Experiences of the Bariatric Pre-Surgery Evaluation Process in a National Health Service—An Interpretative Phenomenological Analysis
Abstract
:1. Introduction
1.1. Expectations of Bariatric Surgery
1.2. Pre-Surgery Evaluation and Candidate Selection Process
1.3. Study Rationale, Aims, and Research Questions
- -
- What are participants’ understanding and expectations of the bariatric PSE process?
- -
- What are participants’ experiences of the bariatric PSE process?
- -
- What are participants’ coping strategies for dealing with the bariatric PSE process?
2. Materials and Methods
2.1. Design, Study Population, and Data Collection
2.2. Data Analysis and Rigour
2.3. Service User Involvement
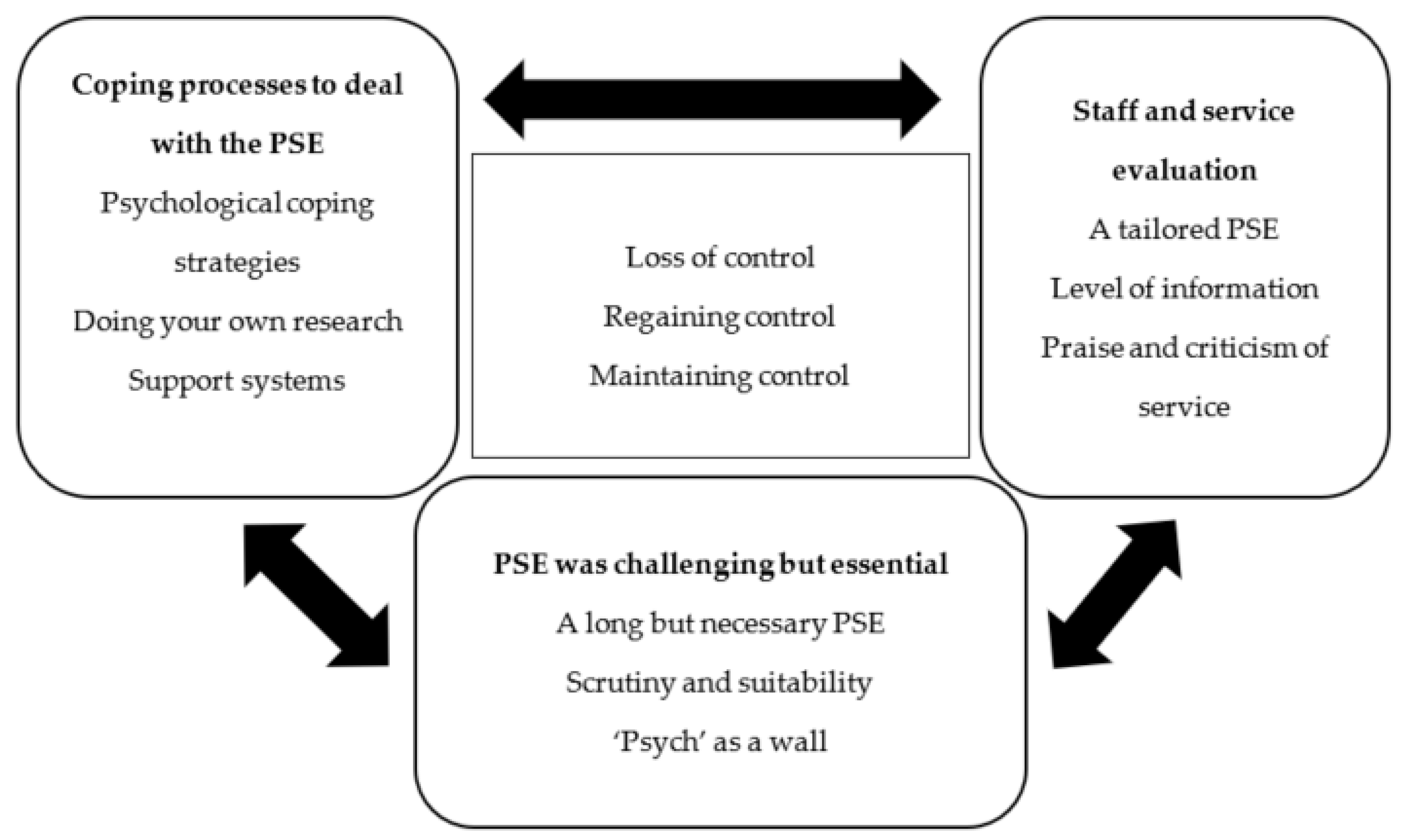
3. Analysis
3.1. Superordinate Theme One—‘PSE Was Challenging but Essential’
3.1.1. A Long but Necessary PSE: ’It Could Be Shorter, but It Gives You Time to Reflect…’
‘To put it in perspective, a good friend of mine she’s gone and have the surgery done privately… and the difference is hers was rushed, she made the decision within a week. […] although mine’s been longer than normal because we’ve had hiccups along the way… I think that were it longer process it allows you to absorb what you going to embark on and what you’re going to have done.’—George
‘[I was told] I’ve been taken off the whole system, […] when I last saw the surgeon, I got an OK, […]. So, it was waste of travel going down there, and then have to wait months to see her again […], it was like a stressful time for me, and, I was like comfort eater, so I had put on a lot of weight during that period […]. I was really depressed because I just thought didn’t know I was coming or going, I’d waited so long, I was just thinking, this whole process is pointless because I’m waiting like 3 years at the time […] and I don’t think I’ll be having this surgery’—Sabina
3.1.2. Scrutiny and Suitability: ‘They Properly Grilled Me’
‘there was an idea that you couldn’t put on weight… that if you were gaining weight then that could go against you so it was… […] and that was a fear’—George
‘I was expecting to go and be grilled on what you eating which is why I had my Slimming World book proof, ‘this is what I’m eating, I keep food diaries’ and they were like, ‘have you been honest?’ and I was like, ‘yes because you can see on that day I ate like a horse’—George
‘I would have to prove I can lose weight and keep off for a certain amount of time… […] aaand work out… […] I was very stressed because I didn’t know how I was going to keep my weight off’—Sabina
‘I was feeling a lot down, because again I was thinking I’m not going to get the surgery. And then, that spirals into putting on weight, so yeah it did affect my life a lot.’—Sabina
‘I was a bit cross [at the time] cuz they were taking something else away from me [food, alcohol…]. And I had to go through this whole thing about what’s left. […] I still went in for the operation cuz it was last chance to live. […] There was the light at the end of the tunnel, so I did toe the line. […] I’ve [now] got a positive attitude towards [PSE] because my life has changed massively.’—Rachel
3.1.3. ‘Psych’ as a Wall: They Can Make-or-Break Surgery
‘I was told that the psychiatrist… that was quite an important meeting because they would kind of the ones that would also sign off to say yes […]. As I said I think I was just worried that that was the [‘psych’] appointment that could make-or-break it.’—George
‘Seeing the psychiatrist, I was really stressed, and really down because I was thinking, ‘what is she going to say, she must be a wall… refuse me for surgery. […] I think just kind of went there knowing… what I was going say and what I wasn’t going to say [because of] fear of her saying no’—Sabina
3.2. Superordinate Theme Two: ‘Coping Processes to Deal with the PSE’
3.2.1. Psychological Coping Strategies: ‘Is It a Case of Going through the Motions?’
‘it was a case of going through the motions on… going through admin on that team […but] If I had to go through the psychologist there, it would been a lip-service/me getting very angry […]’—Holly
‘I toed the line because I knew if I stepped out of that line, I would end up being at back of the queue. […] I felt like I’d been singled out to jump through these hoops, and not everybody else […]. And I passed all the hoops that I had to jump through—Rachel
‘I think that if I were had went in there still saying that I was gonna get to a size 10, they would’ve refused me’—Sabina
3.2.2. Doing Your Own Research: ‘Or You Won’t Be Successful’
‘I don’t think they’re going to have as much success as the people that do the research, their own research for their own questions, and go into it with their eyes wide open… […] I also think each person needs to get it sorted within enough research. I think we need to take control of our destiny and not be led by doctors who think they’re very clever. […] I don’t think the information that I hear from [HPs] is adequate to make a decision’—Holly
‘but yeah it was definitely the support group, it was like, I’ve got this appointment coming up, what should I expect? what question do they going to ask? how long is the appointment going to last? things like that’—George
3.2.3. Support Systems: ‘You’re Kinda on Your Own without a Support Network’
‘The consultants… I got what I eventually expected [i.e., standards of care], which was a knowledgeable person would listen to my individual concerns and… fight my corner for me’—Holly
‘[The psychological evaluation] was a one-off evaluation […] so I had to do something myself to make sure that I will be okay after surgery’—Sabina
‘it doesn’t matter if you don’t get to the crux of why you overeat, operation or not operation, that is still gonna be there. And you’ll still gonna want it. And if you can’t have [food] when you really want it that’s gonna add you more problems than before, so that has to all be straightened out first.’—Rachel
So, if you don’t have a support network at home… you’re kind of on your own’—George
‘if they [family and friends] haven’t gone through it… they don’t appreciate or understand what you’re going through. Whereas people at the support group do. […] I mean even now post-surgery that support group is a mechanism’—George
3.2.4. Past Experiences Influencing Current Perspectives
‘medical professionals that I’ve seen over the years have been very quick to judge that I am the size I am because I’m lazy, I eat too much, and things like that […] I think it’s being prejudged… […] it was having those prejudgments already made.’—George
‘I think it’s just through a life of some particular hard knocks that… […] some incidents happened when I was at work not long before I had the surgery… made me into a ‘don’t mess with me’ type of the person. […]’—Holly
‘because I had lost weight before but I still was very depressed, so I knew that I had to [seek psychological therapy]. So I prepared in that way’—Sabina
3.2.5. Self-Perception: ‘Psychological Functioning and the Need for Psychological Input’
‘I… am of the opinion I’m fairly well enough to stand on my own two feet, and don’t need my head examined. So while some people are blubbery and use food as a tool, I did, started BS to try and buy myself time for my diabetes […] So, the whole morals of why you comfort eat and all the rest of it, I did not think applied to me’—Holly
‘after when I saw that psychiatrist I said to her even in that meeting I’m going to see someone [referring to a mental-HP] on a regular basis because I knew that was paramount for me’—Sabina
‘But I think a lot of it also stems from me being so unhappy about the size I am. Because now, I’m so much happier person. […]. I understand myself a lot more going through this process.’—Rachel
3.3. Superordinate Theme Three: ‘Staff and Service Evaluation’
3.3.1. A Tailored PSE: ‘Everybody Is Different’
‘everybody is different. You also learn along the way that… this operation has an effect on an individual person that is not known until you’ve had the operation. […] as I was an older person, I feel that that wasn’t such a big decision as a person saying in the 30 s, because that’s a hell of a lot longer, you have to have these life changing things for than I do’—Rachel
“And again I think that need to be looked at an early stage because it is a lifestyle change’—George
‘There needs to be a fast track for people like me and that are very strong emotionally and is clear and logical’—Holly
3.3.2. Level of Information
‘I think that they need to have like a booklet or something, or even if they did like a video, and it’s on their public page, even if its private or NHS and it’s on their page to explain each tier and what they expect of the patient, so people aren’t in the dark, and they don’t know what the next steps are and what is going to happen after surgery…’—Sabina
‘I think I would’ve coped further in the beginning, […], if I’d have been given a schedule. […] I was working blind I didn’t know any of that. If I would’ve know that… [long waiting] I would have been a bit more prepared for that. I found all that a little bit shocking [laughing]’—Rachel
‘on the Facebook group [for the Support group] there’s people now as I said that are questioning what to expect and those of us that had it done we then go on and put, ‘this is our experience, what they asked, what they’re likely to cover’—George
‘I didn’t expect to get so much information, like meetings about pre-op, and after the op, so I could be, once I got to that stage, I was mentally much more prepared and ready for my operation’—Rachel
3.3.3. Praise and Criticism of the Service
‘I kind of feel the dietitian, she wasn’t sympathetic […] she kept telling me, you’re not going to meet this goal and you’ll never get there, and so there is something in my notes that says, this patient thinks that she will get to a UK dress size 10, but I’ve explained to her that this is unrealistic, and then, that went to [the MDT]. So, [the ‘psych’] had discussed it with me as well, saying, do you still think that you’re going to get to a size 10, this is unrealistic […] But she was wrong because I’ve lost more than that!’—Sabina
‘I mean I feel like I owe lot to Wallace because obviously what they’ve given me […] so by giving something back, I make an effort to go to the support groups […] to kind of show them and to say thank you to Wallace’s cuz I appreciate what they’ve done for me’—George
‘Well I think my role, is why I go to the support group, is to help others’—Rachel
4. Discussion
4.1. Summary of Main Findings
4.2. Strengths and Limitations
4.3. Themes within the Wider Context
4.4. Future Research and Clinical Implication
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Institute for Care and Excellence. Obesity: Identification, Assessment and Management (Publication No. CG189). 2014. Available online: https://www.nice.org.uk/guidance/cg189 (accessed on 13 May 2021).
- Chang, S.-H.; Stoll, C.R.T.; Song, J.; Varela, J.E.; Eagon, C.J. Colditz, G.A. The Effectiveness and Risks of Bariatric Surgery: An Updated Systematic Review and Meta-analysis, 2003–2012. JAMA Surg. 2014, 149, 275. [Google Scholar] [CrossRef] [Green Version]
- Colquitt, J.L.; Picot, J.; Loveman, E.; Clegg, A.J. Surgery for obesity. In Cochrane Database of Systematic Reviews; The Cochrane Collaboration, Ed.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2009; p. CD003641. [Google Scholar] [CrossRef]
- Gulliford, M.C.; Charlton, J.; Booth, H.P.; Fildes, A.; Khan, O.; Reddy, M.; Ashworth, M.; Littlejohns, P.; Prevost, A.T.; Rudisill, C. Costs and outcomes of increasing access to bariatric surgery for obesity: Cohort study and cost-effectiveness analysis using electronic health records. Health Serv. Deliv. Res. 2016, 4, 1–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Bariatric Surgery Registry Data Committee (NBCR). The United Kingdom National Bariatric Surgery Registry of the British Obesity and Metabolic Surgery Society: Second Registry Report; Dendrite Clinical Systems Ltd.: Reading, UK, 2014. [Google Scholar]
- Sjöström, L.; Lindroos, A.K.; Peltonen, M.; Torgerson, J.; Bouchard, C.; Carlsson, B.; Dahlgren, S.; Larsson, B.; Narbro, K.; Sjöström, C.D.; et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N. Engl. J. Med. 2004, 351, 2683–2693. [Google Scholar] [CrossRef]
- Buchwald, H.; Oien, D.M. Metabolic/bariatric surgery Worldwide 2008. Obes. Surg. 2009, 19, 1605–1611. [Google Scholar] [CrossRef] [PubMed]
- Keidar, A.; Szold, A.; Carmon, E.; Blanc, A.; Abu-Abeid, S. Band slippage after laparoscopic adjustable gastric banding: Etiology and treatment. Surg. Endosc. 2005, 19, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Dimitriadis, G.K.; Randeva, M.S.; Miras, A.D. Potential Hormone Mechanisms of Bariatric Surgery. Curr. Obes. Rep. 2017, 6, 253–265. [Google Scholar] [CrossRef] [Green Version]
- Sarwer, D.B.; Wadden, T.A.; Fabricatore, A.N. Psychosocial and Behavioral Aspects of Bariatric Surgery. Obes. Res. 2005, 13, 639–648. [Google Scholar] [CrossRef]
- Neff, K.; Olbers, T.; le Roux, C. Bariatric surgery: The challenges with candidate selection, individualizing treatment and clinical outcomes. BMC Med. 2013, 11, 8. [Google Scholar] [CrossRef] [Green Version]
- da Silva, S.S.P.; da Costa Maia, Â. Obesity and Treatment Meanings in Bariatric Surgery Candidates: A Qualitative Study. Obes. Surg. 2012, 22, 1714–1722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauchowitz, A.; Azarbad, L.; Day, K.; Gonder-Frederick, L. Evaluation of expectations and knowledge in bariatric surgery patients. Surg. Obes. Relat. Dis. 2007, 3, 554–558. [Google Scholar] [CrossRef] [PubMed]
- Bauchowitz, A.U.; Gonder-Frederick, L.A.; Olbrisch, M.-E.; Azarbad, L.; Ryee, M.-Y.; Woodson, M.; Miller, A.; Schirmer, B. Psychosocial Evaluation of Bariatric Surgery Candidates: A Survey of Present Practices. Psychosom. Med. 2005, 67, 825–832. [Google Scholar] [CrossRef] [PubMed]
- Engström, M.; Wiklund, M.; Olsén, M.F.; Lönroth, H.; Forsberg, A. The Meaning of Awaiting Bariatric Surgery Due to Morbid Obesity. Open Nurs. J. 2011, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kaly, P.; Orellana, S.; Torrella, T.; Takagishi, C.; Saff-Koche, L.; Murr, M.M. Unrealistic weight loss expectations in candidates for bariatric surgery. Surg. Obes. Relat. Dis. 2008, 4, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J.; Clementi, C.; Aylwin, S. The impact of obesity surgery and the paradox of control: A qualitative study. Psychol. Health 2006, 21, 273–293. [Google Scholar] [CrossRef]
- Wysoker, A. The Lived Experience of Choosing Bariatric Surgery to Lose Weight. J. Am. Psychiatr. Nurses Assoc. 2005, 11, 26–34. [Google Scholar] [CrossRef]
- Homer, C.V.; Tod, A.M.; Thompson, A.R.; Allmark, P.; Goyder, E. Expectations and patients’ experiences of obesity prior to bariatric surgery: A qualitative study. BMJ Open 2016, 6, e009389. [Google Scholar] [CrossRef] [Green Version]
- Fischer, L.; Nickel, F.; Sander, J.; Ernst, A.; Bruckner, T.; Herbig, B.; Büchler, M.W.; Müller-Stich, B.P.; Sandbu, R. Patient expectations of bariatric surgery are gender specific—A prospective, multicenter cohort study. Surg. Obes. Relat. Dis. 2014, 10, 516–523. [Google Scholar] [CrossRef]
- Owen-Smith, A.; Donovan, J.; Coast, J. How clinical rationing works in practice: A case study of morbid obesity surgery. Soc. Sci. Med. 2015, 147, 288–295. [Google Scholar] [CrossRef]
- Ratcliffe, D.; Ali, R.; Ellison, N.; Khatun, M.; Poole, J.; Coffey, C. Bariatric psychology in the UK National Health Service: Input across the patient pathway. BMC Obes. 2014, 1, 20. [Google Scholar] [CrossRef] [Green Version]
- Fabricatore, A.; Crerand, C.; Wadden, T.; Sarwer, D.; Krasucki, J. How Do Mental Health Professionals Evaluate Candidates for Bariatric Surgery? Survey Results. Obes. Surg. 2006, 16, 567–573. [Google Scholar] [CrossRef]
- Glinski, J.; Wetzler, S.; Goodman, E. The Psychology of Gastric Bypass Surgery. Obes. Surg. 2001, 11, 581–588. [Google Scholar] [CrossRef]
- Collazo-Clavell, M.L.; Clark, M.M.; McAlpine, D.E.; Jensen, M.D. Assessment and Preparation of Patients for Bariatric Surgery. Mayo Clin. Proc. 2006, 81, S11–S17. [Google Scholar] [CrossRef]
- Livhits, M.; Mercado, C.; Yermilov, I.; Parikh, J.A.; Dutson, E.; Mehran, A.; Ko, C.Y.; Gibbons, M.M. Preoperative Predictors of Weight Loss Following Bariatric Surgery: Systematic Review. Obes. Surg. 2012, 22, 70–89. [Google Scholar] [CrossRef]
- Pull, C.B. Current psychological assessment practices in obesity surgery programs: What to assess and why? Curr. Opin. Psychiatry 2010, 23, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Wadden, T.A.; Sarwer, D.B.; Fabricatore, A.N.; Jones, L.; Stack, R.; Williams, N.S. Psychosocial and Behavioral Status of Patients Undergoing Bariatric Surgery: What to Expect Before and After Surgery. Med. Clin. N. Am. 2007, 91, 451–469. [Google Scholar] [CrossRef] [PubMed]
- Owen-Smith, A.; Donovan, J.; Coast, J. Experiences of accessing obesity surgery on the NHS: A qualitative study. J. Public Health 2016. [Google Scholar] [CrossRef] [Green Version]
- Leary, M.R.; Kowalski, R.M. Impression Management: A Literature Review and Two-Component Model. Psychol. Bull. 1990, 107, 34–47. [Google Scholar] [CrossRef]
- Ambwani, S.; Boeka, A.G.; Brown, J.D.; Byrne, T.K.; Budak, A.R.; Sarwer, D.B.; Fabricatore, A.N.; Morey, L.C.; O’Neil, P.M. Socially desirable responding by bariatric surgery candidates during psychological assessment. Surg. Obes. Relat. Dis. 2013, 9, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Fabricatore, A.N.; Sarwer, D.B.; Combs, C.J.; Krasucki, J.L. Impression management or real change? Reports of depressive symptoms before and after the preoperative psychological evaluation for bariatric surgery. Obes. Surg. 2007, 7, 1213–1219. [Google Scholar] [CrossRef]
- Heinberg, L.J. The Role of Psychological Testing for Bariatric/Metabolic Surgery Candidates. Bariatric Times Online Editor. Available online: https://bariatrictimes.com/the-role-of-psychological-testing-for-bariatricmetabolic-surgery-candidates/ (accessed on 13 May 2021).
- Rosik, C.H. Psychiatric Symptoms among Prospective Bariatric Surgery Patients: Rates of Prevalence and their Relation to Social Desirability, Pursuit of Surgery, and Follow-Up Attendance. Obes. Surg. 2005, 15, 677–683. [Google Scholar] [CrossRef]
- Heinberg, L.J.; Marek, R.; Haskins, I.N.; Bucak, E.; Nor Hanipah, Z.; Brethauer, S. 30-day readmission following weight loss surgery: Can psychological factors predict nonspecific indications for readmission? Surg. Obes. Relat. Dis. 2017, 13, 1376–1381. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Refocusing the Care Programme Approach: Policy and Positive Practice Guidance; Department of Health: London, UK, 2008. Available online: https://webarchive.nationalarchives.gov.uk/20130124042407/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_083649.pdf (accessed on 13 May 2021).
- National Institute for Care and Excellence. Patient Experience in Adult NHS Services: Improving the Experience of Care for People Using Adult NHS Services; Publication No. CG138. 2012. Available online: https://www.nice.org.uk/guidance/cg138 (accessed on 13 May 2021).
- World Health Organisation. Mental Health Action Plan 2013–2020; World Health Organisation: Geneva, Switzerland, 2013; Available online: https://www.who.int/mental_health/publications/action_plan/en/on12/05/2020 (accessed on 13 May 2021).
- Cegala, D.J.; Street, R.L.; Clinch, C.R. The Impact of Patient Participation on Physicians’ Information Provision during a Primary Care Medical Interview. Health Commun. 2007, 21, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Coulter, A.; Ellins, J. Effectiveness of strategies for informing, educating, and involving patients. BMJ 2007, 335, 24–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crawford, M.J. Systematic review of involving patients in the planning and development of health care. BMJ 2002, 325, 1263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- British Obesity & Metabolic Surgery Society. Letter to PM. Available online: https://www.bomss.org.uk/ (accessed on 20 May 2020).
- Smith, J.A.; Flowers, P.; Larkin, M. Interpretative Phenomenological Analysis: Theory, Method and Research; SAGE: Newcastle upon Tyne, UK, 2009. [Google Scholar]
- Peat, G.; Rodriguez, A.; Smith, J. Interpretive phenomenological analysis applied to healthcare research. Evid. Based Nurs. 2019, 22, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Hammarberg, K.; Kirkman, M.; de Lacey, S. Qualitative research methods: When to use them and how to judge them. Hum. Reprod. 2016, 31, 498–501. [Google Scholar] [CrossRef] [Green Version]
- Eatough, V.; Smith, J. I was like a wild wild person: Understanding feelings of anger using interpretative phenomenological analysis. Br. J. Psychol. 2006, 97, 483–498. [Google Scholar] [CrossRef]
- Pietkiewicz, I.; Smith, J.A. A practical guide to using Interpretative Phenomenological Analysis in qualitative research psychology. Czas. Psychol. 2012, 20, 361–369. [Google Scholar] [CrossRef]
- Townshend, K.; Caltabiano, N.J. The extended nervous system: Affect regulation, somatic and social change processes associated with mindful parenting. BMC Psychol. 2019, 7, 41. [Google Scholar] [CrossRef]
- Watson, C.; Riazi, A.; Ratcliffe, D. Exploring the Experiences of Women Who Develop Restrictive Eating Behaviours after Bariatric Surgery. Obes. Surg. 2020, 30, 2131–2139. [Google Scholar] [CrossRef] [Green Version]
- Yardley, L. Dilemmas in qualitative health research. Psychol. Health 2000, 15, 215–228. [Google Scholar] [CrossRef]
- Booth, H.P.; Khan, O.; Fildes, A.; Prevost, A.T.; Reddy, M.; Charlton, J.; Gulliford, M.C. Changing Epidemiology of Bariatric Surgery in the UK: Cohort Study Using Primary Care. Obes. Surg. 2016, 26, 1900–1905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puhl, R.M.; Heuer, C.A. Obesity stigma: Important considerations for public health. Am. J. Public Health 2010, 100, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Maestre, J.F.; Eikey, E.V.; Warner, M.; Yarosh, S.; Pater, J.; Jacobs, M.; Marcu, G.; Shih, P.C. Conducting research with stigmatized populations: Practices, challenges, and lessons learned. In Proceedings of the CSCW ‘18: Companion of the 2018 ACM Conference on Computer Supported Cooperative Work and Social Computing, 3–7 November 2018; Association for Computing Machinery: New York, NY, USA, 2018; pp. 385–392. [Google Scholar]
- Smith, J.A.; Osborn, M. Chapter 4: Interpretive Phenomenological Analysis. In Qualitative Psychology. A practical Guide to Research Methods; Smith, J.A., Ed.; SAGE: Newcastle upon Tyne, UK, 2008; pp. 53–80. [Google Scholar]
- Royal College of Physicians. Action on obesity: Comprehensive care for all. Clin. Med. 2013, 13, 4. Available online: https://www.rcpjournals.org/content/clinmedicine/13/1/4 (accessed on 13 May 2021). [CrossRef]
- Owen-Smith, A.; Kipping, R.; Donovan, J.; Hine, C.; Maslen, C.; Coast, J. NICE example- variation in access to morbid obesity surgery in England. BMJ 2013, 346, 21–23. [Google Scholar] [CrossRef] [PubMed]
- Welbourn, R.; le Roux, C.W.; Owen-Smith, A.; Wordsworth, S.; Blazeby, J.M. Why the NHS should do more bariatric surgery; how much should we do? BMJ 2016, 353. [Google Scholar] [CrossRef] [Green Version]
- Dzeng, E.; Smith, T.J. Rationing Healthcare: Who’s Responsible? Oncology 2014, 27, 91–96. [Google Scholar]
- McKinstry, B. Paternalism and the doctor-patient relationship in general practice. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 1992, 42, 340–342. [Google Scholar]
- Hall, M.A.; Dugan, E.; Zheng, B.; Mishra, A.K. Trust in Physicians and Medical Institutions: What Is It, Can It Be Measured, and Does It Matter? Milbank Q. 2001, 79, 613–639. [Google Scholar] [CrossRef] [Green Version]
- Ommen, O.; Janssen, C.; Neugebauer, E.; Bouillon, B.; Rehm, K.; Rangger, C.; Erli, H.J.; Pfaff, H. Trust, social support and patient type—Associations between patients perceived trust, supportive communication and patients preferences in regard to paternalism, clarification and participation of severely injured patients. Patient Educ. Couns. 2008, 73, 196–204. [Google Scholar] [CrossRef]
- King, A.; Hoppe, R.B. Best Practice” for Patient-Centered Communication: A Narrative Review. J. Grad. Med. Educ. 2013, 5, 385–393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michie, S.; Miles, J.; Weinman, J. Patient-centredness in chronic illness: What is it and does it matter? Patient Educ. Couns. 2003, 51, 197–206. [Google Scholar] [CrossRef]
- Stewart, M.A. Effective physician-patient communication and health outcomes: A review. Can. Med Assoc. J. 1995, 152, 1423–1433. [Google Scholar]
- Ogden, J.; Ratcliffe, D.; Snowdon-Carr, V. British Obesity Metabolic Surgery Society endorsed guidelines for psychological support pre- and post-bariatric surgery. Clin. Obes. 2019, 9. [Google Scholar] [CrossRef] [PubMed]
- Forsyth, J. Boris Johnson Launches a New Battle of the Bulge. The Times. Available online: https://www.thetimes.co.uk/ (accessed on 13 May 2021).
- House of Commons. Covid-19 Response. 18 May 2020. Volume 676. Available online: https://bit.ly/2zOKsec (accessed on 13 May 2021).
- World Obesity Federation. Obesity and COVID-19: Policy Statement. Available online: https://www.worldobesity.org/news/obesity-and-covid-19-policy-statement (accessed on 12 May 2020).
| Participant (Pseudonym) | Gender | Age | Marital Status | Ethnicity | Education Level | Currently in Employment (Y/N) | Hospital Name (Pseudonym) | Type of BS | Time Since Post-Surgery | W/T Since Referral | Weight Management |
|---|---|---|---|---|---|---|---|---|---|---|---|
| George | Male | No info | No info | No info | No info | No info | Wallace Hospital | No info | 2019 * | 48 months ** | No info |
| Holly | Female | 51 | Married | White/Caucasian | Master’s level | No | Wallace/Stanford Hospital | Gastric Banding (private) Gastric Bypass (private) Sleeve Gastrectomy (NHS) | 2012 2013 2016 | 12 months | No |
| Sabina | Female | 29 | Single | Black/African/Caribbean/Black British | A-levels | No | Hillsdale Hospital | Sleeve Gastrectomy (NHS) | 2019 | 48 months * | Yes |
| Rachel | Female | 61 | Married | White/Caucasian | >A-levels | No | Wallace Hospital | Gastric Bypass (NHS) | 2018 | 15 months | Yes |
| Superordinate Themes | Subordinate Themes | Number of Transcripts Contributing to Theme |
| PSE was challenging but essential | A long but necessary PSE | 4 |
| Scrutiny and suitability | 4 | |
| ‘Psych’ as a wall | 4 | |
| Coping processes to deal with the PSE | Psychological coping strategies | 3 |
| Doing your own research | 4 | |
| Support systems | 4 | |
| Past experiences influencing current perspectives | 4 | |
| Self-perception | 4 | |
| Staff and service evaluation | A tailored PSE | 3 |
| Level of information | 4 | |
| Praise and criticism of service | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sahar, K.; Riazi, A. Experiences of the Bariatric Pre-Surgery Evaluation Process in a National Health Service—An Interpretative Phenomenological Analysis. Surgeries 2021, 2, 199-215. https://doi.org/10.3390/surgeries2020021
Sahar K, Riazi A. Experiences of the Bariatric Pre-Surgery Evaluation Process in a National Health Service—An Interpretative Phenomenological Analysis. Surgeries. 2021; 2(2):199-215. https://doi.org/10.3390/surgeries2020021
Chicago/Turabian StyleSahar, Karan, and Afsane Riazi. 2021. "Experiences of the Bariatric Pre-Surgery Evaluation Process in a National Health Service—An Interpretative Phenomenological Analysis" Surgeries 2, no. 2: 199-215. https://doi.org/10.3390/surgeries2020021
APA StyleSahar, K., & Riazi, A. (2021). Experiences of the Bariatric Pre-Surgery Evaluation Process in a National Health Service—An Interpretative Phenomenological Analysis. Surgeries, 2(2), 199-215. https://doi.org/10.3390/surgeries2020021







