Socioeconomic Position in Modern Contraceptive Uptake and Fertility Rate among Women of Childbearing Age in 37 Sub-Saharan Countries
Abstract
1. Background
2. Materials and Methods
2.1. Data Source
2.2. Selection and Measurement of Variables
2.2.1. Outcome
2.2.2. Independent Variables
2.3. Statistical Analysis
2.4. Ethical Consideration
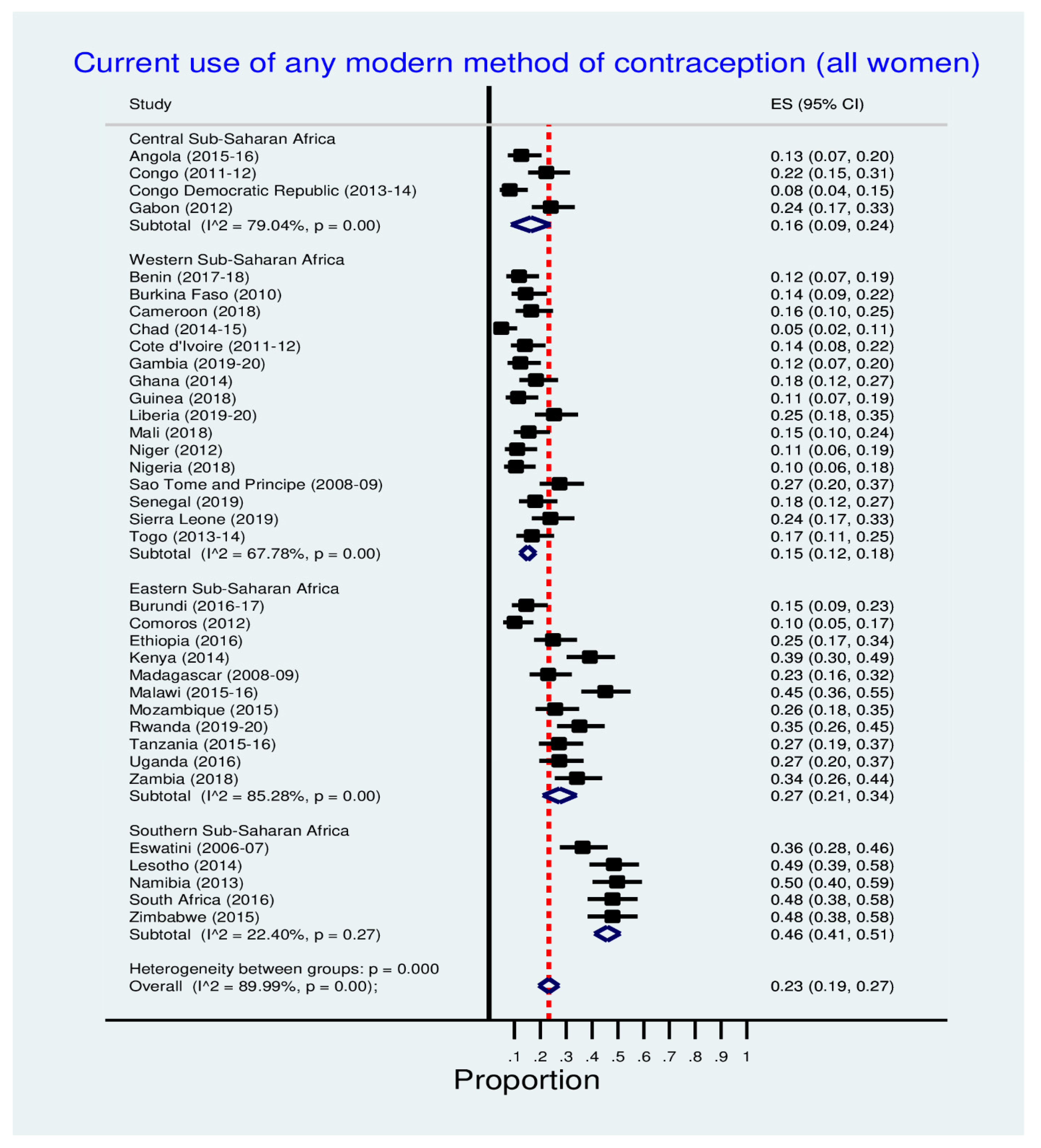
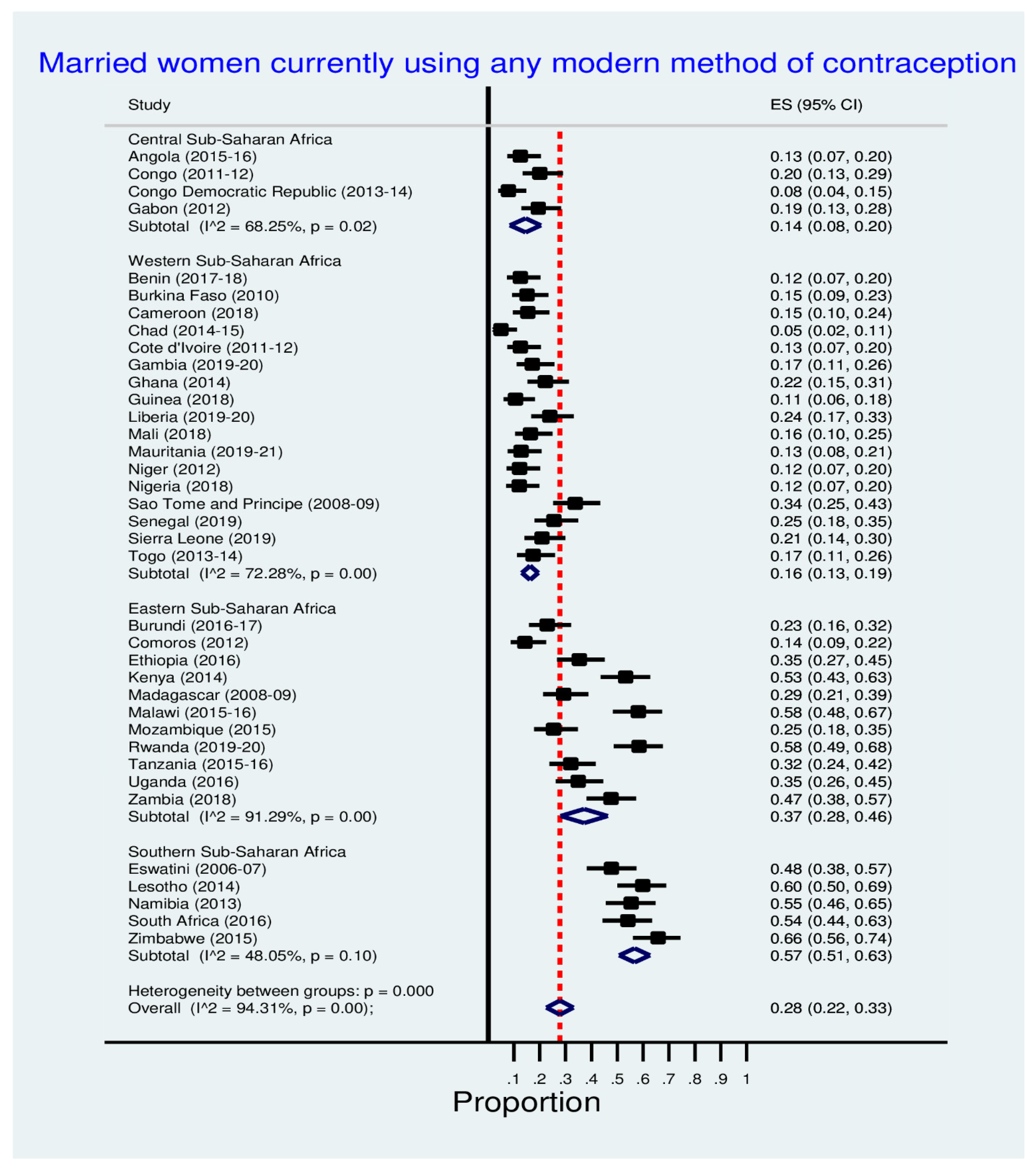
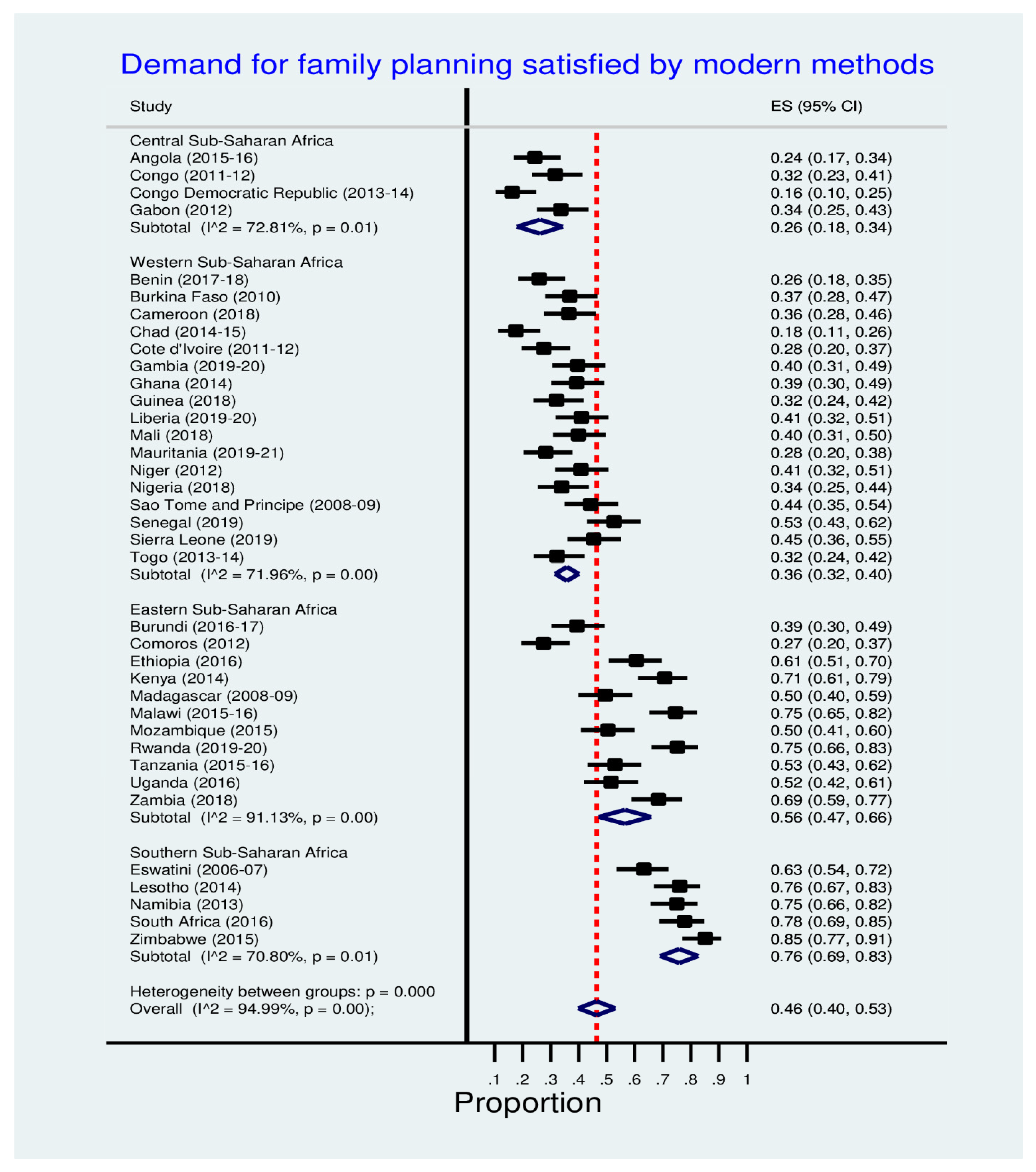
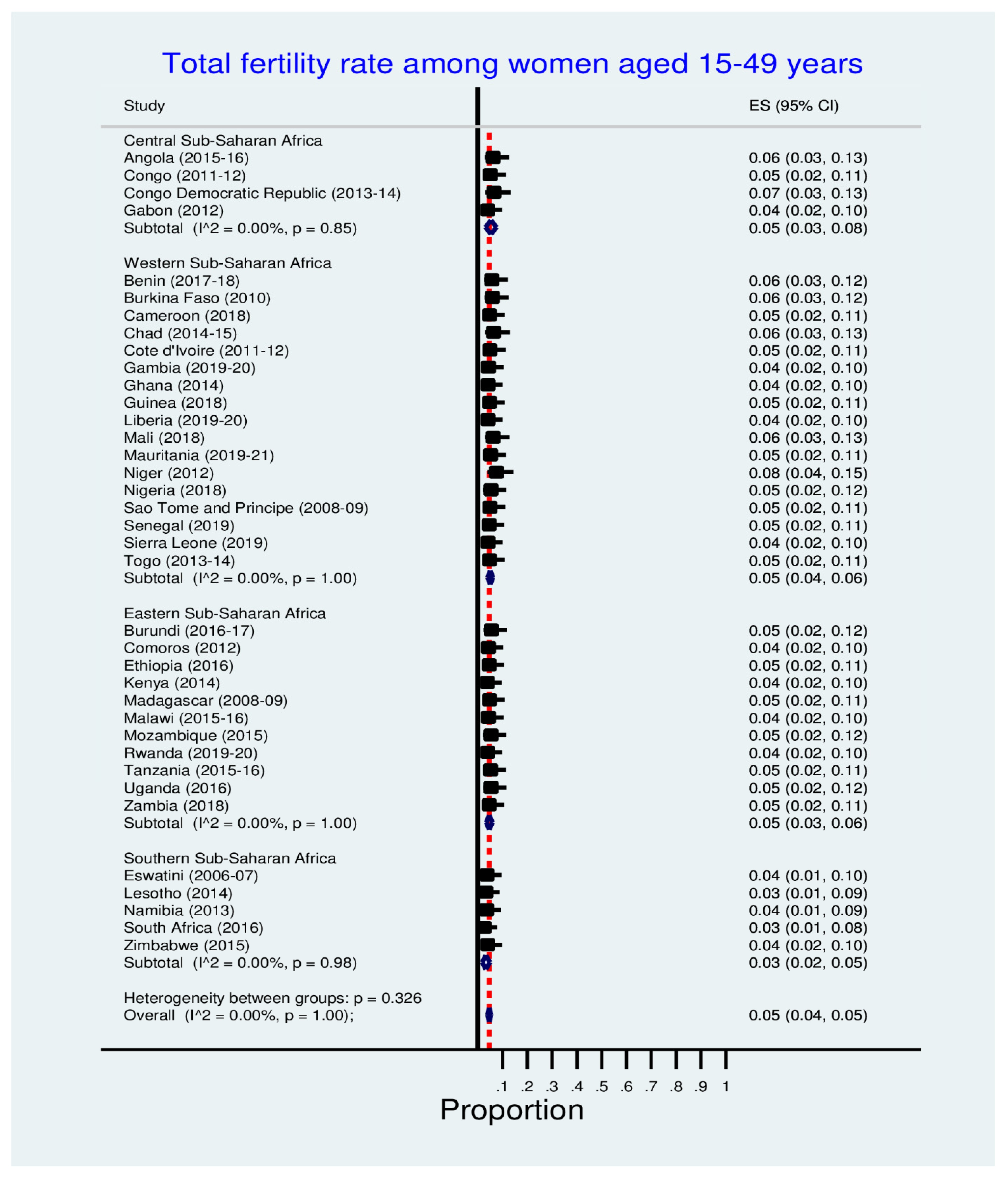
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alvarez-Nieto, C.; Pastor-Moreno, G.; Grande-Gascón, M.L.; Linares-Abad, M. Sexual and reproductive health beliefs and practices of female immigrants in Spain: A qualitative study. Reprod. Health 2015, 12, 79. [Google Scholar] [CrossRef]
- Rosa, W. (Ed.) Transforming Our World: The 2030 Agenda for Sustainable Development. A New Era in Global Health; Springer: New York, NY, USA, 2017. [Google Scholar] [CrossRef]
- Starbird, E.; Norton, M.; Marcus, R. Investing in family planning: Key to achieving the sustainable development goals. Glob. Health Sci. Pract. 2016, 4, 191–210. [Google Scholar] [CrossRef] [PubMed]
- Oye-Adeniran, B.A.; Adewole, I.F.; Umoh, A.V.; Oladokun, A.; Gbadegesin, A.; Ekanem, E.E. Community-based study of contraceptive behaviour in Nigeria. Afr. J. Reprod. Health 2006, 10, 90–104. [Google Scholar] [CrossRef] [PubMed]
- Ekholuenetale, M.; Olorunju, S.; Fowobaje, K.R.; Onikan, A.; Tudeme, G.; Barrow, A. When Do Nigerian Women of Reproductive Age Initiate and What Factors Influence Their Contraceptive Use? A Contextual Analysis. Open Access J. Contracept. 2021, 12, 133–147. [Google Scholar] [CrossRef] [PubMed]
- Do, M.; Kurimoto, N. Women’s Empowerment and Choice of Contraceptive Methods in Selected African Countries. Int. Perspect. Sex. Reprod. Health 2012, 38, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Eo, O.; Vy, A.; Va, W. Prevalence and determinants of contraceptive use among women of child-bearing age in a rural community in southern Nigeria. J. Community Med. Prim. Health Care 2017, 29, 97–107. [Google Scholar]
- Tsui, A.O.; McDonald-Mosley, R.; Burke, A.E. Family planning and the burden of unintended pregnancies. Epidemiol. Rev. 2010, 32, 152–174. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Kumar, N.; Vivekadhish, S. Millennium Development Goals (MDGs) to Sustainable Development Goals (SDGs): Addressing Unfinished Agenda and Strengthening Sustainable Development and Partnership. Indian J. Community Med. Off. Publ. Indian Assoc. Prev. Soc. Med. 2016, 41, 1. [Google Scholar] [CrossRef] [PubMed]
- Cleland, J.; Conde-Agudelo, A.; Peterson, H.; Ross, J.; Tsui, A. Contraception and health. Lancet 2012, 380, 149–156. [Google Scholar] [CrossRef]
- Ahmed, S.; Li, Q.; Liu, L.; Tsui, A.O. Maternal deaths averted by contraceptive use: An analysis of 172 countries. Lancet 2012, 380, 111–125. [Google Scholar] [CrossRef]
- Nonvignon, J.; Novignon, J. Trend and determinants of contraceptive use among women of reproductive age in Ghana. Afr. Popul. Stud. 2014, 28, 956–967. [Google Scholar] [CrossRef]
- Shapiro, D.; Hinde, A. On the pace of fertility decline in sub-Saharan Africa. Demogr. Res. 2017, 37, 1327–1338. [Google Scholar] [CrossRef]
- United Nations, Department of Economic and Social Affairs, Population Division. World Fertility and Family Planning 2020: Highlights; United Nations: New York, NY, USA, 2020. [Google Scholar]
- Tsui, A.O.; Brown, W.; Li, Q. Contraceptive Practice in sub-Saharan Africa. Popul. Dev. Rev. 2017, 43, 166–191. [Google Scholar] [CrossRef] [PubMed]
- Blackstone, S.R.; Iwelunmor, J. Determinants of contraceptive use among Nigerian couples: Evidence from the 2013 Demographic and Health Survey. Contracept. Reprod. Med. 2017, 2, 9. [Google Scholar] [CrossRef] [PubMed]
- Corsi, D.J.; Neuman, M.; Finlay, J.E.; Subramanian, S. Demographic and health surveys: A profile. Int. J. Epidemiol. 2012, 41, 1602–1613. [Google Scholar] [CrossRef] [PubMed]
- Rutstein, S.O.; Staveteig, S. Making the Demographic and Health Surveys Wealth Index Comparable; DHS Methodological Reports No. 9; ICF International: Rockville, MD, USA, 2014. [Google Scholar]
- Bain, L.E.; Amu, H.; Tarkang, E.E. Barriers and motivators of contraceptive use among young people in Sub-Saharan Africa: A systematic review of qualitative studies. PLoS ONE 2021, 16, e0252745. [Google Scholar] [CrossRef]
- Ankomah, A.; Anyanti, J.; Adebayo, S.B.; Giwa, A. Barriers to Contraceptive Use among Married Young Adults in Nigeria: A Qualitative Study. Int. J. Trop. Dis. 2014, 3, 267–282. [Google Scholar] [CrossRef]
- Sumankuuro, J.; Crockett, J.; Wang, S. Sociocultural barriers to maternity services delivery: A qualitative meta-synthesis of the literature. Public Health 2018, 157, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Ochako, R.; Mbondo, M.; Aloo, S.; Kaimenyi, S.; Thompson, R.; Temmerman, M.; Kays, M. Barriers to modern contraceptive methods uptake among young women in Kenya: A qualitative study. BMC Public Health 2015, 15, 118. [Google Scholar] [CrossRef]
- Muanda, M.F.; Ndongo, G.P.; Messina, L.J.; Bertrand, J.T. Barriers to modern contraceptive use in rural areas in DRC. Cult. Health Sex. 2017, 19, 1011–1023. [Google Scholar] [CrossRef]
- Blackstone, S.R.; Nwaozuru, U.; Iwelunmor, J. Factors Influencing Contraceptive Use in Sub-Saharan Africa: A Systematic Review. Int. Q. Community Health Educ. 2017, 37, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Pratley, P. Associations between quantitative measures of women’s empowerment and access to care and health status for mothers and their children: A systematic review of evidence from the developing world. Soc. Sci. Med. 2016, 169, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Van Rooyen, C.; Stewart, R.; de Wet, T. The Impact of Microfinance in Sub-Saharan Africa: A Systematic Review of the Evidence. World Dev. 2012, 40, 2249–2262. [Google Scholar] [CrossRef]
- United Nations. Trade as a Tool for the Economic Empowerment of Women. 2016. Available online: http://unctad.org/meetings/en/SessionalDocuments/ciem8d2_en.pdf (accessed on 20 July 2022).
- Liu, D.H.; Raftery, A.E. How do education and family planning accelerate fertility decline? Popul. Dev. Rev. 2020, 46, 409–441. [Google Scholar] [CrossRef] [PubMed]
- Asaolu, I.O.; Alaofè, H.; Gunn, J.K.L.; Adu, A.K.; Monroy, A.J.; Ehiri, J.E.; Hayden, M.H.; Ernest, K.C. Measuring Women’s Empowerment in Sub-Saharan Africa: Exploratory and Confirmatory Factor Analyses of the Demographic and Health Surveys. Front. Psychol. 2018, 9, 994. [Google Scholar] [CrossRef]
- Phan, L. Measuring Women’s Empowerment at Household Level Using DHS Data of Four Southeast Asian Countries. Soc. Indic. Res. 2016, 126, 359–378. [Google Scholar] [CrossRef]
- Ouida, C.; Jessica Davis, P.; Michaela, L.; Alison, T. Women’s Economic Empowerment in Sub-Saharan Africa Recommendations for Business Action. BSR (Business for Social Responsiblity). 2017. Available online: https://www.bsr.org/reports/BSR_Womens_Empowerment_Africa_Main_Report.pdf (accessed on 20 July 2022).
- Bakibinga, P.; Matanda, D.J.; Ayiko, R.; Rujumba, J.; Muiruri, C.; Amendah, D.; Atela, M. Pregnancy history and current use of contraception among women of reproductive age in Burundi, Kenya, Rwanda, Tanzania and Uganda: Analysis of demographic and health survey data. BMJ Open 2016, 6, e009991. [Google Scholar] [CrossRef]
- Kabagenyi, A.; Habaasa, G.; Rutaremwa, G. Low contraceptive use among young females in Uganda: Does birth history and age at birth have an influence? Analysis of 2011 Demographic and Health Survey. J. Contracept. Stud. 2016, 1, 4. [Google Scholar]
- Bishwajit, G.; Tang, S.; Yaya, S.; Ide, S.; Fu, H.; Wang, M.; He, Z.; Da, F.; Feng, Z. Factors associated with male involvement in reproductive care in Bangladesh. BMC Public Health 2017, 17, 3. [Google Scholar] [CrossRef]
- Ekholuenetale, M.; Barrow, A. Inequalities in out-of-pocket health expenditure among women of reproductive age: After-effects of national health insurance scheme initiation in Ghana. J. Egypt. Public Health Assoc. 2021, 96, 6. [Google Scholar] [CrossRef]
- Dagnew, G.W.; Asresie, M.B.; Fekadu, G.A.; Gelaw, Y.M. Modern contraceptive use and factors associated with use among postpartum women in Ethiopia; further analysis of the 2016 Ethiopia demographic and health survey data. BMC Public Health 2020, 20, 661. [Google Scholar] [CrossRef] [PubMed]
- Alkema, L.; Kantorova, V.; Menozzi, C.; Biddlecom, A. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: A systematic and comprehensive analysis. Lancet 2013, 381, 1642–1652. [Google Scholar] [CrossRef]
- Elfstrom, K.M.; Stephenson, R. The Role of Place in Shaping Contraceptive Use among Women in Africa. PLoS ONE 2012, 7, e40670. [Google Scholar] [CrossRef]
- Adebayo, S.B.; Gayawan, E.; Ujuju, C.; Ankomah, A. Modelling geographical variations and determinants of use of modern family planning methods among women of reproductive age in Nigeria. J. Biosoc. Sci. 2013, 45, 57–77. [Google Scholar] [CrossRef] [PubMed]
| Country | Survey Year | Total Sample Size | Percentage of Women from the Total Sample Size | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (5-Year Groups) | Residence | Education (Groups) | Wealth Quintile | Marital Status | |||||||||||||||||||||
| 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | Urban | Rural | No Education or Primary | Secondar y or Higher | Lowest | Second | Middle | Fourth | Highest | Never Married | Married | Living Together | Divorced/Separate d | Widowed | Married or Living Together | Widowed, Divorced, Separated | |||
| Angola | 2015–16 DHS | 14,379 | 24 | 21.2 | 17.1 | 12.5 | 10.5 | 8.6 | 6.2 | 69.6 | 30.4 | 56.9 | 43.1 | 16.9 | 17.6 | 19.5 | 22.5 | 23.6 | 35.2 | 10.8 | 44.5 | 7.4 | 2 | 55.3 | 9.4 |
| Benin | 2017–18 DHS | 15,928 | 21 | 18.4 | 18.7 | 13.8 | 11.8 | 8.3 | 7.9 | 42.4 | 57.6 | 74.9 | 25.1 | 17.2 | 19 | 19.5 | 21.4 | 22.9 | 24.4 | 55.1 | 15 | 3.4 | 2 | 70.1 | 5.5 |
| Burkina Faso | 2010 DHS | 17,087 | 19.4 | 19.4 | 17.3 | 15.1 | 11.7 | 9.6 | 7.5 | 27.1 | 72.9 | 87.6 | 12.4 | 17.5 | 18.7 | 19 | 19.9 | 24.9 | 17.5 | 75.6 | 3.8 | 1.3 | 1.8 | 79.4 | 3.1 |
| Burundi | 2016–17 DHS | 17,269 | 22.3 | 18.8 | 17.4 | 14.1 | 11.4 | 8.9 | 7 | 12.9 | 87.1 | 75.5 | 24.5 | 19.2 | 19.9 | 20 | 19.5 | 21.4 | 34.6 | 41.8 | 14.8 | 5.1 | 3.7 | 56.6 | 8.8 |
| Cameroon | 2018 DHS | 14,677 | 24.3 | 17.8 | 17.8 | 14.5 | 11 | 8 | 6.6 | 55.4 | 44.6 | 47.1 | 52.9 | 16.4 | 18.4 | 19.8 | 21.6 | 23.8 | 34.5 | 43.9 | 13 | 5.9 | 2.7 | 56.9 | 8.6 |
| Chad | 2014–15 DHS | 17,719 | 22.2 | 17.3 | 18.3 | 14.5 | 11.6 | 8.5 | 7.6 | 23.8 | 76.2 | 85.1 | 14.9 | 19 | 19.5 | 19.6 | 20.2 | 21.6 | 16.6 | 68.1 | 6.8 | 5.3 | 3.3 | 74.8 | 8.6 |
| Comoros | 2012 DHS | 5329 | 24.7 | 18.7 | 16.9 | 14 | 11.8 | 8.5 | 5.5 | 33.1 | 66.9 | 50.6 | 49.1 | 16.3 | 20.1 | 20.5 | 21.1 | 22 | 32.3 | 55.6 | 5.6 | 5.8 | 0.7 | 61.2 | 6.5 |
| Congo | 2011–12 DHS | 10,819 | 20.3 | 18.8 | 18.7 | 14.4 | 12.6 | 8.4 | 6.9 | 68.6 | 31.4 | 29.6 | 70.4 | 16.7 | 19.6 | 20.7 | 21.7 | 21.3 | 25.9 | 10.7 | 47.4 | 14.1 | 1.9 | 58.1 | 16 |
| Congo Democratic Republic | 2013–14 DHS | 18,827 | 21.5 | 19.6 | 18.8 | 13.9 | 11.6 | 8.1 | 6.4 | 38.4 | 61.6 | 52.3 | 47.7 | 18.6 | 19.1 | 18.6 | 19.4 | 24.3 | 26 | 46.5 | 17.7 | 7.5 | 2.2 | 64.2 | 9.7 |
| Cote d’Ivoire | 2011–12 DHS | 10,060 | 20.1 | 19.4 | 19.1 | 15 | 11.2 | 8.5 | 6.7 | 51.4 | 48.6 | 78.6 | 21.4 | 17.6 | 17.3 | 18.2 | 20.8 | 26.2 | 30.2 | 39.3 | 23.4 | 4.9 | 2.2 | 62.7 | 7.1 |
| Eswatini | 2006–07 DHS | 4987 | 25.5 | 21 | 14.6 | 12.3 | 10.1 | 8.8 | 7.7 | 26.7 | 73.3 | 40.7 | 59.3 | 15.7 | 17.3 | 19.4 | 22.3 | 25.3 | 49.9 | 31.9 | 9.5 | 3.2 | 5.6 | 41.3 | 8.8 |
| Ethiopia | 2016 DHS | 15,683 | 21.6 | 17.6 | 18.9 | 15 | 12.3 | 8.2 | 6.5 | 22.2 | 77.8 | 82.8 | 17.2 | 16.8 | 17.9 | 19 | 19.8 | 26.5 | 25.7 | 63.9 | 1.3 | 6.3 | 2.7 | 65.2 | 9.1 |
| Gabon | 2012 DHS | 8422 | 21.2 | 19.4 | 17.6 | 14.4 | 11.7 | 8.9 | 6.8 | 88.6 | 11.4 | 25.6 | 74.4 | 14.5 | 19.3 | 21.2 | 22.3 | 22.7 | 36.2 | 19 | 34.2 | 9.1 | 1.6 | 53.1 | 10.7 |
| Gambia | 2019–20 DHS | 11,865 | 22.2 | 18.4 | 18.9 | 13.6 | 12.1 | 8.7 | 6 | 73.7 | 26.3 | 50.3 | 49.7 | 16.8 | 18 | 19.3 | 21.8 | 24 | 31.2 | 63.2 | 0.2 | 3.8 | 1.5 | 63.4 | 5.4 |
| Ghana | 2014 DHS | 9396 | 17.3 | 17.2 | 17.1 | 14.6 | 13.8 | 11 | 9.1 | 53.8 | 46.2 | 36.9 | 63.1 | 16.1 | 17.4 | 20.6 | 22.5 | 23.3 | 32.9 | 42.2 | 14.4 | 7.7 | 2.7 | 56.6 | 10.4 |
| Guinea | 2018 DHS | 10,874 | 24 | 16.2 | 17.5 | 13.2 | 12.1 | 8.7 | 8.3 | 37.6 | 62.4 | 80.4 | 19.6 | 18.9 | 19.7 | 18.9 | 19.8 | 22.7 | 25.2 | 68.8 | 2.3 | 2.1 | 1.7 | 71.1 | 3.7 |
| Kenya | 2014 DHS | 31,079 | 18.7 | 18.5 | 19.6 | 14.5 | 12.1 | 9.3 | 7.3 | 40.8 | 59.2 | 57.3 | 42.7 | 15.6 | 17.6 | 19.4 | 21.1 | 26.4 | 28.9 | 54.6 | 5.1 | 7.7 | 3.7 | 59.7 | 11.4 |
| Lesotho | 2014 DHS | 6621 | 21.7 | 20 | 16.5 | 14.5 | 11.2 | 8.5 | 7.5 | 36.5 | 63.5 | 39.6 | 60.4 | 14.5 | 15.6 | 18.8 | 24.2 | 26.9 | 33.1 | 53.6 | 1 | 5.4 | 7 | 54.6 | 12.4 |
| Liberia | 2019–20 DHS | 8065 | 20.5 | 18.7 | 17 | 13.8 | 12.6 | 9.5 | 7.8 | 62.3 | 37.7 | 54.4 | 45.6 | 17.1 | 17.7 | 18.8 | 22.7 | 23.7 | 38.8 | 25.6 | 26.6 | 7.2 | 1.7 | 52.3 | 8.9 |
| Madagascar | 2008–09 DHS | 17,375 | 22.8 | 16.2 | 15.9 | 14.4 | 12.3 | 10 | 8.5 | 17.3 | 82.7 | 67.9 | 32.1 | 18 | 18.2 | 18.9 | 20.1 | 24.8 | 18.1 | 60.5 | 8.8 | 10.7 | 1.9 | 69.3 | 12.6 |
| Malawi | 2015–16 DHS | 24,562 | 21.4 | 21 | 16.1 | 14.9 | 11.9 | 8.3 | 6.4 | 18.3 | 81.7 | 74.2 | 25.8 | 19.3 | 19.1 | 18.9 | 19.1 | 23.7 | 21 | 61.7 | 4 | 10.4 | 2.9 | 65.7 | 13.3 |
| Mali | 2018 DHS | 10,519 | 20 | 18 | 19.1 | 15.3 | 13.2 | 8.5 | 6 | 26.3 | 73.7 | 78.7 | 21.3 | 17.5 | 18.8 | 19.1 | 21.1 | 23.4 | 16 | 80.7 | 0.7 | 1.4 | 1.2 | 81.4 | 2.6 |
| Mauritania | 2019–21 DHS | 15,714 | 23.5 | 17.2 | 16.7 | 14 | 11.9 | 9.4 | 7.3 | 51.2 | 48.8 | 71.3 | 28.7 | 17.2 | 18.2 | 20 | 22.1 | 22.5 | 26.6 | 62.5 | 9.4 | 1.5 | 62.5 | 10.8 | |
| Mozambique | 2015 AIS | 7749 | 21.6 | 20 | 15.7 | 12.5 | 12.8 | 9.3 | 8.1 | 35.2 | 64.8 | 77.2 | 22.8 | 19.3 | 18.9 | 18.2 | 20.6 | 23 | 17 | 36.9 | 29.1 | 12.8 | 4.1 | 66 | 16.9 |
| Namibia | 2013 DHS | 10,018 | 20.8 | 19.5 | 16.2 | 13.7 | 12.1 | 10 | 7.7 | 56.6 | 43.4 | 24.2 | 75.8 | 15.6 | 17.7 | 19.6 | 23.1 | 24.1 | 59.5 | 17.9 | 16.1 | 4.4 | 2.1 | 34 | 6.5 |
| Niger | 2012 DHS | 11,160 | 16.4 | 17.8 | 20.4 | 16.6 | 12.9 | 8.9 | 7 | 18.8 | 81.2 | 91.4 | 8.5 | 18.1 | 18.8 | 19.7 | 20.6 | 22.8 | 7.9 | 88.4 | 0.2 | 2.5 | 1.1 | 88.5 | 3.6 |
| Nigeria | 2018 DHS | 41,821 | 20.2 | 16.3 | 17.3 | 14.8 | 13.1 | 9.4 | 8.9 | 45.8 | 54.2 | 49.4 | 50.6 | 17.3 | 19.2 | 19.6 | 21.5 | 22.4 | 25.2 | 67.2 | 2.3 | 2.7 | 2.5 | 69.6 | 5.2 |
| Rwanda | 2019–20 DHS | 14,634 | 22.3 | 16.5 | 14.2 | 14.5 | 14.2 | 10.2 | 8.3 | 19.9 | 80.1 | 67.7 | 32.3 | 18.7 | 18.8 | 18.8 | 20.3 | 23.3 | 40.4 | 32.1 | 18.4 | 6.4 | 2.6 | 50.6 | 9 |
| Sao Tome and Principe | 2008–09 DHS | 2615 | 21.2 | 17.6 | 17.3 | 15.2 | 9.9 | 10.8 | 8.1 | 54.8 | 45.2 | 63.9 | 36.1 | 17.7 | 19.7 | 18.2 | 21.3 | 23.1 | 23.1 | 3.6 | 62.1 | 10.8 | 0.3 | 65.7 | 11.1 |
| Senegal | 2019 DHS | 8649 | 22 | 19.1 | 16 | 14.9 | 12.5 | 8.4 | 7 | 48.9 | 51.1 | 68.3 | 31.7 | 16.4 | 17.7 | 19.5 | 21.6 | 24.9 | 29.8 | 65.3 | 0.1 | 4 | 0.7 | 65.4 | 4.8 |
| Sierra Leone | 2019 DHS | 15,574 | 22 | 16.9 | 17.5 | 12.5 | 14.3 | 8.6 | 8.3 | 46 | 54 | 59 | 41 | 17.6 | 18.2 | 19 | 21.7 | 23.5 | 32.5 | 58.5 | 3.9 | 2.9 | 2.3 | 62.4 | 5.1 |
| South Africa | 2016 DHS | 8514 | 16.8 | 16.6 | 17 | 15.7 | 12.6 | 11 | 10.4 | 67.3 | 32.7 | 11.1 | 88.9 | 19.4 | 20.1 | 21.2 | 20.7 | 18.6 | 58.6 | 23.3 | 12.5 | 3.4 | 2.2 | 35.8 | 5.5 |
| Tanzania | 2015–16 DHS | 13,266 | 21.9 | 18.7 | 16 | 13.2 | 12.4 | 10.3 | 7.5 | 36.3 | 63.7 | 76.6 | 23.4 | 16.9 | 17.1 | 17.6 | 21.3 | 27.1 | 25.3 | 44.9 | 17 | 10 | 2.9 | 61.9 | 12.8 |
| Togo | 2013–14 DHS | 9480 | 17.9 | 17.6 | 17.8 | 15 | 13.7 | 9.7 | 8.3 | 45.4 | 54.6 | 65.2 | 34.8 | 16.6 | 16.9 | 18.2 | 22.8 | 25.5 | 26.8 | 51.4 | 14.9 | 4.2 | 2.6 | 66.3 | 6.9 |
| Uganda | 2016 DHS | 18,506 | 23 | 20.7 | 16.5 | 13.7 | 10.9 | 8.7 | 6.5 | 26.7 | 73.3 | 67.1 | 32.9 | 17.5 | 18.4 | 18.7 | 19.9 | 25.5 | 25.8 | 30.3 | 30.3 | 10.7 | 2.8 | 60.6 | 13.5 |
| Zambia | 2018 DHS | 13,683 | 21.9 | 20 | 16.4 | 13.6 | 12.4 | 9.2 | 6.6 | 46.6 | 53.4 | 52 | 48 | 17.8 | 17.4 | 18.1 | 22 | 24.6 | 31.2 | 55.4 | 0.5 | 10 | 2.9 | 55.9 | 12.9 |
| Zimbabwe | 2015 DHS | 9955 | 22.1 | 17 | 16.6 | 16.3 | 12.4 | 9.7 | 5.9 | 38.5 | 61.5 | 27.1 | 72.9 | 17.1 | 17 | 17.6 | 23.2 | 25.1 | 25.2 | 58.7 | 3.1 | 8.6 | 4.4 | 61.8 | 13 |
| Country | Residence (%) | Education (%) | Wealth Quintile (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | No Education or Primary | Secondary or Higher | Lowest | Second | Middle | Fourth | Highest | |
| Angola | 17.1 | 1.9 | 4.7 | 22.7 | 1.1 | 3 | 9.3 | 17.2 | 25.7 |
| Benin | 13.7 | 10.2 | 10.7 | 14.6 | 8.7 | 9.2 | 11.3 | 12.3 | 15.6 |
| Burkina Faso | 25.9 | 9.9 | 12 | 30.4 | 6.4 | 8 | 8.9 | 15.3 | 27.7 |
| Burundi | 15.9 | 14.4 | 16.2 | 9.5 | 14.9 | 14.8 | 14.4 | 12.7 | 15.9 |
| Cameroon | 20.5 | 11.3 | 10.4 | 21.7 | 4.8 | 12.9 | 17.3 | 20.3 | 22.7 |
| Chad | 9.6 | 3.4 | 3.8 | 11.1 | 3.5 | 3.8 | 3.7 | 2.7 | 9.9 |
| Comoros | 14.6 | 7.5 | 10.2 | 9.5 | 7.7 | 8.8 | 11.1 | 12.3 | 8.9 |
| Congo | 26.6 | 12.9 | 14.8 | 25.4 | 10.1 | 18.5 | 22.8 | 27.4 | 29.6 |
| Congo Democratic Republic | 13.1 | 5 | 4.7 | 11.8 | 3.6 | 5 | 5 | 11.2 | 14 |
| Cote d’Ivoire | 17.4 | 10.2 | 11.8 | 21.8 | 7.6 | 10.1 | 13.5 | 16.2 | 19.2 |
| Eswatini | 44.1 | 33.5 | 30.1 | 40.5 | 25.9 | 31.7 | 38.7 | 36.6 | 43.9 |
| Ethiopia | 27.2 | 24.2 | 25.3 | 22.7 | 16 | 24 | 27 | 28.1 | 27.1 |
| Gabon | 25.3 | 13.8 | 14 | 27.4 | 14.7 | 21.9 | 22.3 | 26.8 | 30.3 |
| Gambia | 12.3 | 12.1 | 14.3 | 10.1 | 12.6 | 11.6 | 12.5 | 13.6 | 11 |
| Ghana | 16 | 20.6 | 19 | 17.7 | 17.8 | 20.5 | 21 | 16.5 | 15.8 |
| Guinea | 16.5 | 8.4 | 9.9 | 17.8 | 4.5 | 8.6 | 10.6 | 15.1 | 17.1 |
| Kenya | 41.5 | 37.5 | 39.8 | 38.3 | 23.5 | 40 | 43 | 44.4 | 40.7 |
| Lesotho | 51 | 47.1 | 47.6 | 49.2 | 41.6 | 47.1 | 50.2 | 50.6 | 50.1 |
| Liberia | 25.3 | 25.3 | 21.8 | 29.5 | 22.3 | 25.2 | 27.1 | 27.8 | 23.7 |
| Madagascar | 25.7 | 22.4 | 22.4 | 24.2 | 15.4 | 20.1 | 23.2 | 27.9 | 26.5 |
| Malawi | 43.4 | 45.5 | 47.1 | 39.7 | 42.2 | 48.4 | 46.8 | 46.7 | 42.3 |
| Mali | 19.7 | 13.9 | 13.4 | 22.9 | 10 | 10 | 15.4 | 19.4 | 20.3 |
| Mozambique | 34.1 | 21.2 | 21.7 | 39.2 | 16.7 | 17 | 18.9 | 30.9 | 41.2 |
| Namibia | 55.1 | 42.7 | 40.6 | 52.6 | 38.9 | 48.5 | 52.4 | 52.1 | 53.1 |
| Niger | 19.4 | 9.1 | 10.4 | 16.9 | 8.1 | 7.2 | 8 | 11.6 | 18.4 |
| Nigeria | 14 | 7.6 | 6.4 | 14.6 | 3.5 | 5.9 | 9.8 | 14.4 | 16.9 |
| Rwanda | 30.4 | 36.3 | 40.3 | 24.2 | 40.8 | 36.7 | 38 | 35.6 | 26.6 |
| Sao Tome and Principe | 23.7 | 31.9 | 29.2 | 24.4 | 24.6 | 27.1 | 27.1 | 29.2 | 28.6 |
| Senegal | 18.9 | 16.9 | 19.8 | 13.7 | 14.4 | 17 | 19.4 | 19.2 | 18.6 |
| Sierra Leone | 27.5 | 20.8 | 18.4 | 31.8 | 18.3 | 19.9 | 24.9 | 29.3 | 25.5 |
| South Africa | 48.2 | 47.2 | 40.8 | 48.8 | 46.3 | 49.7 | 50 | 49.1 | 43.8 |
| Tanzania | 28.8 | 26.2 | 28.5 | 22.7 | 19 | 24.9 | 30.6 | 32.1 | 27.5 |
| Togo | 19 | 14.8 | 14.3 | 21.2 | 13.6 | 15.5 | 14.9 | 17.7 | 20 |
| Uganda | 30.5 | 26.1 | 25.7 | 30.5 | 18.9 | 25.5 | 28.2 | 31 | 30.8 |
| Zambia | 34.2 | 34 | 35.1 | 33 | 31.3 | 33.7 | 37.4 | 37.7 | 30.7 |
| Zimbabwe | 47.6 | 48.1 | 49.9 | 47.1 | 48.7 | 49 | 45.7 | 50.8 | 45.3 |
| Country | Residence (%) | Education (%) | Wealth Quintile (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | No Education or Primary | Secondary or Higher | Lowest | Second | Middle | Fourth | Highest | |
| Angola | 18.4 | 1.8 | 5.3 | 26.8 | 1 | 2.6 | 8.9 | 18.5 | 30.7 |
| Benin | 14.5 | 11 | 11.6 | 16.6 | 9.4 | 9.9 | 11.9 | 12.9 | 17.9 |
| Burkina Faso | 30.8 | 10.8 | 12.9 | 44.2 | 7.1 | 8.6 | 9.7 | 16.3 | 33.6 |
| Burundi | 28.5 | 22.3 | 22.3 | 28.5 | 22.2 | 22.5 | 22.7 | 20 | 27.6 |
| Cameroon | 20.7 | 10.6 | 9.9 | 23.6 | 4.2 | 13 | 17.2 | 19.8 | 24.3 |
| Chad | 10.1 | 3.8 | 4.1 | 13.7 | 3.8 | 4.1 | 4.3 | 3.1 | 10.6 |
| Comoros | 20.6 | 11 | 12.3 | 17.4 | 10.9 | 13.2 | 14.1 | 17.8 | 14.2 |
| Congo | 24.6 | 11.7 | 14.6 | 22.8 | 9.5 | 15.4 | 22.7 | 22.9 | 28.8 |
| Congo Democratic Republic | 14.6 | 4.6 | 4.6 | 12.9 | 3.3 | 4.7 | 4.5 | 11 | 17.2 |
| Cote d’Ivoire | 16.3 | 9.8 | 11.5 | 19.9 | 7.4 | 9.7 | 11.3 | 15 | 20.1 |
| Eswatini | 55.8 | 44.8 | 37.1 | 56.9 | 35.7 | 40.7 | 50.3 | 47.2 | 59 |
| Ethiopia | 49.8 | 32.4 | 33.4 | 50.7 | 19.5 | 31 | 36.7 | 40.6 | 47.4 |
| Gabon | 20.7 | 11.3 | 12.3 | 22.8 | 11.9 | 18.8 | 20.2 | 22.1 | 21.9 |
| Gambia | 17.9 | 15.3 | 16.4 | 18.4 | 15.7 | 15.3 | 16.2 | 20.5 | 17.7 |
| Ghana | 19.8 | 24.6 | 21.2 | 23.1 | 21.2 | 24.9 | 24 | 22.1 | 19.5 |
| Guinea | 15.5 | 8.4 | 9.5 | 19.1 | 4.4 | 9.1 | 9.6 | 14.5 | 17.1 |
| Kenya | 56.9 | 50.9 | 49.9 | 59 | 29.2 | 54.1 | 59.5 | 60.9 | 57.7 |
| Lesotho | 65.2 | 57.3 | 55 | 63.8 | 49.9 | 56.3 | 62.3 | 60.8 | 65.9 |
| Liberia | 22.4 | 25.6 | 21.8 | 27.7 | 23.5 | 25.2 | 23.2 | 29 | 18.4 |
| Madagascar | 35.6 | 28 | 27.1 | 34.4 | 17.6 | 23.8 | 29.2 | 36.4 | 36.4 |
| Malawi | 61.4 | 57.5 | 58.1 | 58.4 | 53.2 | 58 | 58.8 | 59.6 | 60.6 |
| Mali | 21.4 | 15 | 14.2 | 28.7 | 11 | 10.7 | 16.5 | 20 | 23.5 |
| Mauritania | 19.9 | 7 | 10.9 | 20.8 | 4.5 | 7.6 | 11.8 | 18.2 | 23 |
| Mozambique | 34.3 | 21.5 | 22.6 | 39.2 | 16.7 | 17.4 | 20.3 | 31.1 | 43 |
| Namibia | 60.5 | 48 | 45 | 59.8 | 42.1 | 53 | 56.8 | 58.4 | 62.3 |
| Niger | 27 | 9.7 | 11.2 | 30 | 8.7 | 7.7 | 8.3 | 12.8 | 23.7 |
| Nigeria | 18.2 | 7.8 | 6.9 | 19.9 | 3.7 | 6.3 | 11.2 | 18 | 22.3 |
| Rwanda | 55 | 59.2 | 59 | 56.5 | 60.2 | 60.6 | 60.8 | 59.2 | 51.8 |
| Sao Tome and Principe | 28 | 40.1 | 34.5 | 31.5 | 31.1 | 32.3 | 30.9 | 36.8 | 36.8 |
| Senegal | 32.4 | 20.9 | 24.4 | 30.7 | 16.6 | 21.2 | 27.3 | 30.2 | 32.6 |
| Sierra Leone | 25.8 | 18.1 | 18.1 | 29.2 | 15.8 | 17.9 | 20.8 | 25.9 | 25.8 |
| South Africa | 54.6 | 52.5 | 39.5 | 56.3 | 53.6 | 50.5 | 53.3 | 57.8 | 55.1 |
| Tanzania | 35.2 | 30.6 | 31.8 | 33.2 | 20.3 | 27.9 | 35.8 | 40.4 | 35.4 |
| Togo | 18.8 | 16.3 | 16 | 21.4 | 15.5 | 16.7 | 16.7 | 16.4 | 20.8 |
| Uganda | 40.6 | 33 | 32.2 | 41.1 | 22.4 | 32.2 | 35.8 | 40.2 | 42.1 |
| Zambia | 52.6 | 44 | 44.5 | 52.1 | 38 | 43.4 | 51.1 | 53.6 | 51.3 |
| Zimbabwe | 70.7 | 63.2 | 60.2 | 68.3 | 61.8 | 61.5 | 63.1 | 68.7 | 72.3 |
| Country | Residence (%) | Education (%) | Wealth Quintile (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | No Education or Primary | Secondary or Higher | Lowest | Second | Middle | Fourth | Highest | |
| Angola | 31.5 | 4.6 | 11.5 | 42.8 | 2.9 | 6.1 | 16.2 | 31.2 | 48.4 |
| Benin | 28.1 | 24.3 | 25.1 | 29.7 | 23.4 | 22 | 24.9 | 25.7 | 31.9 |
| Burkina Faso | 54.9 | 29.5 | 33.1 | 67.2 | 22.3 | 24.4 | 26.6 | 38.8 | 57.9 |
| Burundi | 48.4 | 38.3 | 38.2 | 49 | 39.4 | 38.9 | 39 | 34.4 | 45.4 |
| Cameroon | 42.2 | 29.2 | 28.1 | 44.4 | 15 | 32.3 | 37.7 | 41 | 47.2 |
| Chad | 27.1 | 14.3 | 15.1 | 32.4 | 13.6 | 15.3 | 16.5 | 12.4 | 27.7 |
| Comoros | 38.3 | 21.8 | 25 | 31.2 | 19.8 | 25.8 | 26.8 | 33.9 | 29.7 |
| Congo | 38.4 | 19.1 | 23.3 | 35.9 | 16 | 24.5 | 36.8 | 34.3 | 44.8 |
| Congo Democratic Republic | 24.6 | 10.8 | 10.8 | 22.7 | 8 | 10.9 | 9.9 | 21.6 | 27.6 |
| Cote d’Ivoire | 33.9 | 22.5 | 25.6 | 40.8 | 18.3 | 21.6 | 24.6 | 30.6 | 42.6 |
| Eswatini | 70.6 | 60.5 | 53 | 71.2 | 49.8 | 58.8 | 63.7 | 62.5 | 74.3 |
| Ethiopia | 78.6 | 56.7 | 58.3 | 77.2 | 42.2 | 52.9 | 60.3 | 66 | 75.2 |
| Gabon | 35.4 | 21.3 | 24.5 | 37.2 | 22 | 31.7 | 34.1 | 38.2 | 38.6 |
| Gambia | 40.8 | 37 | 38 | 42.6 | 38.5 | 35.4 | 37.5 | 46.1 | 40.5 |
| Ghana | 36.3 | 41.9 | 40 | 38.7 | 39.8 | 41.8 | 40.9 | 37.5 | 36.6 |
| Guinea | 41.5 | 27.2 | 29.7 | 46.3 | 16.1 | 29.5 | 29.3 | 38.2 | 45.9 |
| Kenya | 76.7 | 66.7 | 67 | 76.7 | 45.6 | 66.4 | 72.8 | 78.2 | 78.8 |
| Lesotho | 82.4 | 73.1 | 70.9 | 80.3 | 66.6 | 70.6 | 78.2 | 77.5 | 82.7 |
| Liberia | 38.5 | 43.6 | 39.4 | 43.3 | 40.9 | 41.7 | 40 | 44.6 | 36 |
| Madagascar | 49.9 | 49.4 | 50.4 | 47.8 | 41 | 47.7 | 50.9 | 55.1 | 49.3 |
| Malawi | 77.5 | 74 | 74.4 | 75.2 | 71 | 73.8 | 75.1 | 75.5 | 77.2 |
| Mali | 49.2 | 37 | 35.5 | 60.1 | 26.5 | 29.3 | 39.5 | 47 | 54.2 |
| Mauritania | 40.1 | 16.7 | 24.8 | 40.2 | 11.4 | 17.4 | 25.7 | 37.3 | 46.3 |
| Mozambique | 60 | 45.5 | 47 | 64.6 | 38 | 38.6 | 45.2 | 58 | 66 |
| Namibia | 80.6 | 66.9 | 63.8 | 79.7 | 60.9 | 72 | 74.2 | 77.3 | 85.2 |
| Niger | 58.3 | 35.7 | 38.8 | 62.6 | 31.5 | 31.8 | 33.4 | 41 | 56.7 |
| Nigeria | 39.4 | 27.7 | 25.5 | 40.9 | 17.8 | 25 | 31.4 | 38.3 | 43.2 |
| Rwanda | 73 | 75.6 | 74.6 | 77.3 | 75.7 | 76.2 | 77.1 | 75.2 | 71.5 |
| Sao Tome and Principe | 37.1 | 52.3 | 45.8 | 40.3 | 39.1 | 43.1 | 41 | 49.4 | 48.2 |
| Senegal | 59.6 | 46.8 | 51 | 59 | 40.6 | 45.7 | 56.6 | 54.5 | 62.8 |
| Sierra Leone | 50 | 42.3 | 41.9 | 53.6 | 39.7 | 41 | 45.4 | 50.4 | 50.3 |
| South Africa | 78.6 | 75.4 | 65.5 | 79.4 | 76.7 | 72.7 | 80.2 | 80.4 | 78.7 |
| Tanzania | 53.5 | 52.6 | 53.3 | 51.1 | 39.2 | 48.9 | 57.2 | 62.5 | 53.8 |
| Togo | 34.2 | 31 | 30.6 | 37.2 | 30 | 31.5 | 31.6 | 29.7 | 38 |
| Uganda | 59 | 49.3 | 48.5 | 59 | 36.3 | 48.2 | 52 | 58.8 | 60 |
| Zambia | 73.4 | 65.1 | 64.5 | 74.7 | 59.5 | 63.1 | 71.7 | 74.5 | 72.6 |
| Zimbabwe | 87.3 | 84.1 | 80.3 | 87.4 | 80.4 | 82.5 | 86.4 | 85.9 | 90.3 |
| Country | Residence (%) | Education (%) | Wealth Quintile (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | No Education or Primary | Secondary or Higher | Lowest | Second | Middle | Fourth | Highest | |
| Angola | 5.3 | 8.2 | 7.5 | 4.5 | 8.5 | 8.2 | 6.8 | 4.7 | 4 |
| Benin | 5.2 | 6.1 | 6.1 | 4.2 | 7 | 6.2 | 6.1 | 5.3 | 4.2 |
| Burkina Faso | 3.9 | 6.7 | 6.4 | 3.1 | 7.1 | 6.9 | 6.7 | 6.2 | 3.7 |
| Burundi | 4.1 | 5.7 | 6.1 | 4.1 | 6 | 6 | 5.5 | 5.8 | 4.4 |
| Cameroon | 3.8 | 6 | 5.9 | 3.8 | 6.6 | 6 | 5.1 | 4 | 3 |
| Chad | 5.4 | 6.8 | 6.7 | 4.8 | 7 | 7 | 6.8 | 6.2 | 5.3 |
| Comoros | 3.5 | 4.8 | 5.5 | 3.1 | 6.7 | 4.6 | 4.2 | 3.5 | 3.4 |
| Congo | 4.5 | 6.5 | 6.6 | 4.5 | 7 | 6.1 | 4.9 | 4.1 | 3.8 |
| Congo Democratic Republic | 5.4 | 7.3 | 7.5 | 5.6 | 7.6 | 7.4 | 7.1 | 6.5 | 4.9 |
| Cote d’Ivoire | 3.7 | 6.3 | 5.5 | 2.6 | 6.7 | 6.4 | 5.3 | 4.5 | 2.9 |
| Eswatini | 3 | 4.2 | 4.6 | 3.4 | 5.5 | 5 | 3.9 | 3.3 | 2.6 |
| Ethiopia | 2.3 | 5.2 | 5 | 2.1 | 6.4 | 5.6 | 4.9 | 4.3 | 2.6 |
| Gabon | 3.9 | 6.1 | 5.7 | 3.6 | 6.6 | 4.6 | 3.8 | 3.5 | 2.9 |
| Gambia | 3.9 | 5.9 | 5.5 | 3.4 | 6 | 5.2 | 4.6 | 3.8 | 3.2 |
| Ghana | 3.4 | 5.1 | 5.5 | 3.5 | 6.3 | 5.5 | 3.9 | 3.5 | 2.8 |
| Guinea | 3.8 | 5.5 | 5.1 | 3.5 | 5.9 | 5.5 | 4.9 | 4.7 | 3.4 |
| Kenya | 3.1 | 4.5 | 4.7 | 3 | 6.4 | 4.7 | 3.8 | 3.1 | 2.8 |
| Lesotho | 2.3 | 3.9 | 3.9 | 2.9 | 5 | 3.9 | 3.8 | 2.7 | 2.1 |
| Liberia | 3.4 | 5.5 | 5.1 | 3.2 | 6.2 | 5.3 | 4.2 | 3.3 | 2.8 |
| Madagascar | 2.9 | 5.2 | 5.6 | 3.1 | 6.8 | 5.9 | 5.1 | 4.4 | 2.7 |
| Malawi | 3 | 4.7 | 4.9 | 3.2 | 5.7 | 5.2 | 4.6 | 4.1 | 2.9 |
| Mali | 4.9 | 6.8 | 6.7 | 4.5 | 7.5 | 7.2 | 7 | 5.5 | 4.6 |
| Mauritania | 4.1 | 6.4 | 5.8 | 3.6 | 7.6 | 6.4 | 5.1 | 4.3 | 3.5 |
| Mozambique | 3.6 | 6.1 | 5.8 | 3.2 | 6.1 | 6.6 | 6.2 | 4.8 | 3.1 |
| Namibia | 2.9 | 4.7 | 4.9 | 3.3 | 5.5 | 4.4 | 3.9 | 3.1 | 2.3 |
| Niger | 5.6 | 8.1 | 7.9 | 4.9 | 8.2 | 8 | 8 | 8.1 | 6.1 |
| Nigeria | 4.5 | 5.9 | 6.5 | 4.2 | 6.7 | 6.2 | 5.6 | 4.6 | 3.8 |
| Rwanda | 3.4 | 4.3 | 4.4 | 3.7 | 4.9 | 4.4 | 4.2 | 4 | 3.4 |
| Sao Tome and Principe | 4.4 | 5.5 | 5.5 | 4.2 | 5.6 | 5.4 | 5.7 | 4.3 | 3.9 |
| Senegal | 3.8 | 5.6 | 5.4 | 3.6 | 6.8 | 5.6 | 4.6 | 4 | 3.4 |
| Sierra Leone | 3.1 | 5.1 | 5 | 3 | 5.6 | 5.1 | 4.7 | 3.6 | 2.6 |
| South Africa | 2.4 | 3.1 | 3.4 | 2.6 | 3.1 | 2.9 | 2.7 | 2.3 | 2.1 |
| Tanzania | 3.8 | 6 | 5.7 | 3.6 | 7.5 | 6.5 | 5.7 | 4.5 | 3.1 |
| Togo | 3.7 | 5.7 | 5.5 | 3.5 | 6.3 | 5.8 | 5.4 | 3.9 | 3.5 |
| Uganda | 4 | 5.9 | 6 | 4.2 | 7.1 | 6.3 | 5.6 | 4.9 | 3.8 |
| Zambia | 3.4 | 5.8 | 5.7 | 3.6 | 6.7 | 5.9 | 4.9 | 3.7 | 3 |
| Zimbabwe | 3 | 4.7 | 5.1 | 3.7 | 5.6 | 4.9 | 4.5 | 3.7 | 2.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ekholuenetale, M.; Owobi, O.U.; Shishi, B.T. Socioeconomic Position in Modern Contraceptive Uptake and Fertility Rate among Women of Childbearing Age in 37 Sub-Saharan Countries. World 2022, 3, 858-875. https://doi.org/10.3390/world3040048
Ekholuenetale M, Owobi OU, Shishi BT. Socioeconomic Position in Modern Contraceptive Uptake and Fertility Rate among Women of Childbearing Age in 37 Sub-Saharan Countries. World. 2022; 3(4):858-875. https://doi.org/10.3390/world3040048
Chicago/Turabian StyleEkholuenetale, Michael, Olah Uloko Owobi, and Benedict Terfa Shishi. 2022. "Socioeconomic Position in Modern Contraceptive Uptake and Fertility Rate among Women of Childbearing Age in 37 Sub-Saharan Countries" World 3, no. 4: 858-875. https://doi.org/10.3390/world3040048
APA StyleEkholuenetale, M., Owobi, O. U., & Shishi, B. T. (2022). Socioeconomic Position in Modern Contraceptive Uptake and Fertility Rate among Women of Childbearing Age in 37 Sub-Saharan Countries. World, 3(4), 858-875. https://doi.org/10.3390/world3040048






