Self-Reported Use and Effectiveness of Marijuana for Pelvic Pain Among Women with Endometriosis
Abstract
1. Introduction
2. Materials and Methods
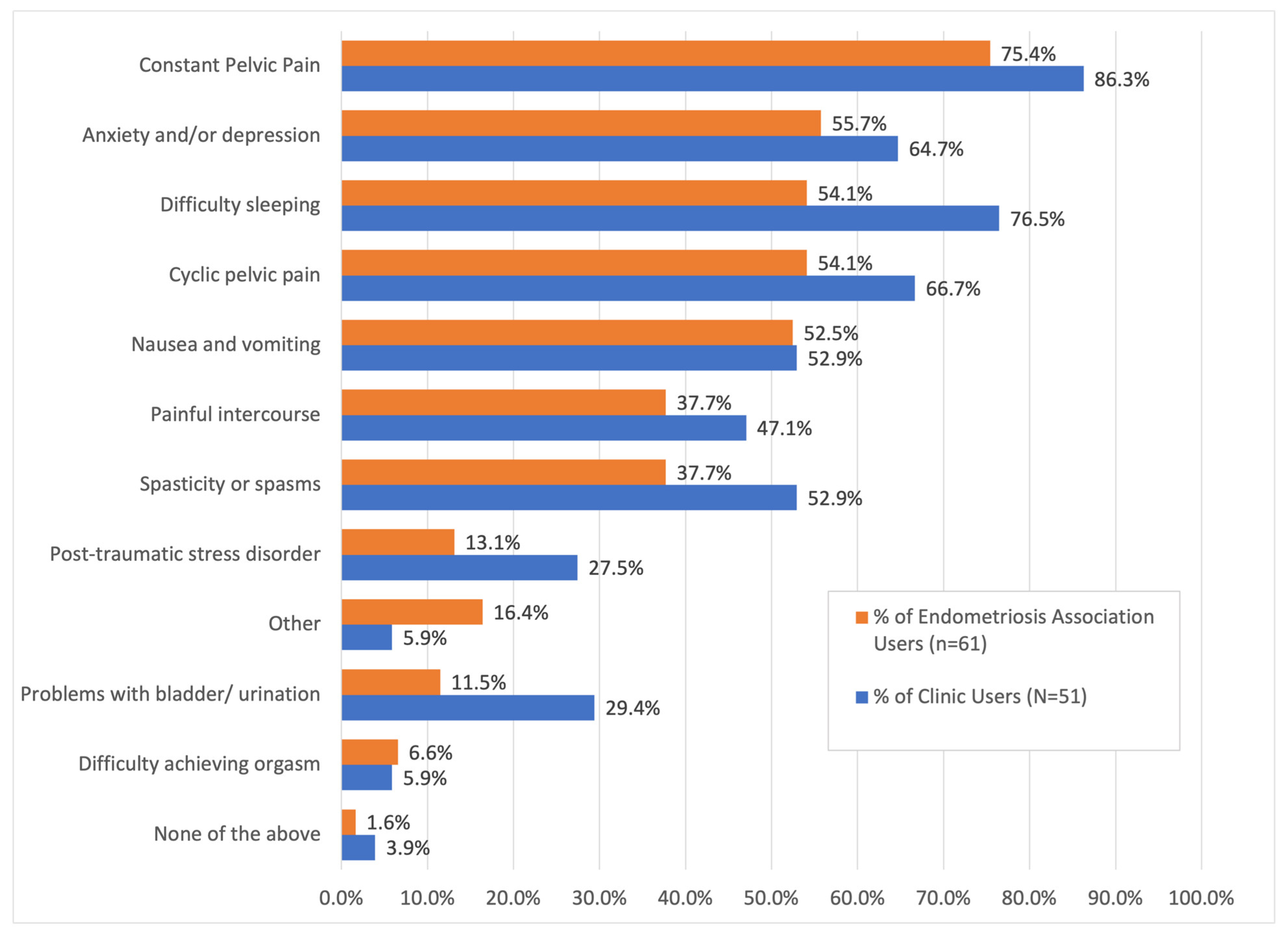
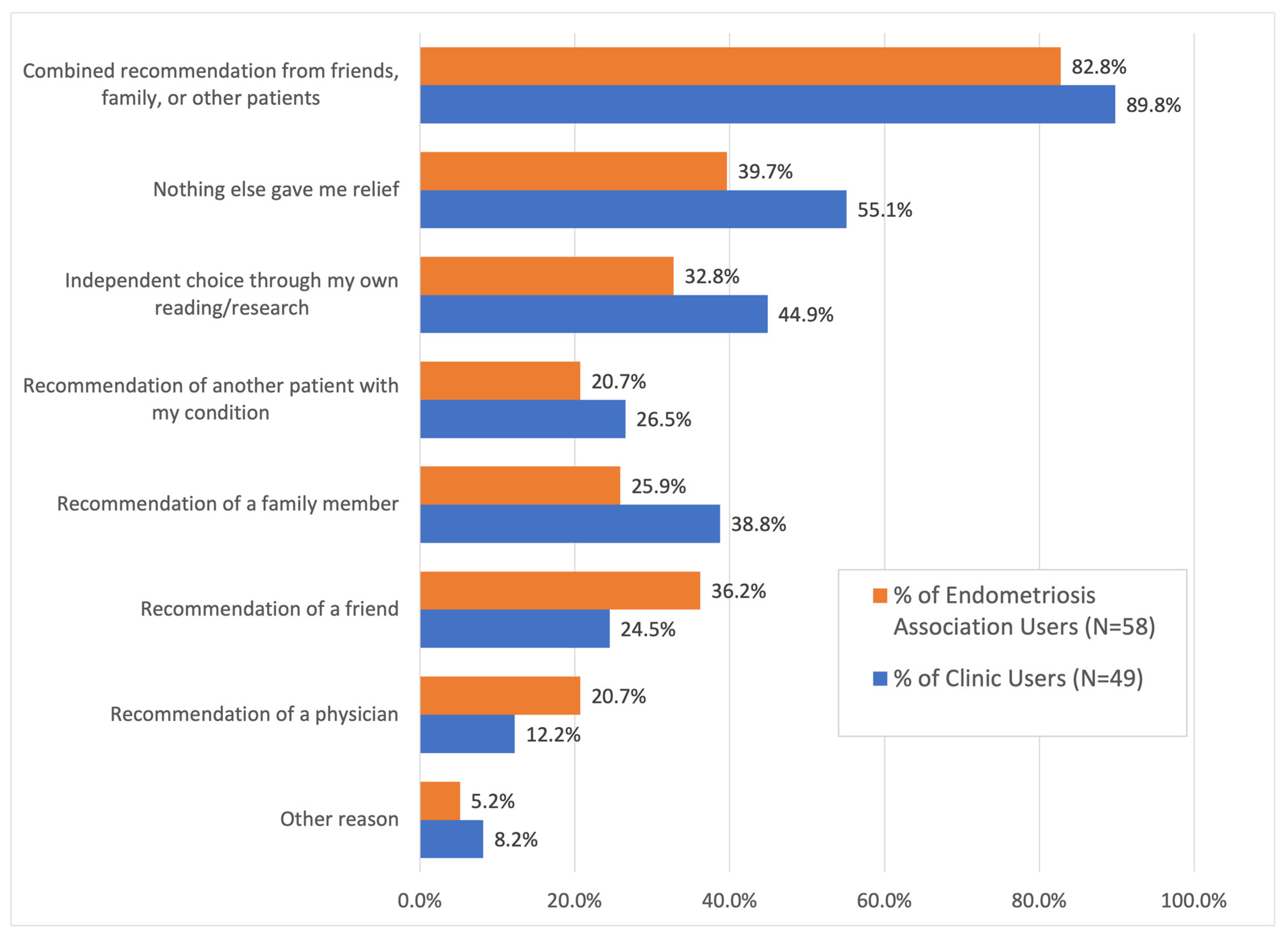
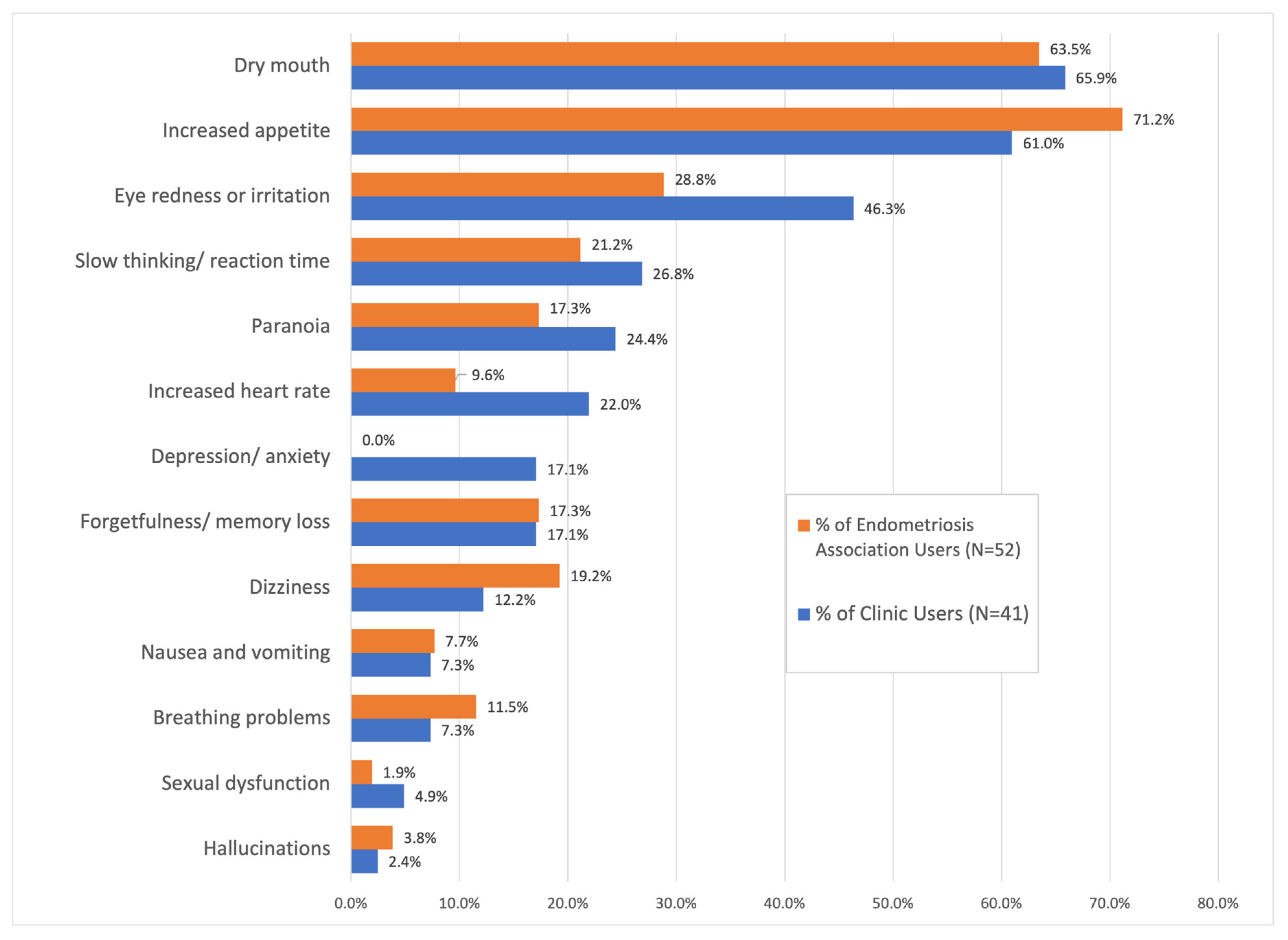
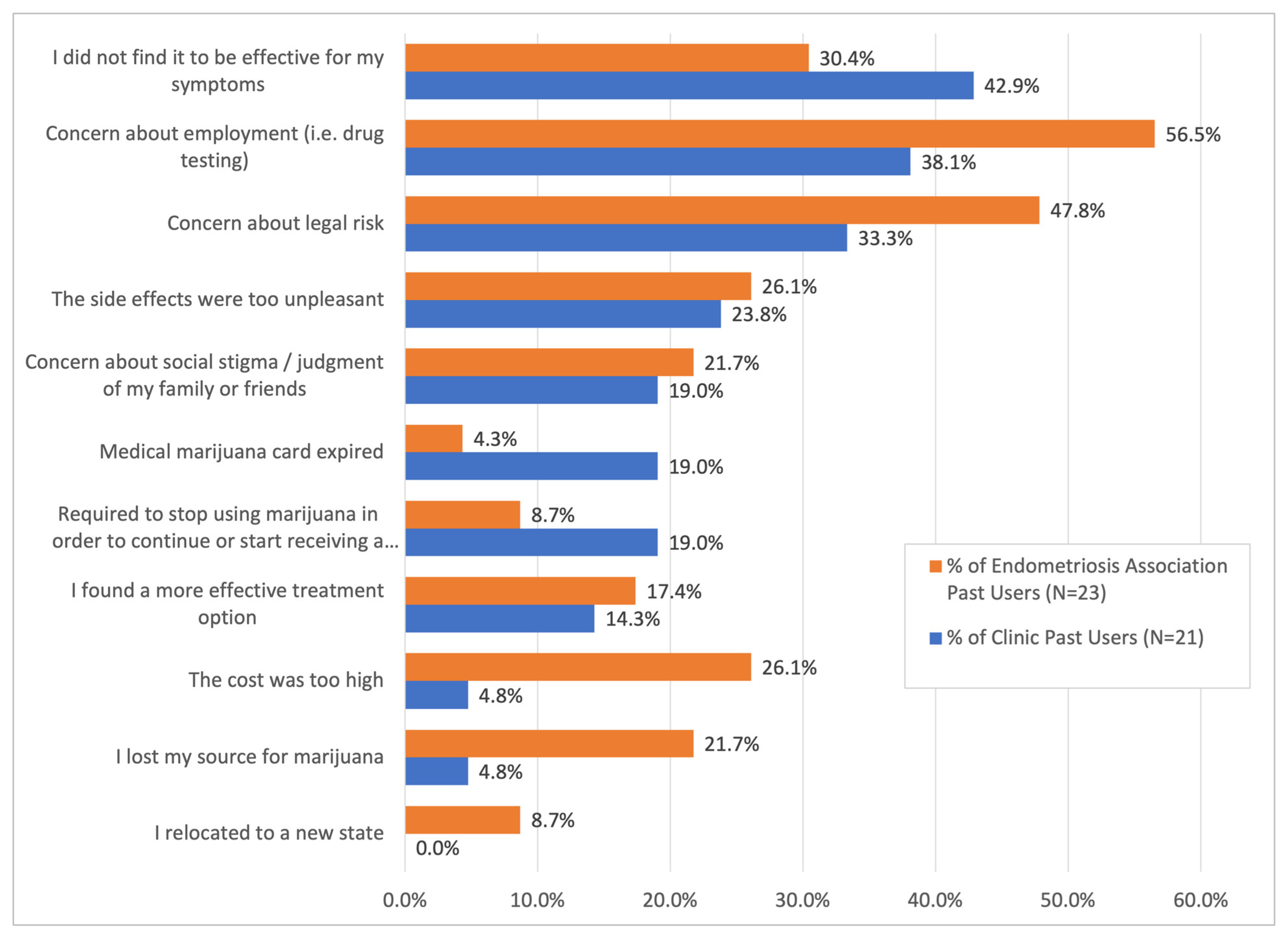
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ASRM. Treatment of pelvic pain associated with endometriosis: A committee opinion. Fertil. Steril. 2014, 101, 927–935. [Google Scholar] [CrossRef]
- Evans, S.; Villegas, V.; Dowding, C.; Druitt, M.; O’Hara, R.; Mikocka-Walus, A. Treatment use and satisfaction in Australian women with endometriosis: A mixed-methods study. Intern. Med. J. 2022, 52, 2096–2106. [Google Scholar] [CrossRef]
- Armour, M.; Sinclair, J.; Chalmers, K.J.; Smith, C.A. Self-management strategies amongst Australian women with endometriosis: A national online survey. BMC Complement. Altern. Med. 2019, 19, 17. [Google Scholar] [CrossRef]
- Resuehr, D.; Glore, D.R.; Taylor, H.S.; Bruner-Tran, K.L.; Osteen, K.G. Progesterone-dependent regulation of endometrial cannabinoid receptor type 1 (CB1-R) expression is disrupted in women with endometriosis and in isolated stromal cells exposed to 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD). Fertil. Steril. 2012, 98, 948–956.e1. [Google Scholar] [CrossRef] [PubMed]
- Leconte, M.; Nicco, C.; Ngô, C.; Arkwright, S.; Chéreau, C.; Guibourdenche, J.; Weill, B.; Chapron, C.; Dousset, B.; Batteux, F. Antiproliferative effects of cannabinoid agonists on deep infiltrating endometriosis. Am. J. Pathol. 2010, 177, 2963–2970. [Google Scholar] [CrossRef] [PubMed]
- Escudero-Lara, A.; Argerich, J.; Cabañero, D.; Maldonado, R. Disease-modifying effects of natural Δ9-tetrahydrocannabinol in endometriosis-associated pain. eLife 2020, 9, e50356. [Google Scholar] [CrossRef] [PubMed]
- Dmitrieva, N.; Nagabukuro, H.; Resuehr, D.; Zhang, G.; McAllister, S.L.; McGinty, K.A.; Mackie, K.; Berkley, K.J. Endocannabinoid involvement in endometriosis. Pain 2010, 151, 703–710. [Google Scholar] [CrossRef]
- Bouaziz, J.; Bar On, A.; Seidman, D.S.; Soriano, D. The Clinical Significance of Endocannabinoids in Endometriosis Pain Management. Cannabis Cannabinoid Res. 2017, 2, 72–80. [Google Scholar] [CrossRef]
- Sanchez, A.M.; Vigano, P.; Mugione, A.; Panina-bordignon, P.; Candiani, M. The molecular connections between the cannabinoid system and endometriosis. Mol. Hum. Reprod. 2012, 18, 563–571. [Google Scholar] [CrossRef]
- Lingegowda, H.; Williams, B.J.; Spiess, K.G.; Sisnett, D.J.; Lomax, A.E.; Koti, M.; Tayade, C. Role of the endocannabinoid system in the pathophysiology of endometriosis and therapeutic implications. J. Cannabis Res. 2022, 4, 54. [Google Scholar] [CrossRef]
- Sinclair, J.; Smith, C.A.; Abbott, J.; Chalmers, K.J.; Pate, D.W.; Armour, M. Cannabis Use, a Self-Management Strategy Among Australian Women with Endometriosis: Results from a National Online Survey. J. Obstet. Gynaecol. Can. 2020, 42, 256–261. [Google Scholar] [CrossRef]
- Sinclair, J.; Collett, L.; Abbott, J.; Pate, D.W.; Sarris, J.; Armour, M. Effects of cannabis ingestion on endometriosis-associated pelvic pain and related symptoms. PLoS ONE 2021, 16, e0258940. [Google Scholar] [CrossRef]
- Carrubba, A.R.; Ebbert, J.O.; Spaulding, A.C.; Destephano, D.; Destephano, C.C. Use of Cannabis for Self-Management of Chronic Pelvic Pain. J. Women’s Health 2021, 30, 1344–1351. [Google Scholar] [CrossRef]
- Mistry, M.; Simpson, P.; Morris, E.; Fritz, A.-K.; Karavadra, B.; Lennox, C.; Prosser-Snelling, E. Cannabidiol for the Management of Endometriosis and Chronic Pelvic Pain. J. Minim. Invasive Gynecol. 2022, 29, 169–176. [Google Scholar] [CrossRef]
- Liang, A.L.; Gingher, E.L.; Coleman, J.S. Medical Cannabis for Gynecologic Pain Conditions: A Systematic Review. Obstet. Gynecol. 2022, 139, 287–296. [Google Scholar] [CrossRef]
- Eichorn, N.L.; Shult, H.T.; Kracht, K.D.; Berlau, D.J. Making a joint decision: Cannabis as a potential substitute for opioids in obstetrics and gynecology. Best Pract. Res. Clin. Obstet. Gynaecol. 2022, 85 Pt B, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z. Model building strategy for logistic regression: Purposeful selection. Ann. Transl. Med. 2016, 4, 111. [Google Scholar] [CrossRef] [PubMed]
- Armour, M.; Sinclair, J.; Cheng, J.; Davis, P.; Hameed, A.; Meegahapola, H.; Rajashekar, K.; Suresh, S.; Proudfoot, A.; Leonardi, M. Endometriosis and Cannabis Consumption During the COVID-19 Pandemic: An International Cross-Sectional Survey. Cannabis Cannabinoid Res. 2022, 7, 473–481. [Google Scholar] [CrossRef]
- Jasinski, V.; Voltolini Velho, R.; Sehouli, J.; Mechsner, S. Cannabis use in endometriosis: The patients have their say—An online survey for German-speaking countries. Arch. Gynecol. Obstet. 2024, 310, 2673–2680. [Google Scholar] [CrossRef]
- Geoffrion, R.; Yang, E.C.; Koenig, N.A.; Brotto, L.A.; Barr, A.M.; Lee, T.; Allaire, C.; Bedaiwy, M.A.; Yong, P.J. Recreational Cannabis Use Before and After Legalization in Women with Pelvic Pain. Obstet. Gynecol. 2021, 137, 91–99. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. Clinical Consensus No. 7: The use of cannabis products for the management of pain associated with gynecologic conditions. Obstet. Gynecol. 2024, 144, e24–e34. [Google Scholar] [CrossRef]
- Robert, M.; Graves, L.E.; Allen, V.M.; Dama, S.; Gabrys, R.L.; Tanguay, R.L.; Turner, S.D.; Green, C.R.; Cook, J.L. Guideline No. 425a: Cannabis Use Throughout Women’s Lifespans—Part 1: Fertility, Contraception, Menopause, and Pelvic Pain. J. Obstet. Gynaecol. Can. 2022, 44, 407–419.e4. [Google Scholar] [CrossRef] [PubMed]

| Clinic Group Participants | EA Group Participants | Total Sample | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Marijuana Use: | Non-Users | Users | Total | Non-Users | Users | Total | Non-Users | Users | Total |
| N = 66 | N = 58 | N = 124 | N = 171 | N = 78 | N = 249 | N = 237 | N = 136 | N = 373 | |
| A. Demographic Characteristics of Participants | |||||||||
| Age (years) | 34.5 (8.9) | 31.4 (6.5) | 33.1 (8.1) | 49.3 (11.4) | 41.8 (10.5) | 46.9 (11.6) | 44.9 (12.7) | 37.5 (10.4) | 42.2 (12.4) |
| p-value 2 | 0.032 | <0.001 | <0.001 | ||||||
| Pain duration (years) | 11.7 (10.7) | 13.6 (9.3) | 12.6 (10.1) | 24.3 (12.94) | 21.1 (12.1) | 23.3 (12.8) | 20.7 (13.6) | 17.9 (11.6) | 19.7 (12.9) |
| p-value 2 | 0.287 | 0.066 | 0.046 | ||||||
| Income | |||||||||
| Less than $20,000 | 4 (6.1%) | 3 (5.2%) | 7 (5.6%) | 8 (4.7%) | 13 (16.7%) | 21 (8.4%) | 12 (5.1%) | 16 (11.8%) | 28 (7.5%) |
| $20,000–$34,999 | 7 (10.6%) | 7 (12.1%) | 14 (11.3%) | 11 (6.4%) | 11 (14.1%) | 22 (8.6%) | 18 (7.6%) | 18 (13.2%) | 36 (9.7%) |
| $35,000–$49,999 | 9 (13.6%) | 8 (13.8%) | 17 (13.7%) | 22 (12.9%) | 6 (7.7%) | 28 (11.2%) | 31 (13.1%) | 14 (10.3%) | 45 (12.1%) |
| $50,000–$74,999 | 18 (27.3%) | 11 (19.0%) | 29 (23.4%) | 19 (11.1%) | 14 (17.9%) | 33 (13.3%) | 37 (15.6%) | 25 (18.4%) | 62 (16.6%) |
| $75,000–$99,999 | 9 (13.6%) | 10 (17.2%) | 19 (15.3%) | 25 (14.6%) | 11 (14.1%) | 36 (14.5%) | 34 (14.3%) | 21 (15.4%) | 55 (14.7%) |
| $100,000 or more | 16 (24.2%) | 13 (22.4%) | 29 (23.4%) | 62 (36.3%) | 16 (20.5%) | 78 (31.3%) | 78 (32.9%) | 29 (21.3%) | 107 (28.7%) |
| p-value 2 | 0.944 | 0.002 | 0.024 | ||||||
| Employment | |||||||||
| Full-time | 43 (65.2%) | 35 (60.3%) | 78 (62.9%) | 79 (46.2%) | 28 (35.9%) | 107 (43.0%) | 122 (51.5%) | 63 (46.3%) | 185 (49.6%) |
| Part-time | 5 (7.6%) | 3 (5.2%) | 8 (6.5%) | 19 (11.1%) | 14 (17.9%) | 33 (13.3%) | 24 (10.1%) | 17 (12.5%) | 41 (11.0%) |
| Freelancer | 2 (3.0%) | 0 (0%) | 2 (1.6%) | 10 (5.8%) | 4 (5.1%) | 14 (5.6%) | 12 (5.1%) | 4 (2.9%) | 16 (4.3%) |
| Unemployed | 7 (10.8%) | 5 (9.6%) | 12 (10.3%) | 10 (6.5%) | 7 (9.6%) | 17 (7.5%) | 17 (7.7%) | 12 (9.6%) | 29 (7.8%) |
| Student | 2 (3.0%) | 4 (6.9%) | 6 (4.8%) | 3 (1.8%) | 1 (1.3%) | 4 (1.6%) | 5 (2.1%) | 5 (3.7%) | 10 (2.7%) |
| Retired | 2 (3.0%) | 0 (0%) | 2 (1.6%) | 23 (13.5%) | 3 (3.8%) | 26 (10.4%) | 25 (10.5) | 3 (2.2%) | 28 (7.5%) |
| Disabled | 4 (6.1%) | 5 (8.6%) | 9 (7.3%) | 11 (6.4%) | 16 (20.5%) | 27 (10.8%) | 15 (6.3%) | 21 (15.4%) | 36 (9.7%) |
| p-value 2 | 0.653 | 0.010 | 0.010 | ||||||
| Education | |||||||||
| High school or less | 6 (9.1%) | 11 (19.0%) | 17 (13.7%) | 11 (6.4%) | 4 (5.1%) | 15 (6.0%) | 17 (7.2%) | 15 (11.0%) | 32 (8.6%) |
| Some college | 11 (16.7%) | 18 (31.0%) | 29 (23.4%) | 26 (15.2%) | 17 (21.8%) | 43 (17.3%) | 37 (15.6%) | 35 (25.7%) | 72 (19.3%) |
| Associate degree | 9 (13.6%) | 4 (6.9%) | 13 (10.5%) | 12 (7.0%) | 14 (17.9%) | 26 (10.4%) | 21 (8.9%) | 18 (13.2%) | 39 (10.5%) |
| Bachelor’s degree | 25 (37.9%) | 14 (24.1%) | 39 (31.5%) | 56 (32.7%) | 24 (30.8%) | 80 (32.1%) | 81 (34.2%) | 38 (27.9%) | 119 (31.9%) |
| Masters, Prof, Doc | 14 (21.2%) | 5 (8.6%) | 19 (15.3%) | 50 (29.2%) | 14 (17.9%) | 64 (25.7%) | 64 (27.0%) | 19 (14.0%) | 83 (22.3%) |
| p-value 2 | 0.025 | 0.038 | 0.004 | ||||||
| Relationship Status | |||||||||
| Married/Dom par | 34 (51.5%) | 26 (44.8%) | 102 (82.3%) | 102 (59.6%) | 46 (59.0%) | 148 (59.4%) | 136 (57.4%) | 72 (52.9%) | 208 (55.8%) |
| Separated | 0 (0%) | 2 (3.4%) | 2 (1.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (1.5%) | 2 (0.5%) |
| Divorced | 5 (7.6%) | 3 (5.2%) | 8 (6.5%) | 22 (12.9%) | 12 (15.4%) | 34 (13.7%) | 27 (11.5%) | 15 (11.0%) | 42 (11.3%) |
| Widowed | 2 (3.0%) | 0 (0%) | 2 (1.6%) | 4 (2.3%) | 0 (0%) | 4 (1.6%) | 6 (2.5%) | 0 (0%) | 6 (1.6%) |
| Single | 23 (34.8%) | 21 (36.2%) | 44 (35.5%) | 26 (15.2%) | 14 (17.9%) | 40 (16.1%) | 49 (20.7%) | 35 (25.7%) | 84 (22.5%) |
| p-value 2 | 0.347 | 0.517 | 0.083 | ||||||
| Age of Children (years) | |||||||||
| All children ≥ 18 | 9 (13.6%) | 4 (6.9%) | 13 (10.5%) | 41 (24.0%) | 9 (11.5%) | 50 (20.1%) | 50 (21.1%) | 13 (9.6%) | 63 (16.9%) |
| Some children < 18 | 20 (30.3%) | 16 (27.6%) | 36 (29.0%) | 46 (26.9%) | 23 (29.5%) | 69 (27.7%) | 66 (27.8%) | 39 (28.7%) | 105 (28.2%) |
| No children | 36 (54.5%) | 32 (55.2%) | 68 (54.8%) | 67 (39.2%) | 40 (51.3%) | 107 (43.0%) | 103 (43.5%) | 72 (52.9%) | 175 (46.9%) |
| p-value 2 | 0.556 | 0.05 | 0.014 | ||||||
| Sexual Orientation | |||||||||
| Heterosexual | 59 (89.4%) | 43 (74.1%) | 102 (82.3%) | 147 (86.0%) | 59 (75.6%) | 206 (82.7%) | 206 (86.9%) | 102 (75%) | 308 (82.6%) |
| Homosexual | 0 (0%) | 1 (1.7%) | 1 (0.8%) | 3 (1.8%) | 2 (2.6%) | 5 (2.0%) | 3 (1.3%) | 3 (2.2%) | 6 (1.6%) |
| Bisexual | 3 (4.5%) | 7 (12.1%) | 10 (8.1%) | 2 (1.2%) | 7 (9.0%) | 9 (3.6%) | 5 (2.1%) | 14 (10.3%) | 19 (5.1%) |
| Pansexual | 0 (0%) | 1 (1.7%) | 1 (0.8%) | 0 (0%) | 3 (3.8%) | 3 (1.2%) | 0 (0%) | 4 (2.9%) | 4 (1.1%) |
| Other | 0 (0%) | 0 (0%) | 1 (0.8%) | 2 (1.2%) | 1 (1.3%) | 3 (1.2%) | 3 (1.3%) | 1 (0.7%) | 4 (1.1%) |
| p-value 2 | 0.191 | 0.003 | <0.001 | ||||||
| Race/Ethnicity | |||||||||
| White | 45 (68.2%) | 37 (63.8%) | 82 (66.1%) | 128 (74.9%) | 62 (79.5%) | 190 (76.3%) | 173 (73.0%) | 99 (72.8%) | 272 (72.9%) |
| Hispanic | 11 (16.7%) | 8 (13.8%) | 19 (15.3%) | 10 (5.8%) | 5 (6.4%) | 15 (6.0%) | 21 (8.9%) | 13 (9.6%) | 34 (9.1%) |
| Black | 3 (4.5%) | 5 (8.6%) | 8 (6.5%) | 10 (5.8%) | 3 (3.8%) | 13 (5.2%) | 13 (5.5%) | 8 (5.9%) | 21 (5.6%) |
| Native Am. | 1 (1.5%) | 1 (1.7%) | 2 (1.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.4%) | 1 (0.7%) | 2 (0.5%) |
| Hawaiian/Pac Isla | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1.3%) | 1 (0.4%) | 0 (0%) | 1 (0.7%) | 1 (0.3%) |
| Multi-racial | 3 (4.5%) | 1 (1.7%) | 4 (3.2%) | 4 (2.3%) | 1 (1.3%) | 5 (2.0%) | 7 (3.0%) | 2 (1.5%) | 9 (2.4%) |
| Other | 1 (1.5%) | 0 (0%) | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.4%) | 0 (0%) | 1 (0.3%) |
| p-value 2 | 0.770 | 0.563 | 0.766 | ||||||
| A. Marijuana and Other Substance Use among Participants. | |||||||||
| Has used marijuana for pain relief? | |||||||||
| No, never | - | - | 67 (54.0%) | - | - | 167 (67.1%) | - | - | 234 (62.7%) |
| Yes, in past | - | - | 26 (21.0%) | - | - | 28 (11.2%) | - | - | 54 (14.5%) |
| Yes, currently | - | - | 29 (23.4%) | - | - | 38 (15.3%) | - | - | 67 (18.0%) |
| Possession of medical marijuana card? | |||||||||
| Never | 65 (98.5%) | 26 (44.8%) | 91 (73.4%) | 155 (90.6%) | 57 (73.1%) | 212 (85.1%) | 220 (92.8%) | 83 (61.0%) | 303 (81.2%) |
| In the past | 1 (1.5%) | 11 (19.0%) | 12 (9.7%) | 2 (1.2%) | 7 (9.0%) | 9 (3.6%) | 3 (1.3%) | 18 (13.2%) | 21 (5.6%) |
| Yes, currently | 0 (0%) | 19 (32.8%) | 19 (15.3%) | 0 (0%) | 13 (16.7%) | 13 (5.2%) | 0 (0%) | 32 (23.5%) | 32 (8.6%) |
| Legal status of marijuana where participant lives | |||||||||
| Not legal | 4 (6.1%) | 1 (1.7%) | 5 (4.0%) | 35 (20.5%) | 13 (16.7%) | 48 (19.3%) | 39 (16.5%) | 14 (10.3%) | 53 (14.2%) |
| Medicinal legal | 53 (80.3%) | 53 (91.4%) | 106 (85.5%) | 52 (30.4%) | 28 (35.9%) | 80 (32.1%) | 105 (44.3%) | 81 (59.6%) | 186 (49.9%) |
| Recreational legal | 1 (1.5%) | 0 (0%) | 1 (0.8%) | 37 (21.6%) | 33 (42.3%) | 70 (28.1%) | 38 (16.0%) | 33 (24.3%) | 71 (19.0%) |
| Use of CBD alone 3 | 9 (13.6%) | 48 (82.8%) | 57 (46.0%) | 21 (12.3%) | 51 (65.4%) | 72 (28.9%) | 30 (12.7%) | 99 (72.8%) | 129 (34.6%) |
| p-value 2 | <0.001 | <0.001 | <0.001 | ||||||
| History of Tobacco Use | 18 (27.3%) | 28 (48.3%) | 46 (37.1%) | 40 (23.4%) | 35 (44.9%) | 75 (30.1%) | 58 (24.5%) | 63 (46.3%) | 121 (32.4%) |
| p-value 2 | 0.034 | 0.001 | <0.001 | ||||||
| Recreational Drug Use | 7 (10.6%) | 20 (34.5%) | 27 (21.8%) | 23 (13.5%) | 40 (51.2%) | 63 (25.3%) | 30 (12.7%) | 60 (44.1%) | 90 (24.1%) |
| p-value 2 | <0.001 | <0.001 | |||||||
| Alcohol Use | 58 (87.9%) | 49 (84.5%) | 107 (86.3%) | 137 (80.1%) | 66 (84.6%) | 203 (81.5%) | 195 (82.3%) | 115 (84.6%) | 310 (83.1%) |
| p-value 2 | 0.538 | 0.828 | 0.183 | ||||||
| A. Comorbidities of Participants. | |||||||||
| Allergies | 33 (50.0%) | 24 (41.4%) | 57 (46.0%) | 83 (48.5%) | 42 (53.8%) | 125 (50.2%) | 116 (48.9%) | 66 (48.5%) | 182 (48.8%) |
| p-value 2 | 0.337 | 0.437 | 0.938 | ||||||
| Arthritis | 10 (15.2%) | 5 (8.6%) | 15 (12.1%) | 48 (28.1%) | 21 (25.9%) | 69 (27.7%) | 58 (24.5%) | 26 (19.1%) | 84 (22.5%) |
| p-value 2 | 0.266 | 0.851 | 0.233 | ||||||
| Asthma | 10 (15.2%) | 12 (20.7%) | 22 (17.7%) | 27 (15.8%) | 12 (15.4%) | 39 (15.7%) | 37 (15.6%) | 24 (17.6%) | 61 (16.4%) |
| p-value 2 | 0.421 | 0.935 | 0.609 | ||||||
| Blood pressure | 4 (6.1%) | 2 (3.4%) | 6 (4.8%) | 30 (17.5%) | 13 (16.7%) | 43 (17.3%) | 34 (14.3%) | 15 (11.0%) | 49 (13.1%) |
| p-value 2 | 0.49 | 0.865 | 0.361 | ||||||
| Cancer | 1 (1.5%) | 0 (0%) | 1 (0.8%) | 12 (7.0%) | 2 (2.6%) | 14 (5.6%) | 13 (5.5%) | 2 (1.5%) | 15 (4.0%) |
| p-value 2 | 0.347 | 0.157 | 0.057 | ||||||
| Cholesterol | 1 (1.5%) | 2 (3.4%) | 3 (2.4%) | 38 (22.2%) | 6 (7.7%) | 44 (17.7%) | 39 (16.5%) | 8 (5.9%) | 47 (12.6%) |
| p-value 2 | 0.485 | 0.005 | 0.003 | ||||||
| Depression | 18 (27.3%) | 24 (41.4%) | 42 (33.9%) | 62 (36.3%) | 33 (42.3%) | 95 (38.2%) | 80 (33.8%) | 57 (41.9%) | 137 (36.7%) |
| p-value 2 | 0.098 | 0.362 | 0.116 | ||||||
| Diabetes | 1 (1.5%) | 0 (0%) | 1 (0.8%) | 7 (4.1%) | 4 (5.1%) | 11 (4.4%) | 8 (3.4%) | 4 (2.9%) | 12 (3.2%) |
| p-value 2 | 0.347 | 0.712 | 0.819 | ||||||
| Digestion Problems | 14 (21.2%) | 15 (25.9%) | 29 (23.4%) | 57 (33.3%) | 24 (30.8%) | 81 (32.5%) | 71 (30.0%) | 39 (28.7%) | 110 (29.5%) |
| p-value 2 | 0.542 | 0.689 | 0.794 | ||||||
| Eyesight | 5 (7.6%) | 8 (13.8%) | 13 (10.5%) | 18 (10.5%) | 9 (11.5%) | 27 (10.8%) | 23 (9.7%) | 17 (12.5%) | 40 (10.7%) |
| p-value 2 | 0.259 | 0.812 | 0.401 | ||||||
| Fibromyalgia | 8 (12.1%) | 5 (8.6%) | 13 (10.5%) | 21 (12.3%) | 15 (19.2%) | 36 (14.5%) | 29 (12.2%) | 20 (14.7%) | 49 (13.1%) |
| p-value 2 | 0.526 | 0.148 | 0.497 | ||||||
| Headaches | 29 (43.9%) | 26 (44.8%) | 55 (44.4%) | 60 (35.1%) | 33 (42.3%) | 93 (37.3%) | 89 (37.6%) | 59 (43.4%) | 148 (39.7%) |
| p-value 2 | 0.921 | 0.275 | 0.268 | ||||||
| Hearing | 0 (0%) | 2 (3.4%) | 2 (1.6%) | 11 (6.4%) | 1 (1.3%) | 12 (4.8%) | 11 (4.6%) | 3 (2.2%) | 14 (3.8%) |
| p-value 2 | 0.128 | 0.078 | 0.234 | ||||||
| Heart disease | 0 (0%) | 0 (0%) | 0 (0%) | 7 (4.1%) | 4 (5.1%) | 11 (4.4%) | 7 (3.0%) | 4 (2.9%) | 11 (2.9%) |
| p-value 2 | NA | 0.712 | 0.995 | ||||||
| Infectious disease | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| p-value 2 | NA | NA | NA | ||||||
| Obesity | 8 (12.1%) | 2 (3.4%) | 10 (8.1%) | 22 (12.9%) | 12 (15.4%) | 34 (13.7%) | 30 (12.7%) | 14 (10.3%) | 44 (11.8%) |
| p-value 2 | 0.077 | 0.591 | 0.496 | ||||||
| Sexual problems | 8 (12.1%) | 7 (12.1%) | 15 (12.1%) | 27 (15.8%) | 9 (11.5%) | 36 (14.5%) | 35 (14.8%) | 16 (11.8%) | 51 (13.7%) |
| p-value 2 | 0.993 | 0.376 | 0.416 | ||||||
| Sleep problems | 13 (19.7%) | 20 (34.5%) | 33 (26.6%) | 46 (26.9%) | 31 (39.7%) | 77 (30.9%) | 59 (24.9%) | 51 (37.5%) | 110 (29.5%) |
| p-value 2 | 0.063 | 0.042 | 0.010 | ||||||
| Skin problems | 6 (9.1%) | 4 (6.9%) | 10 (8.1%) | 24 (14.0%) | 10 (12.8%) | 34 (13.7%) | 30 (12.7%) | 14 (10.3%) | 44 (11.8%) |
| p-value 2 | 0.654 | 0.796 | 0.496 | ||||||
| Substance abuse | 0 (0%) | 1 (1.7%) | 1 (0.8%) | 1 (0.6%) | 2 (2.6%) | 3 (1.2%) | 1 (0.4%) | 3 (2.2%) | 4 (1.1%) |
| p-value 2 | 0.284 | 0.184 | 0.107 | ||||||
| Thyroid | 12 (18.2%) | 6 (10.3%) | 18 (14.5%) | 28 (16.4%) | 10 (12.8%) | 38 (15.3%) | 40 (16.9%) | 16 (11.8%) | 56 (15.0%) |
| p-value 2 | 0.216 | 0.470 | 0.183 | ||||||
| Other | 11 (16.7%) | 6 (10.3%) | 17 (13.7%) | 23 (13.5%) | 18 (23.1%) | 41 (16.5%) | 34 (14.3%) | 24 (17.6%) | 58 (15.5%) |
| p-value 2 | 0.0304 | 0.057 | 0.397 | ||||||
| Clinic Group | EA Group | Total Sample | ||||
|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
| Age (years) 2 | 0.95 (0.90, 0.99) | 0.92 (0.84, 0.99) | 0.94 (0.91, 0.97) | 0.91 (0.86, 0.95) | 0.95 (0.93, 0.97) | 0.93 (0.90, 0.96) |
| Recreational drug use | 5.18 (1.98, 13.56) | 2.71 (0.74, 9.88) | 6.96 (3.67, 13.18) | 8.60 (3.41, 21.71) | 5.85 (3.47, 9.84) | 5.77 (2.90, 11.49) |
| Tobacco use | 3.05 (1.41, 6.58) | 3.28 (1.06, 10.16) | 2.67 (1.49, 4.79) | 0.95 (0.40, 2.26) | 2.86 (1.80, 4.53) | 1.50 (0.80, 2.81) |
| Sleep Problems | 2.15 (0.95, 4.84) | 4.53 (1.26, 16.29) | 1.79 (1.02, 3.16) | 3.46 (1.46, 8.23) | 1.81 (1.15, 2.85) | 2.65 (1.39, 5.04) |
| Legal status of Marijuana where participant lives 3 Not legal Medicinal legal Recreational legal | Ref 4.0 (0.43, 36.98) NA 4 | Ref 12.43 (0.70, 221) NA 4 | Ref 1.45 (0.66, 3.18) 2.40 (1.09, 5.30) | Ref 3.32 (1.15, 9.60) 7.76 (2.44, 24.63) | Ref 2.15 (1.09, 4.23) 2.42 (1.12, 5.22) | Ref 3.04 (1.29, 7.17) 7.13 (2.57, 19.81) |
| Education High school or less Some college Associate degree Bachelor’s degree Master’s, Prof, Doc | 3.27 (0.99, 10.77) 2.92 (1.08, 7.91) Ref 0.79 (0.21, 3.05) 0.64 (0.19, 2.15) | 6.07 (1.12, 32.87) 4.17 (1.12, 15.60) Ref 0.78 (0.12, 15.60) 1.14 (0.28, 4.67) | 0.85 (0.25, 2.93) 1.53 (0.70, 3.32) Ref 2.72 (1.10, 6.75) 0.65 (0.31, 1.40) | 0.82 (0.14, 4.98) 1.20 (0.36, 4.03) Ref 2.40 (0.69, 8.32) 1.05 (0.39, 2.82) | 1.88 (0.85, 4.16) 2.02 (1.11, 3.68) Ref 1.83 (0.87, 3.82) 0.63 (0.33, 1.20) | 3.07 (1.06, 8.88) 2.48 (1.10, 5.61) Ref 1.57 (0.60, 4.12) 1.13 (0.52, 2.46) |
| Employment Full-time Part-time Freelancer Unemployed Student Retired Disabled | Ref 0.74 (0.17, 3.30) NA 4 0.88 (0.26, 3.01) 2.46 (0.43, 14.21) NA 4 1.54 (0.38, 6.16) | Ref 0.68 (0.09, 4.98) NA 4 0.50 (0.07, 3.69) 0.93 (0.06, 14.32) NA 4 1.47 (0.23, 9.55) | Ref 2.08 (0.92, 4.69) 1.13 (0.33, 3.89) 1.98 (0.69, 5.69) 0.94 (0.09, 9.42) 0.37 (0.10, 1.32) 4.10 (1.70, 9.90) | Ref 6.03 (1.75, 20.73) 1.25 (0.27, 5.88) 2.34 (0.52, 10.52) 0.34 (0.03, 4.47) 2.75 (0.38, 19.91) 9.21 (2.34, 35.94) | Ref 1.37 (0,69, 2.74) 0.65 (0.20, 2.08) 1.37 (0.62, 3.04) 1.94 (0.54, 6.94) 0.23 (0.07, 0.80) 2.71 (1.31, 5.62) | Ref 2.11 (0.82, 5.43) 0.61 (0.15, 2.51) 0.71 (0.24, 2.09) 0.65 (0.13, 3.12) 0.81 (0.15, 4.43) 3.49 (1.27, 9.62) |
| Number (%) of with Feature or Mean (SD) Value of Feature | |||
|---|---|---|---|
| Variable | Clinic Group N = 58 | EA Group N = 78 | Total Sample N = 136 |
| Duration of marijuana use (years) | 4.9 (6.6) | 9.8 (13.2) | 7.6 (11.0) |
| p-value 1 | 0.023 | ||
| Marijuana use frequency | |||
| <once per month | 12 (20.7%) | 13 (16.7%) | 25 (18.4%) |
| Monthly | 5 (8.6%) | 5 (6.4%) | 10 (7.4%) |
| Weekly | 5 (8.6%) | 8 (10.3%) | 13 (9.6%) |
| Several times per week | 4 (6.9%) | 11 (14.1%) | 15 (11.0%) |
| Daily | 9 (15.5%) | 10 (12.8%) | 19 (14.0%) |
| Several times per day | 13 (22.4%) | 11 (14.1%) | 24 (17.6%) |
| p-value 1 | 0.581 | ||
| Effectiveness of marijuana use | |||
| Not effective | 5 (8.6%) | 9 (11.5%) | 14 (10.3%) |
| Slightly effective | 9 (15.5%) | 16 (20.5%) | 25 (18.4%) |
| Moderately effective | 13 (22.4%) | 22 (28.2%) | 35 (25.7%) |
| Very effective | 31 (53.4%) | 31 (39.7%) | 62 (45.6%) |
| p-value 1 | 0.470 | ||
| Most effective route of marijuana | |||
| Smoke/inhale | 14 (24.1%) | 25 (32.1%) | 39 (28.7%) |
| Vaporize | 4 (6.9%) | 2 (2.6%) | 6 (4.4%) |
| Edibles | 15 (25.9%) | 21 (26.9%) | 36 (26.5%) |
| Prescription THC medications | 0 (0.0%) | 3 (3.8%) | 3 (2.2%) |
| Transdermal medications | 5 (8.6%) | 3 (3.8%) | 8 (5.9%) |
| Vaginal suppository | 1 (1.7%) | 1 (1.3%) | 2 (1.5%) |
| Vape pen | 5 (8.6%) | 3 (3.8%) | 8 (5.9%) |
| Other route | 4 (6.9%) | 0 (0.0%) | 4 (2.9%) |
| p-value 1 | 0.103 | ||
| Marijuana use in pregnancy | |||
| No use in pregnancy | 45 (77.6%) | 53 (67.9%) | 98 (72.1%) |
| Use in early pregnancy + stopped upon discovering pregnancy | 3 (5.2%) | 3 (3.8%) | 6 (4.4%) |
| Continued use throughout pregnancy | 1 (1.7%) | 3 (3.8%) | 4 (2.9%) |
| p-value 1 | 0.693 | ||
| Legal status of marijuana in state | |||
| Neither recreational nor medicinal | 1 (1.9%) | 13 (17.6%) | 14 (10.3%) |
| Medicinal is legal, recreational is not | 53 (98.1%) | 28 (37.8%) | 81 (59.6%) |
| Currently has a physician-issued medical marijuana card | 19 (35.8%) | 5 (17.9%) | 24 (29.7%) |
| Had physician-issued card in the past but no longer | 10 (18.9%) | 1 (3.5%) | 11 (13.6%) |
| Never had physician-issued card | 24 (45.3%) | 22 (78.6%) | 46 (56.8%) |
| p-value 1 | 0.005 | ||
| Recreation and medicinal are legal | 0 (0.0%) | 33 (34.6%) | 33 (24.3%) |
| Currently has a physician-issued medical marijuana card | 0 | 8 (24.2%) | 8 (24.2%) |
| Had physician-issued card in the past but no longer | 0 | 5 (15.2%) | 5 (15.2%) |
| Never had physician-issued card | 0 | 20 (60.6%) | 20 (60.6%) |
| p-value 1 | NA | ||
| Legal marijuana use among current users only | Clinic Group | EA Group | Total Sample |
| N = 29 | N = 38 | N = 67 | |
| Neither recreational nor medicinal is legal in state | 0 (0%) | 6 (16.7%) | 6 (8.9%) |
| Medicinal use is legal, recreational is not in state | 29 (100%) | 15 (38.9%) | 44 (65.7%) |
| Currently has a physician-issued medical marijuana card | 19 (65.5%) | 4 (28.6%) | 23 (52.3%) |
| Had physician-issued card in the past but no longer | 3 (10.3%) | 0 (0%) | 3 (6.8%) |
| Never had physician-issued card | 7 (24.1%) | 11 (78.6%) | 18 (40.9%) |
| Recreation and medicinal are legal in state | 0 (0.0%) | 17 (44.4%) | 17 (25.4%) |
| Currently has a physician-issued medical marijuana card | 0 | 7 (41.2%) | 7 (41.2%) |
| Had physician-issued card in the past but no longer | 0 | 3 (17.6%) | 3 (17.6%) |
| Never had physician-issued card | 0 | 7 (41.2%) | 7 (41.2%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reinert, A.E.; Bolshakova, M.; Wong, A.S.; Cortessis, V.K. Self-Reported Use and Effectiveness of Marijuana for Pelvic Pain Among Women with Endometriosis. Reprod. Med. 2025, 6, 23. https://doi.org/10.3390/reprodmed6030023
Reinert AE, Bolshakova M, Wong AS, Cortessis VK. Self-Reported Use and Effectiveness of Marijuana for Pelvic Pain Among Women with Endometriosis. Reproductive Medicine. 2025; 6(3):23. https://doi.org/10.3390/reprodmed6030023
Chicago/Turabian StyleReinert, Anna E., Maria Bolshakova, Alexander S. Wong, and Victoria K. Cortessis. 2025. "Self-Reported Use and Effectiveness of Marijuana for Pelvic Pain Among Women with Endometriosis" Reproductive Medicine 6, no. 3: 23. https://doi.org/10.3390/reprodmed6030023
APA StyleReinert, A. E., Bolshakova, M., Wong, A. S., & Cortessis, V. K. (2025). Self-Reported Use and Effectiveness of Marijuana for Pelvic Pain Among Women with Endometriosis. Reproductive Medicine, 6(3), 23. https://doi.org/10.3390/reprodmed6030023






