Vaccination Is Not Enough: Understanding the Increase in Cases of COVID-19 in Chile despite a High Vaccination Rate
Abstract
:1. Introduction
2. Methods and Case Presentation
2.1. Methods
2.2. Case Presentation
2.2.1. Demographic, Political, and Economic Characteristics of the Country
2.2.2. Healthcare System
3. Results
3.1. Management and Outcome of the COVID-19 Outbreak
3.2. Economic and Social Impact
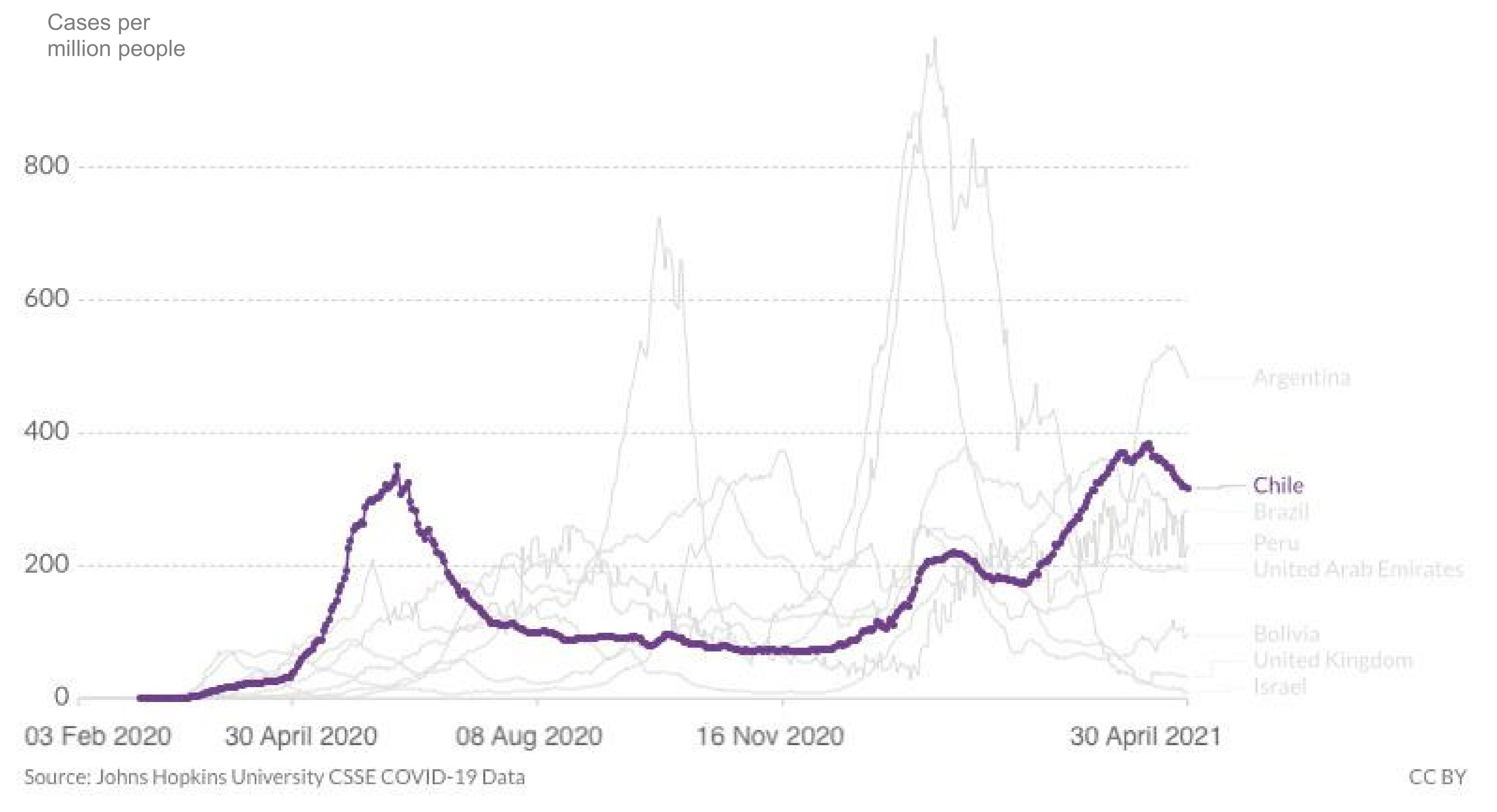
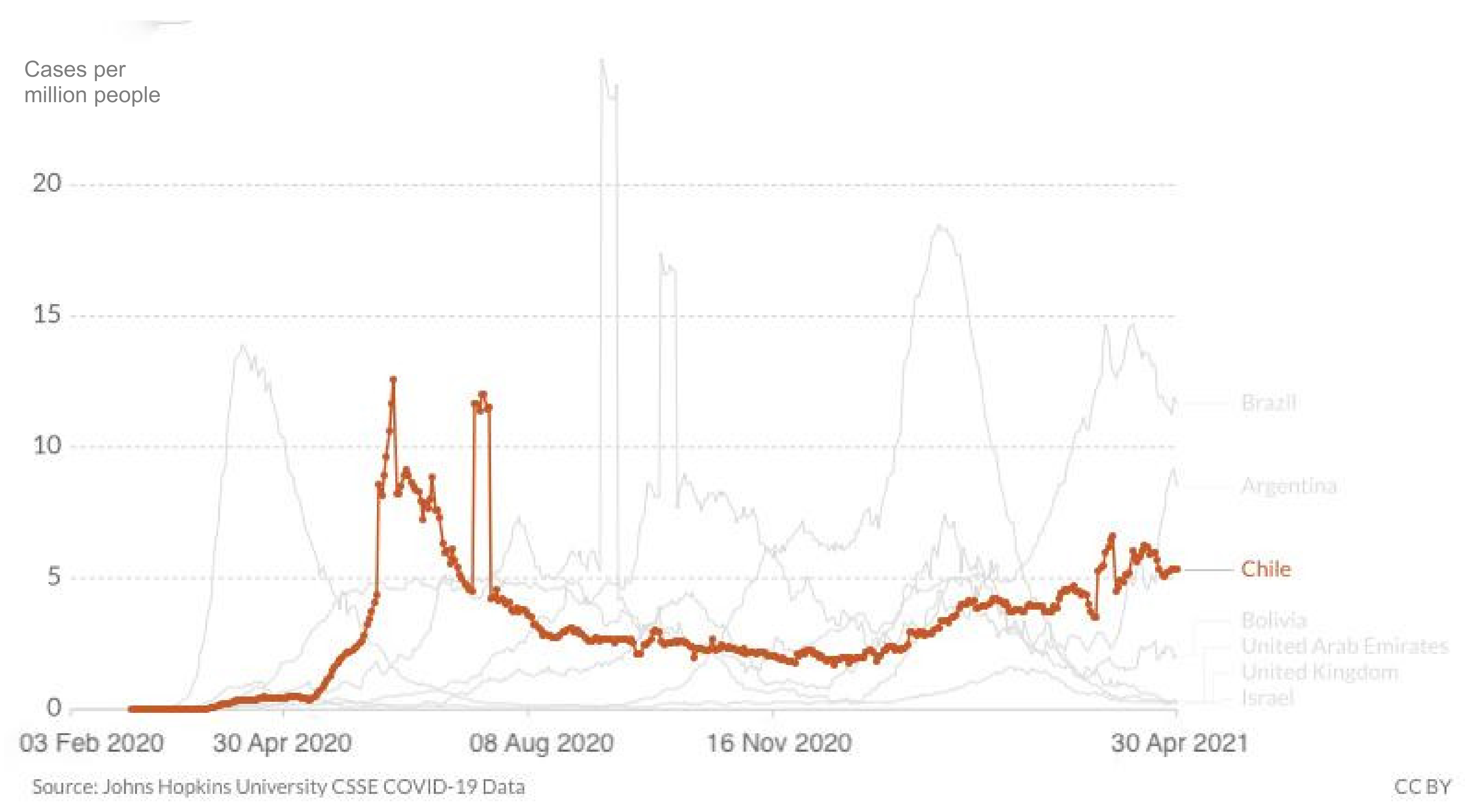
3.3. Epidemiological Situation
3.4. National Vaccination Plan
3.4.1. Vaccines Purchasing Strategy
3.4.2. Characteristics of Available Vaccines
3.4.3. Prioritisation of Target Groups
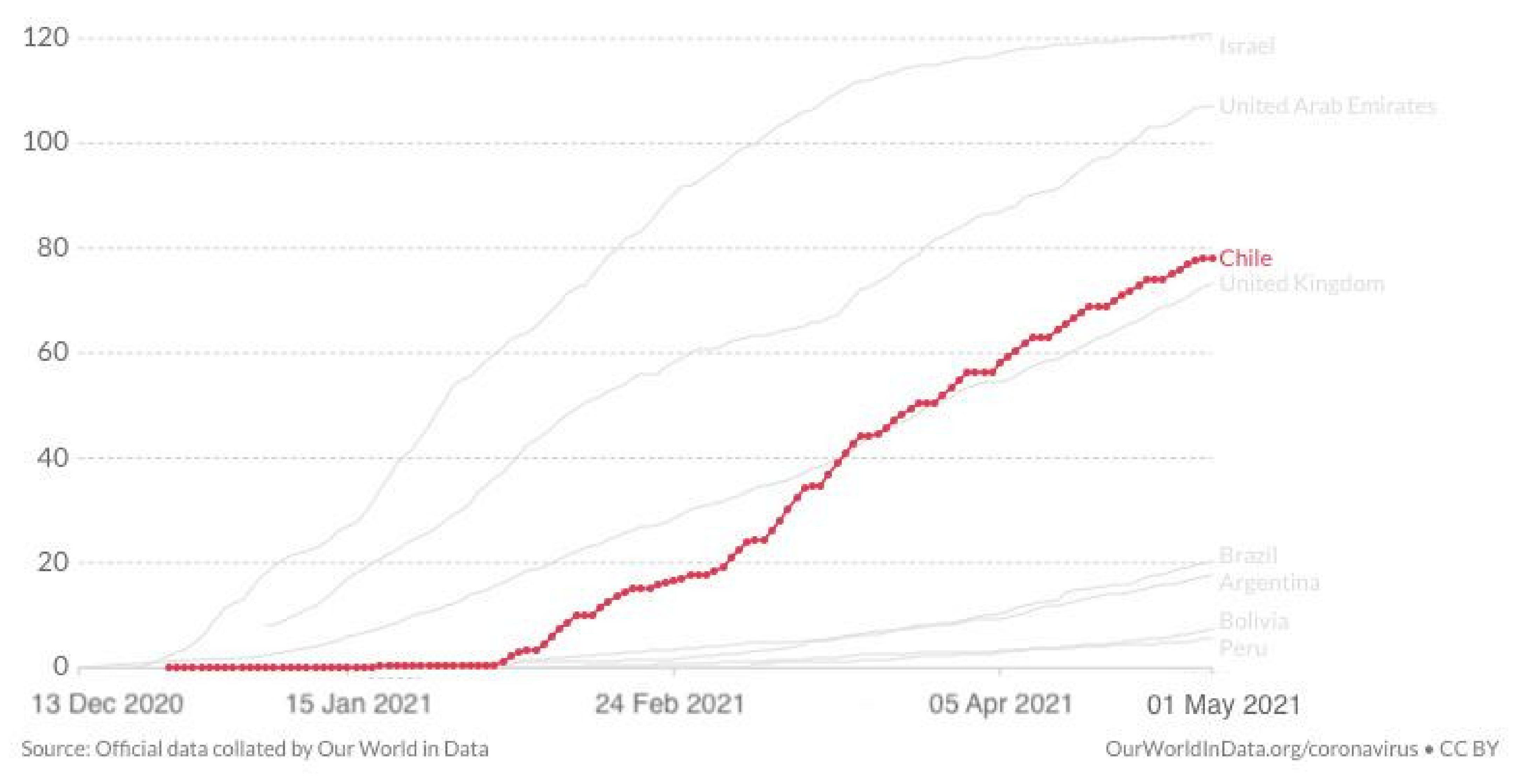
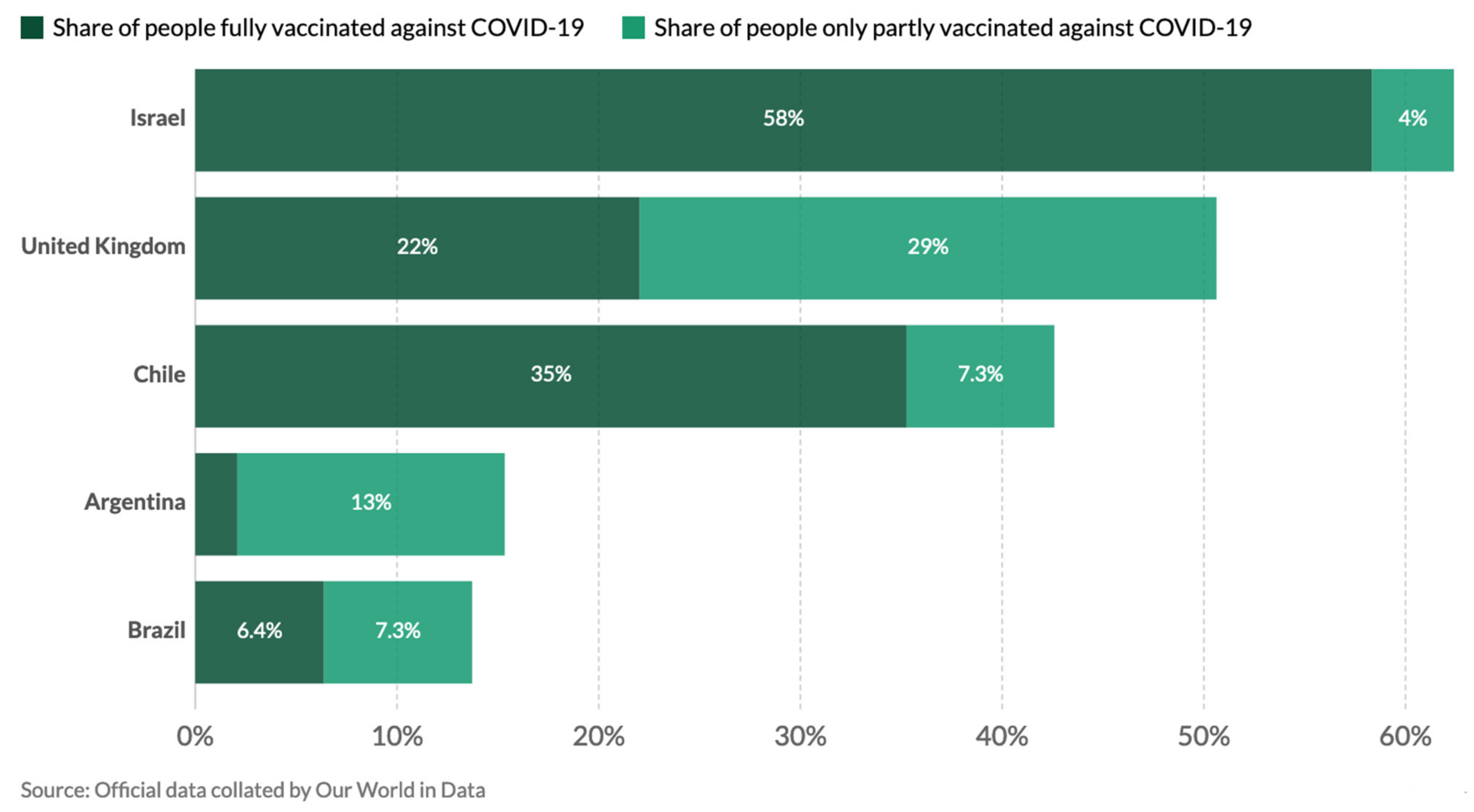
3.4.4. National Vaccination Campaign
3.4.5. Vaccination Outcome
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Economic Commission for Latin America and the Caribbean. Social Panorama of Latin America. 2019. Available online: https://www.cepal.org/es/publicaciones/44969-panorama-social-america-latina-2019 (accessed on 25 March 2021).
- What You Need to Know about the Unrest in Chile. The New York Times. Available online: https://www.nytimes.com/2019/10/21/world/americas/why-chile-protests.html (accessed on 5 April 2021).
- Erin, A.T. Health Care System Overview. Developing a Strategic Program for Chilean Health Information Technology: Environmental Scan and Key Informant Interviews, RAND Corporation. 2016. Available online: www.jstor.org/stable/10.7249/j.ctt19w739p.9 (accessed on 20 April 2021).
- Pan American Health Organisation/World Health Organisation. Epidemiological Update: Coronavirus Disease (COVID-19); PAHO/WHO: Washington, DC, USA, 2021. Available online: https://bit.ly/3lfCYoh (accessed on 14 April 2021).
- Taylor, L. How South America Became the New Centre of the Coronavirus Pandemic New Scientist. 2020. Available online: https://bit.ly/33Ox7hi (accessed on 4 April 2021).
- OurWorldInData. Available online: www.ourworldindata.org (accessed on 1 May 2021).
- Britannica. Available online: https://www.britannica.com/place/Chile (accessed on 25 March 2021).
- United Nations Country Data (Chile). Available online: http://data.un.org/en/iso/cl.html (accessed on 25 March 2021).
- Organisation of Economic Cooperation and Development, Country Profile (Chile). Available online: https://www.oecd.org/chile/ (accessed on 5 May 2021).
- Court, J.; Correo, J.T. Chiles’ Political and Institutional Response to COVID-19. The RegReview. 2020. Available online: https://www.theregreview.org/2020/06/24/court-correa-chile-political-institutional-response-COVID-19/ (accessed on 3 April 2021).
- World Inequality Database. Available online: https://wid.world/country/chile/ (accessed on 6 May 2021).
- Pan American Health Organisation. (2017). Health in the Americas (Chile). Available online: www.https://www.paho.org/salud-en-las-americas-2017/?page_id=105 (accessed on 1 May 2021).
- Cariola Díez Pérez-Cotapos. Chile: COVID-19 Sanitary Governmental Measures. L&E Global. Available online: https://knowledge.leglobal.org/corona/country/chile/chile-COVID-19-sanitary-governmental-measures/ (accessed on 10 May 2021).
- Martín Böhner and Valentina Zagmut, Argentina and Chile: Non-Compliance with Quarantine and Criminal Sanctions, Southern Voice. 2021. Available online: http://southernvoice.org/chile-and-argentina-criminal-sanctions-and-non-compliance-with-quarantines/ (accessed on 25 April 2021).
- International Monetary Fund, Policy Responses to COVID-19 (Chile). Available online: https://www.imf.org/en/Topics/imf-and-COVID19/Policy-Responses-to-COVID-19#C (accessed on 2 May 2021).
- Chile Initiates Clinical Study for COVID-19 Vaccine, Government of Chile. 2020. Available online: https://chilereports.cl/en/news/2020/08/04/chile-initiates-clinical-study-for-COVID-19-vaccine (accessed on 15 April 2021).
- World Bank, Country Profile (Chile). Available online: https://www.worldbank.org/en/country/chile (accessed on 25 April 2021).
- de Campos-Rudinsky, T.C.; Undurraga, E. Public health decisions in the COVID-19 pandemic require more than ‘follow the science’. J. Med. Ethics 2021, 10, 1–4. [Google Scholar] [CrossRef]
- Diego, G.; Patricio, D.; Eduardo, A.; Undurraga, E.V. The Socioeconomic Impact of COVID-19 in Urban Informal Settlements. medRxiv 2021, 21, 9935. [Google Scholar] [CrossRef]
- COVID-19 Crisis and the Informal Economy: Immediate Responses and Policy Challenges, International Labour Organisation Brief, Geneva. 2020. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---travail/documents/briefingnote/wcms_743623.pdf (accessed on 5 April 2021).
- How Chile Built One of the World’s Most Successful Vaccination Campaigns, Vox. 2021. Available online: https://www.vox.com/22309620/chile-COVID-19-vaccination-campaign (accessed on 10 April 2021).
- Vacunas, las Negociaciones Reservadas de Chile, Latercera. 2020. Available online: https://www.latercera.com/la-tercera-domingo/noticia/vacunas-las-negociaciones-reservadas-de-chile/SSEG4BRZJZB4FCWYOZSJ4JNMWY/ (accessed on 26 April 2021).
- Pan American Health Organisation, Covax COVID-19 Vaccines Deliveries in the Americas. Available online: https://www.paho.org/en/covax-americas (accessed on 1 May 2021).
- Coronavirus en Chile: Las Claves que Explican la Exitosa Campaña de Vacunación Contra la COVID-19 en el País Sudamericano, BBC. 2021. Available online: https://www.bbc.com/mundo/noticias-america-latina-5602603711.02.21 (accessed on 25 April 2021).
- Gobierno de Chile, Plan Nacional de Vacunación COVID-19. Available online: https://www.gob.cl/yomevacuno/ (accessed on 25 April 2021).
- Amnesty International, Chile: Plan Nacional Debe Incluir Vacunas Contra el COVID-19 Para Todas las Personas que Residen en el país. 2021. Available online: https://www.amnesty.org/es/latest/news/2021/02/chile-plan-nacional-debe-incluir-vacunas-contra-COVID-para-todas (accessed on 30 April 2021).
- United Nations Development Programme. Support to the National Response and Recovery to Contain the Impact of COVID-19. Available online: https://www.latinamerica.undp.org/UNDP-RBLAC-CHLCV19RespondFiche_v3Jun2020-1.pdf (accessed on 30 April 2021).
- Pan American Health Organisation. Director’s Statement. 2021. Available online: https://www.paho.org/en/news/14-4-2021-paho-director-warns-vaccines-alone-will-not-stop-current-COVID-19-surge (accessed on 14 April 2021).
- La Contradicción Chilena: Por qué el Exito de la Vacunación no Frena la Pandemia? DW. 2021. Available online: https://www.dw.com/es/la-contradicci%C3%B3n-chilena-por-qu%C3%A9-el-%C3%A9xito-de-la-vacunaci%C3%B3n-no-frena-la-pandemia/a-56955777 (accessed on 30 March 2021).
- Taylor, L. COVID-19: Spike in cases in Chile is blamed on people mixing after first vaccine shot. BMJ 2021, 373, 1023. [Google Scholar] [CrossRef]
- Buss, L.F.; Prete, C.A.; Abrahim, C.M.; Mendrone, A.; Salomon, T.; de Almeida-Neto, C.; França, R.F.; Belotti, M.C.; Carvalho, M.P.; Costa, A.G. Three-quarters attack rate of SARS-CoV-2 in the Brazilian Amazon during a largely unmitigated epidemic. Science 2021, 371, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Bueno, S.M.; Abarca, K.; González, P.A.; Gálvez, N.M.; Soto, J.A.; Duarte, L.F.; Schultz, B.M.; Pacheco, G.A.; González, L.A.; Vázquez, Y.; et al. Interim report: Safety and immunogenicity of an inactivated vaccine against SARS-CoV-2 in healthy chilean adults in a phase 3 clinical trial vaccination implementation. MedRxiv 2021, 21, 4494. [Google Scholar] [CrossRef]
- Coutinho, R.M.; Marquitti, F.M.D.; Ferreira, L.S.; Borges, M.E.; da Silva, R.L.P.; Canton, O.; Portella, T.P.; Lyra, S.P.; Franco, C.; da Silva, A.A.M.; et al. Model-Based Evaluation of Transmissibility and Reinfection for the P.1 Variant of SARS-CoV-2. Available online: https://www.medrxiv.org/content/10.1101/2021.03.03.21252706v1.full.pdf (accessed on 30 April 2021).
- Reporte de Circulación de Variantes Sars-CoV-2 en Chile, Ministerio de la Salud, Chile. 2021. Available online: https://www.minciencia.gob.cl/legacy-files/reporte-circulacion-variantes-al-9.04.21-.pdf (accessed on 30 April 2021).
- Moore, S. Vaccination and non-pharmaceutical interventions for COVID-19: A mathematical modelling study. Lancet Infect Dis. 2021, 21, 739–802. [Google Scholar] [CrossRef]
- Nature. Five Reasons Why COVID Herd Immunity Is Probably Impossible. 2021. Available online: https://www.nature.com/articles/d41586-021-00728-2 (accessed on 30 March 2021).
- A Pesar de la Rápida Campaña de Vacunación Contra la COVID-19 en Chile, los Casos Aumentan, The New York Times. 2021. Available online: https://www.nytimes.com/es/2021/03/30/espanol/chile-vacunacion.html (accessed on 30 March 2021).
- Chandrakant, L. Vaccine epidemiology: A review. J. Fam. Med. Prim. Care 2016, 5, 7–15. [Google Scholar] [CrossRef]
- Asahi, K.; Undurraga, E.A.; Valdés, R.; Wagner, R. The effect of COVID-19 on the economy: Evidence from an early adopter of localized lockdowns. J. Glob. Health 2021, 11, 05002. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, A. COVID-19: Chile joins top five countries in world vaccination league. BMJ News 2021, 372, 718. [Google Scholar] [CrossRef]

| Company | Name | Country | Type | Doses | Conservation Temperature | Emergency Authorisation |
|---|---|---|---|---|---|---|
| Pfizer Inc-BioNTech | BNT162b2 | USA/Germany | mRNA | two | −30 °C | Approved on 16 December 2020 |
| Sinovac | Corona Vac | China | Inactivated virus | two | 2–8 °C | Approved on 20 January 2021 |
| Oxford AstraZeneca | Vaxzevria | UK/Sweden | Adenovirus viral vector | two | 2–8 °C | Approved on 27 January 2021 |
| CanSino Biologics | Ad5-nCoV | China | Adenovirus viral vector | one | 2–8 °C | Approved on 7 April 2021 |
| Janssen Pharmaceuticals (J&J) | JNJ-78436735 | USA | Adenovirus viral vector | one | 2–8 °C | Not approved |
| Gamaleya Research Institute | Sputnik V | Russia | Adenovirus viral vector | two | 2–8 °C | in Phase III trials |
| Company | Purchased Doses In Millions | Delivered Doses In Millions (% of Purchased) | Administered Doses (% of Delivered) |
|---|---|---|---|
| Pfizer Inc-BioNTech | 10 | 5 (50) | 2.190.388 (44) |
| Sinovac | 60 | 14.2 (24) | 12.790.551 (90) |
| Oxford AstraZeneca (Covax Facility) | 14.4 | 0.158 (1.1) | 44.010 (28) |
| CanSino Biologics | 1.8 | None | None |
| Janssen Pharmaceuticals (J&J) | 4 Mio | None | None |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lanzavecchia, S.; Beyer, K.J.; Evina Bolo, S. Vaccination Is Not Enough: Understanding the Increase in Cases of COVID-19 in Chile despite a High Vaccination Rate. Epidemiologia 2021, 2, 377-390. https://doi.org/10.3390/epidemiologia2030028
Lanzavecchia S, Beyer KJ, Evina Bolo S. Vaccination Is Not Enough: Understanding the Increase in Cases of COVID-19 in Chile despite a High Vaccination Rate. Epidemiologia. 2021; 2(3):377-390. https://doi.org/10.3390/epidemiologia2030028
Chicago/Turabian StyleLanzavecchia, Sabrina, Katharina Johanna Beyer, and Sophie Evina Bolo. 2021. "Vaccination Is Not Enough: Understanding the Increase in Cases of COVID-19 in Chile despite a High Vaccination Rate" Epidemiologia 2, no. 3: 377-390. https://doi.org/10.3390/epidemiologia2030028
APA StyleLanzavecchia, S., Beyer, K. J., & Evina Bolo, S. (2021). Vaccination Is Not Enough: Understanding the Increase in Cases of COVID-19 in Chile despite a High Vaccination Rate. Epidemiologia, 2(3), 377-390. https://doi.org/10.3390/epidemiologia2030028






