Upfront Normothermic Machine Perfusion for a Liver Graft with Severe Macrovesicular Steatosis: A Proof-of-Concept Case
Abstract
:1. Introduction
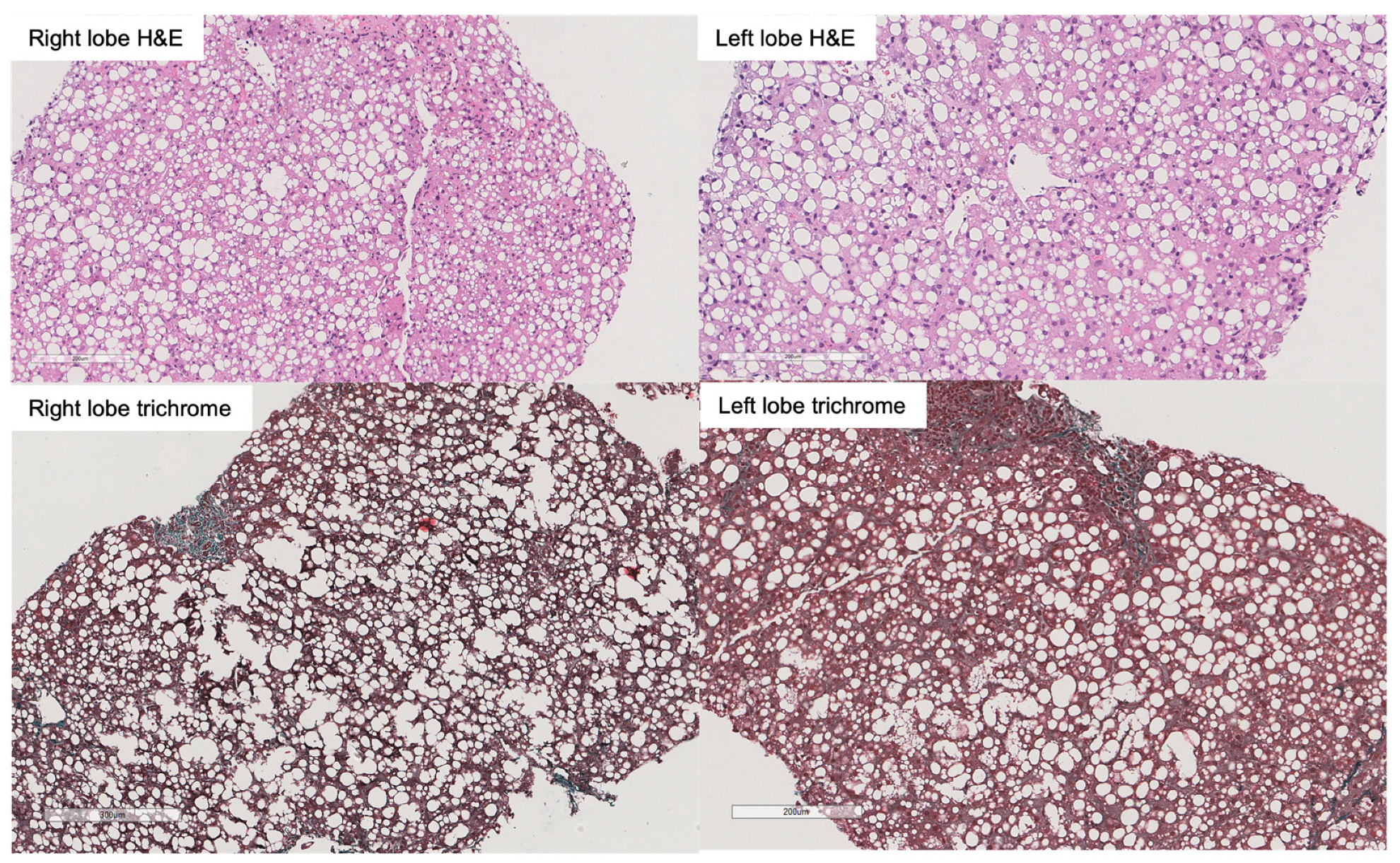
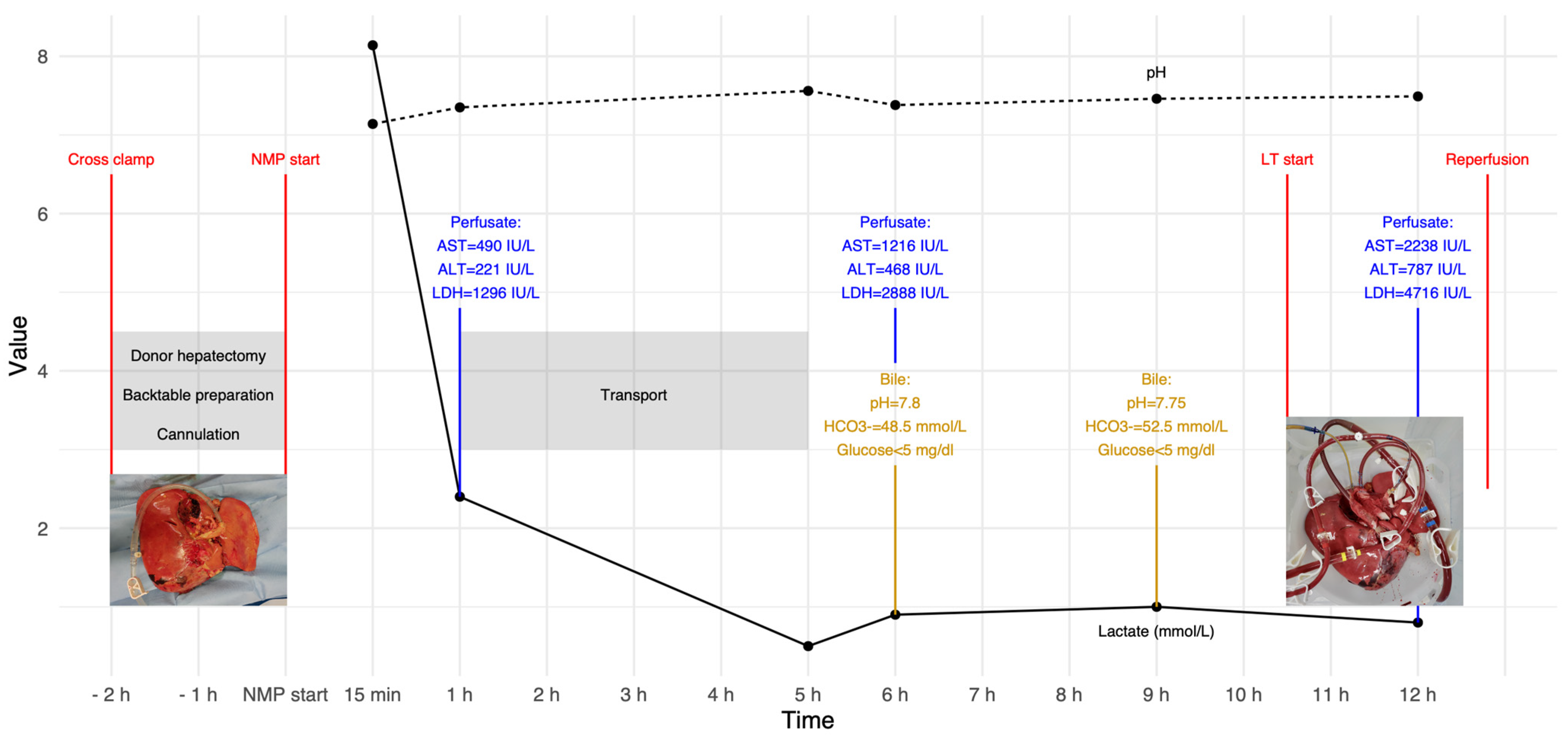
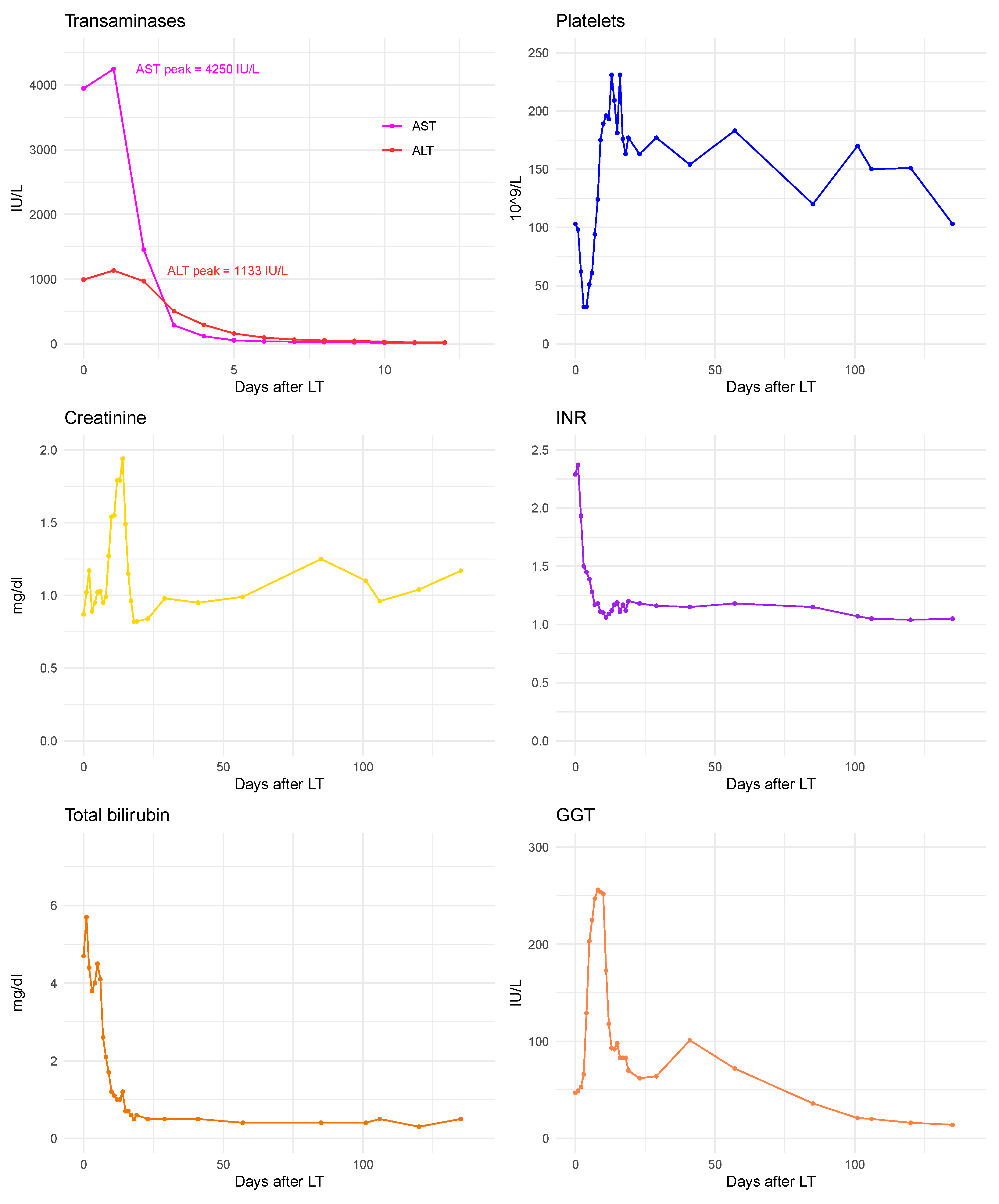
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Croome, K.P.; Lee, D.D.; Taner, C.B. The “Skinny” on Assessment and Utilization of Steatotic Liver Grafts: A Systematic Review. Liver Transplant. 2019, 25, 488–499. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M. Non-alcoholic fatty liver disease—A global public health perspective. J. Hepatol. 2019, 70, 531–544. [Google Scholar] [CrossRef] [PubMed]
- Ceresa, C.D.L.; Nasralla, D.; Watson, C.J.E.; Butler, A.J.; Coussios, C.C.; Crick, K.; Hodson, L.; Imber, C.; Jassem, W.; Knight, S.R.; et al. Transient Cold Storage Prior to Normothermic Liver Perfusion May Facilitate Adoption of a Novel Technology. Liver Transplant. 2019, 25, 1503–1513. [Google Scholar] [CrossRef]
- Chen, M.; Chen, Z.; Lin, X.; Hong, X.; Ma, Y.; Huang, C.; He, X.; Ju, W. Application of ischaemia-free liver transplantation improves prognosis of patients with steatotic donor livers—A retrospective study. Transpl. Int. 2021, 34, 1261–1270. [Google Scholar] [CrossRef]
- Fodor, M.; Cardini, B.; Peter, W.; Weissenbacher, A.; Oberhuber, R.; Hautz, T.; Otarashvili, G.; Margreiter, C.; Maglione, M.; Resch, T.; et al. Static cold storage compared with normothermic machine perfusion of the liver and effect on ischaemic-type biliary lesions after transplantation: A propensity score-matched study. Br. J. Surg. 2021, 108, 1082–1089. [Google Scholar] [CrossRef]
- Guarrera, J.V.; Henry, S.D.; Samstein, B.; Reznik, E.; Musat, C.; Lukose, T.I.; Ratner, L.E.; Brown, R.S., Jr.; Kato, T.; Emond, J.C. Hypothermic machine preservation facilitates successful transplantation of “orphan” extended criteria donor livers. Am. J. Transplant. 2015, 15, 161–169. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Guo, Z.; Zhao, Q.; Ju, W.; Wang, D.; Wu, L.; Yang, L.; Ji, F.; Tang, Y.; Zhang, Z.; et al. The first case of ischemia-free organ transplantation in humans: A proof of concept. Am. J. Transplant. 2018, 18, 737–744. [Google Scholar] [CrossRef]
- Kron, P.; Schlegel, A.; Mancina, L.; Clavien, P.A.; Dutkowski, P. Hypothermic oxygenated perfusion (HOPE) for fatty liver grafts in rats and humans. J. Hepatol. 2018, 68, 82–91. [Google Scholar] [CrossRef]
- Mergental, H.; Laing, R.W.; Kirkham, A.J.; Perera, M.; Boteon, Y.L.; Attard, J.; Barton, D.; Curbishley, S.; Wilkhu, M.; Neil, D.A.H.; et al. Transplantation of discarded livers following viability testing with normothermic machine perfusion. Nat. Commun. 2020, 11, 2939. [Google Scholar] [CrossRef]
- Patrono, D.; Catalano, G.; Rizza, G.; Lavorato, N.; Berchialla, P.; Gambella, A.; Caropreso, P.; Mengozzi, G.; Romagnoli, R. Perfusate Analysis During Dual Hypothermic Oxygenated Machine Perfusion of Liver Grafts: Correlations with Donor Factors and Early Outcomes. Transplantation 2020, 104, 1929–1942. [Google Scholar] [CrossRef]
- Patrono, D.; Cussa, D.; Sciannameo, V.; Montanari, E.; Panconesi, R.; Berchialla, P.; Lepore, M.; Gambella, A.; Rizza, G.; Catalano, G.; et al. Outcome of liver transplantation with grafts from brain-dead donors treated with dual hypothermic oxygenated machine perfusion, with particular reference to elderly donors. Am. J. Transplant. 2022, 22, 1382–1395. [Google Scholar] [CrossRef] [PubMed]
- Patrono, D.; De Carlis, R.; Gambella, A.; Farnesi, F.; Podesta, A.; Lauterio, A.; Tandoi, F.; De Carlis, L.; Romagnoli, R. Viability assessment and transplantation of fatty liver grafts using end-ischemic normothermic machine perfusion. Liver Transplant. 2022, 29, 508–520. [Google Scholar] [CrossRef] [PubMed]
- Rayar, M.; Beaurepaire, J.M.; Bajeux, E.; Hamonic, S.; Renard, T.; Locher, C.; Desfourneaux, V.; Merdrignac, A.; Bergeat, D.; Lakehal, M.; et al. Hypothermic Oxygenated Perfusion Improves Extended Criteria Donor Liver Graft Function and Reduces Duration of Hospitalization Without Extra Cost: The PERPHO Study. Liver Transplant. 2021, 27, 349–362. [Google Scholar] [CrossRef]
- Watson, C.J.E.; Kosmoliaptsis, V.; Pley, C.; Randle, L.; Fear, C.; Crick, K.; Gimson, A.E.; Allison, M.; Upponi, S.; Brais, R.; et al. Observations on the ex situ perfusion of livers for transplantation. Am. J. Transplant. 2018, 18, 2005–2020. [Google Scholar] [CrossRef] [PubMed]
- Ghinolfi, D.; Lai, Q.; Dondossola, D.; De Carlis, R.; Zanierato, M.; Patrono, D.; Baroni, S.; Bassi, D.; Ferla, F.; Lauterio, A.; et al. Machine Perfusions in Liver Transplantation: The Evidence-Based Position Paper of the Italian Society of Organ and Tissue Transplantation. Liver Transplant. 2020, 26, 1298–1315. [Google Scholar] [CrossRef]
- Ravikumar, R.; Jassem, W.; Mergental, H.; Heaton, N.; Mirza, D.; Perera, M.T.; Quaglia, A.; Holroyd, D.; Vogel, T.; Coussios, C.C.; et al. Liver Transplantation After Ex Vivo Normothermic Machine Preservation: A Phase 1 (First-in-Man) Clinical Trial. Am. J. Transplant. 2016, 16, 1779–1787. [Google Scholar] [CrossRef] [PubMed]
- Vogel, T.; Brockmann, J.G.; Quaglia, A.; Morovat, A.; Jassem, W.; Heaton, N.D.; Coussios, C.C.; Friend, P.J. The 24-hour normothermic machine perfusion of discarded human liver grafts. Liver Transplant. 2017, 23, 207–220. [Google Scholar] [CrossRef]
- Nasralla, D.; Coussios, C.C.; Mergental, H.; Akhtar, M.Z.; Butler, A.J.; Ceresa, C.D.L.; Chiocchia, V.; Dutton, S.J.; Garcia-Valdecasas, J.C.; Heaton, N.; et al. A randomized trial of normothermic preservation in liver transplantation. Nature 2018, 557, 50–56. [Google Scholar] [CrossRef]
- Matton, A.P.M.; de Vries, Y.; Burlage, L.C.; van Rijn, R.; Fujiyoshi, M.; de Meijer, V.E.; de Boer, M.T.; de Kleine, R.H.J.; Verkade, H.J.; Gouw, A.S.H.; et al. Biliary Bicarbonate, pH, and Glucose Are Suitable Biomarkers of Biliary Viability During Ex Situ Normothermic Machine Perfusion of Human Donor Livers. Transplantation 2019, 103, 1405–1413. [Google Scholar] [CrossRef]
- Mergental, H.; Perera, M.T.; Laing, R.W.; Muiesan, P.; Isaac, J.R.; Smith, A.; Stephenson, B.T.; Cilliers, H.; Neil, D.A.; Hubscher, S.G.; et al. Transplantation of Declined Liver Allografts Following Normothermic Ex-Situ Evaluation. Am. J. Transplant. 2016, 16, 3235–3245. [Google Scholar] [CrossRef]
- van Leeuwen, O.B.; Bodewes, S.B.; Lantinga, V.A.; Haring, M.P.D.; Thorne, A.M.; Bruggenwirth, I.M.A.; van den Berg, A.P.; de Boer, M.T.; de Jong, I.E.M.; de Kleine, R.H.J.; et al. Sequential hypothermic and normothermic machine perfusion enables safe transplantation of high-risk donor livers. Am. J. Transplant. 2022, 22, 1658–1670. [Google Scholar] [CrossRef] [PubMed]
- Watson, C.J.E.; Gaurav, R.; Fear, C.; Swift, L.; Selves, L.; Ceresa, C.D.L.; Upponi, S.S.; Brais, R.; Allison, M.; Macdonald-Wallis, C.; et al. Predicting Early Allograft Function After Normothermic Machine Perfusion. Transplantation 2022, 106, 2391–2398. [Google Scholar] [CrossRef] [PubMed]
- Croome, K.P. Introducing Machine Perfusion into Routine Clinical Practice for Liver Transplantation in the United States: The Moment Has Finally Come. J. Clin. Med. 2023, 12, 909. [Google Scholar] [CrossRef]
- Mergental, H.; Stephenson, B.T.F.; Laing, R.W.; Kirkham, A.J.; Neil, D.A.H.; Wallace, L.L.; Boteon, Y.L.; Widmer, J.; Bhogal, R.H.; Perera, M.; et al. Development of Clinical Criteria for Functional Assessment to Predict Primary Nonfunction of High-Risk Livers Using Normothermic Machine Perfusion. Liver Transplant. 2018, 24, 1453–1469. [Google Scholar] [CrossRef] [PubMed]
- Olthoff, K.M.; Kulik, L.; Samstein, B.; Kaminski, M.; Abecassis, M.; Emond, J.; Shaked, A.; Christie, J.D. Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors. Liver Transplant. 2010, 16, 943–949. [Google Scholar] [CrossRef]
- Agopian, V.G.; Harlander-Locke, M.P.; Markovic, D.; Dumronggittigule, W.; Xia, V.; Kaldas, F.M.; Zarrinpar, A.; Yersiz, H.; Farmer, D.G.; Hiatt, J.R.; et al. Evaluation of Early Allograft Function Using the Liver Graft Assessment Following Transplantation Risk Score Model. JAMA Surg. 2018, 153, 436–444. [Google Scholar] [CrossRef]
- Avolio, A.W.; Franco, A.; Schlegel, A.; Lai, Q.; Meli, S.; Burra, P.; Patrono, D.; Ravaioli, M.; Bassi, D.; Ferla, F.; et al. Development and Validation of a Comprehensive Model to Estimate Early Allograft Failure Among Patients Requiring Early Liver Retransplant. JAMA Surg. 2020, 155, e204095. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef]
- Hann, A.; Lembach, H.; Dassanayake, B.; Carvalheiro, A.; McKay, S.; Rajoriya, N.; Armstrong, M.J.; Bartlett, D.; David, M.; Perera, M. Severe Sepsis Mimicking Primary Nonfunction Following Liver Transplantation: Normothermic Machine Perfusion Is a Potential Environment for Bacterial Overgrowth and Transmission From Donor to Recipient. A Case Report. Transplant. Proc. 2020, 52, 2781–2785. [Google Scholar] [CrossRef]
- Lau, N.-S.; Ly, M.; Dennis, C.; Toomath, S.; Huang, J.L.; Huang, J.; Ly, H.; Chanda, S.; Marinelli, T.; Davis, R.; et al. Microbial Contamination During Long-term Ex Vivo Normothermic Machine Perfusion of Human Livers. Transplantation, 2023; online ahead of print. [Google Scholar] [CrossRef]
- Tandoi, F.; Salizzoni, M.; Brunati, A.; Lupo, F.; Romagnoli, R. Excellent outcomes of liver transplantation using severely steatotic grafts from brain-dead donors. Liver Transplant. 2016, 22, 377–378. [Google Scholar] [CrossRef]
- Patrono, D.; Surra, A.; Catalano, G.; Rizza, G.; Berchialla, P.; Martini, S.; Tandoi, F.; Lupo, F.; Mirabella, S.; Stratta, C.; et al. Hypothermic Oxygenated Machine Perfusion of Liver Grafts from Brain-Dead Donors. Sci. Rep. 2019, 9, 9337. [Google Scholar] [CrossRef] [PubMed]
- Patrono, D.; Zanierato, M.; Vergano, M.; Magaton, C.; Diale, E.; Rizza, G.; Catalano, S.; Mirabella, S.; Cocchis, D.; Potenza, R.; et al. Normothermic Regional Perfusion and Hypothermic Oxygenated Machine Perfusion for Livers Donated After Controlled Circulatory Death With Prolonged Warm Ischemia Time: A Matched Comparison With Livers From Brain-Dead Donors. Transpl. Int. 2022, 35, 10390. [Google Scholar] [CrossRef] [PubMed]
- Schlegel, A.; de Rougemont, O.; Graf, R.; Clavien, P.A.; Dutkowski, P. Protective mechanisms of end-ischemic cold machine perfusion in DCD liver grafts. J. Hepatol. 2013, 58, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Muller, X.; Schlegel, A.; Kron, P.; Eshmuminov, D.; Wurdinger, M.; Meierhofer, D.; Clavien, P.A.; Dutkowski, P. Novel Real-time Prediction of Liver Graft Function During Hypothermic Oxygenated Machine Perfusion Before Liver Transplantation. Ann. Surg. 2019, 270, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Patrono, D.; Roggio, D.; Mazzeo, A.T.; Catalano, G.; Mazza, E.; Rizza, G.; Gambella, A.; Rigo, F.; Leone, N.; Elia, V.; et al. Clinical assessment of liver metabolism during hypothermic oxygenated machine perfusion using microdialysis. Artif. Organs 2022, 46, 281–295. [Google Scholar] [CrossRef] [PubMed]
- Schlegel, A.; Muller, X.; Mueller, M.; Stepanova, A.; Kron, P.; de Rougemont, O.; Muiesan, P.; Clavien, P.A.; Galkin, A.; Meierhofer, D.; et al. Hypothermic oxygenated perfusion protects from mitochondrial injury before liver transplantation. EBioMedicine 2020, 60, 103014. [Google Scholar] [CrossRef]
- Sousa Da Silva, R.X.; Weber, A.; Dutkowski, P.; Clavien, P.A. Machine perfusion in liver transplantation. Hepatology 2022, 76, 1531–1549. [Google Scholar] [CrossRef]
- Guo, Z.; Zhao, Q.; Jia, Z.; Huang, C.; Wang, D.; Ju, W.; Zhang, J.; Yang, L.; Huang, S.; Chen, M.; et al. A randomized-controlled trial of ischemia-free liver transplantation for end-stage liver disease. J. Hepatol. 2023, 79, 394–402. [Google Scholar] [CrossRef]
- Cucchetti, A.; Vivarelli, M.; Ravaioli, M.; Cescon, M.; Ercolani, G.; Piscaglia, F.; Del Gaudio, M.; Grazi, G.L.; Ridolfi, L.; Pinna, A.D. Assessment of donor steatosis in liver transplantation: Is it possible without liver biopsy? Clin. Transplant. 2009, 23, 519–524. [Google Scholar] [CrossRef]
- Cesaretti, M.; Brustia, R.; Goumard, C.; Cauchy, F.; Pote, N.; Dondero, F.; Paugam-Burtz, C.; Durand, F.; Paradis, V.; Diaspro, A.; et al. Use of Artificial Intelligence as an Innovative Method for Liver Graft Macrosteatosis Assessment. Liver Transplant. 2020, 26, 1224–1232. [Google Scholar] [CrossRef]
| Perfusate Composition (Priming) | ||
| Product | Dilution | Volume |
| 4% Succinylated gelatine | n/a | 500 mL |
| Third party ABO-compatible PRBC | n/a | 3 units |
| Meropenem | 500 mg/10 mL | 10 mL |
| Heparin | 5000 u/mL | 2 mL |
| 10% calcium gluconate | 94 mg/mL | 10 mL |
| 8.4% sodium bicarbonate | 84 mg/mL | 20 mL * |
| Infusion Solutions | ||
| Product | Dilution | Infusion rate |
| Sodium taurocholate | 5.6 g/30 mL | 1.25 mL/h |
| Epoprostenol sodium | 0.25 mg/30 mL | 1.25 mL/h |
| Heparin | 25,000 u/30 mL | 1.25 mL/h |
| Insulin | 200 u/30 mL | 1.25 mL/h |
| Parenteral Nutrition | ||
| Product | Dilution | Infusion rate |
| Clinimix E5/25 | n/a | 0.5 mL/min ** |
| Author, Year | n | Intervention | Findings |
|---|---|---|---|
| Watson et al., 2018 [14] | 1 | End-ischemic NMP | One liver described as “very steatotic” was accepted for research but not transplanted. Perfusate ALT level was 7542 IU/L at 2 h and the liver showed no glucose metabolism |
| Ceresa et al., 2019 [3] | 1 | End-ischemic NMP | Of 3 (9.7%) discarded livers, one DBD liver with 80% MaS was discarded due to insufficient lactate clearance, as well as lack of bile production and glucose metabolism |
| Mergental et al., 2020 [9] | 2 | End-ischemic NMP | Of 9 (29%) discarded livers, 2 had moderate or severe MaS, respectively. Prevalence of medium-large droplet steatosis was higher among discarded livers (77.8% vs. 40.9%). No liver with MaS ≥ 30% was accepted for LT |
| Fodor et al., 2021 [5] | 3 | End-ischemic NMP | Of 59 included patients, 3 (5.1%) received a liver with MaS ≥ 30%. Specific outcomes were not reported |
| Patrono et al., 2022 [12] | 14 | End-ischemic NMP | Of 14 evaluated livers with MaS ≥ 30%, 10 (71%) were transplanted but 2 (14%) developed PNF. Graft function was good in the remaining patients |
| He et al., 2018 [7] | 1 | IFLT | First report of IFLT in a liver from a DBD donor with 85–95% MaS. |
| Chen et al., 2021 [4] | 26 | IFLT | Twenty-six livers with moderate (n = 16) or severe (n = 10) MaS were included, of which six were treated by IFLT. IFLT was associated with reduced AST, GGT and creatinine peak after LT, and lower EAD rate (0% vs. 60%, p = 0.001) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patrono, D.; Apostu, A.L.; Rizza, G.; Cussa, D.; Barreca, A.; Limoncelli, S.; Mirabella, S.; Romagnoli, R. Upfront Normothermic Machine Perfusion for a Liver Graft with Severe Macrovesicular Steatosis: A Proof-of-Concept Case. Transplantology 2023, 4, 151-160. https://doi.org/10.3390/transplantology4030015
Patrono D, Apostu AL, Rizza G, Cussa D, Barreca A, Limoncelli S, Mirabella S, Romagnoli R. Upfront Normothermic Machine Perfusion for a Liver Graft with Severe Macrovesicular Steatosis: A Proof-of-Concept Case. Transplantology. 2023; 4(3):151-160. https://doi.org/10.3390/transplantology4030015
Chicago/Turabian StylePatrono, Damiano, Ana Lavinia Apostu, Giorgia Rizza, Davide Cussa, Antonella Barreca, Selene Limoncelli, Stefano Mirabella, and Renato Romagnoli. 2023. "Upfront Normothermic Machine Perfusion for a Liver Graft with Severe Macrovesicular Steatosis: A Proof-of-Concept Case" Transplantology 4, no. 3: 151-160. https://doi.org/10.3390/transplantology4030015
APA StylePatrono, D., Apostu, A. L., Rizza, G., Cussa, D., Barreca, A., Limoncelli, S., Mirabella, S., & Romagnoli, R. (2023). Upfront Normothermic Machine Perfusion for a Liver Graft with Severe Macrovesicular Steatosis: A Proof-of-Concept Case. Transplantology, 4(3), 151-160. https://doi.org/10.3390/transplantology4030015






