Delirium in Older Adults: What a Surgeon Needs to Know
Abstract
:1. Introduction
2. Materials and Methods
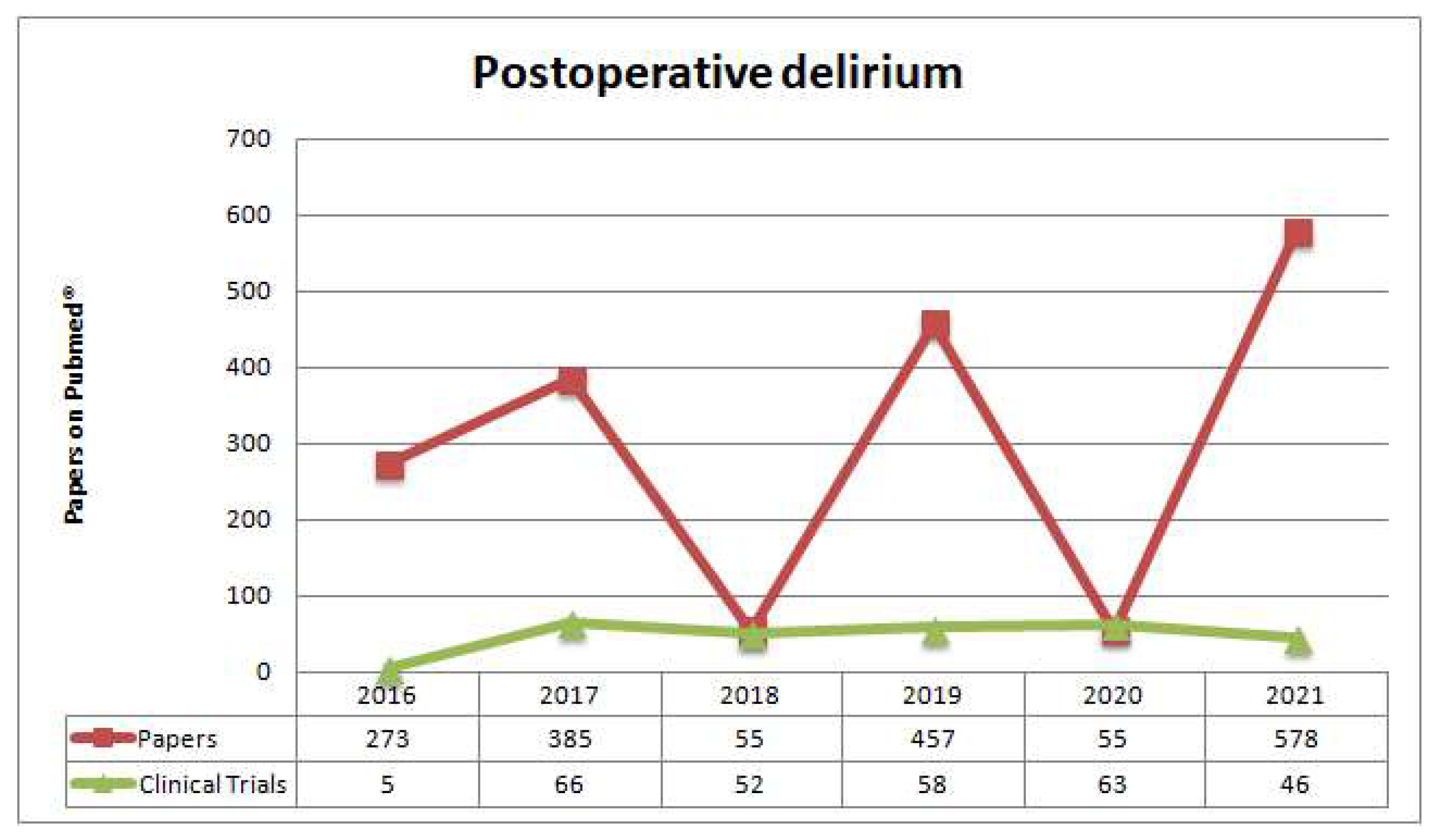
3. Results
3.1. Delirium Definition
- (A)
- Disturbance in attention (for example, reduced ability to direct, focus, sustain, and shift attention) and awareness (reduced orientation to the environment);
- (B)
- Disturbance that develops over a short period (usually hours to a few days), represents an acute change from baseline attention and awareness, and tends to fluctuate in severity during a day;
- (C)
- An additional disturbance in cognition (for example, deficit of memory, disorientation, language, visuospatial ability, or perception);
- (D)
- The disturbances in Criteria A and C are not better explained by a pre-existing, established, or evolving neurocognitive disorder, and do not occur in the context of a severely reduced level of arousal, such as a coma (Criterion D must not occur in the context of a severely reduced level of arousal, such as a coma);
- (E)
- There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substance intoxication or withdrawal (i.e., due to a drug of abuse or to a medication), or exposure to a toxin, or is due to multiple etiologies [3,4].
3.2. Delirium Pathophysiology
- Systemic inflammation, as a septic shock syndrome, can lead to neuroinflammation with microglial cells activation, neuronal dysfunction, synaptic dysfunction, cellular apoptosis, and neuronal ischemia by the passage through a damaged blood–brain barrier (BBB) of proinflammatory cytokines (such as interleukin (IL) IL6, IL1, IL8, tumor necrosis factor alpha (TNFα), and C reactive protein CRP [9]).
- Stress conditions cause neuroinflammation with the unbalance of the limbic–hypothalamic–pituitary–adrenal axis (LHPA) by increasing cortisol blood levels. Several factors can influence cortisol levels, one of them being an alteration in melatonin pathways caused by sleep deprivation [10].
- Studies have demonstrated that prolonged exposure of neurons to high levels of cortisol, insulin, and glucose leads to neuronal malfunction and damage because of continuous metabolic stress. Therefore, people develop cognitive failure, and the devastating effect is more evident in older adults in which the LHPA axis is often already dysregulated. Inflammatory conditions can lead to hyperactivation of microglia and the consequent release of inflammatory cytokines and direct neuronal damage [11].
- Abnormal gamma-aminobutyric acid (GABA)-related transmission in the nervous system actively contributes to the development of delirium. It has been largely demonstrated that the use of drugs that increase GABAergic synaptic transmission, such as benzodiazepines, increases the risk of delirium manifestation [12].
3.3. Delirium Assessment
- The mini-mental test is one of the most accurate and known cognitive tests, but is often not simple to perform.
- The four ‘A’s test (4AT) (Appendix B) is a simple, quick clinical test that requires less than 2 min to perform and is a well-validated bedside test to detect delirium in day-to-day practice and different settings [20]. It does not require special training, and it is easy to implement for delirium diagnosis. A recent article reported this test’s sensitivity and specificity as over 81.5% and 87.5%, respectively [21,22,23,24].
- The Confusion Assessment Method (CAM4) (Appendix C) was developed in 1990. It has high sensitivity (94–100%) and high specificity (90–95%), and is easy to perform [26]. Nurses and physicians can perform it, but delirium diagnosis can only be confirmed by physician experts in the field. It can be used in clinical and research settings, with expert judgment, and is helpful to avoid hypoactive delirium.
- In recent years, the CAM4 score was also adapted for intensive care units and critically ill patients. The CAM-ICU score for intensive care unit (ICU) patients (Appendix D) has a pooled sensitivity of 80.0% and a pooled specificity of 95.9% [27]. This score investigates the presence of acute onset or fluctuating course and inattention with either disorganized thinking or altered level of consciousness; these features indicate a possible delirium diagnosis [28,29]. Like the CAM4, this tool evaluates the same core features of delirium, but in a different way, with clinical tests or observations. Furthermore, this assessment needs to be combined with the Richmond Agitation–Sedation Scale to evaluate the arousal/sedation [30]. This test is helpful in conditions such as coma or arousal, which nurses can easily perform.
- The severity of delirium and the clinical course of the delirium can be measured with these tools [34,35,36]. The Delirium Rating Scale—Revised-98 and The Memorial Delirium Assessment have both been traduced in many languages, which is helpful for longitudinal studies and assessing and evaluating answers to the treatments.
- Recently, two delirium-prediction models in ICUs have been introduced: the model for delirium (PRE-DELIRIC) and the early prediction model for delirium (E-PRE-DELIRIC). In these models, the delirium prediction, as reported above, demonstrated both a moderate-to-good performance to predict delirium, especially in ICU; however, more validations are necessary [37,38,39,40]. These tools allow practicing preventive strategies to avoid delirium in critical patients.
3.4. Postoperative Delirium: Epidemiology and Risk Factors
3.5. Perioperative Management of Delirium
3.6. Therapies for Postoperative Delirium
3.6.1. Non-Pharmacological Interventions: Behavioral and Multimodal Approach
- It is necessary to understand why the patient is delirious and to treat precipitating factors (such as treating hypotension, giving oxygen therapy when needed, treating overdose of drugs, and controlling pain).
- It is fundamental to free the patient from medical devices as soon as possible. This allows starting early rehabilitation and promoting a reorientation program with the patient’s family collaboration.
- In addition, some advantages could come from educational programs for staff to illustrate how to deal with this pathology [70].
3.6.2. Pharmacological Interventions
- Haloperidol (a dopaminergic agonist) is the antipsychotic drug traditionally used in emergency intravenously in both non-intensive and intensive care settings. It seems to reduce the length of delirium and agitation. However, there are some safety issues because it can prolong QTc on ECG. In addition, there are little evidence and guidelines that support its use, with a paucity of data regarding its use in non-intensive care settings [71,72].
- An α2 agonist, dexmedetomidine, has been used in the ICU setting to treat delirium in mechanically ventilated patients. Recent guidelines suggest it helps to wean patients from ventilators by reducing ventilation days and the length of stay in the ICU. Evidence suggests that it reduces delirium in postoperative cardiovascular patients and. When haloperidol fails, it can be used in non-ventilated patients. As well as dexmedetomidine, the use of clonidine (α2 agonist) seems to be promising, but further studies are necessary to better define its role in delirium treatment [30,75,76].
4. Outcomes on Postoperative Delirium
5. The Perspectives of the Postoperative Delirium through the COVID-19 Era
Limits
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A. The Rapid Cognitive Screen Test
- −
- Name.
- −
- Age.
- −
- Date of assessment.
- −
- Is the patient alert?
- −
- Level of education.
- −
- Read each object to the patient using approximately 1 s intervals.
- ○
- ‘Please remember these five objects. I will ask you what they are later’ Apple, Pen, Tie, House, Car.’
- ○
- ‘Please repeat the objects for me.’ If the patient does not repeat all five objects correctly, repeat until all objects are recalled correctly or up to a maximum of two times. Give the patient a pencil and a blank sheet with a clock face. ‘This is a clock face. Please put in the hour markers and the time at ten minutes to eleven o’clock’.
- ○
- ‘What were the five objects I asked you to remember?’
- ○
- ‘I’m going to tell you a story. Please listen carefully because afterward, I’m going to ask you about it. Jill was a very successful stockbroker. She made a lot of money on the stock market. She then met Jack, a handsome man. She married him and had three children. They lived in Chicago. She then stopped work and stayed at home to bring up her children. When they were teenagers, she went back to work. She and Jack lived happily ever after. What state did she live in?’
Appendix B. The 4 AT: Assessment Test for Delirium and Cognitive Impairment
- −
- Normal (fully alert, but not agitated, throughout assessment). 0
- −
- Mild sleepiness for <10 s after waking, then normal. 0
- −
- Clearly abnormal. 4
- −
- No mistakes. 0
- −
- 1 mistake. 1
- −
- 2 or more mistakes/untestable. 2
- −
- Achieves 7 months or more correctly. 0
- −
- Starts but scores < 7 months/refuses to start. 1
- −
- Untestable (cannot start because unwell, drowsy, inattentive). 2
- −
- No. 0
- −
- Yes. 4
Appendix C. The CAM SCALE: Confusion Assessment Method
- −
- Name.
- −
- Age.
- −
- Date of assessment.
- −
- Acute Onset.
- ○
- Is there evidence of an acute change in mental status from the patient’s baseline?
- −
- Inattention
- ○
- Did the patient have difficulty focusing attention (for example, being easily distractible or having difficulty keeping track of what was being said)?
- ○
- Did this behavior fluctuate during the interview (that is, tend to come and go or increase and decrease in severity, if present or abnormal)?
- ○
- Please describe this behavior (if present or abnormal).
- −
- Disorganized Thinking
- ○
- Was the patient’s thinking disorganized, incoherent, such as rambling, or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable, switching from subject to subject?
- −
- Altered Level of Consciousness
- ○
- Overall, how would you rate this patient’s level of consciousness?
- −
- Disorientation
- ○
- Was the patient disoriented at any time during the interview, such as thinking that he or she was somewhere other than the hospital, using the wrong bed, or misjudging the time of day?
- −
- Memory Impairment
- ○
- Did the patient demonstrate any memory problems during the interview, such as an inability to remember events in the hospital or difficulty remembering instructions?
- −
- Perceptual Disturbances
- ○
- Did the patient have any evidence of perceptual disturbances, such as hallucinations, illusions, or misinterpretations (for example, thinking something was moving when it was not)?
- −
- Psychomotor Agitation
- ○
- At any time during the interview, did the patient have an unusually increased level of motor activity, such as restlessness, picking at bedclothes, tapping fingers, or making frequent, sudden changes in position?
- −
- Psychomotor Retardation
- ○
- At any time during the interview, did the patient have an unusually decreased level of motor activity, such as sluggishness, staring into space, staying in one position for a long time, or moving very slowly?
- −
- Altered Sleep–Wake Cycle
- ○
- Did the patient have evidence of disturbance of the sleep–wake cycle, such as excessive daytime sleepiness with insomnia at night?
Appendix D. The CAM-ICU SCALE: Confusion Assessment Method for the ICU
- −
- Name.
- −
- Age.
- −
- Date of assessment.
- −
- Acute onset or fluctuating course.
- ○
- Is the patient different from his/her baseline mental status? Alternatively, has the patient had any fluctuation in mental status in the past 24 h as evidenced by fluctuation on a sedation/level of consciousness scale (i.e., RASS/SAS), GCS, or previous delirium assessment?
- −
- Inattention
- ○
- Letters attention test. Say to the patient, ‘I am going to read you a series of 10 letters. Whenever you hear the letter ‘A’, indicate by squeezing my hand.’ Read letters from the following letter list in a normal tone 3 s apart.
- −
- Altered level of consciousness
- ○
- Present if the actual RASS score is anything other than alert and calm (zero).
- −
- Disorganized thinking
- ○
- Yes/no questions.
- Will a stone float on water?
- Are there fish in the sea?
- Does one pound weigh more than two pounds?
- Can you use a hammer to pound a nail?
‘Now do the same thing with the other hand’ (Do not repeat the number of fingers). If the patient is unable to move both arms, for the second part of the command, ask the patient to ‘Add one more finger’.
- −
- Acute onset or fluctuating course plus inattention either altered level of consciousness or disorganized thinking present = CAM-ICU positive and delirium present.
References
- Johnson, J.R. Delirium in Hospitalized Older Adults. N. Engl. J. Med. 2018, 378, 96. [Google Scholar] [CrossRef] [PubMed]
- Marcantonio, E.R. Delirium in Hospitalized Older Adults. N. Engl. J. Med. 2017, 377, 1456–1466. [Google Scholar] [CrossRef] [PubMed]
- Hshieh, T.T.; Inouye, S.K.; Oh, E.S. Delirium in the Elderly. Clin. Geriatr. Med. 2020, 36, 183–199. [Google Scholar] [CrossRef] [PubMed]
- Association, A.P. Diagnostic and Statistical Manual of Dsm-5 TM, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Maclullich, A.M.J.; Shenkin, S.D.; Goodacre, S.; Godfrey, M.; Hanley, J.; Stíobhairt, A.; Lavender, E.; Boyd, J.; Stephen, J.; Weir, C.; et al. The 4 ‘a’s test for detecting delirium in acute medical patients: A diagnostic accuracy study. Health Technol. Assess. 2019, 23, 1–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Browndyke, J.N.; Devinney, M.; Mathew, J.P. The Devil Is in the Details: Comparison of Postoperative Delirium and Neurocognitive Dysfunction. Anesthesiology 2019, 131, 456–458. [Google Scholar] [CrossRef]
- Daiello, L.A.; Racine, A.M.; Yun Gou, R.; Marcantonio, E.R.; Xie, Z.; Kunze, L.J.; Vlassakov, K.V.; Inouye, S.K.; Jones, R.N.; Alsop, D.; et al. Postoperative Delirium and Postoperative Cognitive Dysfunction: Overlap and Divergence. Anesthesiology 2019, 131, 477–491. [Google Scholar] [CrossRef] [Green Version]
- Mattison, M.L.P. Delirium. Ann. Intern. Med. 2020, 173, ITC49–ITC64. [Google Scholar] [CrossRef]
- Maldonado, J.R. Acute Brain Failure: Pathophysiology, Diagnosis, Management, and Sequelae of Delirium. Crit. Care Clin. 2017, 33, 461–519. [Google Scholar] [CrossRef]
- Wang, Y.; Shen, X. Postoperative delirium in the elderly: The potential neuropathogenesis. Aging Clin. Exp. Res. 2018, 30, 1287–1295. [Google Scholar] [CrossRef]
- Yang, T.; Velagapudi, R.; Terrando, N. Neuroinflammation after surgery: From mechanisms to therapeutic targets. Nat. Immunol. 2020, 21, 1319–1326. [Google Scholar] [CrossRef]
- Arumugam, S.; El-Menyar, A.; Al-Hassani, A.; Strandvik, G.; Asim, M.; Mekkodithal, A.; Mudali, I.; Al-Thani, H. Delirium in the Intensive Care Unit. J. Emerg. Trauma. Shock 2017, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, I.; Prabhakar, H.; Mahajan, C. Postoperative Cognitive Dysfunction. Indian J. Crit. Care Med. 2019, 23, S162. [Google Scholar] [CrossRef] [PubMed]
- Charbek, E.; Huynh, K.; Kim, E.; Nayak, R.P. Assessment of Cognitive Impairment in Patients with Chronic Obstructive Pulmonary Disease Using the Rapid Cognitive Screen. J. Nutr. Health Aging 2019, 23, 102–104. [Google Scholar] [CrossRef] [PubMed]
- Lucke, J.A.; De Gelder, J.; Heringhaus, C.; Van Der Mast, R.C.; Fogteloo, A.J.; Anten, S.; Blauw, G.J.; De Groot, B.; Mooijaart, S.P. Impaired cognition is associated with adverse outcome in older patients in the emergency department; the Acutely Presenting Older patients (APOP) study. Age Ageing 2018, 47, 679–684. [Google Scholar] [CrossRef] [Green Version]
- O’Reilly-Shah, V.N.; Hemani, S.; Davari, P.; Glowka, L.; Gebhardt, E.; Hill, L.; Lee, S.; Master, V.A.; Rodriguez, A.D.; García, P.S. A Preoperative Cognitive Screening Test Predicts Increased Length of Stay in a Frail Population: A Retrospective Case-Control Study. Anesth. Analg. 2019, 129, 1283–1290. [Google Scholar] [CrossRef]
- Amado, J.; Gago, P.; Santos, W.; Mimoso, J.; de Jesus, I. Choque cardiogénico–fármacos inotrópicos e vasopressores. Rev. Port. Cardiol. 2016, 35, 681–695. [Google Scholar] [CrossRef]
- Amado, L.A.; Perrie, H.; Scribante, J.; Ben-Israel, K.A. Preoperative cognitive dysfunction in older elective noncardiac surgical patients in South Africa. Br. J. Anaesth. 2020, 125, 275–281. [Google Scholar] [CrossRef]
- Oh, E.S.; Fong, T.G.; Hshieh, T.T.; Inouye, S.K. Delirium in Older Persons: Advances in Diagnosis and Treatment. JAMA 2017, 318, 1161–1174. [Google Scholar] [CrossRef]
- Shenkin, S.D.; Fox, C.; Godfrey, M.; Siddiqi, N.; Goodacre, S.; Young, J.; Anand, A.; Gray, A.; Hanley, J.; MacRaild, A.; et al. Delirium detection in older acute medical inpatients: A multicentre prospective comparative diagnostic test accuracy study of the 4AT and the confusion assessment method. BMC Med. 2019, 17, 138. [Google Scholar] [CrossRef] [Green Version]
- Jeong, E.; Park, J.; Lee, J. Diagnostic test accuracy of the Nursing Delirium Screening Scale: A systematic review and meta-analysis. J. Adv. Nurs. 2020, 76, 2510–2521. [Google Scholar] [CrossRef]
- Jeong, E.; Park, J.; Lee, J. Diagnostic Test Accuracy of the 4AT for Delirium Detection: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7515. [Google Scholar] [CrossRef] [PubMed]
- Myrstad, M.; Kuwelker, K.; Haakonsen, S.; Valebjørg, T.; Langeland, N.; Kittang, B.R.; Hagberg, G.; Neerland, B.E.; Bakken, M.S. Delirium screening with 4AT in patients aged 65 years and older admitted to the Emergency Department with suspected sepsis: A prospective cohort study. Eur. Geriatr. Med. 2021. epub ahead of print. [Google Scholar] [CrossRef]
- Tieges, Z.; Maclullich, A.M.J.; Anand, A.; Brookes, C.; Cassarino, M.; O’connor, M.; Ryan, D.; Saller, T.; Arora, R.C.; Chang, Y.; et al. Diagnostic accuracy of the 4AT for delirium detection in older adults: Systematic review and meta-analysis. Age Ageing 2021, 50, 733–743. [Google Scholar] [CrossRef] [PubMed]
- 4AT-Rapid Clinical Test for Delirium. Available online: https://www.the4at.com/ (accessed on 28 November 2021).
- Chaiwat, O.; Chanidnuan, M.; Pancharoen, W.; Vijitmala, K.; Danpornprasert, P.; Toadithep, P.; Thanakiattiwibun, C. Postoperative delirium in critically ill surgical patients: Incidence, risk factors, and predictive scores. BMC Anesthesiol. 2019, 19, 39. [Google Scholar] [CrossRef] [Green Version]
- Kotfis, K.; Marra, A.; Wesley Ely, E. ICU delirium—A diagnostic and therapeutic challenge in the intensive care unit. Anaesthesiol. Intensive Ther. 2018, 50, 128–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krewulak, K.D.; Rosgen, B.K.; Ely, E.W.; Stelfox, H.T.; Fiest, K.M. The CAM-ICU-7 and ICDSC as measures of delirium severity in critically ill adult patients. PLoS ONE 2020, 15, e0242378. [Google Scholar] [CrossRef]
- Riker, R.R.; Fraser, G.L. Delirium-Beyond the CAM-ICU. Crit. Care Med. 2020, 48, 134–136. [Google Scholar] [CrossRef]
- Pop, M.K.; Dervay, K.R.; Dansby, M.; Jones, C. Evaluation of Richmond Agitation Sedation Scale (RASS) in Mechanically Ventilated in the Emergency Department. Adv. Emerg. Nurs. J. 2018, 40, 131–137. [Google Scholar] [CrossRef]
- Krewulak, K.D.; Hiploylee, C.; Ely, E.W.; Stelfox, H.T.; Inouye, S.K.; Fiest, K.M. Adaptation and Validation of a Chart-Based Delirium Detection Tool for the ICU (CHART-DEL-ICU). J. Am. Geriatr. Soc. 2021, 69, 1027–1034. [Google Scholar] [CrossRef]
- Wang, C.; Qin, Y.; Wan, X.; Song, L.; Li, Z.; Li, H. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J. Orthop. Surg. Res. 2018, 13, 186. [Google Scholar] [CrossRef] [Green Version]
- Shi, Z.; Wu, Y.; Li, C.; Fu, S.; Li, G.; Zhu, Y.; Swain, C.A.; Marcantonio, E.R.; Xie, Z.; Shen, Y. Using the Chinese version of Memorial Delirium Assessment Scale to describe postoperative delirium after hip surgery. Front. Aging Neurosci. 2014, 6, 297. [Google Scholar] [CrossRef] [PubMed]
- Noh, G.; Kwon, I.; Lee, M.; Ahn, S.H.; Kim, J.L. Factor Analysis of Delirium in Elderly, Using the Korean Version of Delirium Rating Scale-Revised-98. Psychiatry Investig. 2018, 15, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Grover, S.; Ghosh, A.; Sarkar, S.; Desouza, A.; Yaddanapudi, L.N.; Basu, D. Delirium in Intensive Care Unit: Phenomenology, Subtypes, and Factor Structure of Symptoms. Indian J. Psychol. Med. 2018, 40, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Malhotra, S.; Grover, S.; Jindal, S.K. Symptom profile as assessed on delirium rating scale-revised-98 of delirium in respiratory intensive care unit: A study from India. Lung India 2017, 34, 434–440. [Google Scholar] [CrossRef]
- Wassenaar, A.; Schoonhoven, L.; Devlin, J.W.; van Haren, F.M.P.; Slooter, A.J.C.; Jorens, P.G.; van der Jagt, M.; Simons, K.S.; Egerod, I.; Burry, L.D.; et al. External Validation of Two Models to Predict Delirium in Critically Ill Adults Using Either the Confusion Assessment Method-ICU or the Intensive Care Delirium Screening Checklist for Delirium Assessment. Crit. Care Med. 2019, 47, e827–e835. [Google Scholar] [CrossRef]
- Wassenaar, A.; Schoonhoven, L.; Devlin, J.W.; van Haren, F.M.P.; Slooter, A.J.C.; Jorens, P.G.; van der Jagt, M.; Simons, K.S.; Egerod, I.; Burry, L.D.; et al. Delirium prediction in the intensive care unit: Comparison of two delirium prediction models. Crit. Care 2018, 22, 114. [Google Scholar] [CrossRef]
- Chen, T.J.; Chung, Y.W.; Chang, H.C.; Chen, P.Y.; Wu, C.R.; Hsieh, S.H.; Chiu, H.Y. Diagnostic accuracy of the CAM-ICU and ICDSC in detecting intensive care unit delirium: A bivariate meta-analysis. Int. J. Nurs. Stud. 2021, 113, 103782. [Google Scholar] [CrossRef]
- Ho, M.H.; Shen, S.T.H. Application of the delirium risk prediction model in the TED ICU smart intensive care system during the current COVID-19 pandemic. Intensive Crit. Care Nurs. 2021, 63, 103007. [Google Scholar] [CrossRef]
- Wildes, T.S.; Mickle, A.M.; Abdallah, A.B.; Maybrier, H.R.; Oberhaus, J.; Budelier, T.P.; Kronzer, A.; McKinnon, S.L.; Park, D.; Torres, B.A.; et al. Effect of electroencephalography-guided anesthetic administration on postoperative delirium among older adults undergoing major surgery the engages randomized clinical trial. JAMA-J. Am. Med. Assoc. 2019, 321, 473–483. [Google Scholar] [CrossRef] [Green Version]
- Wildes, T.S.; Winter, A.C.; Maybrier, H.R.; Mickle, A.M.; Lenze, E.J.; Stark, S.; Lin, N.; Inouye, S.K.; Schmitt, E.M.; McKinnon, S.L.; et al. Protocol for the Electroencephalography Guidance of Anesthesia to Alleviate Geriatric Syndromes (ENGAGES) study: A pragmatic, randomised clinical trial. BMJ Open 2016, 6, e011505. [Google Scholar] [CrossRef]
- Punjasawadwong, Y.; Chau-in, W.; Laopaiboon, M.; Punjasawadwong, S.; Pin-on, P. Processed electroencephalogram and evoked potential techniques for amelioration of postoperative delirium and cognitive dysfunction following non-cardiac and non-neurosurgical procedures in adults. Cochrane Database Syst. Rev. 2018, 2018, 1465–1858. [Google Scholar] [CrossRef] [PubMed]
- Dunne, S.S.; Coffey, J.C.; Konje, S.; Gasior, S.; Clancy, C.C.; Gulati, G.; Meagher, D.; Dunne, C.P. Biomarkers in delirium: A systematic review. J. Psychosom. Res. 2021, 147, 110530. [Google Scholar] [CrossRef] [PubMed]
- Wilson, J.E.; Mart, M.F.; Cunningham, C.; Shehabi, Y.; Girard, T.D.; MacLullich, A.M.J.; Slooter, A.J.C.; Ely, E.W. Delirium. Nat. Rev. Dis. Prim. 2020, 6, 90. [Google Scholar] [CrossRef] [PubMed]
- Slooter, A.J.C.; Van De Leur, R.R.; Zaal, I.J. Delirium in critically ill patients. Handb. Clin. Neurol. 2017, 141, 449–466. [Google Scholar] [CrossRef] [PubMed]
- Folbert, E.C.; Hegeman, J.H.; Gierveld, R.; van Netten, J.J.; van der Velde, D.; Ten Duis, H.J.; Slaets, J.P. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch. Orthop. Trauma Surg. 2017, 137, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.P.; Jing, Z.Z.; Song, J.F.; Zhang, P. A retrospective study on risk factors associated with postoperative delirium in elderly patients with spinal operation. Zhongguo Gu Shang 2019, 32, 549–554. [Google Scholar] [CrossRef]
- Pérez-Ros, P.; Martínez-Arnau, F.M.; Baixauli-Alacreu, S.; Caballero-Pérez, M.; García-Gollarte, J.F.; Tarazona-Santabalbina, F. Delirium Predisposing and Triggering Factors in Nursing Home Residents: A Cohort Trial-Nested Case-Control Study. J. Alzheimers. Dis. 2019, 70, 1113–1122. [Google Scholar] [CrossRef]
- Seiler, A.; Blum, D.; Deuel, J.W.; Hertler, C.; Schettle, M.; Zipser, C.M.; Ernst, J.; Schubert, M.; Von Känel, R.; Boettger, S. Delirium is associated with an increased morbidity and in-hospital mortality in cancer patients: Results from a prospective cohort study. Palliat. Support. Care 2021, 19, 294–303. [Google Scholar] [CrossRef]
- Zhang, X.; Yang, J.; Chen, X.; Du, L.; Li, K.; Zhou, Y. Enhanced recovery after surgery on multiple clinical outcomes: Umbrella review of systematic reviews and meta-analyses. Medicine 2020, 99, e20983. [Google Scholar] [CrossRef]
- Monacelli, F.; Signori, A.; Prefumo, M.; Giannotti, C.; Nencioni, A.; Romairone, E.; Scabini, S.; Odetti, P. Delirium, Frailty, and Fast-Track Surgery in Oncogeriatrics: Is There a Link? Dement. Geriatr. Cogn. Dis. Extra 2018, 8, 33–41. [Google Scholar] [CrossRef]
- Golder, H.J.; Papalois, V. Enhanced Recovery after Surgery: History, Key Advancements and Developments in Transplant Surgery. J. Clin. Med. 2021, 10, 1634. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.C.; Tseng, P.T.; Tu, Y.K.; Hsu, C.Y.; Liang, C.S.; Yeh, T.C.; Chen, T.Y.; Chu, C.S.; Matsuoka, Y.J.; Stubbs, B.; et al. Association of Delirium Response and Safety of Pharmacological Interventions for the Management and Prevention of Delirium: A Network Meta-analysis. JAMA Psychiatry 2019, 76, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zhao, X.; Dong, T.; Yang, Z.; Zhang, Q.; Zhang, Y. Risk factors for postoperative delirium following hip fracture repair in elderly patients: A systematic review and meta-analysis. Aging Clin. Exp. Res. 2017, 29, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Melegari, G.; Albertini, G.; Romani, A.; Malaguti, S.; Traccitto, F.; Giuliani, E.; Cavallini, G.M.; Bertellini, E.; Barbieri, A. Why should you stay one night? Prospective observational study of enhanced recovery in elderly patients. Aging Clin. Exp. Res. 2020, 33, 1955–1961. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Hu, J.; Ma, D. Postoperative delirium: Perioperative assessment, risk reduction, and management. Br. J. Anaesth. 2020, 125, 492–504. [Google Scholar] [CrossRef]
- Miller, D.; Lewis, S.R.; Pritchard, M.W.; Schofield-Robinson, O.J.; Shelton, C.L.; Alderson, P.; Smith, A.F. Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non-cardiac surgery. Cochrane Database Syst. Rev. 2018, 8, 1465–1858. [Google Scholar] [CrossRef] [PubMed]
- Ishii, K.; Makita, T.; Yamashita, H.; Matsunaga, S.; Akiyama, D.; Toba, K.; Hara, K.; Sumikawa, K.; Hara, T. Total intravenous anesthesia with propofol is associated with a lower rate of postoperative delirium in comparison with sevoflurane anesthesia in elderly patients. J. Clin. Anesth. 2016, 33, 428–431. [Google Scholar] [CrossRef]
- Kinjo, S.; Lim, E.; Magsaysay, M.V.; Sands, L.P.; Leung, J.M. Volatile anaesthetics and postoperative delirium in older surgical patients-A secondary analysis of prospective cohort studies. Acta Anaesthesiol. Scand. 2019, 63, 18–26. [Google Scholar] [CrossRef]
- Shaefi, S.; Shankar, P.; Mueller, A.L.; O’Gara, B.P.; Spear, K.; Khabbaz, K.R.; Bagchi, A.; Chu, L.M.; Banner-Goodspeed, V.; Leaf, D.E.; et al. Intraoperative Oxygen Concentration and Neurocognition after Cardiac Surgery. Anesthesiology 2021, 134, 189–201. [Google Scholar] [CrossRef]
- Shaefi, S.; Marcantonio, E.R.; Mueller, A.; Banner-Goodspeed, V.; Robson, S.C.; Spear, K.; Otterbein, L.E.; O’Gara, B.P.; Talmor, D.S.; Subramaniam, B. Intraoperative oxygen concentration and neurocognition after cardiac surgery: Study protocol for a randomized controlled trial. Trials 2017, 18, 600. [Google Scholar] [CrossRef] [Green Version]
- Leenders, J.; Overdevest, E.; van Straten, B.; Golab, H. The influence of oxygen delivery during cardiopulmonary bypass on the incidence of delirium in CABG patients; a retrospective study. Perfusion 2018, 33, 656–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janssen, T.L.; Alberts, A.R.; Hooft, L.; Mattace-Raso, F.U.S.; Mosk, C.A.; Van Der Laan, L. Prevention of postoperative delirium in elderly patients planned for elective surgery: Systematic review and meta-analysis. Clin. Interv. Aging 2019, 14, 1095–1117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rains, J.; Chee, N. The role of occupational and physiotherapy in multi-modal approach to tackling delirium in the intensive care. J. Intensive Care Soc. 2017, 18, 318–322. [Google Scholar] [CrossRef] [PubMed]
- Simons, K.S.; Laheij, R.J.F.; van den Boogaard, M.; Moviat, M.A.M.; Paling, A.J.; Polderman, F.N.; Rozendaal, F.W.; Salet, G.A.M.; van der Hoeven, J.G.; Pickkers, P.; et al. Dynamic light application therapy to reduce the incidence and duration of delirium in intensive-care patients: A randomised controlled trial. Lancet. Respir. Med. 2016, 4, 194–202. [Google Scholar] [CrossRef]
- Soiza, R.L.; Myint, P.K. The Scottish Intercollegiate Guidelines Network (SIGN) 157: Guidelines on Risk Reduction and Management of Delirium. Medicina 2019, 55, 491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Méndez-Martínez, C.; Fernández-Martínez, M.N.; García-Suárez, M.; Martínez-Isasi, S.; Fernández-Fernández, J.A.; Fernández-García, D. Related Factors and Treatment of Postoperative Delirium in Old Adult Patients: An Integrative Review. Healthcare 2021, 9, 1103. [Google Scholar] [CrossRef]
- Ludolph, P.; Stoffers-Winterling, J.; Kunzler, A.M.; Rösch, R.; Geschke, K.; Vahl, C.F.; Lieb, K. Non-Pharmacologic Multicomponent Interventions Preventing Delirium in Hospitalized People. J. Am. Geriatr. Soc. 2020, 68, 1864–1871. [Google Scholar] [CrossRef]
- Enomoto, K.; Kosaka, S.; Kimura, T.; Matsubara, M.; Kitada, Y.; Mieno, M.; Okamura, H. Prevention of postoperative delirium after cardiovascular surgery: A team-based approach. J. Thorac. Cardiovasc. Surg. 2021, 24, in press. [Google Scholar] [CrossRef]
- Rood, P.J.T.; Zegers, M.; Slooter, A.J.C.; Beishuizen, A.; Simons, K.S.; van der Voort, P.H.J.; van der Woude, M.C.E.; Spronk, P.E.; van der Hoeven, J.G.; Pickkers, P.; et al. Prophylactic Haloperidol Effects on Long-term Quality of Life in Critically Ill Patients at High Risk for Delirium: Results of the REDUCE Study. Anesthesiology 2019, 131, 328–335. [Google Scholar] [CrossRef]
- Duprey, M.S.; Devlin, J.W.; Der Hoeven, J.G.V.; Pickkers, P.; Briesacher, B.A.; Saczynski, J.S.; Griffith, J.L.; Boogaard, M. Van Den Association between Incident Delirium Treatment with Haloperidol and Mortality in Critically Ill Adults. Crit. Care Med. 2021, 1303–1311. [Google Scholar] [CrossRef]
- Devlin, J.W.; Skrobik, Y. Antipsychotics for the prevention and treatment of delirium in the intensive care unit: What is their role? Harv. Rev. Psychiatry 2011, 19, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Neufeld, K.J.; Yue, J.; Robinson, T.N.; Inouye, S.K.; Needham, D.M. Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalized Adults: A Systematic Review and Meta-Analysis. J. Am. Geriatr. Soc. 2016, 64, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Frölich, M.A.; Banks, C.; Ness, T.J. The effect of sedation on cortical activation: A randomized study comparing the effects of sedation with midazolam, propofol, and dexmedetomidine on auditory processing. Anesth. Analg. 2017, 124, 1603–1610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soltani, F.; Tabatabaei, S.; Jannatmakan, F.; Nasajian, N.; Amiri, F.; Darkhor, R.; Moravej, M. Comparison of the Effects of Haloperidol and Dexmedetomidine on Delirium and Agitation in Patients with a Traumatic Brain Injury Admitted to the Intensive Care Unit. Anesthesiol. Pain Med. 2021, 11, e113802. [Google Scholar] [CrossRef]
- Dawson, A.H.; Buckley, N.A. Pharmacological management of anticholinergic delirium—Theory, evidence and practice. Br. J. Clin. Pharmacol. 2016, 81, 516–524. [Google Scholar] [CrossRef] [Green Version]
- Alagiakrishnan, K. Melatonin based therapies for delirium and dementia. Discov. Med. 2016, 21, 363–371. [Google Scholar]
- Robinson, T.N.; Kovar, A.; Carmichael, H.; Overbey, D.M.; Goode, C.M.; Jones, T.S. Postoperative delirium is associated with decreased recovery of ambulation one-month after surgery. Am. J. Surg. 2021, 221, 856–861. [Google Scholar] [CrossRef]
- Austin, C.A.; O’Gorman, T.; Stern, E.; Emmett, D.; Stürmer, T.; Carson, S.; Busby-Whitehead, J. Association between postoperative delirium and long-term cognitive function after major nonemergent surgery. JAMA Surg. 2019, 154, 328–334. [Google Scholar] [CrossRef]
- Park, E.A.; Kim, M.Y. Postoperative Delirium is Associated with Negative Outcomes and Long-Term Mortality in Elderly Koreans: A Retrospective Observational Study. Medicina 2019, 55, 618. [Google Scholar] [CrossRef] [Green Version]
- Epstein, D.; Diu, E.; Abeysekera, T.; Kam, D.; Chan, Y. Review of non-convulsive status epilepticus and an illustrative case history manifesting as delirium. Australas. J. Ageing 2009, 28, 110–115. [Google Scholar] [CrossRef]
- Woodford, H.J.; George, J.; Jackson, M. Non-convulsive status epilepticus: A practical approach to diagnosis in confused older people. Postgrad. Med. J. 2015, 91, 655–661. [Google Scholar] [CrossRef]
- Melegari, G.; Rivi, V.; Zelent, G.; Nasillo, V.; De Santis, E.; Melegari, A.; Bevilacqua, C.; Zoli, M.; Meletti, S.; Barbieri, A. Mild to Severe Neurological Manifestations of COVID-19: Cases Reports. Int. J. Environ. Res. Public Health 2021, 18, 3673. [Google Scholar] [CrossRef] [PubMed]
- Fabrazzo, M.; Russo, A.; Camerlengo, A.; Tucci, C.; Luciano, M.; De Santis, V.; Perris, F.; Catapano, F.; Coppola, N. Delirium and Cognitive Impairment as Predisposing Factors of COVID-19 Infection in Neuropsychiatric Patients: A Narrative Review. Medicina 2021, 57, 1244. [Google Scholar] [CrossRef] [PubMed]
- Rivi, V.; Melegari, G.; Blom, J.M.C. How to humanise the COVID-19 intensive care units. BMJ Evidence-Based Med. 2021, 26, 141–142. [Google Scholar] [CrossRef] [PubMed]
| Categories of Risk | Factors |
|---|---|
| Predisposing factors | Age > 65 years Male gender Low autonomy in daily activities Low educational level History of alcohol abuse Illicit drug use Pre-existing neurological and cognitive impairments (dementia) Comorbidities and pre-existing organ failures High critical prognostic score at the hospital admission Sepsis or septic shock Stroke Trauma Frailty Visual and hearing impairment Depression Poor nutrition, dehydration, electrolyte unbalance Endocrinopathies History of delirium Use of predisposing drugs Impairment in oxygenation (anemia, anoxic/hypoxic state, low organs perfusion) |
| Precipitant factors | Surgery (especially if emergency and high-risk) Sedation or general anesthesia Mechanical ventilation > 96 h Psychoactive drugs (benzodiazepines, opiates plus corticosteroids, dihydropyridinic drugs, antihistamines) Sepsis or septic shock Stroke Dehydration or electrolyte unbalance Uncontrolled pain Invasive devices on the body Immobility Circadian rhythm alterations Psychological stress Isolation |
| Timing of Action | Strategies |
|---|---|
| Preoperative | Daily evaluation of clinical conditions Consider predisposing and precipitant factors (if possible, treat them) Preoperative geriatric consult Evaluate surgery and anesthetic risk |
| Intraoperative | Prefer total intravenous anesthesia to inhalational anesthesia Choose desflurane over other inhalational agents Avoid drugs that facilitate postoperative delirium (benzodiazepines) Maintain normoxia during surgery and normal DO2 Reduce blood loss Maintain the normal level of hemoglobin Monitor anesthesia depth with BIS or EEG (>60-year-old, surgery lasts > 1 h) |
| Postoperative | Early physical rehabilitation Early mental activities Reorientation in usual life routine (presence of patient’s family, familiar objects nearby) Supplying patient’s daily prosthesis Listening to music Promote the normal circadian rhythm (reduce night exposure to lights, noises with the help of earplugs, incremental exposure to light daily, reduce medications and interventions at night, facilitate single-room bed rest, administer melatonin agonist) Remove invasive and non-invasive medical devices as soon as possible Avoid physical restraints |
| Steps to Detect and Manage | Actions |
|---|---|
| Wards strategies | Implement cognitive screening as soon as possible Monitor delirium (5 points of DSM-5 definitions, Mini-Mental State Evaluation, Rapid Cognitive Screen, 4A test, CAM4 Scale, CAM-ICU) Optimization environment (family support, reorientation programs, maintain a circadian rhythm, communication with the patient) |
| Optimize perioperative settings | Avoid/treat infections Maintain physiological DO2 oxygenation, glycemia, hydro-electrolytic balance, and physiological functions Treat pain Accurately select drugs and avoid benzodiazepines Prefer intravenous anesthesia Monitor anesthesia’s depth EEG monitoring |
| Treatment | First-line treatment: behavioural and multimodal approach (rapid rehabilitation, remove medical devices, reduce ward transfers, reorientation programs, family support, maintain the circadian rhythm, communication with patients) Second-line treatment: drugs (haloperidol, α2 agonists such as dexmedetomidine/clonidine, melatonin, acetylcholinesterase inhibitors) |
| Continuous postoperative follow up |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melegari, G.; Gaspari, A.; Gualdi, E.; Zoli, M.; Meletti, S.; Barbieri, A. Delirium in Older Adults: What a Surgeon Needs to Know. Surgeries 2022, 3, 28-43. https://doi.org/10.3390/surgeries3010006
Melegari G, Gaspari A, Gualdi E, Zoli M, Meletti S, Barbieri A. Delirium in Older Adults: What a Surgeon Needs to Know. Surgeries. 2022; 3(1):28-43. https://doi.org/10.3390/surgeries3010006
Chicago/Turabian StyleMelegari, Gabriele, Arianna Gaspari, Eugenia Gualdi, Michele Zoli, Stefano Meletti, and Alberto Barbieri. 2022. "Delirium in Older Adults: What a Surgeon Needs to Know" Surgeries 3, no. 1: 28-43. https://doi.org/10.3390/surgeries3010006
APA StyleMelegari, G., Gaspari, A., Gualdi, E., Zoli, M., Meletti, S., & Barbieri, A. (2022). Delirium in Older Adults: What a Surgeon Needs to Know. Surgeries, 3(1), 28-43. https://doi.org/10.3390/surgeries3010006






