Abstract
Huntington’s disease (HD) is a rare genetic disorder resulting in progressive neurodegeneration leading to motor, cognitive and psychiatric symptoms. A high percentage of HD patients suffer from comorbid major depressive disorder (MDD). We are not aware of any literature on the use of repetitive transcranial magnetic stimulation (rTMS) for treating comorbid MDD in HD. We present the case of a 57-year-old man suffering from HD in which comorbid MDD was successfully treated with rTMS. Further work is required to better characterize the safety, tolerability and effectiveness of rTMS to treat comorbid MDD in HD.
1. Introduction
Huntington’s disease (HD) is a rare neurodegenerative condition usually caused by an inherited genetic mutation in the huntingtin gene. Neurodegeneration occurs in many brain regions, including the thalamus, cerebellum, hypothalamus, and basal ganglia [1]. The activity of various neurotransmitters is also altered in HD, including dopamine, glutamate and γ-aminobutyric acid (GABA) [2]. HD is mainly characterized by a hyperkinetic movement disorder known as chorea, resulting from basal ganglia degeneration. HD is also characterized by cognitive and psychiatric symptoms, with 15–69% of patients suffering from comorbid major depressive disorder (MDD) [3]. MDD is often one of the earliest presentations of HD [4], with patients at a significantly higher risk of suicidal behavior compared to the general population [5,6]. In this context, optimal treatment of MDD in HD patients is essential.
In HD patients suffering from comorbid MDD, antidepressants remain the first-line treatment [7]. Still, pharmacotherapy is burdened by limited effectiveness and several side-effects [8]. Given those limitations, new therapies have been developed and are now available for MDD. In the past decade, repetitive transcranial magnetic stimulation (rTMS) has emerged as a safe, well-tolerated and effective treatment for treatment-resistant depression [9]. rTMS uses a rapidly alternating and powerful magnetic field to modulate neural activity in specific brain regions known to be abnormal in MDD. The most recent literature indicates that rTMS consistently achieves response and remission rates of 40–55% and 25–35% in treatment-resistant depression, respectively, with little to no side-effects [7].
There is a limited number of publications reporting the use of rTMS for treating comorbid MDD in neurological disorders. A meta-analysis including seven studies reported that rTMS effectively reduced depressive symptoms in Parkinson’s Disease [10]. A recent double-blind, sham-controlled study reported significant improvement in the depressive symptoms of eleven patient suffering from post-stroke depression with high-frequency rTMS [11]. So far, we are not aware of any reports on the use of rTMS in HD patients suffering from comorbid MDD.
2. Case Report
We report on the case of a 57-year-old man suffering from both HD and MDD. The patient initially had positive HD genetic testing in 1993, which was conducted given his positive family history for the disease. Initial MDD symptoms appeared in the early 2000s and diagnosis of HD was made in 2005. The patient was initially started on venlafaxine, to which mirtazapine was added 6 months later. The episodic increase in symptoms was managed by medication dose increase. The patient initially responded favorably to antidepressant medication, achieving stability for several years with only few relapses. Around 2010, bupropion was added to the regimen because of an increase in depressive symptoms but was not tolerated and therefore discontinued. Around 2015, valproic acid was introduced to manage impulsivity issues. Depressive relapses became more severe in 2018, and medication changes did not bring any additional benefits. rTMS was therefore offered in early 2019.
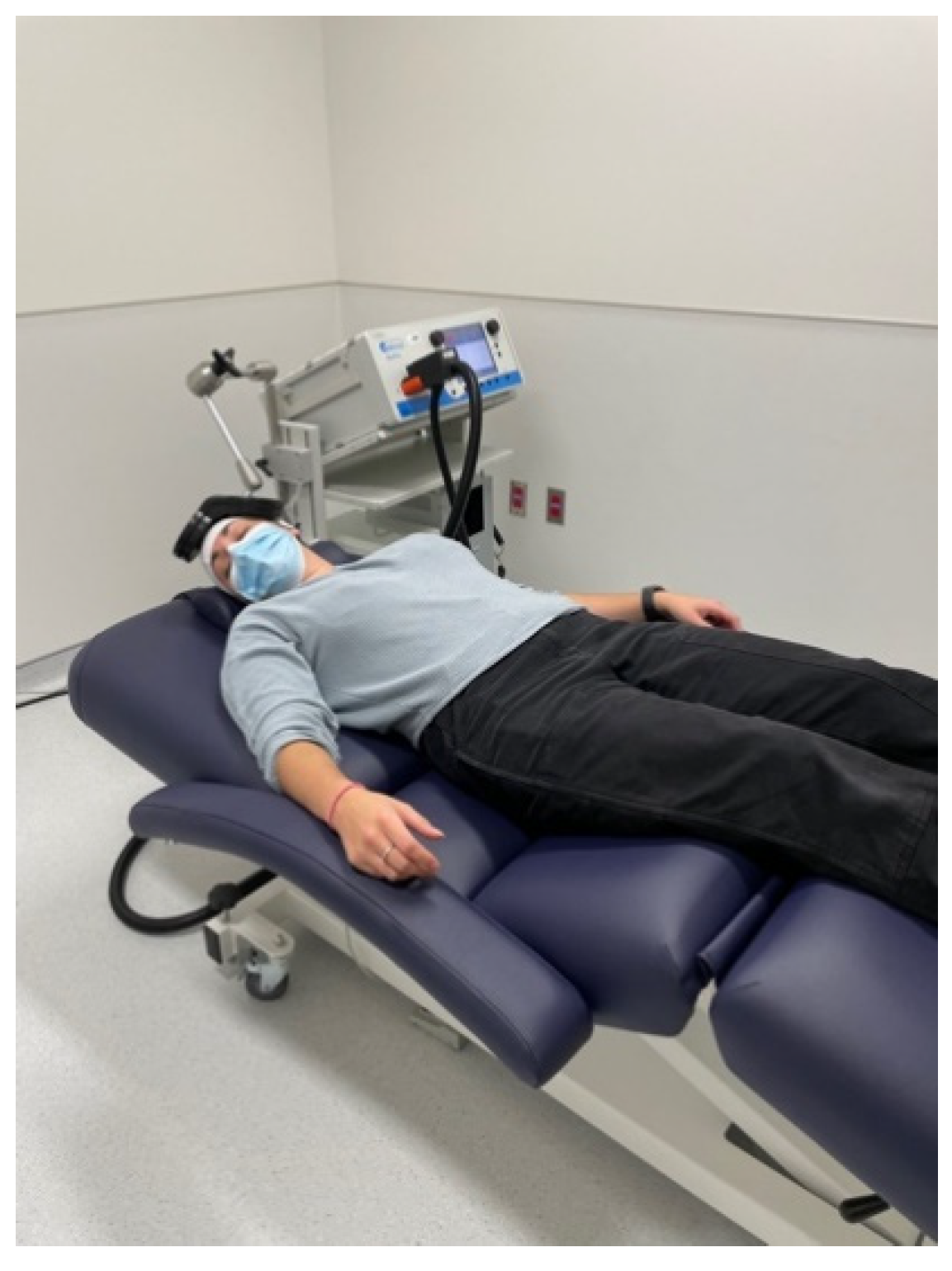
Treatment consisted of a high-frequency (HF) 20 Hz rTMS protocol (5 s ON, 25 s OFF, 3000 pulses, ~15 min duration) delivered over the left dorsolateral prefrontal cortex (DLPFC) using the BeamF3 algorithm [12] at 120% of the resting motor threshold (rMT), using R30/X100 stimulators equipped with a DB80 coil (MagVenture, Farum, Denmark). We used the same intensive protocol reported in a previous publication from our group for which we observed good results with older patients [13]. High-frequency protocols seem to have a higher efficacy in older adults with cortical atrophy [14,15]. The DB80 coil was chosen given the light diffuse cerebral atrophy seen on MRI, and a quite elevated motor threshold with a B-70 coil. The treatment course consisted of three daily sessions every weekday over 2 weeks, for a total of 30 sessions. The movements induced by the chorea was initially an issue, as the patient was involuntarily moving away from the coil at times. This was addressed by having him lie on his back instead of sitting during treatment, securing the head between the coil and the headrest (Figure 1). The patient did not report any pain or side effects during treatment.
Figure 1.
Supine treatment position to limit chorea.
Symptoms were assessed pre- and post-treatment using the Montgomery–Asberg Depression Rating Scale (MADRS). Remission was defined as a score < 10. After his first treatment series in 2019, he achieved remission, with MADRS scores going from 24 at baseline (moderate depression) down to 5 (normal range) at follow-up. Following rTMS, the patient reported increased energy as well as an increased interest in his daily activities. He remained stable until 21 months later without any maintenance treatment, after which he experienced a depressive recurrence. The patient subsequently underwent a second course of treatment using the same protocol, after which he once again reached remission, with MADRS scores decreasing from 18 at baseline (mild depression) to 10 post-treatment (mild depression). To optimize response, the patient underwent maintenance treatments once a week over 7 weeks (three sessions on weeks 1 and 2, two sessions on weeks 3, 4 and 5, and one session on weeks 6 and 7). His MADRS score went down to 6 (normal range) at follow-up.
3. Discussion
Several hypotheses have been put forward to explain the high comorbidity between HD and MDD. One explanation is that depressive symptoms are the direct result of cerebral degeneration (more specifically neuronal loss in the striatum), also affecting limbic structures [16]. This in turn can affect prefrontal activity, a region central to MDD [17]. Dopaminergic activity is also known to be altered in HD. Even though dopamine (DA) activity is increased during the early stages of HD, DA deficit leading to hypokinesia is the hallmark of the later stages of the disease. In and of itself, alterations in DA neurotransmission could contribute to depressive symptoms, while also affecting glutamate activity, leading to excitotoxicity [18].
Multiple studies have attempted to characterize the antidepressant effects of rTMS in MDD. The effects of rTMS on cell-signaling pathways, including an increase in cell proliferation and BDNF in limbic areas, could be part of its antidepressant effect [19,20]. Left-DLPFC rTMS has also been shown to modulate DA activity in striatal areas and beyond, such as the anterior cingulate cortex and orbitofrontal areas, which have a central role in MDD [21,22,23].
The effect of rTMS on chorea was not formally monitored during treatment, and neither the patient nor the medical team noticed any changes on that front. The effect of rTMS applied over the motor cortex in the context of motor disturbances in patients with HD has been found to be highly variable [24]. Some studies reported a decrease in movement disorders in HD patients [25], while others reported no significant changes [26]. Still, as rTMS is known to increase DA activity in the striatum [27], it could potentially influence chorea. Future studies should prospectively assess motor symptoms using validated scales such as the Unified Huntington Disease Rating Scale (UHDRS) [28].
Significant brain atrophy is often observed in patients with HD. The presence of regional brain atrophy might attenuate rTMS current density in the cortex, but there is evidence that rTMS can have clinical benefits in populations with known brain atrophy, such as in Alzheimer’s disease [29,30]. Therefore, rTMS should not be excluded in HD patients suffering from comorbid MDD simply because of brain atrophy.
4. Conclusions
We report on the first demonstration of safe and successful treatment of MDD in a HD patient with rTMS. Of note, initial rTMS-induced antidepressant effects persisted almost 2 years post-treatment in our patient. Similar mood improvements were observed during both courses of rTMS treatment. Chorea might be a barrier to rTMS therapy in HD patients suffering from comorbid MDD, jeopardizing reliable coil placement during stimulation. Instead of the classical seating position, we therefore recommend a supine position, decreasing the odds of movement away from the optimal stimulation area. As this study is a case report, we cannot generalize the results and future studies need to replicate these findings in larger samples and should also assess whether rTMS influences chorea and cognition in HD patients suffering from comorbid MDD.
Author Contributions
C.N.: writing original draft; J.-P.M.: conceptualization, writing—original draft, supervision, writing—review & editing; V.D.J. and T.R.C.: conceptualization, supervision, writing—review & editing; S.C.: writing—review & editing; P.L.: writing—review & editing. All authors have approved the final article. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Acknowledgments
The authors are pleased to acknowledge Sylvie Tieu and Ana Baker, clinical nurses, who provided treatments to the patient.
Conflicts of Interest
The authors report no potential conflict of interest.
References
- Ross, C.A.; Tabrizi, S. Huntington’s disease: From molecular pathogenesis to clinical treatment. Lancet Neurol. 2011, 10, 83–98. [Google Scholar] [CrossRef]
- Jamwal, S.; Kumar, P. Insight Into the Emerging Role of Striatal Neurotransmitters in the Pathophysiology of Parkinson’s Disease and Huntington’s Disease: A Review. Curr. Neuropharmacol. 2019, 17, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Galts, C.P.; Bettio, L.; Jewett, D.C.; Yang, C.C.; Brocardo, P.S.; Rodrigues, A.L.S.; Thacker, J.S.; Gil-Mohapel, J. Depression in neurodegenerative diseases: Common mechanisms and current treatment options. Neurosci. Biobehav. Rev. 2019, 102, 56–84. [Google Scholar] [CrossRef]
- Kirkwood, S.C.; Su, J.L.; Conneally, P.M.; Foroud, T. Progression of Symptoms in the Early and Middle Stages of Huntington Disease. Arch. Neurol. 2001, 58, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Bindler, L.; Travers, D.; Millet, B. [Suicide in Huntington’s disease: A review]. Rev. Med. Suisse 2009, 5, 646–648. [Google Scholar]
- Hawton, K.; Comabella, C.C.I.; Haw, C.; Saunders, K. Risk factors for suicide in individuals with depression: A systematic review. J. Affect. Disord. 2013, 147, 17–28. [Google Scholar] [CrossRef]
- Milev, R.V.; Giacobbe, P.; Kennedy, S.; Blumberger, D.M.; Daskalakis, Z.J.; Downar, J.; Modirrousta, M.; Patry, S.; Vila-Rodriguez, F.; Lam, R.W.; et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder. Can. J. Psychiatry 2016, 61, 561–575. [Google Scholar] [CrossRef]
- Akil, H.; Gordon, J.; Hen, R.; Javitch, J.; Mayberg, H.; McEwen, B.; Meaney, M.J.; Nestler, E.J. Treatment resistant depression: A multi-scale, systems biology approach. Neurosci. Biobehav. Rev. 2018, 84, 272–288. [Google Scholar] [CrossRef]
- Rossi, S.; Hallett, M.; Rossini, P.M.; Pascual-Leone, A. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin. Neurophysiol. 2009, 120, 2008–2039. [Google Scholar] [CrossRef] [Green Version]
- Lesenskyj, A.M.; Samples, M.P.; Farmer, J.M.; Maxwell, C.R. Treating refractory depression in Parkinson’s disease: A meta-analysis of transcranial magnetic stimulation. Transl. Neurodegener. 2018, 7, 8. [Google Scholar] [CrossRef]
- Hordacre, B.; Comacchio, K.; Williams, L.; Hillier, S. Repetitive transcranial magnetic stimulation for post-stroke depression: A randomised trial with neurophysiological insight. J. Neurol. 2021, 268, 1474–1484. [Google Scholar] [CrossRef] [PubMed]
- Beam, W.; Borckardt, J.J.; Reeves, S.T.; George, M.S. An efficient and accurate new method for locating the F3 position for prefrontal TMS applications. Brain Stimul. 2009, 2, 50–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jodoin, V.D.; Miron, J.-P.; Lespérance, P. Safety and Efficacy of Accelerated Repetitive Transcranial Magnetic Stimulation Protocol in Elderly Depressed Unipolar and Bipolar Patients. Am. J. Geriatr. Psychiatry 2019, 27, 548–558. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.A.; Darwish, E.S.; Khedr, E.M.; Elserogy, Y.; Ali, A.M. Effects of low versus high frequencies of repetitive transcranial magnetic stimulation on cognitive function and cortical excitability in Alzheimer’s dementia. J. Neurol. 2012, 259, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Guse, B.; Falkai, P.; Wobrock, T. Cognitive effects of high-frequency repetitive transcranial magnetic stimulation: A systematic review. J. Neural Transm. 2009, 117, 105–122. [Google Scholar] [CrossRef] [Green Version]
- Paoli, R.A.; Botturi, A.; Ciammola, A.; Silani, V.; Prunas, C.; Lucchiari, C.; Zugno, E.; Caletti, E. Neuropsychiatric Burden in Huntington’s Disease. Brain Sci. 2017, 7, 67. [Google Scholar] [CrossRef]
- Slaughter, J.R.; Martens, M.P.; Slaughter, K.A. Depression and Huntington’s Disease: Prevalence, Clinical Manifestations, Etiology, and Treatment. CNS Spectrums 2001, 6, 306–326. [Google Scholar] [CrossRef]
- Cepeda, C.; Murphy, K.P.S.; Parent, M.; Levine, M.S. The role of dopamine in huntington’s disease. In Progress in Brain Research; Elsevier: Amsterdam, The Netherlands, 2014; Volume 211, pp. 235–254. [Google Scholar]
- Yukimasa, T.; Yoshimura, R.; Tamagawa, A.; Uozumi, T.; Shinkai, K.; Ueda, N.; Tsuji, S.; Nakamura, J. High-Frequency Repetitive Transcranial Magnetic Stimulation Improves Refractory Depression by Influencing Catecholamine and Brain-Derived Neurotrophic Factors. Pharmacopsychiatry 2006, 39, 52–59. [Google Scholar] [CrossRef] [Green Version]
- Zhao, X.; Li, Y.; Tian, Q.; Zhu, B.; Zhao, Z. Repetitive transcranial magnetic stimulation increases serum brain-derived neurotrophic factor and decreases interleukin-1β and tumor necrosis factor-α in elderly patients with refractory depression. J. Int. Med. Res. 2019, 47, 1848–1855. [Google Scholar] [CrossRef]
- Cho, S.S.; Strafella, A.P. rTMS of the Left Dorsolateral Prefrontal Cortex Modulates Dopamine Release in the Ipsilateral Anterior Cingulate Cortex and Orbitofrontal Cortex. PLoS ONE 2009, 4, e6725. [Google Scholar] [CrossRef] [Green Version]
- Pogarell, O.; Koch, W.; Pöpperl, G.; Tatsch, K.; Jakob, F.; Zwanzger, P.; Mulert, C.; Rupprecht, R.; Möller, H.-J.; Hegerl, U. Striatal dopamine release after prefrontal repetitive transcranial magnetic stimulation in major depression: Preliminary results of a dynamic [123I] IBZM SPECT study. J. Psychiatr. Res. 2006, 40, 307–314. [Google Scholar] [CrossRef]
- Pogarell, O.; Koch, W.; Pöpperl, G.; Tatsch, K.; Jakob, F.; Mulert, C.; Grossheinrich, N.; Rupprecht, R.; Möller, H.-J.; Hegerl, U.; et al. Acute prefrontal rTMS increases striatal dopamine to a similar degree as d-amphetamine. Psychiatry Res. Neuroimaging 2007, 156, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Latorre, A.; Rocchi, L.; Berardelli, A.; Bhatia, K.P.; Rothwell, J.C. The use of transcranial magnetic stimulation as a treatment for movement disorders: A critical review. Mov. Disord. 2019, 34, 769–782. [Google Scholar] [CrossRef]
- Brusa, L.; Versace, V.; Koch, G.; Bernardi, G.; Iani, C.; Stanzione, P.; Centonze, D. Improvement of choreic movements by 1 Hz repetitive transcranial magnetic stimulation in Huntington’s disease patients. Ann. Neurol. 2005, 58, 655–656. [Google Scholar] [CrossRef] [PubMed]
- Shukla, A.; Jayarajan, R.N.; Muralidharan, K.; Jain, S. Repetitive Transcranial Magnetic Stimulation Not Beneficial in Severe Choreiform Movements of Huntington Disease. J. ECT 2013, 29, e16–e17. [Google Scholar] [CrossRef]
- Keck, M.; Welt, T.; Müller, M.; Erhardt, A.; Ohl, F.; Toschi, N.; Holsboer, F.; Sillaber, I. Repetitive transcranial magnetic stimulation increases the release of dopamine in the mesolimbic and mesostriatal system. Neuropharmacology 2002, 43, 101–109. [Google Scholar] [CrossRef]
- Unified Huntington’s disease rating scale: Reliability and consistency. Mov. Disord. 1996, 11, 136–142. [CrossRef]
- Rutherford, G.; Lithgow, B.; Moussavi, Z. Short and Long-term Effects of rTMS Treatment on Alzheimer’s Disease at Different Stages: A Pilot Study. J. Exp. Neurosci. 2015, 9, S24004. [Google Scholar] [CrossRef] [Green Version]
- Xie, Y.; Li, Y.; Nie, L.; Zhang, W.; Ke, Z.; Ku, Y. Cognitive Enhancement of Repetitive Transcranial Magnetic Stimulation in Patients with Mild Cognitive Impairment and Early Alzheimer’s Disease: A Systematic Review and Meta-Analysis. Front. Cell Dev. Biol. 2021, 9, 734046. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).