The Behavior of Self-Monitoring of Blood Glucose and Glycemic Control in Taiwanese Population
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
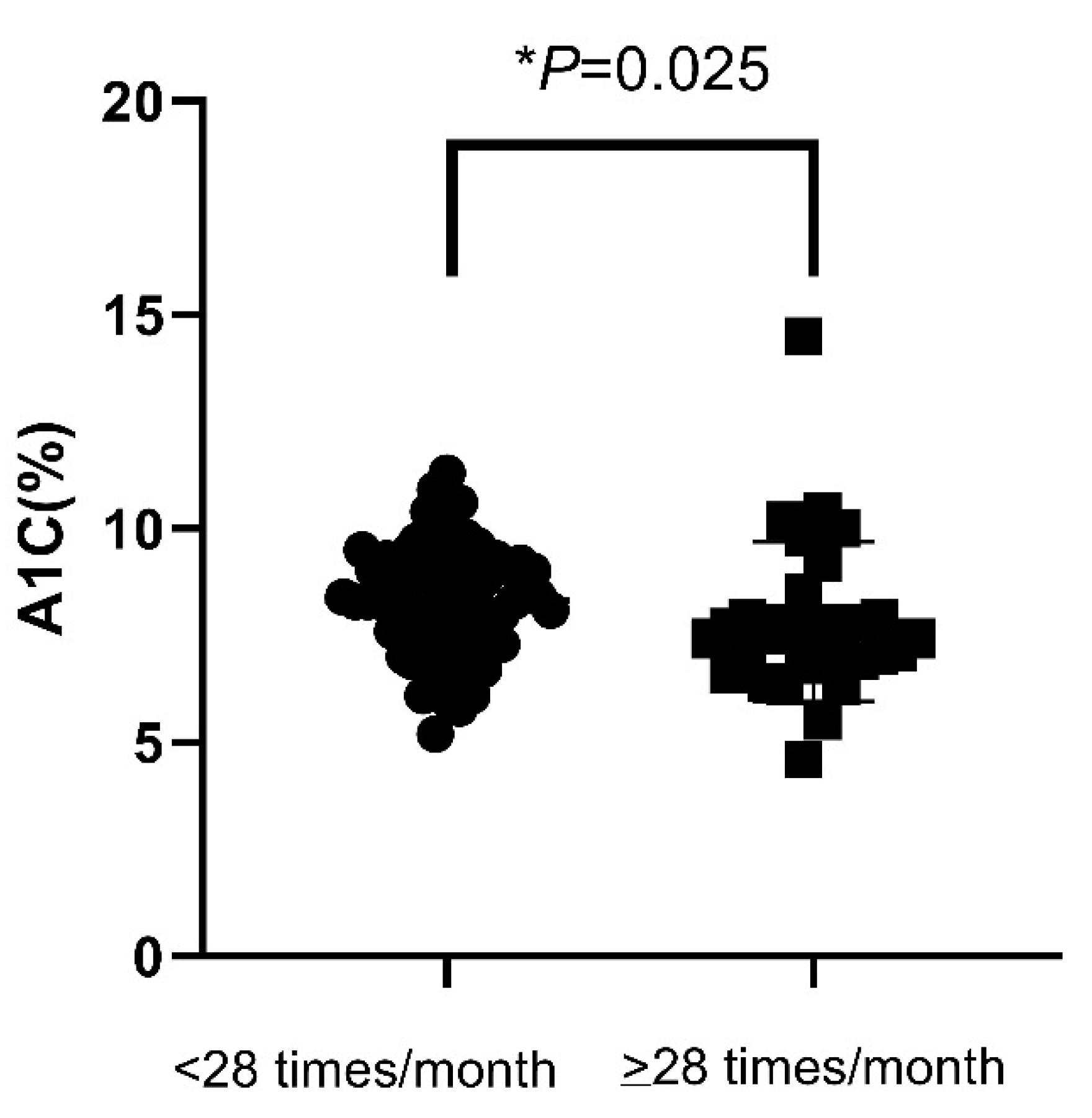
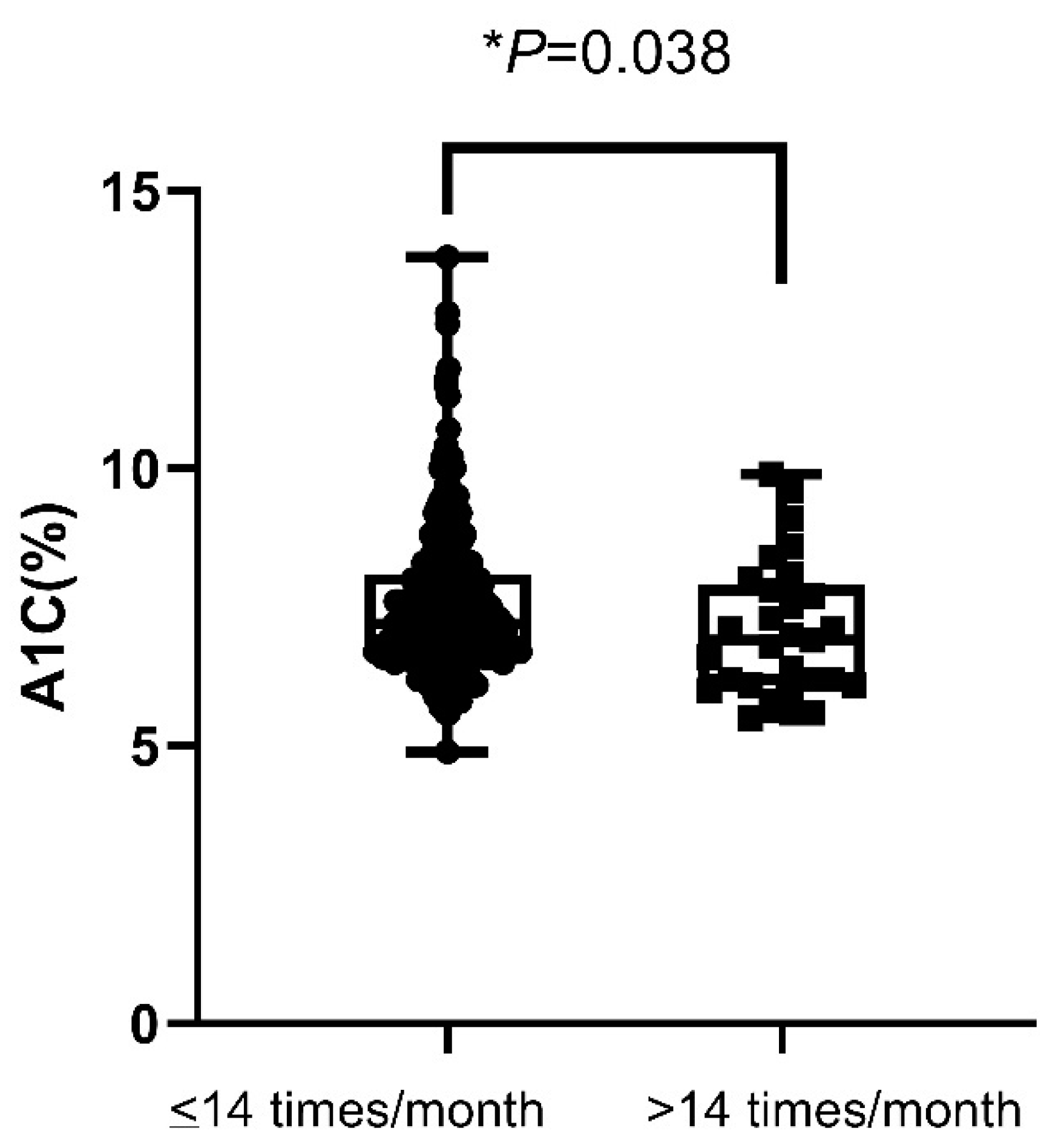
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44, S85–S99. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.M.; Beck, R.W.; Bergenstal, R.M.; Goland, R.S.; Haller, M.J.; McGill, J.B.; Rodriguez, H.; Simmons, J.H.; Hirsch, I.B. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care 2013, 36, 2009–2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ziegler, R.; Heidtmann, B.; Hilgard, D.; Hofer, S.; Rosenbauer, J.; Holl, R. Frequency of SMBG correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatric Diabetes 2011, 12, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, J.; Davies, M.; Home, P.D.; Larsen, J.; Koenen, C.; Schernthaner, G. A randomised, 52-week, treat-to-target trial comparing insulin detemir with insulin glargine when administered as add-on to glucose-lowering drugs in insulin-naive people with type 2 diabetes. Diabetologia 2008, 51, 408–416. [Google Scholar] [CrossRef] [Green Version]
- Garber, A.J. Treat-to-target trials: Uses, interpretation and review of concepts. Diabetes Obes. Metab. 2014, 16, 193–205. [Google Scholar] [CrossRef] [Green Version]
- Nauck, M.A.; Haastert, B.; Trautner, C.; Müller, U.A.; Nauck, M.A.; Heinemann, L. A randomised, controlled trial of self-monitoring of blood glucose in patients with type 2 diabetes receiving conventional insulin treatment. Diabetologia 2014, 57, 868–877. [Google Scholar] [CrossRef]
- Murata, G.H.; Shah, J.H.; Hoffman, R.M.; Wendel, C.S.; Adam, K.D.; Solvas, P.A.; Bokhari, S.U.; Duckworth, W.C. Intensified blood glucose monitoring improves glycemic control in stable, insulin-treated veterans with type 2 diabetes: The Diabetes Outcomes in Veterans Study (DOVES). Diabetes Care 2003, 26, 1759–1763. [Google Scholar] [CrossRef] [Green Version]
- Farmer, A.; Wade, A.; Goyder, E.; Yudkin, P.; French, D.; Craven, A.; Holman, R.; Kinmonth, A.L.; Neil, A. Impact of self monitoring of blood glucose in the management of patients with non-insulin treated diabetes: Open parallel group randomised trial. BMJ (Clin. Res. Ed.) 2007, 335, 132. [Google Scholar] [CrossRef] [Green Version]
- O’Kane, M.J.; Bunting, B.; Copeland, M.; Coates, V.E. Efficacy of self monitoring of blood glucose in patients with newly diagnosed type 2 diabetes (ESMON study): Randomised controlled trial. BMJ 2008, 336, 1174–1177. [Google Scholar] [CrossRef] [Green Version]
- Simon, J.; Gray, A.; Clarke, P.; Wade, A.; Neil, A.; Farmer, A. Cost effectiveness of self monitoring of blood glucose in patients with non-insulin treated type 2 diabetes: Economic evaluation of data from the DiGEM trial. BMJ 2008, 336, 1177–1180. [Google Scholar] [CrossRef] [Green Version]
- Young, L.A.; Buse, J.B.; Weaver, M.A.; Vu, M.B.; Mitchell, C.M.; Blakeney, T.; Grimm, K.; Rees, J.; Niblock, F.; Donahue, K.E. Glucose Self-monitoring in Non-Insulin-Treated Patients With Type 2 Diabetes in Primary Care Settings: A Randomized Trial. JAMA Intern. Med. 2017, 177, 920–929. [Google Scholar] [CrossRef] [PubMed]
- Polonsky, W.H.; Fisher, L.; Schikman, C.H.; Hinnen, D.A.; Parkin, C.G.; Jelsovsky, Z.; Petersen, B.; Schweitzer, M.; Wagner, R.S. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, noninsulin-treated type 2 diabetes: Results from the Structured Testing Program study. Diabetes Care 2011, 34, 262–267. [Google Scholar] [CrossRef] [Green Version]
- Mannucci, E.; Antenore, A.; Giorgino, F.; Scavini, M. Effects of Structured Versus Unstructured Self-Monitoring of Blood Glucose on Glucose Control in Patients With Non-insulin-treated Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials. J. Diabetes Sci. Technol. 2018, 12, 183–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malanda, U.L.; Welschen, L.M.C.; Riphagen, I.I.; Dekker, J.M.; Nijpels, G.; Bot, S.D.M. Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Cochrane Database Syst. Rev. 2012, 1, CD005060. [Google Scholar] [CrossRef] [Green Version]
- Willett, L.R.; ACP Journal Club. Meta-analysis: Self-monitoring in non-insulin-treated type 2 diabetes improved HbA1c by 0.25%. Ann. Intern. Med. 2012, 156, Jc6-12. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2022. Diabetes Care 2021, 45, S17–S38. [Google Scholar] [CrossRef]
- Cheung, A.K.L. Structured Questionnaires. In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 6399–6402. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee 6. Glycemic Targets: Standards of Medical Care in Diabetes—2022. Diabetes Care 2021, 45, S83–S96. [Google Scholar] [CrossRef]
- Blood Glucose Monitoring Devices. Available online: https://www.fda.gov/medical-devices/in-vitro-diagnostics/blood-glucose-monitoring-devices (accessed on 24 March 2022).
- Cheng, A.Y. Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada. Introduction. Can. J. Diabetes 2013, 37 (Suppl. 1), S1–S3. [Google Scholar] [CrossRef] [Green Version]
- Gryczynski, J.; Nordeck, C.; Mitchell, S.G.; O’Grady, K.E.; McNeely, J.; Wu, L.T.; Schwartz, R.P. Reference periods in retrospective behavioral self-report: A qualitative investigation. Am. J. Addict. 2015, 24, 744–747. [Google Scholar] [CrossRef] [Green Version]
- Association, A.D. Standards of Medical Care in Diabetes—2010. Diabetes Care 2010, 33, S11–S61. [Google Scholar] [CrossRef] [Green Version]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Ghasemi, A.; Zahediasl, S. Normality tests for statistical analysis: A guide for non-statisticians. Int. J. Endocrinol. Metab. 2012, 10, 486–489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guidelines: Self-Monitoring of Blood Glucose in Non-Insulin Treated Type 2 Diabetes. Available online: https://www.idf.org/e-library/guidelines/85-self-monitoring-of-blood-glucose-in-non-insulin-treated-type-2-diabetes.html (accessed on 23 January 2022).
- Self-Monitoring Blood Glucose (SMBG) Frequency & Pattern Tool. Available online: https://guidelines.diabetes.ca/self-management/smbg-tool (accessed on 23 January 2022).
- Nathan, D.M.; Genuth, S.; Lachin, J.; Cleary, P.; Crofford, O.; Davis, M.; Rand, L.; Siebert, C. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Wambui Charity, K.; Kumar, A.M.V.; Hinderaker, S.G.; Chinnakali, P.; Pastakia, S.D.; Kamano, J. Do diabetes mellitus patients adhere to self-monitoring of blood glucose (SMBG) and is this associated with glycemic control? Experiences from a SMBG program in western Kenya. Diabetes Res. Clin. Pract. 2016, 112, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Iwuala, S.O.; Olamoyegun, M.A.; Sabir, A.A.; Fasanmade, O.A. The relationship between self-monitoring of blood glucose and glycaemic control among patients attending an urban diabetes clinic in Nigeria. Ann. Afr. Med. 2015, 14, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.C.; Burns, E.; Whittle, J.; Fleming, R.; Knudson, P.; Flax, S.; Leventhal, H. Randomized trial of technology-assisted self-monitoring of blood glucose by low-income seniors: Improved glycemic control in type 2 diabetes mellitus. J. Behav. Med. 2016, 39, 1001–1008. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Tan, D.H.Y.; Lee, J.Y. Evaluating the impact of self-monitoring of blood glucose frequencies on glucose control in patients with type 2 diabetes who do not use insulin: A systematic review and meta-analysis. Int. J. Clin. Pract. 2019, 73, e13357. [Google Scholar] [CrossRef]
| ALL | Insulin Group | No Insulin Group | |
|---|---|---|---|
| (n = 382) | (n = 92) | (n = 290) | |
| Age | 65.11 ± 11.78 | 67.08 ± 12.13 | 64.48 ± 11.60 |
| Gender | |||
| male | 163 (42.67%) | 41 (44.57%) | 122 (42.07%) |
| female | 219 (57.33%) | 51 (55.43%) | 168 (57.93%) |
| Durations of diabetes | 11.61 ± 8.65 | 15.01 ± 9.70 | 8.83 ± 7.71 |
| Type of treatment | |||
| diet only | 6 (1.57%) | - | 6 (2.07%) |
| oral hypoglycemic agents only | 284 (74.35%) | - | 284 (97.93%) |
| insulin once/day | 27 (7.07%) | 27 (29.35%) | - |
| insulin twice/day | 65 (17.02%) | 65 (70.65%) | - |
| insulin ≥ three times/day | 0 (0.00%) | 0 (0.00%) | - |
| Hypoglycemia | 41 (10.73%) | 22 (23.91%) | 19 (6.55%) |
| A1C (%) | 7.66 ± 1.38 | 8.17 ± 1.50 | 7.50 ± 1.29 |
| A1C ≤ 7% | 150 (39.27%) | 22 (23.91%) | 128 (44.14%) |
| Behaviors | Patients |
|---|---|
| Frequency (n = 382) | |
| none | 131 (34.29%) |
| 1 time | 7 (1.83%) |
| 2 to 4 times | 72 (18.85%) |
| 5 to 14 times | 105 (27.49%) |
| over 14 times | 67 (17.54%) |
| Time (n = 381) | |
| did not check | 131 (34.38%) |
| before breakfast | 214 (56.17%) |
| after breakfast | 52 (13.65%) |
| before lunch | 16 (4.20%) |
| after lunch | 20 (5.25%) |
| before dinner | 34 (8.92%) |
| after dinner | 34 (8.90%) |
| before sleep | 21 (5.51%) |
| during discomfort | 11 (2.89%) |
| Number of times a day (n = 250) | |
| fixed at 1 time | 145 (58.00%) |
| 2 separate times | 79 (31.60%) |
| 3 separate times | 15 (6.00%) |
| 4 separate times | 5 (2.00%) |
| 5 separate times | 3 (1.20%) |
| 6 separate times | 2 (0.80%) |
| 7 separate times | 1 (0.40%) |
| Questions | Almost Never | Less Than Half of the Time | About Half of the Time | Most of the Time | Usually |
|---|---|---|---|---|---|
| (<20%) | (20–40%) | (40–60%) | (60–80%) | (>80%) | |
| Record the results on a piece of paper or book. | 61 (24.50%) | 24 (9.64%) | 25 (10.04%) | 32 (12.85%) | 107 (42.97%) |
| Review the reason for hypoglycemia or hyperglycemia according to the results of SMBG. | 7 (2.81%) | 15 (6.02%) | 29 (11.65%) | 46 (18.47%) | 152 (61.04%) |
| Adjust the drugs according to the results of SMBG. | 192 (77.11%) | 32 (12.85%) | 7 (2.81%) | 11 (4.42%) | 7 (2.81%) |
| Give the results of SMBG to medical personnel. | 67 (26.91%) | 39 (15.66%) | 27 (10.84%) | 33 (13.25%) | 83 (33.33%) |
| Compare the results of SMBG to laboratory-measured fasting plasma glucose annually. | 181 (72.69%) | 36 (14.46%) | 9 (3.61%) | 12 (4.82%) | 11 (4.42%) |
| Questions | Almost Never | Less than Half of the Time | About Half of the Time | Most of the Time | Usually | p Value |
|---|---|---|---|---|---|---|
| (<20%) | (20–40%) | (40–60%) | (60–80%) | (>80%) | ||
| A1C | ||||||
| Record the results on a piece paper or book. | 7.61 ± 1.34 | 8.14 ± 1.60 | 7.62 ± 1.24 | 7.32 ± 1.20 | 7.71 ± 1.39 | 0.284 |
| Review the reasons of hypoglycemia and hyperglycemia. | 9.19 ± 2.51 | 8.15 ± 1.95 | 8.23 ± 1.43 | 7.39 ± 1.24 | 7.52 ± 1.18 | 0.000 |
| Adjust the drugs according to the results of SMBG. | 7.66 ± 1.44 | 7.53 ± 1.23 | 6.90 ± 0.43 | 8.25 ± 1.07 | 8.26 ± 0.95 | 0.099 |
| Give the results of SMBG to medical personnel. | 7.67 ± 1.37 | 7.93 ± 1.47 | 7.50 ± 1.15 | 7.38 ± 1.23 | 7.70 ± 1.43 | 0.375 |
| Compare the results of SMBG to laboratory-measured fasting plasma glucose annually. | 7.70 ± 1.46 | 7.41 ± 0.97 | 8.10 ± 1.50 | 7.46 ± 0.97 | 7.74 ± 1.10 | 0.908 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, C.; Tseng, C.-H.; Liao, K.C.-W.; Yang, H.-J.; Chen, P.-Y.; Perng, M.-D. The Behavior of Self-Monitoring of Blood Glucose and Glycemic Control in Taiwanese Population. Endocrines 2022, 3, 214-222. https://doi.org/10.3390/endocrines3020019
Lu C, Tseng C-H, Liao KC-W, Yang H-J, Chen P-Y, Perng M-D. The Behavior of Self-Monitoring of Blood Glucose and Glycemic Control in Taiwanese Population. Endocrines. 2022; 3(2):214-222. https://doi.org/10.3390/endocrines3020019
Chicago/Turabian StyleLu, Ching, Chin-Hsiao Tseng, Karen Chia-Wen Liao, Hong-Jyh Yang, Pei-Yu Chen, and Ming-Der Perng. 2022. "The Behavior of Self-Monitoring of Blood Glucose and Glycemic Control in Taiwanese Population" Endocrines 3, no. 2: 214-222. https://doi.org/10.3390/endocrines3020019
APA StyleLu, C., Tseng, C.-H., Liao, K. C.-W., Yang, H.-J., Chen, P.-Y., & Perng, M.-D. (2022). The Behavior of Self-Monitoring of Blood Glucose and Glycemic Control in Taiwanese Population. Endocrines, 3(2), 214-222. https://doi.org/10.3390/endocrines3020019







