Highlights
What are the main findings?
- The results of in vitro toxicity studies demonstrated asperuloside’s safety profile with the evaluation of cell viability and proliferation, while simultaneously establishing dose recommendations for future animal studies.
- In vivo, the anti-obesity effects of asperuloside were evidenced by significant reductions in blood leptin levels and in the expression of orexigenic peptides (NPY and AgRP) in high-fat diet (HFD)-fed mice, with no effects observed in those on a standard diet.
- The anti-inflammatory properties of asperuloside were demonstrated by significant reductions in the mRNA levels of pro-inflammatory cytokines (IL-1, IL-6, and TNF-α) in the hypothalamus and liver, along with decreased levels of circulating plasminogen activator inhibitor-1 (PAI-1), which is linked to insulin resistance and cardiovascular complications.
What is the implication of the main finding?
- Our results indicate that asperuloside is a safe compound for long-term use in animal models and that it promotes weight loss while simultaneously reducing the elevated levels of pro-inflammatory cytokines that occur in obesity.
- This distinctive mechanism of action, which targets the inflammatory processes occurring in obesity, opens new avenues for anti-obesity drug discovery and the identification of clinically relevant weight loss agents.
Abstract
Obesity produces a systemic low-grade inflammation associated with many adverse health conditions and, as we recently learned, with complications of COVID-19. Functional studies in animal models have demonstrated that asperuloside, an iridoid glycoside found in many medicinal plants, has produced promising anti-obesity results. However, the safety profile and the anti-inflammatory properties of asperuloside remain unknown. Here, we confirmed the previously reported anti-obesity properties of asperuloside, and, importantly, we performed toxicity studies assessing cell viability providing a dose reference for future animal experiments. Asperuloside significantly reduced blood levels of leptin and the mRNA levels of orexigenic peptides, such as NPY and AgRP in mice consuming HFD, with no effect on mice eating a standard chow diet. In addition, our results indicate that ASP reduced both hypothalamic and hepatic mRNA levels of pro-inflammatory cytokines such as IL-1, IL-6 and TNF-α as well as the blood levels of plasminogen activator inhibitor-1 (PAI-1), which are known to play a major role in the development of insulin resistance and cardiovascular complications. Collectively, our findings suggest that asperuloside is a safe compound for long-term use in animal models and that it reduces the elevated levels of pro-inflammatory cytokines occurring in obesity.
Keywords:
asperuloside; inflammation; TNF-α; IL-1; IL-6; hypothalamus; obesity; food intake; weight loss 1. Introduction
The consequences of obesity represent a major public health concern. Obesity produces a systemic low-grade inflammation associated with many adverse health conditions, including cardiovascular disease, type 2 diabetes, multiple types of cancers and, as we recently learned, complications of COVID-19 [1,2].
In the pathophysiology of obesity, there is growing evidence that the development of inflammatory processes in peripheral organs affects the function of brain areas responsible for the regulation of energy homeostasis and systemic metabolism [3]. The hypothalamus, an area of the brain that controls and integrates peripheral signals to regulate feeding behaviour and energy expenditure, is particularly affected by systemic inflammation, which leads the body to a vicious cycle of metabolic derangements associated with insulin resistance [4,5].
In the treatment of obesity, the short-term use of weight-loss medications has been proven unsuccessful when the patients need to maintain the reduced weight indefinitely [6]. On the other hand, long-term pharmacological approaches appear to be the most effective tool to help patients adhere to dietary requirements and maintain a reduced body weight [7]. However, subsequent to the withdrawal from the market of several anti-obesity medications for safety reasons [8], there is a need for a better and safer pharmacological strategy.
Recent interest has turned to the anti-obesity compound asperuloside (ASP), an iridoid glycoside commonly found in dicotyledonous plant families, including Apocynaceae Verbenaceae, Loganiaceae and Rubiaceae, which has produced promising results in animal models [9,10,11,12]. The mechanisms by which asperuloside exerted its anti-obesity properties are not fully clarified; however, three months of compound administration reduced food intake, body weight, adipose masses as well as plasma levels of triacylglycerol, non-esterified fatty acids and total cholesterol in rats consuming a high-fat diet (HFD) [9,10]. More recently, the anti-obesity properties of asperuloside were confirmed by another animal study in a mouse model of obesity and some mechanisms that could be responsible for its therapeutic effect were also identified [11]. The compound reduced body weight and food intake in rodents consuming HFD by 10.5% and 12.8%, respectively, with no effect on mice eating a standard chow diet. Fasting glucose and plasma insulin were also significantly reduced, and mechanistically, asperuloside significantly reduced hypothalamic mRNA ghrelin, leptin, orexin1, melanocortin 4, pro-opiomelanocortin and cannabinoid 1 receptor only in mice consuming HFD [11]. The expression of sweet (TAS1R2 and TAS1R3) and fat (FFAR1 and FFAR4) lingual receptors was increased almost 2-fold by the administration of asperuloside, suggesting that asperuloside might exert its therapeutic effects by altering nutrient-sensing receptors in the oral cavity as well as hypothalamic receptors involved in food intake when mice are exposed to obesogenic diets [11]. Asperuloside also showed anti-inflammatory properties, downregulating inflammatory markers such as tumour necrosis factor-alpha (TNF-α), interleukin (IL)-1β, and IL-6 levels in a mouse model of acute lung injury (ALI) [13]. Similarly, in lipopolysaccharide (LPS)-induced inflammation in Raw 264.7 cells, pre-treatment with asperuloside remarkably blunted the phosphorylation of inhibitor of nuclear factor kappa-B (IκBα), extracellular signal-related kinases 1 and 2 (ERK1/2), c-Jun N-terminal kinase (JNK) and p38 mitogen-activated protein kinase (p38MAPK) [13]. These results indicated that the compound exerted its anti-inflammatory effect in suppressing the pro-inflammatory nuclear factor kappa-B (NF-κB) and MAPK phosphorylation in a concentration-dependent manner [13]. In line with these results, other investigations confirmed the previously reported anti-inflammatory properties of asperuloside, confirming that the effects are related to inhibiting inflammatory cytokines and mediators via suppression of the NF-κB and mitogen-activated protein kinase (MAPK) signalling pathways [14,15,16].
However, the safety profile and the anti-inflammatory properties of asperuloside in obesity and specifically in peripheral and central organs remain unknown. This study is one of the first to address the safety of the compound as well as its anti-inflammatory role in the hypothalamus and liver of obese mice.
2. Material and Methods
2.1. Cell Culture
The human liver carcinoma cell line HepG2 (ATCC® HB-8065™) was maintained in low glucose Dulbecco’s Modified Eagle Medium (DMEM, Sigma-Aldrich, Sydney, NSW, Australia) supplemented with 10% foetal bovine serum (FBS, Sigma-Aldrich, Sydney, NSW, Australia) without antibiotics. Culture conditions were maintained at 37 °C in a humidified incubator with 5% CO2. Cells were sub-cultured twice a week upon reaching approximately 80–90% confluency.
2.2. WST-1 Assay
The colorimetric WST-1 viability assay kit (Cayman, Sapphire Biosciences, Redfern, NSW, Australia) is based on the enzymatic reduction in the WST-1 tetrazolium salt to formazan, which is directly related to the cell’s metabolic activity. The assay was carried out as recommended by the supplier. HepG2 cells were seeded at 5000 cells/well in a transparent 96-well plate and allowed to adhere overnight. Subsequently, cells were treated with 0–1 mM asperuloside (ASP) for 24 h. DMSO was used as vehicle control, while the mitochondrial complex I inhibitor rotenone was used as a positive control. After 2 h of incubation at 37 °C, WST-1 absorbance at 450 nm was determined with a microplate reader (Multiskan Go, Thermo Fisher Scientific, Scoresby, VIC, Australia). Absorbance values were standardised on the total protein content for each well before standardised on the untreated control and expressed as % viability. Average viability data were derived from 3 independent experiments (n = 3) with six replicates per experiment for each drug concentration. The results are presented as mean ± S.D. Similarly, the time-dependent toxicity of 1 mM asperuloside was assessed over a period of 24 h, 48 h, and 72 h, respectively. WST-1 absorbance was detected and analysed as described above.
2.3. ATP Assay
Cellular ATP levels as an indicator of cell viability were measured by luminescence from the ATP-dependent enzymatic oxidation of luciferin by luciferase as previously described [17]. HepG2 cells were seeded at 10,000 cells per well in transparent 96-well plates and incubated overnight to adhere before being exposed to increasing concentrations of ASP (0, 50, 100, 200, 400, 600, 800, and 1000 µM) for 24 h. DMSO was used as a solvent control while the mitochondrial complex I inhibitor rotenone served as a positive control. HepG2 cells were washed with 1× 100 µL PBS and lysed in 100 µL lysis solution (4 mM EDTA, 0.2% Triton X-100) for five minutes at room temperature. In a white 96-well plate, 100 µL of ATP measurement buffer (25 mM HEPES pH 7.25, 300 µM D-luciferin, 5 µg/mL firefly luciferase, 75 µM DTT, 6.25 mM MgCl2, 625 µM EDTA and 1 mg/mL BSA) was combined with 10 µL cell lysate to initiate the reaction. Luciferase-based luminescence was acquired immediately using a plate reader (Fluoroskan, Thermo Fisher Scientific, Scoresby, VIC, Australia). Relative luminescence unit (RLU) values were standardised against the total protein content for each well, and the results were expressed as RLU/mg/mL. Data represent the average of 3 independent experiments (n = 3) with 6 replicates/experiment and was expressed as the mean ± S.D. Similarly, time-dependent toxicity was also assessed with this assay as described for the WST-1 assay above.
2.4. Colony Formation Assay (CFA)
Colony formation was employed to determine the long-term effects of ASP treatment on HepG2 cells. Cells were seeded in low glucose DMEM culture media with 10% FBS at 2000 cells per well in a 6-well plate. After overnight adhesion, the cells were exposed to ASP concentrations up to 1000 µM for two weeks without a media change. The assay was terminated by fixation of cells with 2% w/v paraformaldehyde in PBS for 10–15 min at room temperature. Colonies were stained with 0.25% Coomassie Brilliant Blue in 50% (v/v) methanol, 10% (v/v) acetic acid for 5 min at room temperature. Colonies of more than 50 cells were counted by eye or under the microscope. The experimental results were derived from the average of four independent experiments with four replicates/experiments for each drug concentration. The results are presented as percentage colony formation (compared with the untreated control cells) and expressed as average ± SEM.
2.5. Animals and Experimental Set-Up
Three-week-old (21 days) C57BL/6J male mice were housed at a temperature of 20 ± 2 °C and were maintained on a standard 12:12 h light/dark cycle at the University of Tasmania Animal Services breeding facility for one week after arrival. Post acclimatisation period, mice with equal average starting body weight (21.01 ± 0.27 g) were randomised into two diet groups (n = 40) and were fed either standard chow (12.8 MJ/kg, 6% fat, 20% protein, 3.2% crude fibre, Barastoc, Victoria, Australia) or commercial calorie-rich high-fat pelleted diet (HFD) (19.4 MJ/kg, 23.5% fat, 23% protein, 5.4% crude fibre, Specialty Feeds, Glen Forest, Western Australia). All the mice were singularly housed with free access to food and drinking water ad libitum. Each cage was equipped with a free-running wheel to avoid social stress associated with isolation. The body weight gain was measured each week during the experimental period. After 12 weeks of ASP administration, the mice were euthanised to collect the tissues of interest. All animal work and procedures in this study were performed according to the guidelines of the University of Tasmania, following the Australian national law for the care and use of Animals for Scientific Purposes (8th Edition 2013) and authorised by the local animal ethics committee (University of Tasmania Animal Ethics Committee, permit # A0015841).
2.6. Preparation of ASP
ASP was extracted and purified from the native Tasmanian plant Coprosma quadrifida (F. Rubiaceae) according to the protocol outlined in Deans et al. [18]. Crystalline ASP was ground to a powder and homogenously combined with commercial standard chow powder (Barastoc, Victoria, Australia) and sucrose (4% w/w of food mash) in autoclaved water. The food pellets, each equivalent to 1 g containing a daily dose of 3 mg of crystalline ASP, were prepared and served daily in a small dish to the treated group. Similarly, a food pellet of 1 g containing a mixture of commercial standard chow powder and sucrose (4% w/w) was daily served in a small dish to the control group.
2.7. Sample Collection
At the end of 12 weeks of the experimental period, all mice were fasted overnight for 12 h before being euthanised by carbon dioxide asphyxiation for plasma and tissue collection. Blood samples were collected in a 1.5 mL Eppendorf tube containing 7.5 µL of Heparin (1000 U/mL) by cardiac puncture and kept on Ice. Plasma supernatants were collected by centrifugation (10 min, 12,000 × rpm, R.T.), aliquoted, and stored at −80 °C until use. Plasma levels of Leptin and Plasma plasminogen activator inhibitor-1 (PAI) were measured with a commercial Bio-plex pro mouse diabetes kit (Cat#171F7001M, Bio-Rad, Australia). The hypothalamus and liver were dissected, snap-frozen in liquid nitrogen, and stored at −80 °C for RNA extraction for gene expression studies.
2.8. RNA Extraction and cDNA Synthesis
Total RNA was extracted from hypothalamic and liver tissues using RNeasy Mini kit (Cat# 74104, Qiagen, Japan) and stored at −80 °C. The concentration and purity ratios (A260/280 and A260/230) of RNA were measured using NanoDropTM 8000 Spectrophotometer (NanoDrop Technologies Inc., Wilmington, DE, USA); only samples with optimum RNA integrity numbers were used for further processing. According to the manufacturer’s recommendations, complementary DNA (cDNA) was synthesised using iScript™ Reverse Transcription SuperMix kit (Cat# 1708840, Bio-Rad, South Granville NSW 2142, Australia). One microgram of RNA per sample in a final volume adjusted to 20 µL.
2.9. Primer Designing and Quantitative Real-Time PCR (qRT-PCR)
Gene-specific primer pairs for hypothalamic and hepatic markers responsible for food intake, inflammation and addiction were designed for exon-exon junction sequences to only amplify the transcript (mRNA) using the PrimerQuest tool (Integrated DNA Technologies, Inc., Clareville, IA, USA). The optimisation of custom-designed primers for the hypothalamus and liver was achieved with gradient qPCR to ensure the best melting temperature and efficiency to amplify the target gene. Quantitative PCR was performed using a QuantStudio™ 3 real-time PCR system (Thermo Fisher Scientific, Australia). Each PCR was performed in a 10 μL reaction mixture containing SsoAdvanced™ Universal Inhibitor-tolerant SYBR green SuperMix (Cat # 1725017, Bio-Rad, Australia), 2.5 ng/µL of cDNA, and 400 µM of primers according to the manufacturer’s instructions. All samples including housekeeping genes and controls were run in duplicates with qPCR conditions as follows: 3 min at 98 °C, followed by 40 cycles of 10 sec at 95 °C, 12 sec at 54–60 °C (optimal temperature for each primer pair), and 20 sec at 72 °C. The melting curve analysis was performed after each amplification to ensure the reliability of the results and product specificity. A GeNorm analysis was performed on the housekeeping genes across all the treatment groups to calculate the expression stability, while RefFinder algorithm was used to generate a comprehensive ranking [19]. Target gene expression was normalised against b-actin and ribosomal protein 19 housekeeping genes using a sample from the control group as a calibrator. All the analysis was performed using the comparative ΔΔCt method.
2.10. Statistical Analysis
Statistical analysis was performed using GraphPad Prism version 8.3.0 for Windows (GraphPad Software, San Diego, CA, USA, www.graphpad.com, accessed on 1 August 2022) and results were expressed as mean ± SEM. The effects of asperuloside on mRNA gene expression and plasma hormones were analysed by two-way ANOVA. ANOVA results were then followed by a post hoc analysis using Fisher’s least significant difference test (LSD) as appropriate. Results were considered statistically significant when p < 0.05. The effects of asperuloside on cell viability were analysed by one-way ANOVA. ANOVA results were then followed by a post hoc analysis using Fisher’s least significant difference test (LSD) as appropriate. Results were considered statistically significant when p < 0.05.
3. Results
3.1. Effect of ASP on Hypothalamic Genes
In mice consuming HFD, 12 weeks of ASP administration significantly reduced the mRNA expression levels of hypothalamic markers including agouti-related peptide (AgRP) (n = 6; F (3, 12) = 5.661; p < 0.05; Figure 1A) and neuropeptide Y (NPY) (n = 6; F (3, 15) = 3.668; p < 0.05; Figure 1B), interleukin 1 beta (IL-1) (n = 6; F (3, 12) = 9.250; p < 0.05; Figure 1C), interleukin 6 (IL-6) (n = 6; F (3, 12)= 13.17; p < 0.05; Figure 1D), and tumour necrosis factor-alpha (TNF-α) (n = 5–6; F (3, 15) = 12.40); p < 0.05; Figure 1E). ASP did not alter the hypothalamic mRNA expression of mice exposed to a standard diet. Overall, HFD increased the expression levels of these genes compared with the standard chow diet (HFD and HFD + ASP) vs. (CHOW and CHOW + ASP).
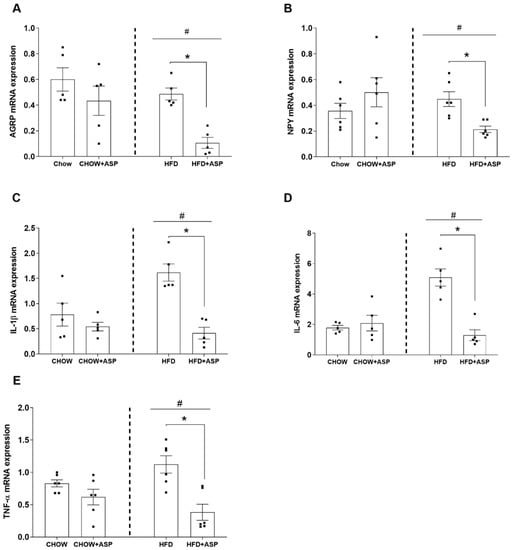
Figure 1.
Effect of asperuloside on hypothalamic genes involved in food intake and inflammation: (A) Agouti-related peptide (AgRP); (B) Neuropeptide Y (NPY); (C) Interleukin 1 beta (IL-1β); (D) Interleukin 6 (IL-6); and (E) Tumour necrosis factor-alpha (TNF-α). n = 6. Standard chow diet (CHOW), high-fat diet (HFD), asperuloside (ASP). Results are expressed as mean ± SEM. Data were analysed by Two-way ANOVA followed by a least significant difference. * Significant ASP effect (p < 0.05); # Significant overall diet effect [HFD and HFD + ASP] vs. [CHOW and CHOW + ASP] (p < 0.05).
3.2. Effects of ASP on Hepatic Genes Involved in Inflammation
In mice consuming HFD, 12 weeks of ASP administration significantly reduced the mRNA expression levels of IL-1β (n = 6; F (3, 15) = 7.062; p < 0.05; Figure 2A), IL-6 (n = 5; F (3, 12) = 13.17; p < 0.05; Figure 2B), TNF-α (n = 6; F (3, 15) = 12.40; p < 0.05; Figure 2C). ASP did not alter the hepatic mRNA expression of mice exposed to a standard diet. Overall, HFD increased the expression levels of these genes compared with the standard chow diet (HFD and HFD + ASP) vs. (CHOW and CHOW + ASP).
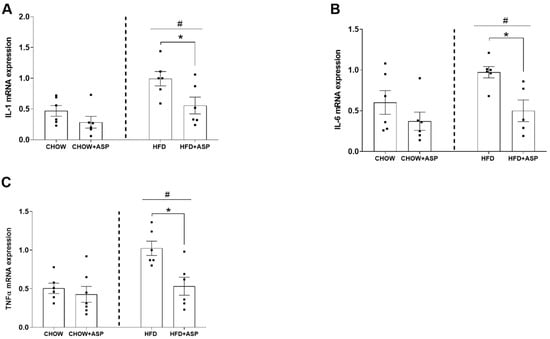
Figure 2.
Effect of asperuloside on hepatic genes involved in inflammation: (A) Interleukin 1 beta (IL-1β); (B) Interleukin 6 (IL-6); (C) Tumour necrosis factor-alpha (TNF-α). Standard chow diet (CHOW), High-fat diet (HFD), Asperuloside (ASP). n = 5–6. Standard chow diet (CHOW), high-fat diet (HFD), asperuloside (ASP). Results are expressed as mean ± SEM. Data were analysed by Two-way ANOVA followed by a least significant difference. * Significant ASP effect (p < 0.05); # Significant overall diet effect [HFD and HFD + ASP] vs. [CHOW and CHOW + ASP] (p < 0.05).
3.3. Effects of ASP on Plasma Hormones
In mice consuming HFD, 12 weeks of ASP administration significantly reduced the plasma levels of Leptin (n = 6; F (3, 15) = 6.867; p < 0.05; Figure 3A), and plasminogen activator inhibitor-1 (PAI) (n = 6; F (3, 15) = 3.412; p < 0.05; Figure 3B). Overall, HFD increased plasma Leptin and PAI-1 levels compared with the standard chow diet (HFD and HFD + ASP) vs. (CHOW and CHOW + ASP).
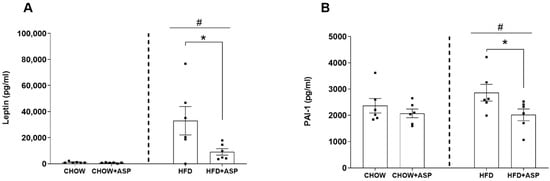
Figure 3.
Effect of asperuloside on plasma hormones: (A) Leptin; (B) Plasminogen activator inhibitor-1 (PAI); n = 6. Standard chow diet (CHOW), high-fat diet (HFD), asperuloside (ASP). Results are expressed as mean ± SEM. Data were analysed by Two-way ANOVA followed by a least significant difference. * Significant ASP effect (p < 0.05); # Significant overall diet effect [HFD and HFD + ASP] vs. [CHOW and CHOW + ASP] (p < 0.05).
3.4. Metabolic Toxicity of ASP In Vitro
ASP at doses up to 1 mM did not affect WST-1 absorbance (Figure 4A) or ATP-derived luminescence (Figure 4B) over 24 h. In addition, time course experiments up to 72 h at the highest concentration did not show any signs of metabolic toxicity in both assays (Figure 4C,D). In contrast, ASP significantly (p < 0.05) reduced colony formation at the highest concentration (1 mM) to 1000 mM (Figure 4E).
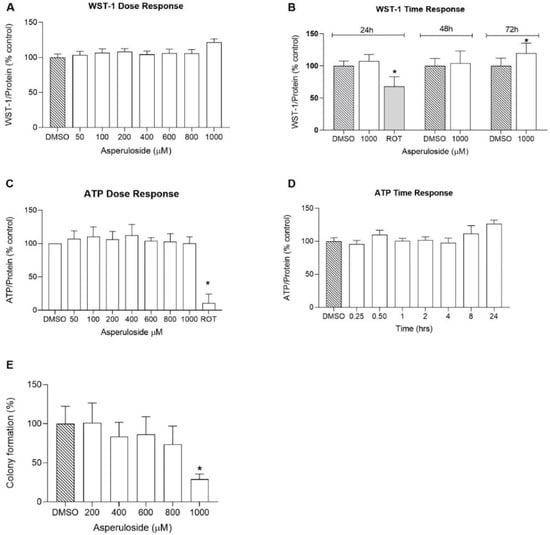
Figure 4.
Doses and time-dependent in vitro cell viability and survival assays: (A–D) HepG2 cell culture viability was measured with WST-1 and ATP assays under varying concentrations of ASP and incubation periods in the presence of vehicle (DMSO). ATP activity was measured at 750 nm, while WST-1 absorbance was measured at 450 nm. Data are expressed as mean ± S.E. (n = 6 wells per group). Data were analysed by one-way ANOVA followed by LSD test. * Significant effect (p < 0.05). (E) Long-term cell viability was measured with colony forming assay using varying concentrations of ASP. Error bars show the S.E. for at least four independent experiments, and every drug concentration was added in four replicates (n = 16). Data were analysed by one-way ANOVA followed by LSD test. * Significant effect (p < 0.05).
4. Discussion
In the present study, we performed gene expression studies in the hypothalamus and liver of obese mice highlighting some anti-inflammatory properties of the natural compound asperuloside (ASP) that might be responsible for its marked anti-obesity effects [11,12]. In addition, we performed a battery of in vitro experiments which demonstrated that ASP ameliorates mitochondrial function in liver cells.
In our previous study, oral ASP administration (3 mg/day) significantly reduced food intake and body weight only in mice consuming HFD compared with those eating a standard chow diet [11]. Similarly, ASP promoted a significant reduction in visceral adipose mass as well as blood glucose and insulin levels only in mice consuming HFD. In addition, we suggested that ASP might exert its therapeutic effect by altering fat and sweet receptors in the oral cavity, which are known to affect appetite, satiety and metabolism through afferent signalling to the hypothalamus, the section of the brain that regulates homeostatic energy responses to nutrient utilisation. However, the mechanisms by which ASP reduces food intake and the safety properties of the compound are still not fully elucidated. For these reasons, here we offer an integrative investigation of the safety features of the natural compound as well as an attempt to clarify the mechanisms of action by which it reduces food intake.
The hypothalamus is the area of the brain that regulates feeding behaviour [20]. Early lesion studies of hypothalamic regions resulted in changes in food intake, and, among several neuronal hypothalamic populations, the melanocortin system plays a major role in regulating feeding behaviours [3]. One subset of neurons of the melanocortin system expresses the orexigenic neuropeptides agouti-related peptide (AgRP) and neuropeptide Y (NPY), whereas another subset of neurons of the same system expresses anorexigenic peptides such as pro-opiomelanocortin (POMC) and amphetamine-regulated transcript (CART). Both subsets of hypothalamic neurons possess receptors that bind hormones regulating food intake, such as ghrelin, leptin and insulin, leading to a decreased or increased food intake depending on the energy demand [21]. During fasting, low levels of leptin and insulin and elevated ghrelin levels lead to the activation of AgRP/NPY neurons which in turn provide further signals to the hypothalamus to increase hunger and decrease energy expenditure. In contrast, the rise of leptin and insulin levels after a meal inhibit the activity of AgRP/NPY neurons stimulating POMC/CART neurons to promotes satiety and increase thermogenesis.
In our murine model, 12 weeks of ASP treatment significantly decreased the hypothalamic mRNA levels of the orexigenic peptides AgRP and NPY only in mice consuming HFD. Similarly, ASP reduced the orexigenic plasma leptin hormone in the same treatment group resulting in a 12.8% food intake reduction. Collectively, our last results reinforce our previous findings in which we suggested that ASP might induce weight loss via the downregulation of hypothalamic signalling [11].
Surprisingly, ASP treatment also decreased the hypothalamic mRNA levels of inflammatory markers IL-1, IL-6 and TNF-α as well. It is known that the pro-inflammatory cytokines IL-1, IL-6 and TNF-α decrease the anorectic effect of central leptin, impairing its ability to inhibit food intake [22]. It is also well known that in obesity, a low-grade inflammation affects several organs, including the liver, gut, adipose tissue and the brain [23]. It has to be specified that depending on the magnitude and duration, hypothalamic inflammation might lead to paradoxical effects on the regulation of food intake and body weight, either favouring a positive or negative energy balance [24].
For instance, in a systemic and/or acute infection, hypothalamic inflammation mediates the sickness response, which might result in fever, anorexia and cachexia, promoting a negative energy balance [24]. Conversely, chronic exposure to high-fat diets and saturated fats is associated with inflammation and altered control of energy homeostasis [25]. Recent evidence suggests that chronic high-fat diet (HFD) feeding triggers the release of pro-inflammatory cytokines such as TNF-α which in turn promotes the early onset of insulin and leptin resistance in the brain [26]. The literature also shows that in rodents consuming an HFD, hypothalamic inflammation develops prior to substantial weight gain, and it is evident in both rats and mice within 1 to 3 days of HFD consumption [27].
In our murine model, 12 weeks of ASP treatment reduced the mRNA hypothalamic levels of inflammatory markers such as IL-1, IL-6 and TNF-α, suggesting that the natural compound could ameliorate the consequences of hypothalamic inflammation by restoring the metabolic feedback signals from insulin, leptin and ghrelin [3]. However, further pharmacological studies are needed to elucidate the mechanistic properties of ASP in the hypothalamus that might affect the cross-link between peripheral signals and the central regulation of food intake.
Hypothalamic inflammation precedes inflammatory events in peripheral tissues such as the liver [28]. Pro-inflammatory cytokines such as IL-1, IL-6 and TNF-α play a major role in the development of insulin resistance, which is a key factor in the pathogenesis of non-alcoholic fatty liver disease (NAFLD), a common feature of obesity [29]. IL-1 and TNF-α can also induce PAI-1 production, a protein found elevated in obese patients and patients with cancer and metabolic syndrome, with increased occurrence of thrombosis [30]. In fact, recent literature demonstrated that elevated PAI-1 levels appear to increase the risk of atherothrombotic events and may also promote the progression of vascular disease [31]. In our study, ASP reduced PAI-1 in obese mice plausibly due to its anti-inflammatory role. We could speculate that the natural compound might reduce the risk of cardiovascular complications due to obesity as chronic administration of a Eucommia leaf extract (ASP is the main compound) restored vascular function and prevented hypertrophy of the thoracic aorta in obese rodents [32] and in spontaneously hypertensive rats [33].
Animal models have demonstrated that the pro-inflammatory cytokine IL-1 and its superfamily members are elevated under pathological conditions [34]. Their upregulation dramatically decreases hepatic inhibitor of kappa B (IκB) levels and NF-κB pathway activation, leading to IL-6 and TNFα secretion, which contributes to apoptosis, and ultimately to organ damage and animal death [35].
In previous in vivo investigations, ASP showed anti-inflammatory properties downregulating inflammatory markers such as IL-1, IL-6 and TNF-α in a mouse model of acute lung injury [13]. Similarly, in vitro studies demonstrated that pre-treatment with ASP remarkably blunted the phosphorylation of inhibitor of nuclear factor kappa-B (IκBα), extracellular signal-related kinases 1 and 2 (ERK1/2), c-Jun. N-Terminal kinase (JNK) and p38 mitogen-activated protein kinase (p38MAPK) in lipopolysaccharide (LPS)-induced inflammation in Raw 264.7 cells [13]. In line with previous results, our investigations support the reported anti-inflammatory properties of ASP. We demonstrated that the natural compound reduced the mRNA expression of inflammatory cytokines such as IL-1, IL-6 and TNF-α induced by chronic HFD consumption. Taken together, we speculate that ASP might exert its anti-inflammatory role via inhibition of the pro-inflammatory nuclear factor kappa-B (NF-κB) and MAPK phosphorylation via suppression of the NF-κB and mitogen-activated protein kinase (MAPK) signalling pathways [14,15,16]. Further studies such as immunohistochemical investigations or immunoassays are needed to validate the anti-inflammatory effects of ASP.
Since the safety properties of ASP were unknown, this study aimed to assess the effects of the natural compound on cellular viability using the human hepatocarcinoma cell line HepG2. This cell line is widely used for toxicity studies due to its high phenotypic stability for robust and reproducible outcomes, although HepG2 cells are less metabolically active compared with primary hepatocytes and other cell lines such as C3A or HepaRG [36].
First, we performed the colorimetric WST-1 assay to quantify cellular NAD(P)H synthesis as a surrogate marker for cellular viability. We evaluated both the time and dose–response properties of the compound, which did not show any sign of toxicity even at high concentrations (1000 µM) and after 72 h of incubation.
The measurement of cell viability can also be used to provide more accurate activity profiles of compounds, for example, to measure anabolic activity. Active cells generate ATP through mitochondrial oxidative phosphorylation, and for this reason, ATP can be used as an endpoint to study mitochondrial function [37]. In our experiments, HepG2 cells were treated with varying concentrations of ASP to investigate the dose-dependent effect of ASP on mitochondria. Our results demonstrate that the natural compound did not inhibit ATP levels even at a high concentration of 1000 μM, indicating ASP to be a mitochondrial-safe compound.
Overall, the results of this study indicate that ASP up to 1 mM does not negatively affect cell metabolism in general. However, at the highest concentration tested, it significantly reduced colony formation in vitro. This effect is likely due to the inhibitory activity of ASP towards iNOS, reported previously [16]. As a consequence of iNOS inhibition, signalling through the mitogen-activated protein kinase (MAKP) pathway is reduced, which could account for an inhibitory effect on cell growth, and therefore colony numbers. Given that most cells in an organism are quiescent, it remains to be demonstrated, if this in vitro observation has any relevance for ASP use in vivo. At most, highly proliferative tissues such as epithelia might be affected but given the required concentration observed in the present study, it is not clear if this concentration could be achieved through dietary ASP exposure and/or if epithelial tissues show different dose–responses. Then, as we wanted to investigate whether ASP would have any short time effect on the ATP levels, we carried out a time course experiment in which Hep2 cells were treated with ASP in different time intervals ranging from 15 min to 24 h, with the first treatment occurring after 6 h of cell seeding. Surprisingly, ASP increased the ATP levels after 24 h of incubation, indicating that the natural compound could improve mitochondrial function [38]. In addition, we complemented our toxicity investigations by performing a colony formation assay to assess the long-term toxicity effects of ASP. Our results indicated that the HepG2 colony number reached about a 30% reduction in 1000 µM of asperuloside treatment and a 100% reduction when treated with 2000 µM asperuloside. The half-maximal inhibitory concentration (IC50) of asperuloside on HepG2 was identified as a concentration of 1350µM. Collectively, our findings provided a reference for a dose selection in future animal studies suggesting that ASP is a safe compound for long-term use.
5. Conclusions
The pharmacological treatment of obesity has produced insufficient results due to the dubious safety and insufficient efficacy of the medications.
To the best of our knowledge, this is the first study assessing the safety properties of ASP as well as its anti-inflammatory role in the hypothalamus and liver of obese mice. We also confirmed the previously reported anti-obesity properties of ASP [9,10,11]. Specifically, we demonstrated that the natural compound reduces the blood levels of leptin and reduces the mRNA expression of orexigenic peptides such as NPY and AgRP, which contributes to the reduction in food intake reported in our previous study [11]. In addition, our additional results indicate that ASP reduces the hypothalamic and hepatic mRNA levels of pro-inflammatory cytokines, such as IL-1, IL-6 and TNF-α play, as well as the blood levels of PAI-1 which play a major role in the development of insulin resistance and cardiovascular complications. We also demonstrated that ASP is a safe compound for long-term use, and we provided a dose reference for future animal experiments.
Author Contributions
Conceptualisation, V.C.; Data curation, M.I. (Muhammad Ishaq); Formal analysis, M.I. (Muhammad Ishaq) and V.C.; Funding acquisition, V.C.; Investigation, M.I. (Muhammad Ishaq), D.T., C.Y., M.J.N., A.K., K.T., S.V. and T.A.; Methodology, V.C.; Resources, B.J.D., M.B., P.S., A.C.B. and J.A.S.; Software, M.I. (Muhammad Ishaq); Supervision, R.E., M.I. (Miguel Iglesias) and V.C.; Writing—original draft, M.I. (Miguel Iglesias) and V.C.; Writing—review and editing, C.R., C.V., M.R., M.Z., R.C., D.K.C., G.J., A.C.B., J.A.S., R.E., J.J.C., M.I. (Muhammad Ishaq), N.G. and V.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The animal study was reviewed and approved by Animal Ethics Committee University of Tasmania A0015841.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sanchis-Gomar, F.; Lavie, C.J.; Mehra, M.R.; Henry, B.M.; Lippi, G. Obesity and Outcomes in COVID-19: When an Epidemic and Pandemic Collide. Mayo Clin. Proc. 2020, 95, 1445–1453. [Google Scholar] [CrossRef]
- Hotamisligil, G.S. Inflammation and metabolic disorders. Nature 2006, 444, 860–867. [Google Scholar] [CrossRef]
- Jais, A.; Brüning, J.C. Hypothalamic inflammation in obesity and metabolic disease. J. Clin. Investig. 2017, 127, 24–32. [Google Scholar] [CrossRef]
- Powell, K. The two faces of fat. Nature 2007, 447, 525–527. [Google Scholar] [CrossRef]
- De Souza, C.T.; Araujo, E.P.; Bordin, S.; Ashimine, R.; Zollner, R.L.; Boschero, A.C.; Saad, M.J.; Velloso, L.A. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology 2005, 146, 4192–4199. [Google Scholar] [CrossRef]
- Yanovski, S.Z.; Yanovski, J.A. Obesity. N. Engl. J. Med. 2002, 346, 591–602. [Google Scholar] [CrossRef]
- Dietz, W.M.; Goodwin, N.J.; Yanovski, S.Z. Long-term pharmacotherapy in the management of obesity. JAMA 1996, 276, 1907–1915. [Google Scholar]
- Tak, Y.J.; Lee, S.Y. Anti-Obesity Drugs: Long-Term Efficacy and Safety: An Updated Review. World J. Mens Health 2021, 39, 208. [Google Scholar] [CrossRef]
- Hirata, T.; Kobayashi, T.; Wada, A.; Ueda, T.; Fujikawa, T.; Miyashita, H.; Ikeda, T.; Tsukamoto, S.; Nohara, T. Anti-obesity compounds in green leaves of Eucommia ulmoides. Bioorg. Med. Chem. Lett. 2011, 21, 1786–1791. [Google Scholar] [CrossRef]
- Fujikawa, T.; Hirata, T.; Hosoo, S.; Nakajima, K.; Wada, A.; Yurugi, Y.; Soya, H.; Matsui, T.; Yamaguchi, A.; Ogata, M.; et al. Asperuloside stimulates metabolic function in rats across several organs under high-fat diet conditions, acting like the major ingredient of Eucommia leaves with anti-obesity activity. J. Nutr. Sci. 2012, 1, e10. [Google Scholar] [CrossRef]
- Ishaq, M.; Tran, D.; Wu, Y.; Nowak, K.; Deans, B.J.; Xin, J.T.Z.; Loh, H.L.; Ng, W.Y.; Yee, C.W.; Southam, B.; et al. Asperuloside Enhances Taste Perception and Prevents Weight Gain in High-Fat Fed Mice. Front. Endocrinol. 2021, 12, 615446. [Google Scholar] [CrossRef]
- Chan, Y.; Ng, S.W.; Xin Tan, J.Z.; Gupta, G.; Tambuwala, M.M.; Bakshi, H.A.; Dureja, H.; Dua, K.; Ishaq, M.; Caruso, V.; et al. Emerging therapeutic potential of the iridoid molecule, asperuloside: A snapshot of its underlying molecular mechanisms. Chem. Biol. Interact. 2020, 315, 108911. [Google Scholar] [CrossRef]
- Qiu, J.; Chi, G.; Wu, Q.; Ren, Y.; Chen, C.; Feng, H. Pretreatment with the compound asperuloside decreases acute lung injury via inhibiting MAPK and NF-kappaB signaling in a murine model. Int. Immunopharmacol. 2016, 31, 109–115. [Google Scholar] [CrossRef]
- Mahbob, E.N.M.; Ahmad, R.; Ahmad, S. Nitric oxide (NO) radical inhibitory of Hedyotis philippinensis and its marker compound, asperuloside. Malays. J. Fundam. Appl. Sci. 2014, 10. [Google Scholar] [CrossRef]
- Tran, P.H.; Le, V.D.; Do, T.H.; Nguyen, T.L.; Nguyen, P.T.; Nguyen, T.T.; Nguyen, T.D. Anti-inflammatory constituents from Psychotria prainii H. Lév. Nat. Prod. Res. 2019, 33, 695–700. [Google Scholar] [CrossRef]
- He, J.; Lu, X.; Wei, T.; Dong, Y.; Cai, Z.; Tang, L.; Liu, M. Asperuloside and Asperulosidic Acid Exert an Anti-Inflammatory Effect via Suppression of the NF-κB and MAPK Signaling Pathways in LPS-Induced RAW 264.7 Macrophages. Int. J. Mol. Sci. 2018, 19, 2027. [Google Scholar] [CrossRef]
- Haefeli, R.H.; Erb, M.; Gemperli, A.C.; Robay, D.; Courdier Fruh, I.; Anklin, C.; Dallmann, R.; Gueven, N. NQO1-Dependent Redox Cycling of Idebenone: Effects on Cellular Redox Potential and Energy Levels. PLoS ONE 2011, 6, e17963. [Google Scholar] [CrossRef]
- Deans, B.J.; Bissember, A.C.; Smith, J.A. Practical isolation of Asperuloside from Coprosma quadrifida via rapid pressurised hot water extraction. Aust. J. Chem. 2016, 69, 1219–1222. [Google Scholar] [CrossRef]
- Vandesompele, J.; De Preter, K.; Pattyn, F.; Poppe, B.; Van Roy, N.; De Paepe, A.; Speleman, F. Accurate normalization of real-time quantitative RT-PCR data by geometric averaging of multiple internal control genes. Genome Biol. 2002, 3, 1–12. [Google Scholar] [CrossRef]
- Elmquist, J.K.; Elias, C.F.; Saper, C.B. From lesions to leptin: Hypothalamic control of food intake and body weight. Neuron 1999, 22, 221–232. [Google Scholar] [CrossRef]
- Elmquist, J.K.; Coppari, R.; Balthasar, N.; Ichinose, M.; Lowell, B.B. Identifying hypothalamic pathways controlling food intake, body weight, and glucose homeostasis. J. Comp. Neurol. 2005, 493, 63–71. [Google Scholar] [CrossRef]
- Luheshi, G.N.; Gardner, J.D.; Rushforth, D.A.; Loudon, A.S.; Rothwell, N.J. Leptin actions on food intake and body temperature are mediated by IL-1. Proc. Natl. Acad. Sci. USA 1999, 96, 7047–7052. [Google Scholar] [CrossRef]
- Rohm, T.V.; Meier, D.T.; Olefsky, J.M.; Donath, M.Y. Inflammation in obesity, diabetes, and related disorders. Immunity 2022, 55, 31–55. [Google Scholar] [CrossRef]
- Thaler, J.P.; Choi, S.J.; Schwartz, M.W.; Wisse, B.E. Hypothalamic inflammation and energy homeostasis: Resolving the paradox. Front. Neuroendocrinol. 2010, 31, 79–84. [Google Scholar] [CrossRef]
- Johnson, A.M.; Olefsky, J.M. The Origins and Drivers of Insulin Resistance. Cell 2013, 152, 673–684. [Google Scholar] [CrossRef]
- Romanatto, T.; Cesquini, M.; Amaral, M.E.; Roman, E.A.; Moraes, J.C.; Torsoni, M.A.; Cruz-Neto, A.P.; Velloso, L.A. TNF-alpha acts in the hypothalamus inhibiting food intake and increasing the respiratory quotient—Effects on leptin and insulin signaling pathways. Peptides 2007, 28, 1050–1058. [Google Scholar] [CrossRef]
- Thaler, J.P.; Yi, C.-X.; Schur, E.A.; Guyenet, S.J.; Hwang, B.H.; Dietrich, M.O.; Zhao, X.; Sarruf, D.A.; Izgur, V.; Maravilla, K.R.; et al. Obesity is associated with hypothalamic injury in rodents and humans. J. Clin. Investig. 2012, 122, 153–162. [Google Scholar] [CrossRef]
- Kleinridders, A.; Schenten, D.; Könner, A.C.; Belgardt, B.F.; Mauer, J.; Okamura, T.; Wunderlich, F.T.; Medzhitov, R.; Brüning, J.C. MyD88 signaling in the CNS is required for development of fatty acid-induced leptin resistance and diet-induced obesity. Cell Metab. 2009, 10, 249–259. [Google Scholar] [CrossRef]
- Engin, A. Non-Alcoholic Fatty Liver Disease. In Obesity and Lipotoxicity; Engin, A.B., Engin, A., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 443–467. [Google Scholar]
- Sillen, M.; Declerck, P.J. Targeting PAI-1 in Cardiovascular Disease: Structural Insights into PAI-1 Functionality and Inhibition. Front. Cardiovasc. Med. 2020, 7, 364. [Google Scholar] [CrossRef]
- Vaughan, D.E. PAI-1 and atherothrombosis. J. Thromb. Haemost. 2005, 3, 1879–1883. [Google Scholar] [CrossRef]
- Hosoo, S.; Koyama, M.; Watanabe, A.; Ishida, R.; Hirata, T.; Yamaguchi, Y.; Yamasaki, H.; Wada, K.; Higashi, Y.; Nakamura, K. Preventive effect of Eucommia leaf extract on aortic media hypertrophy in Wistar-Kyoto rats fed a high-fat diet. Hypertens. Res. 2017, 40, 546–551. [Google Scholar] [CrossRef]
- Hosoo, S.; Koyama, M.; Kato, M.; Hirata, T.; Yamaguchi, Y.; Yamasaki, H.; Wada, A.; Wada, K.; Nishibe, S.; Nakamura, K. The Restorative Effects of Eucommia ulmoides Oliver Leaf Extract on Vascular Function in Spontaneously Hypertensive Rats. Molecules 2015, 20, 21971–21981. [Google Scholar] [CrossRef]
- Sultan, M.; Ben-Ari, Z.; Masoud, R.; Pappo, O.; Harats, D.; Kamari, Y.; Safran, M. Interleukin-1α and Interleukin-1β play a central role in the pathogenesis of fulminant hepatic failure in mice. PLoS ONE 2017, 12, e0184084. [Google Scholar] [CrossRef]
- Barbier, L.; Ferhat, M.; Salamé, E.; Robin, A.; Herbelin, A.; Gombert, J.-M.; Silvain, C.; Barbarin, A. Interleukin-1 Family Cytokines: Keystones in Liver Inflammatory Diseases. Front. Immunol. 2019, 10, 2014. [Google Scholar] [CrossRef]
- Feng, Z.; Sedeeq, M.; Daniel, A.; Corban, M.; Woolley, K.L.; Condie, R.; Azimi, I.; Smith, J.A.; Gueven, N. Comparative In Vitro Toxicology of Novel Cytoprotective Short-Chain Naphthoquinones. Pharmaceuticals 2020, 13, 184. [Google Scholar] [CrossRef]
- Vander Heiden, M.G.; Cantley, L.C.; Thompson, C.B. Understanding the Warburg effect: The metabolic requirements of cell proliferation. Science 2009, 324, 1029–1033. [Google Scholar] [CrossRef]
- Marroquin, L.D.; Hynes, J.; Dykens, J.A.; Jamieson, J.D.; Will, Y. Circumventing the Crabtree Effect: Replacing Media Glucose with Galactose Increases Susceptibility of HepG2 Cells to Mitochondrial Toxicants. Toxicol. Sci. 2007, 97, 539–547. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).