Double Versus Single Cervical Cerclage in Women with Cervical Insufficiency: A Systematic Review of Prophylactic and Emergency Indications
Abstract
1. Introduction
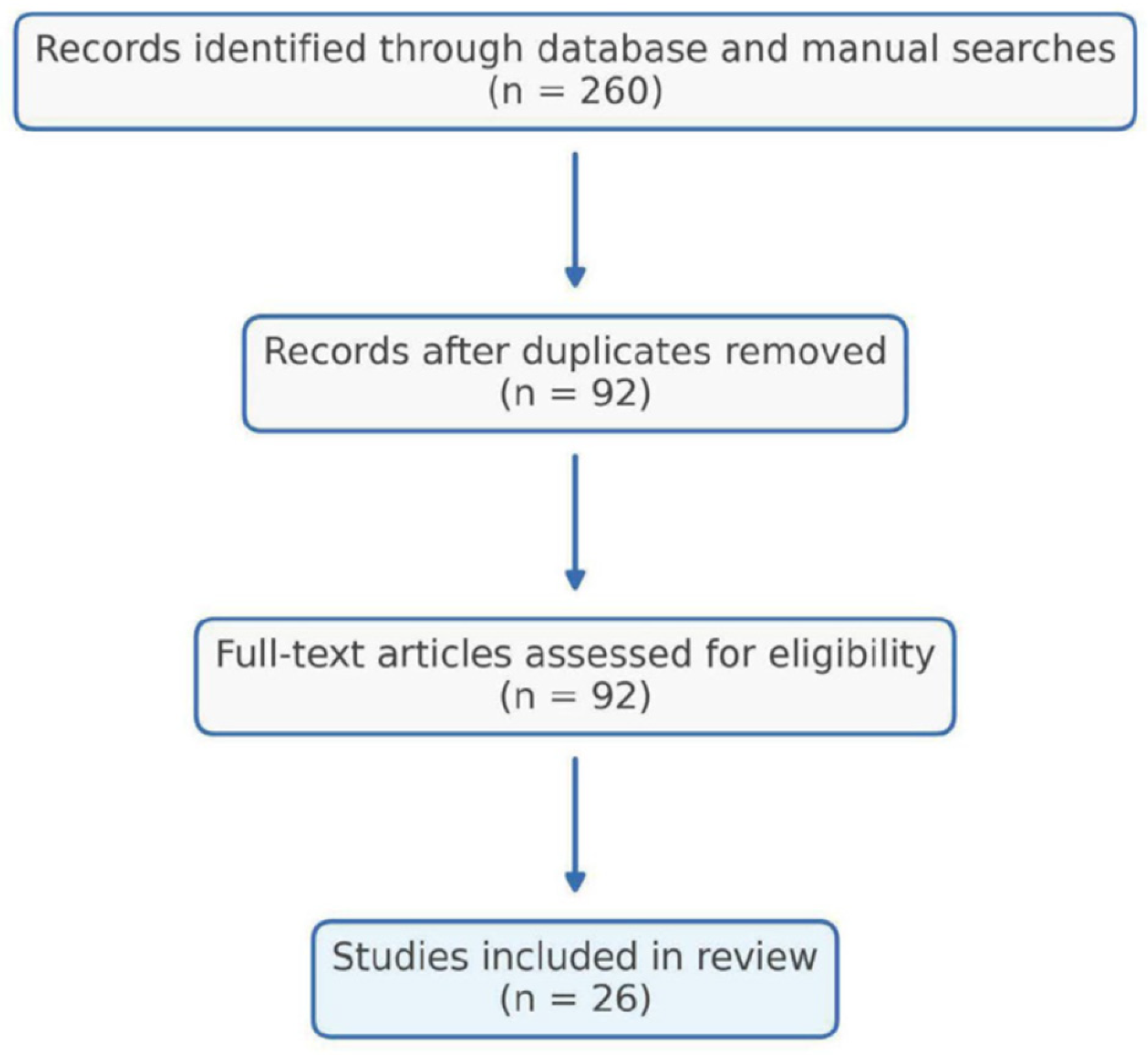
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
2.4. Study Selection
2.5. Data Extraction and Management
2.6. Risk of Bias and Quality Assessment
2.7. Synthesis of Results
2.8. Limitations
3. Results
3.1. Study Selection and Characteristics
- 6 Randomized Controlled Trials or Randomized Abstract Studies
- 6 Comparative Cohort or Matched Case–control Studies
- 3 Published Study Protocols for Ongoing or Completed Randomized Trials (including the CERVO protocol and its corresponding completed RCT outcome report)
- 4 Case Series or Single Case Reports
- 3 Systematic Reviews or Meta-Analyses
- 2 Conference Abstracts
- 2 Historical or Early Technical Descriptions (Including the Foundational Reports From 1987 and 1999)
3.2. Early Evidence
3.3. Indications
3.4. Populations
3.5. Designs
3.6. Outcomes in HI and UI Cerclage
3.7. Outcomes in Emergency Cerclage (ECC)
3.8. Outcomes in Emergency Cerclage (ECC) of Twin Pregnancies
3.9. Modified Double-Level Techniques
3.10. Case Reports and Technical Variations
3.11. Overall Synthesis
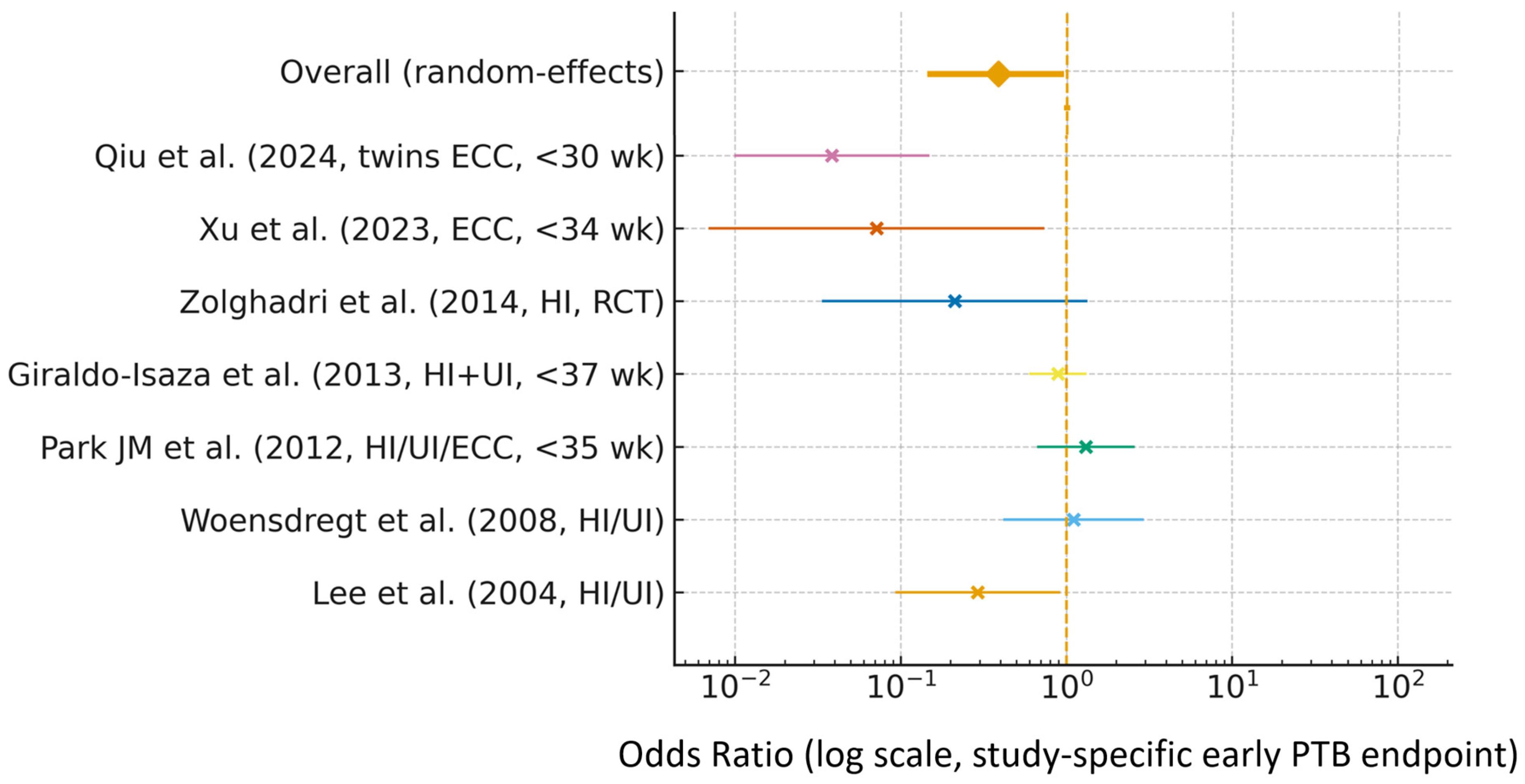
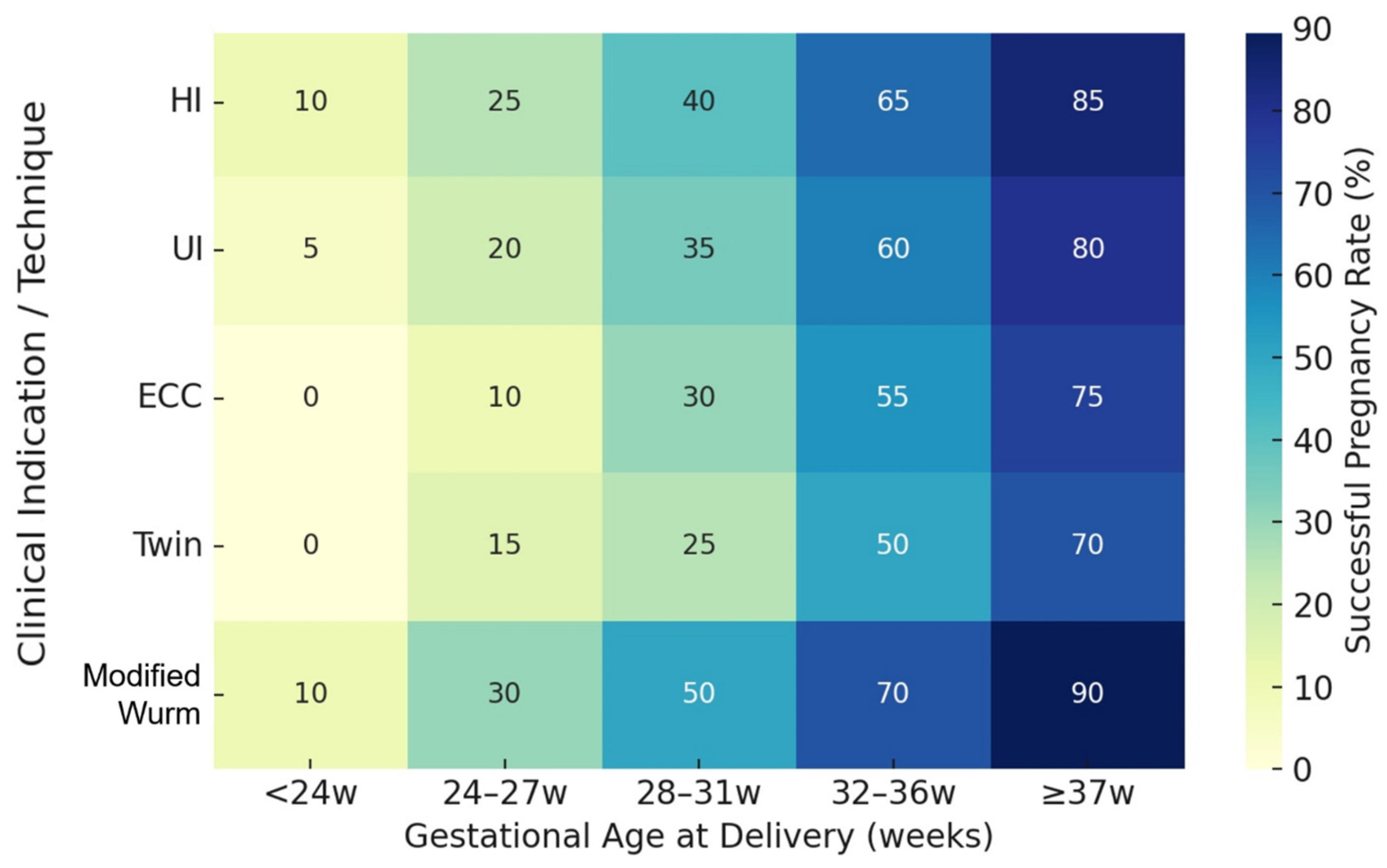
3.12. Quantitative Overview
4. Discussion
4.1. HI and UI Cerclage
- Woensdregt et al. [7] reported similar PTB < 34 weeks (18.4% vs. 16.8%) and comparable median GA (38.3 vs. 38.0 weeks).
- Park JM et al. [17] noted that two stitches allowed higher suture placement but did not improve outcomes.
- Giraldo-Isaza et al. [11] likewise found no overall benefit, though they observed a non-significant trend toward fewer very early PTBs (<28 and <24 weeks) in UI cases managed with double cerclage—suggesting that additional mechanical reinforcement may be advantageous in women with pronounced cervical shortening or funneling, a finding echoed later by Xu ZM et al. [15].
- Broumand et al. [9] reported improved rates of viable extreme preterm birth and more favorable early neonatal outcomes with double cerclage compared with traditional cerclage, although interpretation is limited by small sample size, heterogeneous techniques, and the atypical use of an occlusive distal stitch.
- Zolghadri et al. [10] found later GA at delivery with double cerclage women with recurrent mid-trimester losses, although other outcomes did not differ significantly.
- Earlier Korean experience, particularly Lee et al. [6], also demonstrated improved pregnancy prolongation and reduced preterm delivery rates using a modified double-level technique reinforced with fibrin sealant, though results were limited to a single-center cohort.
4.2. Emergency Cerclage (ECC)
- Xu Z-M et al. [12]—Retrospective case–control study of singleton pregnancies with emergency indications: double cerclage achieved significantly longer GA at delivery (32.7 ± 5.5 vs. 28.0 ± 4.7 weeks, p = 0.028), lower PTB < 34 and <32 weeks, and reduced NICU admission and stay. Neonatal survival was comparable. The matched design under true emergency conditions minimized selection bias.
- Xu ZM et al. [15]—A stratified randomized controlled trial found no benefit in UI cases, but in emergencies, double cerclage markedly reduced extreme PTB < 28 weeks (12% vs. 40%, p = 0.024) and prolonged latency, providing the strongest prospective evidence of context-dependent benefit.
- Park and Park [28]—A series of 25 women referred after failed initial cerclage underwent removal of the prior suture and a second emergent double McDonald cerclage. Seventy-five percent delivered beyond 29 weeks—even when re-cerclage occurred after 24 weeks—challenging the traditional view that re-cerclage beyond 24 weeks is contraindicated.
- Qiu et al. [13]—Extended ECC indications to twin pregnancies (18–26 weeks) using a combined McDonald–Shirodkar (functionally double-level) technique. The double-level group achieved longer latency (56 vs. 28 days), higher GA (30.5 vs. 27.0 weeks), and reduced perinatal mortality, particularly with ≥3 cm dilation.
4.3. Mechanistic Insights
- Mechanical reinforcement: Placement of two sutures distributes tension more evenly across the cervix, reducing the risk of suture cutting and maintaining a higher level of cervical closure. This configuration provides greater structural support, minimizing recurrent dilation or downward suture migration.
- Preservation of the mucus plug: Multiple authors (e.g., Namouz et al. [27]; Becher et al. [28]) have proposed that double cerclage more effectively preserves the integrity of the endocervical mucus plug, thereby maintaining local antimicrobial defense and decreasing the likelihood of ascending intrauterine infection.
- Barrier effect of sealant and occlusion: Korean studies [4,5,6] incorporating fibrin sealant reinforcement and cervical occlusion have reported additive protective effects, helping to prevent infection and premature rupture of membranes. Notably, the pioneering work of Baumgarten and Moser [29] demonstrated that fibrin adhesion applied to a modified single cerclage could prolong gestation by creating both a physical and biological barrier within the cervical canal. Subsequent Korean protocols advanced this principle by placing fibrin sealant between two separate sutures, thereby forming a multilayered barrier that not only reinforces mechanical closure but also preserves the integrity of the cervical mucus plug—an important component of local immune defense against ascending infection. This conceptual evolution represents a logical extension from single to double suturing, integrating both mechanical and biological protection.
4.4. Modified Double-Level Techniques
- Banerjee et al. [25]: Preliminary data from high-risk singleton pregnancies suggested comparable trends favoring the modified Wurm type cerclage technique, although full peer-reviewed results remain unavailable.
4.5. Ongoing Trials and Future Directions
4.6. Synthesis and Interpretation of Findings
- Emergency settings:
- Prophylactic (HI and UI) settings:
- Modified and adjunctive techniques:
- Historical context:
- Future research:
4.7. Clinical Implications and Limitations
- Phase 1: Conceptual Foundation (1987–2007)
- Phase 2: Transition and Reassessment (2008–2015)
- Phase 3: Evidence Refinement and International Expansion (2016–2025)
- Phase 4—Future Directions: Technological and Clinical Frontiers (2025 → Beyond)
- (1)
- Next-Generation Technical Evolution
- (2)
- Large-Scale Evidence and Multicenter Trials
- (3)
- Data Harmonization and Registry-Driven Analytics
- (4)
- Refined Indication Stratification
- (5)
- Biomechanical and Infection-Immunologic Insights
- Integrative Concluding Statement
5. Conclusions and Future Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shirodkar, V.N. A new method of operative treatment for habitual abortions in the second trimester of pregnancy. Antiseptic 1955, 52, 299–300. [Google Scholar]
- McDonald, I.A. Suture of the cervix for inevitable miscarriage. J. Obstet. Gynaecol. Br. Emp. 1957, 64, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, M.; Sanada, H.; Tsuda, A.; Hirano, H.; Tanaka, T. Modified cervical cerclage in pregnant women with advanced bulging membranes: Knee-chest positioning. Acta Obstet. Gynecol. Scand. 1999, 78, 779–782. [Google Scholar] [PubMed]
- Park, M.I.; Lee, M.H.; Kong, M.S.; Hwang, J.H.; Chung, S.R.; Moon, H. Clinical experience of 15 cases of modified McDonald cerclage using Beriplast™ in incompetent internal os of cervix. Korean J. Obstet. Gynecol. 2000, 43, 1407–1413. Available online: https://www.ogscience.org/journal/view.php?number=4106 (accessed on 20 November 2025). (In Korean with English Abstract).
- Choi, J.S.; Park, M.S.; Kim, Y.J.; Bae, E.K.; Paek, J.H.; Park, M.I. The comparison between modified transvaginal cerclage and transabdominal cervicoisthmic cerclage after a failure of previous transvaginal cerclage in incompetent internal os of cervix patients. Korean J. Obstet. Gynecol. 2003, 46, 624–631. Available online: https://www.ogscience.org/journal/view.php?number=3130 (accessed on 20 November 2025). (In Korean with English Abstract).
- Lee, S.H.; Yoon, H.J.; Lee, Y.O.; Kim, H.H.; Han, H.J.; Park, M.I. Comparison of outcomes of incompetent cervix patients treated with the transvaginal cerclage and the modified transvaginal cerclage using fibrin sealant. J. Korean Soc. Perinatol. 2004, 15, 147–153. Available online: http://www.perinatol.or.kr/html/sub04_05.asp (accessed on 20 November 2025). (In Korean with English Abstract).
- Woensdregt, K.; Norwitz, E.R.; Cackovic, M.; Paidas, M.J.; Illuzzi, J.L. Effect of 2 stitches vs. 1 stitch on the prevention of preterm birth in women with singleton pregnancies who undergo cervical cerclage. Am. J. Obstet. Gynecol. 2008, 198, 396.e1–396.e7. [Google Scholar] [CrossRef]
- Tsai, Y.L.; Lin, Y.H.; Chong, K.M.; Hsieh, T.T. Effectiveness of double cervical cerclage in women with at least one previous pregnancy loss in the second trimester: A randomized controlled trial. J. Obstet. Gynaecol. Res. 2009, 35, 666–671. [Google Scholar] [CrossRef]
- Broumand, F.; Bahadori, F.; Behrouzilak, T.; Yekta, Z.; Ashrafi, F. Viable Extreme Preterm Birth and Some Neonatal Outcomes in Double Cerclage versus Traditional Cerclage: A Randomized Clinical Trial. Sci. World J. 2011, 11, 1660–1666. [Google Scholar] [CrossRef]
- Zolghadri, J.; Younesi, M.; Asadi, N.; Khosravi, D.; Behdin, S.; Tavana, Z.; Ghaffarpasand, F. Double versus single cervical cerclage for patients with recurrent pregnancy loss: A randomized clinical trial. J. Obstet. Gynaecol. Res. 2014, 40, 375–380. [Google Scholar] [CrossRef]
- Giraldo-Isaza, M.A.; Fried, G.P.; Hegarty, S.E.; Suescum-Diaz, M.A.; Cohen, A.W.; Berghella, V. Comparison of 2 stitches vs. 1 stitch for transvaginal cervical cerclage for preterm birth prevention. Am. J. Obstet. Gynecol. 2013, 208, 209.e1–209.e9. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.-M.; Zhang, J.; Hong, X.-L.; Liu, J.; Yang, Z.-Z.; Pan, M. Comparison of two stitches versus one stitch for emergency cervical cerclage to prevent preterm birth in singleton pregnancies. Int. J. Gynaecol. Obstet. 2023, 160, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Qiu, L.; Lv, M.; Chen, L.; Chen, Z.; Shen, J.; Wang, M.; Cai, Y.; Zhao, B.; Luo, Q. Comparison of two emergency cervical cerclage techniques in twin pregnancies: A retrospective cohort study matched with cervical dilation. Int. J. Gynaecol. Obstet. 2024, 167, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Donadono, V.; Koutikwar, P.; Banerjee, A.; Ivan, M.; Colley, C.S.; Sciacca, M.; Casagrandi, D.; Tetteh, A.; Greenwold, N.; Kindinger, L.M. Transvaginal cervical cerclage: Double monofilament modified Wurm vs. single braided McDonald technique. Ultrasound Obstet. Gynecol. 2025, 65, 344–352. [Google Scholar] [CrossRef]
- Xu, Z.M.; Zheng, Y.J.; Yan, W.X.; Jiang, C.H.; Li, H.; Zhang, J.; Pan, M. Two-stitch versus one-stitch cervical cerclage in women with cervical insufficiency: A stratified randomized controlled trial in China. SSRN 2025. preprint. [Google Scholar] [CrossRef]
- Hochuli, E.; Vogt, H.P. Die “Doppelcerclage”. Die Zervixinsuffizienz im mittleren Trimester und ihre Behandlung [Double cerclage. Cervix insufficiency in the middle trimester and its treatment]. Geburtshilfe Frauenheilkd 1987, 47, 537–538. (In German) [Google Scholar] [CrossRef] [PubMed]
- Park, J.M.; Tuuli, M.G.; Wong, M.; Carbone, J.F.; Ismail, M.; Macones, G.A.; Odibo, A.O. Cervical cerclage: One stitch or two? Am. J. Perinatol. 2012, 29, 477–481. [Google Scholar] [CrossRef]
- Damalie, F.J.M.K.; Nkini, A.N.; Nansubuga, S.; Ntege, R. Double cervical cerclage for cervical insufficiency: A case report. Afr. J. Reprod. Health 2024, 28, 117–125. [Google Scholar]
- Secher, N.J.; McCormack, C.D.; Weber, T.; Hein, M.; Helmig, R.B. Cervical occlusion in women with cervical insufficiency: Protocol for a randomised, controlled trial with cerclage, with and without cervical occlusion. BJOG 2007, 114, 649-e6. [Google Scholar] [CrossRef] [PubMed]
- Kosińska-Kaczyńska, K.; Rebizant, B.; Bednarek, K.; Dabrowski, F.; Kajdy, A.; Muzyka-Placzyńska, K.; Filipecka-Tyczka, D.; Uzar, P.; Kwiatkowski, S.; Torbe, A.; et al. Emergency cerclage using double-level versus single-level suture in the management of cervical insufficiency (Cervical Occlusion double-level Stitch Application, COSA): Study protocol for a multicentre, non-blinded, randomised controlled trial. BMJ Open 2023, 13, e071564. [Google Scholar] [CrossRef]
- Brix, N.; Secher, N.J.; McCormack, C.D.; Helmig, R.B.; Hein, M.; Weber, T.; Mittal, S.; Kurdi, W.; Palacio, M.; Henriksen, T.B.; et al. Randomised trial of cervical cerclage, with and without occlusion, for the prevention of preterm birth in women suspected for cervical insufficiency. BJOG 2013, 120, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Noori, M.; McCormack, C.D.; Weber, T.; Secher, N.J. Cervical occlusion in women with cervical insufficiency: A review. BJOG 2007, 114, 786–792. [Google Scholar] [CrossRef]
- Pergialiotis, V.; Papantoniou, N.; Antsaklis, A. Double versus single cervical cerclage for the prevention of preterm birth: A meta-analysis. J. Matern. Fetal Neonatal Med. 2015, 28, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Gnanarathne, S.; Rathnayake, C. Extending the pregnancy from pre-viable to viable: The place of emergency cerclage. Int. J. Gynaecol. Obstet. 2025. early view. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Smith, J.; Doe, K. Modified Wurm transvaginal cerclage to prevent preterm birth. BJOG 2020, 127, 145. [Google Scholar] [CrossRef]
- Park, Y.; Park, M. Second emergent double McDonald cerclage is useful in patients with amnionic membrane bulging into vagina after the first cervical cerclage. Ultrasound Obstet. Gynecol. 2023, 62, 222–223. [Google Scholar] [CrossRef]
- Namouz, S.; Porat, S.; Okun, N.; Windrim, R.; Farine, D. Emergency cerclage: Literature review. Obstet. Gynecol. Surv. 2013, 68, 379–388. [Google Scholar] [CrossRef]
- Becher, N.; Adams Waldorf, K.; Hein, M.; Uldbjerg, N. The cervical mucus plug: Structured review of the literature. Acta Obstet. Gynecol. Scand. 2009, 88, 502–513. [Google Scholar] [CrossRef]
- Baumgarten, K.; Moser, S. The technique of fibrin adhesion for premature rupture of the membranes during pregnancy. J. Perinat. Med. 1986, 14, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, A.; Watanabe, T. A modified Shirodkar procedure-double cervical cerclage with an auxiliary loop. Nihon Sanka Fujinka Gakkai Zasshi 1989, 41, 173–178. (In Japanese) [Google Scholar] [PubMed]
- Vaughan, M.; Emms, A.; Hodgetts Morton, V.; Morris, R.K.; Israfil-Bayli, F.; Pilarski, N. Optimal surgical technique at cervical cerclage to prevent pregnancy loss, a systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2025. epub ahead of print. [Google Scholar] [CrossRef]

| Study (Year) | Design | Indication | Intervention (N) | Primary Outcome | Main Result/ Conclusion | Quality Tool | Risk of Bias |
|---|---|---|---|---|---|---|---|
| Choi et al. (2003) [5] | Retrospective cohort | Reoperation after failed TVC | Double MTVC n = 28 vs. TAC n = 13 (N = 41) | Fetal salvage, GA at delivery | Fetal salvage: 85.7% (24/28) vs. 100% (13/13), NS; less invasive than TAC. | NOS | 6/9 (moderate) |
| Lee et al. (2004) [6] | Retrospective cohort | HI/UI | Double MTVC n = 44 vs. Single TVC n = 94 (N = 138) | PTB < 34 wk, GA | ≥34 wk: 90.9% (40/44) vs. 74.0% (70/94), p < 0.05; pregnancy prolongation 21.5 vs. 19.5 wk, p = 0.013 (favors double). | NOS | 8/9 (good) |
| Woensdregt et al. (2008) [7] | Retrospective cohort | HI/UI | Double n = 38 vs. Single n = 112 (N = 150) | GA at delivery; PTB < 37, <34, <28 weeks | Median GA 38.3 vs. 38.0 wk, NS; PTB < 34 wk: 18.4% (7/38) vs. 16.8% (19/112), NS; PTB < 28 wk: 2.6% (1/38) vs. 9.4% (10/112), NS → no measurable benefit of double. | NOS | 6/9 (moderate) |
| Tsai et al. (2009) [8] | Randomized trial | HI: ≥1 prior 2nd-trimester loss | Double n = 17 vs. Single n = 34 (N = 51) | GA at delivery, PTB < 28/<34 wk, birthweight | GA 35.9 vs. 32.9 wk (p = 0.045); PTB < 28 wk 5.9% (1/17) vs. 29.4% (10/34), NS; PTB < 34 wk 23.5% (4/17) vs. 38.2% (13/34), NS; higher birthweight and better Apgar with double; neonatal survival similar. | RoB 2.0 | Low risk |
| Broumand et al. (2011) [9] | Randomized trial | HI/UI with CL < 25 mm | Double (TVC + cervical occlusion) n = 28 vs. Single (TVC only) n = 28 (N = 56) | PTB < 33 wk | PTB < 3 3 wk: 0% (0/28) vs. 18% (5/28), p < 0.05; GA 37.4 vs. 36.2 wk, NS; higher 5-min Apgar and better neonatal outcomes with double. | RoB 2.0 | Low risk |
| Park JM et al. (2012) [10] | Retrospective cohort | HI/UI/ECC mixed | Double n = 63 vs. Single n = 83 (N = 146) | PTB < 35 wk, GA at delivery | PTB < 35 wk: 30/63 (47.6%) vs. 34/83 (41.0%), p = 0.63; higher cerclage height with two stitches (20 vs. 17 mm) without outcome benefit. | NOS | 7/9 (good) |
| Giraldo-Isaza et al. (2013) [11] | Retrospective cohort | HI/UI | HI: Double 86 vs. Single 151 (N = 237) UI: Double 117 vs. Single 90 (N = 207) | PTB < 37 wk (both HI & UI) | HI: PTB < 37 wk 35% (30/86) vs. 39% (59/151), NS; no differences at <35–<24 wk UI: PTB < 37 wk 44% (51/117) vs. 49% (44/90), NS; fewer very early PTB < 28 wk (11% vs. 24%) and <24 wk (5% vs. 14%) with double, but underpowered. | NOS | 7/9 (good) |
| Zolghadri et al. (2014) [10] | Randomized trial | HI + recurrent mid-trimester loss | Double n = 19 vs. Single n = 14 (N = 33) | GA at delivery; PTB < 34 weeks | PTB < 34 wk: 10.5% (2/19) vs. 35.7% (5/14), p = 0.106; GA 37.2 ± 2.6 vs. 34.3 ± 3.8 wk (p = 0.016) → later delivery with double; other outcomes similar. | RoB 2.0 | Low risk |
| Xu Z-M et al. (2023) [12] | Retrospective cohort | ECC (singletons) | Double n = 13 vs. Single n = 13 (N = 26) | GA at delivery; PTB < 34/<32 weeks | GA 32.7 ± 5.5 vs. 28.0 ± 4.7 wk (p = 0.028); PTB < 32 wk: 38.5% (5/13) vs. 92.3% (12/13), p = 0.013; PTB < 34 wk: 46.2% (6/13) vs. 92.3% (12/13), p = 0.034 → double associated with later GA and lower early PTB; NICU admission and LOS significantly lower with double. | NOS | 7/9 (good) |
| Qiu et al. (2024) [13] | Retrospective matched cohort | ECC (twins) | Double n = 42 vs. Single n = 42 (N = 84) | GA at delivery; latency; spontaneous PTB < 28/<30/<32/<34 wk | GA 30.5 vs. 27.0 wk (p < 0.001); Pregnancy latency 56 vs. 28 days (p < 0.001); Spontaneous PTB < 28 wk 16.7% vs. 57.1% (p = 0.001); PTB < 30 wk 38.1% vs. 76.8% (p = 0.001); Higher birthweight (1544 vs. 980 g, p < 0.001); Perinatal mortality 7.1% vs. 31% (p = 0.014). | NOS | 7/9 (good) |
| Donadono et al. (2025) [14] | Prospective multicenter cohort | HI/UI, CL ≤ 25 mm | Double (modified Wurm) n = 112 vs. Single n = 118 (N = 230) | PTB < 32 weeks (overall and CL ≤ 25 mm subgroup) | Overall: PTB < 32 wk 13% (7/55) vs. 24% (22/92), p = 0.169, NS; CL ≤ 25 mm subgroup: PTB < 32 wk 9% (3/35) vs. 29% (14/48), p = 0.042 → significant benefit with modified Wurm double cerclage in markedly short cervix. | NOS | 9/9 (excellent) |
| Xu ZM et al. (2025) [15] | Stratified randomized trial | UI/ECC | UI: Double 23 vs. Single 25 (N = 48) ECC: Double 25 vs. Single 25 (N = 50) | PTB < 34 wk (primary); PTB < 28 wk (ECC subgroup) | UI: PTB < 34 wk 8.7% (2/23) vs. 0% (0/25), p = 0.224 → no clear difference; ECC: PTB < 34 wk NS, but PTB < 28 wk reduced with double (12% vs. 40%, p = 0.024). | RoB 2.0 | Low risk |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, Y.-J.; Park, M.-I. Double Versus Single Cervical Cerclage in Women with Cervical Insufficiency: A Systematic Review of Prophylactic and Emergency Indications. Reprod. Med. 2025, 6, 41. https://doi.org/10.3390/reprodmed6040041
Park Y-J, Park M-I. Double Versus Single Cervical Cerclage in Women with Cervical Insufficiency: A Systematic Review of Prophylactic and Emergency Indications. Reproductive Medicine. 2025; 6(4):41. https://doi.org/10.3390/reprodmed6040041
Chicago/Turabian StylePark, Yong-Jin, and Moon-Il Park. 2025. "Double Versus Single Cervical Cerclage in Women with Cervical Insufficiency: A Systematic Review of Prophylactic and Emergency Indications" Reproductive Medicine 6, no. 4: 41. https://doi.org/10.3390/reprodmed6040041
APA StylePark, Y.-J., & Park, M.-I. (2025). Double Versus Single Cervical Cerclage in Women with Cervical Insufficiency: A Systematic Review of Prophylactic and Emergency Indications. Reproductive Medicine, 6(4), 41. https://doi.org/10.3390/reprodmed6040041







