20–29. [Google Scholar] [CrossRef]
- Jankowski, T.; Młynarczyk, M. An Impact of the Efficient Functioning of the Ventilation and Air-Conditioning System on Thermal Comfort of the Medical Staff in the Operating Room. J. Ecol. Eng. 2016, 17, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.; Mahgoub Bassuoni, M.; Elsamadony, M.; Raslan, M. Assessment of Thermal Comfort in Operating Rooms Using PMV-PPD Model. J. Eng. Res. 2020, 4, 51–62. [Google Scholar] [CrossRef]
- Yuan, F.; Yao, R.; Sadrizadeh, S.; Li, B.; Cao, G.; Zhang, S.; Zhou, S.; Liu, H.; Bogdan, A.; Croitoru, C.; et al. Thermal comfort in hospital buildings—A literature review. J. Build. Eng. 2022, 45, 103463. [Google Scholar] [CrossRef]
- Webborn, N.; Price, M.J.; Castle, P.; Goosey-Tolfrey, V.L. Cooling strategies improve intermittent sprint performance in the heat of athletes with tetraplegia. Br. J. Sports Med. 2010, 44, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Lei, T.-H.; Wang, F. Looking ahead of 2021 Tokyo Summer Olympic Games: How Does Humid Heat Affect Endurance Performance? Insight into physiological mechanism and heat-related illness prevention strategies. J. Therm. Biol. 2021, 99, 102975. [Google Scholar] [CrossRef] [PubMed]
- Piil, J.F.; Christiansen, L.; Morris, N.B.; Mikkelsen, C.J.; Ioannou, L.G.; Flouris, A.D.; Lundbye-Jensen, J.; Nybo, L. Direct exposure of the head to solar heat radiation impairs motor-cognitive performance. Sci. Rep. 2020, 10, 7812. [Google Scholar] [CrossRef]
- Mazalan, N.S.; Landers, G.J.; Wallman, K.E.; Ecker, U. A Combination of Ice Ingestion and Head Cooling Enhances Cognitive Performance during Endurance Exercise in the Heat. J. Sports Sci. Med. 2021, 21, 23–32. [Google Scholar] [CrossRef]
- Chinazzo, G.; Wienold, J.; Andersen, M. Daylight affects human thermal perception. Sci. Rep. 2019, 9, 13690. [Google Scholar] [CrossRef] [PubMed]
- Nastase, I.; Danca, P.; Bode, F.; Croitoru, C.; Fechete, L.; Sandu, M.; Coşoiu, C.I. A regard on the thermal comfort theories from the standpoint of Electric Vehicle design—Review and perspectives. Energy Rep. 2022, 8, 10501–10517. [Google Scholar] [CrossRef]
- Huang, C.-H.; Tsai, H.-H.; Chen, H. Influence of Weather Factors on Thermal Comfort in Subtropical Urban Environments. Sustainability 2020, 12, 2001. [Google Scholar] [CrossRef]
- Karahan, A.; Budak Ertürk, E.; Uğurlu, Z.; Ünlü, H.; Akovalı, N.; Tepe, A.; Özhan Elbaş, N. Factors Affecting the Thermal Comfort of Perioperative Personnel in the OR. AORN J. 2020, 111, 333–344. [Google Scholar] [CrossRef] [PubMed]



| Participants (n = 43) | Mean ± SD (Range) or n (%) |
|---|---|
| Gender | |
| Male | 23 (53.5%) |
| Female | 20 (46.5%) |
| Age (years) | 35.5 ± 13.5 (22–66) |
| Area | Sensation | Time | |
|---|---|---|---|
| Mean | SD | Mean | |
| 1 | 4 | 1 | na |
| 2 | 4 | 1 | na |
| 3 | 4 | 1 | na |
| 4 | 5 | 1 | 45 |
| 5 | 4 | 1 | na |
| 6 | 4 | 1 | na |
| 7 | 4 | 2 | na |
| 8 | 4 | 1 | na |
| 9 | 4 | 1 | na |
| 10 | 5 | 2 | 30 |
| 11 | 5 | 2 | 30 |
| 12 | 5 | 2 | 30 |
| 13 | 5 | 1 | 45 |
| 14 | 5 | 1 | 45 |
| 15 | 6 | 1 | 60 |
| 16 | 6 | 1 | 60 |
| 17 | 5 | 2 | 30 |
| 18 | 4 | 1 | na |
| 19 | 5 | 1 | 30 |
| 20 | 5 | 2 | 45 |
| 21 | 6 | 1 | 60 |
| 22 | 6 | 1 | 60 |
| 23 | 5 | 2 | 30 |
| 24 | 4 | 1 | na |
| 25 | 4 | 1 | na |
| 26 | 4 | 1 | na |
| 27 | 5 | 1 | 45 |
| 28 | 5 | 1 | 45 |
| 29 | 5 | 2 | 30 |
| 30 | 5 | 2 | 30 |
| 31 | 5 | 2 | 30 |
| 32 | 4 | 1 | na |
| 33 | 5 | 1 | 60 |
| 34 | 5 | 1 | 60 |
| 35 | 5 | 1 | 60 |
| 36 | 6 | 1 | 60 |
| 37 | 5 | 1 | 60 |
| 38 | 5 | 1 | 60 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mercurio, M.; Galasso, O.; de Filippis, R.; Familiari, F.; Gasparini, G. Head Regional Differences in Thermal Comfort: Evaluating a Novel Surgical Helmet Cooling Method with Phase Change Material. Surgeries 2023, 4, 556-567. https://doi.org/10.3390/surgeries4040054
Mercurio M, Galasso O, de Filippis R, Familiari F, Gasparini G. Head Regional Differences in Thermal Comfort: Evaluating a Novel Surgical Helmet Cooling Method with Phase Change Material. Surgeries. 2023; 4(4):556-567. https://doi.org/10.3390/surgeries4040054
Chicago/Turabian StyleMercurio, Michele, Olimpio Galasso, Renato de Filippis, Filippo Familiari, and Giorgio Gasparini. 2023. "Head Regional Differences in Thermal Comfort: Evaluating a Novel Surgical Helmet Cooling Method with Phase Change Material" Surgeries 4, no. 4: 556-567. https://doi.org/10.3390/surgeries4040054
APA StyleMercurio, M., Galasso, O., de Filippis, R., Familiari, F., & Gasparini, G. (2023). Head Regional Differences in Thermal Comfort: Evaluating a Novel Surgical Helmet Cooling Method with Phase Change Material. Surgeries, 4(4), 556-567. https://doi.org/10.3390/surgeries4040054










