Highlights
What are the main findings?
- None of the patients with overt diabetes had planned their pregnancies, while pregnancy was planned in 26.3% of the patients with pre-existing type 2 diabetes (p < 0.05);
- Periconception and first-trimester glycemic control was poorer in patients with overt diabetes than in those with pre-existing type 2 diabetes;
- Regarding the maternal outcomes, 16.6% of the pregnancies ended in miscarriage, and 5.5% of the women developed gestational hypertension;
- Regarding the newborns’ outcomes, 16.6% of the newborns were LGA, and 11.1% were affected by congenital anomalies, with no significant differences from the newborns of the women with pre-existing type 2 diabetes.
- Overt diabetes, even when characterized by a short disease duration and a low frequency of chronic complications, may lead to negative pregnancy outcomes due to poor metabolic control.
What is the implication of the main finding?
- It is essential to implement diabetes screening protocols for women of childbearing age. These procedures should not only take place at the beginning of pregnancy but also during the preconception phase, particularly for women at high risk of overt diabetes. Key risk factors include a high BMI, pre-existing glycemic disorders, and membership in high-risk ethnic groups.
- Immigrants are particularly vulnerable to diabetes-related pregnancy complications, and targeted screening before pregnancy is necessary to improve their outcomes.
Abstract
Background: Pregestational diabetes mellitus, if not well controlled, determines maternal and fetal complications. According to the new diagnostic criteria for gestational diabetes, the diagnosis of diabetes mellitus can also occur in early pregnancy (overt diabetes). Aim: This study aims to determine pregnancy outcomes in women with overt diabetes compared to women with pre-existing type 2 diabetes. Methods: In this retrospective study, we selected women with pre-existing type 2 and overt diabetes who had at least one pregnancy in the 2010–2022 period at the Diabetic Care Unit of Padova. Results: We analyzed 83 pregnancies, and overt diabetes was diagnosed in 18 pregnancies. In total, 95.5% of patients with overt diabetes and 48% of T2DM patients were immigrants (p < 0.143). No patients with overt diabetes planned their pregnancy, while pregnancy was planned in 26.3% of patients with pre-exiting type 2 diabetes (p < 0.05). Periconception and first-trimester glycemic control were the worst in patients with overt diabetes (HbA1c 9.7 ± 3.1% vs. 7.3% ± 2.3%, p < 0.044, at first visit; 8.1 ± 1.9% and 7.0 ± 1.6%, p < 0.037 in the first trimester) with respect to patients with pre-existing type 2 diabetes. As for maternal outcomes, 16.6% of pregnancies ended in miscarriage, and 5.5% of women developed gestational hypertension; as for newborn outcomes, 16.6% of newborns were LGA, and 11.1% were affected by congenital anomalies without any significant difference with respect to women with pre-existing type 2 diabetes. The high rate of congenital malformations in pregnancies of women with overt diabetes is probably a result of the poor, metabolic control observed during the periconception period when the organogenesis of the fetus takes place. Conclusions: It is essential to utilize procedures for diabetes screening in women of childbearing age not only at the beginning of the pregnancy, but also during the preconception phase or the postmenarcheal period when strong risk factors for diabetes onset are present, such as a high BMI, glycemic disorders, and those who fall under high-risk ethnicity categories.
1. Introduction
The International Association of Diabetes and Pregnancy Study Group (IADPSG) in 2010, based on the results of the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study [1], defined gestational diabetes (GDM) as “a glucose intolerance with the onset or first recognition during pregnancy that is not clearly an overt diabetes” and recommended a new method for the screening and diagnosis of GDM with a one-step approach (OGTT 75 g) with respect to a previous two-step approach (glucose challenge test plus OGTT). Furthermore, the IADPSG underlined the importance of diagnosing “Overt Diabetes”, which is defined as “hyperglycemia first recognized during pregnancy which meets the diagnostic threshold of diabetes in non-pregnant adult” [2]. Overt diabetes in pregnancy is a severe form of hyperglycemia; thus, efforts must be carried out to recognize this condition as soon as possible in order to reduce the adverse maternal and fetal outcomes related to it [3,4,5]. Within this framework, the IADPSG, ADA, WHO, FIGO, Endocrine Society, ACOG, and Italian guidelines have stated that all pregnant women must be screened for overt diabetes at the first prenatal visit by measuring fasting plasma glucose, random plasma glucose, or HbA1c values including the following: fasting plasma glucose equal to or higher than 126 mg/dL; random plasma glucose equal to or higher than 200 mg/dL; and HbA1c equal to or higher than 6.5%. These values must be considered as diagnostics for overt diabetes, if confirmed [2,3,6,7,8,9].
Most studies published in the literature compare the pregnancy outcomes of pregnant women affected by overt diabetes to those of women affected by gestational diabetes, exhibiting worse maternal and fetal outcomes in the former compared to the latter, including higher rates of pregnancy-induced hypertension, pre-eclampsia, neonates that are large for gestational age (LGA), neonatal hypoglycemia, and shoulder dystocia [10,11,12,13,14]. GDM and overt diabetes are two distinct clinical conditions; in fact, GDM is characterized by increased insulin resistance that is induced by the pregnancy, which is not compensated by adequate insulin secretion, while overt diabetes is the result of β-cell dysfunction in the background of chronic insulin resistance in pre-existing pregnancies [2,3].
Type 2 diabetes in pregnancy is increasing, accounting for 30–50% of pregestational diabetes, and it is related to worse maternal and fetal outcomes. As for mothers’ complications, women affected by type 2 diabetes in pregnancies are at a higher risk of miscarriage, pre-eclampsia, gestational hypertension, cesarean delivery, and pre-term delivery [15,16]. Neonates of women with type 2 diabetes are at higher risk of LGA, birth trauma, respiratory distress, hypoglycemia, hyperbilirubinemia, hypocalcemia, and congenital malformations [15,16].
Due to the similar physiopathology of overt diabetes and pre-existing type 2 diabetes, women with overt diabetes may be at the same risk of adverse outcomes as those with known pre-existing diabetes, but data reported in the literature are scarce and conflicting. In particular, Oppermann et al. have shown that there are no differences in pregnancy outcomes in the two groups of evaluated pregnant women [17]. Significant differences in macrosomia and neonatal jaundice are reported by Schiller et al: this study compared pregnant women with prediabetes and pregnant women with pregestational overt type 2 diabetes, which included women with known type 2 diabetes or those that are first diagnosed during pregnancy [18]. Thus, we think it is of interest to study the pregnancy outcomes of women affected by overt diabetes and compare them to those of women with known pre-existing type 2 diabetes.
2. Materials and Methods
We retrospectively evaluated only pregnant women with a diagnosis of pre-existing type 2 diabetes (T2DM) and women with a diagnosis of overt diabetes (ODM), according to IADPSG criteria [2], who had at least one pregnancy in the 2010–2022 period at the Diabetic Care Unit of Padova.
Women with type 1 diabetes, latent autoimmune diabetes of the adult (LADA), maturity onset diabetes of the youth (MODY), and GDM were excluded from the study. Overt diabetes was diagnosed according to the ADA and WHO criteria [3,4]. Data were extracted from electronic medical records. During the first postconception pregnancy visit, physiological and obstetric history were collected: pre-pregnancy weight and BMI, pregnancy planning, date of last menstruation, parity, previous GDM, and pregnancy outcome of previous pregnancies. During pregnancy, glycated hemoglobin, fasting glycemia, microalbuminuria, systolic and diastolic blood pressure, and weight gain were collected. As for chronic diabetes complications, retinopathy (ophthalmological evaluation), nephropathy (albumin/creatinine ratio exceeding 30 mg/g), chronic hypertension (reported in the patient’s medical history or by use of hypertensive drugs), and neuropathy (clinical evaluation) were assessed. At their first and follow-up visits, women were followed by a multidisciplinary team consisting of a diabetologist, a dietician, and a nurse. They were counseled about maternal and fetal risks related to diabetes: they received an individualized diet, which was customized with respect to immigrant patients according to ethnicity; they were educated to perform self monitoring blood glucose and insulin therapy; and they underwent periodic clinical and biochemical evaluations. As for maternal outcomes, miscarriages, the mode and time of delivery, pre-eclampsia, neonatal outcomes, weight and length at birth, shoulder dystocia, hypoglycemia, jaundice, hypocalcemia, respiratory distress, and congenital malformations were recorded.
Height was measured during the first appointment, and weight was measured at each visit. The body mass index (BMI) was calculated as weight in kilograms divided by the square of the height (kg/m2).
Newborns were classified as LGA if their birth weight was in the >90th percentile; alternatively, they were classified as small for gestational age (SGA) if their birth weight was in the <10th percentile, based on the standard growth and development tables of the WHO chart [19].
Plasma glucose levels were measured using the glucose oxidase method [20]. HbA1c was measured using a standardized HPLC method with IFCC aligned [21].
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Province of Padova. Approval study (number 1248). Informed consent was obtained from all subjects involved in the study.
Statistical Evaluation
The data were processed with IBM SPSS 25 statistical programs. Continuous quantitative variables are expressed as means ± standard deviations, and they were compared with Student’s t-test. Non parametric data are expressed as % and analyzed with X2 and Fisher’s tests. A p-value of <0.05 was considered statistically significant.
3. Results
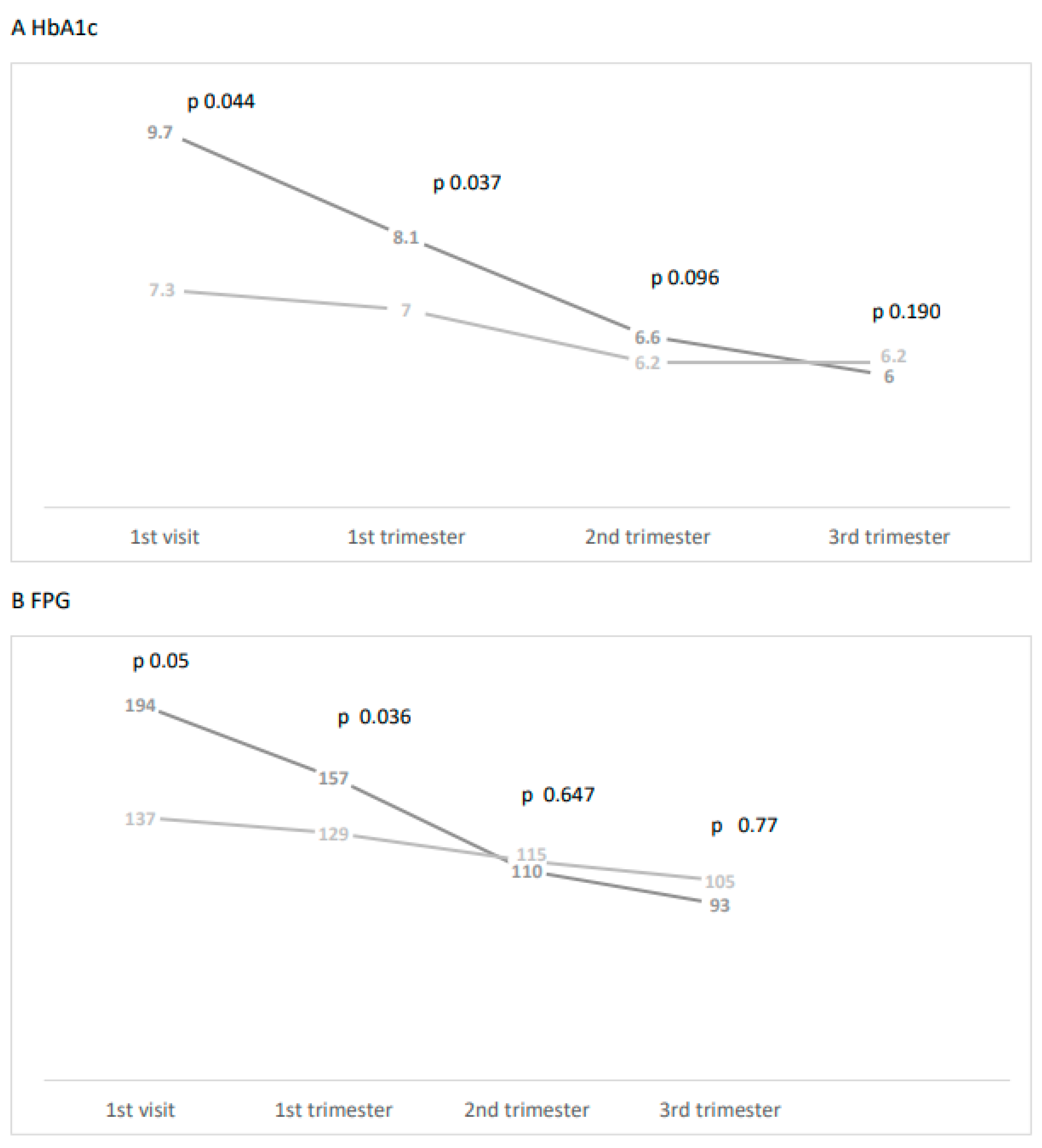
We analyzed 83 pregnancies in 68 patients: Overt diabetes was diagnosed in 18 pregnant women, and 50 women with 65 pregnancies were affected by pre-existing type 2 diabetes. It is noteworthy that 94.5% of patients with ODM were immigrants who were mainly from South East Asia and Sub-Saharan Africa. ODM pregnancies were diagnosed at an average of 8.5 gestational weeks (g.w.). With respect to clinical and metabolic characteristics, the two groups are comparable in terms of age, pre-pregnancy BMI, chronic hypertension, and previous pregnancies. All patients were treated with insulin during pregnancies with a basal bolus approach, and the insulin dosage during the pregnancy is shown in Table 1. Retinopathy was significantly higher, and other diabetic complications were higher even if not significant in women with T2DM with respect to women with ODM (Table 1). On the other hand, the two groups differed significantly in terms of glycemic control at the first visit and in the first trimester, which was worst in women with ODM (HbA1c 9.7± 3.1% vs. 7.3% ± 2.3%, p < 0.044, at first visit; 8.1 ± 1.9% and 7.0 ± 1.6%, p < 0.037, in the first trimester; fasting plasma glucose 194 ± 43 mg/dL vs. 137 ± 37 mg/dL at the first visit, p < 0.05; 157 ± 38 mg/dL vs. 129 ± 39 mg/dL, p > 0.036, in the first trimester) (Figure 1).

Table 1.
Clinical and metabolic characteristics in pregnant women under study.
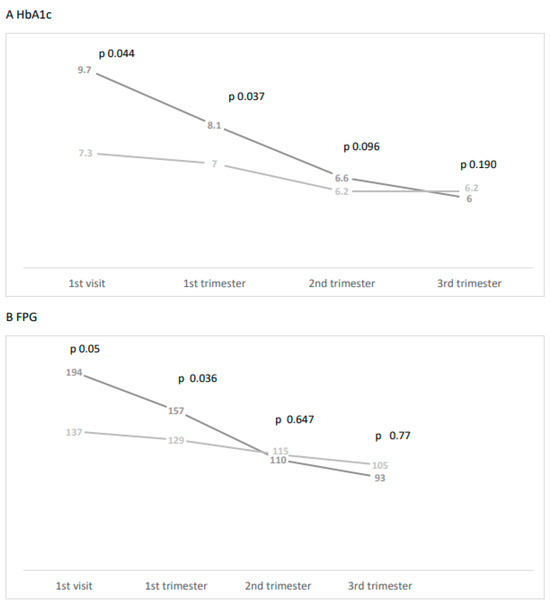
Figure 1.
(A) HbA1c levels during pregnancy in patients with ODM (dark grey) and T2DM (light grey). (B) Fasting plasma glucose levels during pregnancy in patients with ODM (dark grey) and T2DM (light grey).
As for maternal outcomes, the miscarriage rate was higher, even if not significant, in women with ODM with respect to women with T2DM, and gestational hypertension was higher even if not significant in T2DM with respect to women with ODM (Table 1).
As for fetal outcomes, congenital malformations were more frequent, even if not significant in women with ODM with respect to women with T2DM (11.1% vs. 7.7%; p = 0.364), while the rate of the other fetal complications was higher in women with T2DM. No significant differences were observed in LGA and SGA rates (Table 2). The types of congenital malformations are reported in the Supplementary File.

Table 2.
Maternal and fetal outcomes in pregnant women under study.
At a follow-up visit 3 months after delivery, in all women with ODM, the diagnosis of type 2 diabetes was confirmed.
4. Discussion
Most studies are published in the literature in order to better define the physiopathological mean of overt diabetes compared to GDM pathology [11,12,13,14]. In a case–control study, Agha-Jaffar et al. reported a higher frequency of hypertensive disorders and higher frequencies with respect to insulin treatment in ODM compared to women with GDM, and pointed out the fact that ODM is phenotypically a type 2 diabetes mellitus [22]. In a multi-ethnic cohort in Spain, pregnant women with ODM exhibited worse obstetric outcomes with respect to women with GDM, and this was present mainly in women from ethnic minorities [23]. In a recent search of the literature, which has taken into consideration articles up to 2022, worse maternal and fetal outcomes have been evidenced in ODM with respect to women with GDM, even if different diagnostic criteria have been utilized to diagnose ODM in the reported studies [10]. In our study, which has compared maternal and fetal outcomes in pregnant women with overt diabetes to pregnant women with pre-existing type 2 diabetes, the main finding is that ODM shows higher frequencies even if not significant due to the low number of cases of congenital malformations with respect to T2DM. This finding can be explained by the worse glycemic control observed in overt pregnant women and by the fact that none of these women planned their pregnancy. In a case–control study that has evaluated 414 women with T2DM and 204 women with ODM, no differences in maternal and fetal outcomes have been found when also considering congenital malformations; this study underlines that the mean values of HbA1c at the initial appointment were no different and no worse in the two groups (7.2 vs. 7.4%), and 70% of the women were white [17]. It was observed in this study that 52.5% of women with ODM went to a specialized prenatal care center in the third trimester of pregnancy, while those with T2DM went during the first trimester. Late arrival to the specialized prenatal care center has also been reported in the study of Schiller et al. [18]. Similarly, in a retrospective observational study from a tertiary care center in Pakistan, 55.3% cases of overt diabetes were diagnosed and followed up late during pregnancy [13]. It was observed that this is the only publication in which the frequency of overt diabetes has been evaluated, accounting for 16.5% of 2462 pregnant women [13]. Poor glycemic control in the preconception phase [24] and the frequent coexistence of obesity [15] are well-known risk factors in determining a worse neonatal outcome in pregnant women with pre-existing type 2 diabetes. In our cohort, no differences in the frequency of obesity have been observed, but as mentioned previously, the levels of HbA1c were higher in women with overt diabetes relative to women with pre-existing type 2 diabetes. Furthermore, at follow-up visits, in all patients with ODM, the diagnosis of type 2 diabetes was confirmed. Preconception care is of key importance in order to reduce maternal and fetal complications in pregnancies that are complicated by pregestational diabetes; thus, the fact that women with overt diabetes do not plan their pregnancies can further explain the high frequency of congenital malformations [25]. All pregnant women with overt diabetes in our cohort are not known to have diabetes, and even if 77.8% of them have had gestational diabetes treated, none of the women underwent a postpartum evaluation of glucose tolerance in 43% of cases with insulin. The high frequency in our study of immigrant women explains the scarce adherence to postpartum follow-up [26] and the poor attendance relative to antenatal pregnancy care units [27]. These data emphasize the importance of a correct and early diagnosis of overt diabetes, which can reduce the negative effects of a pregnancy-related misdiagnosis and or a late diagnosis of this condition.
The strengths of the study are as follows: All patients with overt diabetes were diagnosed early (8.5 g.w.), and this was followed up by the same multidisciplinary team; patients received an individualized diet; and patients were educated in performing blood glucose self-monitoring and basal bolus insulin therapy. The limitations of this study are its retrospective nature and the low number of patients evaluated, which explains why some differences do not achieve significance.
5. Conclusions
In conclusion, our data show for the first time that overt diabetes, even if characterized by a short disease duration and a low frequency of chronic complications, could result in negative pregnancy outcomes due to poor, metabolic control. Thus, it is essential to utilize procedures for diabetes screening in women of childbearing age, and this should be carried out not only at the beginning of pregnancy, but also during the preconception phase when strong risk factors for overt diabetes are present, such as a high BMI, glycemic disorders, and those who fall under high-risk ethnicity categories. Immigrants are a vulnerable group with respect to diabetes-related pregnancy outcomes; thus, efforts must be carried out in order to diagnose them before pregnancy occurs. Further studies in larger populations are needed to better clarify the impact of ODM on maternal and fetal outcomes in order to improve the management of these women.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/endocrines5020017/s1, Malformations found in pregnant women with pre-existing type 2 diabetes (T2DM) and women with overt diabetes (ODM).
Author Contributions
M.G.F. recorded data, M.G.D. made data curation, data validation, statistical analysis, contribute to writing the paper, S.B. made data validation and contribute to writing the paper, A.L. made data validation, write review and editing the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Province of Padova (approval number 1248).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article and Supplementary Materials.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- HAPO Study Cooperative Research Group. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study. Int. J. Gynaecol. Obstet. 2022, 78, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Metzger, B.E.; Gabbe, S.G.; Persson, B.; Buchanan, T.A.; Catalano, P.A.; Damm, P.; Dyer, A.R.; Leiva, A.D.; International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010, 33, 676–682. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2024. Diabetes Care 2024, 47 (Suppl. S1), S20–S42. [CrossRef] [PubMed]
- World Health Organization. Diagnostic criteria and classification of hyperglycemia first detected in pregnancy. A World Health Organization Guidelines. Diab. Res. Clin. Pract. 2014, 103, 341–363. [Google Scholar] [CrossRef] [PubMed]
- Hod, M.; Kapur, A.; Sacks, D.A.; Hadar, E.; Agarwal, M.; Di Renzo, G.C.; Cabero Roura, L.; McIntyre, H.D.; Morris, J.L.; Divakar, H. The International Federation of Gynecology and Obstetrics (FIGO) Initiative on gestational diabetes mellitus: A pragmatic guide for diagnosis, management, and care. Int. J. Gynaecol. Obstet. 2015, 131 (Suppl. S3), S173–S211. [Google Scholar] [CrossRef] [PubMed]
- Blumer, I.; Hadar, E.; Hadden, D.R.; Jovanovic, L.; Mestman, J.H.; Murad, M.H.; Yogev, Y. Diabetes and pregnancy: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2013, 98, 4227–4249, Update in J. Clin. Endocrinol. Metab. 2018, 103, 4042. [Google Scholar] [CrossRef]
- SNLG-ISS. Gravidanza Fisiologica. In Linea Guida; Ministero Della Salute: Roma, Italy, 2011. [Google Scholar]
- Committee on Practice Bulletins—Obstetrics. ACOG Practice Bullettin: Gestational Diabetes Mellitus. Obstet. Gynecol. 2017, 13, e17–e31. [Google Scholar]
- Wong, T.; Ross, G.P.; Jalaludin, B.B.; Flack, J.R. The clinical significance of overt diabetes in pregnancy. Diabet Med. 2013, 30, 468–474. [Google Scholar] [CrossRef]
- Goyal, A.; Gupta, Y.; Tandon, N. Overt Diabetes in Pregnancy. Diabetes Ther. 2022, 13, 589–600, Erratum in: Diabetes Ther. 2022, 13, 601. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nabi, T.; Rafiq, N.; Arifa, Q.A.; Mishra, S. Effect of Overt Diabetes and Gestational Diabetes Mellitus on Pregnancy Outcomes and Progression. J. Obstet. Gynaecol. India 2022, 72 (Suppl. S1), 235–242. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sampaio, Y.; Porto, L.B.; Lauand, T.C.G.; Marcon, L.P.; Pedrosa, H.C. Gestational diabetes and overt diabetes first diagnosed in pregnancy: Characteristics, therapeutic approach and perinatal outcomes in a public healthcare referral center in Brazil. Arch. Endocrinol. Metab. 2021, 65, 79–84. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wali, A.S.; Rafique, R.; Iftikhar, S.; Ambreen, R.; Yakoob, M.Y. High proportion of overt diabetes mellitus in pregnancy and missed opportunity for early detection of diabetes at a tertiary care centre in Pakistan. Pak. J. Med. Sci. 2020, 36, S38–S43. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, T.; Saito, M.; Nishigori, H.; Nagase, S.; Yaegashi, N.; Sagawa, N.; Kawano, R.; Ichihara, K.; Sanaka, M.; Anazawa, S.; et al. Japan Diabetes and Pregnancy Study Group. Comparison of pregnancy outcomes between women with gestational diabetes and overt diabetes first diagnosed in pregnancy: A retrospective multi-institutional study in Japan. Diabetes Res. Clin. Pract 2014, 103, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Dalfrà, M.G.; Burlina, S.; Lapolla, A. Pregnancy and type 2 diabetes: Unmet goals. Endocrines 2023, 4, 366–377. [Google Scholar] [CrossRef]
- Raets, L.; Ingelbrecht, A.; Benhalima, K. Management of type 2 diabetes in pregnancy: A narrative review. Front. Endocrinol. 2023, 14, 1193271. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Oppermann, M.L.; Campos, M.A.; Hirakata, V.N.; Reichelt, A.J. Overt diabetes imposes a comparable burden on outcomes as pregestational diabetes: A cohort study. Diabetol. Metab. Syndr. 2022, 14, 177. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schiller, T.; Barak, O.; Winter Shafran, Y.; Barak Sacagiu, M.; Cohen, L.; Vaisbuch, E.; Zornitzk, T.; Kirzhner, A. Prediabetes in pregnancy—Follow-up, treatment, and outcomes compared to overt pregestational diabetes. J. Matern. Fetal Neonatal Med. 2023, 36, 2191153. [Google Scholar] [CrossRef] [PubMed]
- Kiserud, T.; Piaggio, G.; Carroli, G.; Widmer, M.; Carvalho, J.; Neerup, J.L.; Giordano, D.; Cecatti, J.G. The World Health Organization Fetal Growth Charts: A Multinational Longitudinal Study of Ultrasound Biometric Measurements and Estimated Fetal Weight. PLoS Med. 2017, 14, e1002220. [Google Scholar] [CrossRef] [PubMed]
- Huggett, A.S.; Nixon, D.A. Use of glucoseoxidase, peroxidase, and O-dianisidine in determination of blood and urinary glucose. Lancet 1957, 273, 368–370. [Google Scholar] [CrossRef] [PubMed]
- Mosca, A.; Paleari, R.; Dalfrà, M.G.; Di Cianni, G.; Cuccuru, I.; Pellegrini, G.; Malloggi, L.; Bonomo, M.; Granata, S.; Ceriotti, F.; et al. Reference intervals for hemoglobin A1c in pregnant women: Data from an Italian multicenter study. Clin. Chem. 2006, 52, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- Agha-Jaffar, R.; Oliver, N.S.; Kostoula, M.; Godsland, I.F.; Yu, C.; Terry, J.; Johnston, D.; Gable, D.; Robinson, S. Hyperglycemia recognised in early pregnancy is phenotypically type 2 diabetes mellitus not gestational diabetes mellitus: A case control study. J. Matern. Fetal Neonatal Med. 2020, 33, 3977–3983. [Google Scholar] [CrossRef] [PubMed]
- Mañé, L.; Flores-Le Roux, J.A.; Benaiges, D.; Chillarón, J.J.; Prados, M.; Pedro-Botet, J.; Llauradó, G.; Gortazar, L.; Payà, A. Impact of overt diabetes diagnosed in pregnancy in a multi-ethnic cohort in Spain. Gynecol. Endocrinol. 2019, 35, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Lapolla, A.; Dalfrà, M.G.; Fedele, D. Pregnancy complicated by diabetes: What is the best level of HbA1c for conception? Acta Diabetol. 2010, 47, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Wahabi, H.A.; Fayed, A.; Esmaeil, S.; Elmorshedy, H.; Titi, M.A.; Amer, Y.S.; Alzeidan, R.A.; Alodhayani, A.A.; Saeed, E.; Bahkali, K.H.; et al. Systematic review and meta-analysis of the effectiveness of pre-pregnancy care for women with diabetes for improving maternal and perinatal outcomes. PLoS ONE 2020, 15, e0237571. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dalfrà, M.G.; Burlina, S.; Del Vescovo, G.G.; Anti, F.; Lapolla, A. Adherence to a follow-up program after gestational diabetes. Acta Diabetol. 2020, 57, 1473–1480. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Rivas, E.; Flores-Le Roux, J.A.; Benaiges, D.; Sagarra, E.; Chillaron, J.J.; Paya, A.; Dou, J.P.-D.; Goday, A.; Lopez-Vilchez, M.A.; Pedro-Botet, J. Gestational diabetes in a multiethnic population of Spain: Clinical characteristics and perinatal outcomes. Diabetes Res. Clin. Pract. 2013, 100, 215–221. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).