Exploring Pregnancy-Related Acute Kidney Injury: Risk Factors and Maternal Outcomes in High-Risk Women in Mwanza, Tanzania
Abstract
1. Introduction
2. Methods and Materials
2.1. Study Design, Sample Size, and Study Area
2.2. Study Population
2.3. Inclusion Criteria
2.4. Statistical Methods
3. Results
3.1. Social Demographic Characteristics of Patients
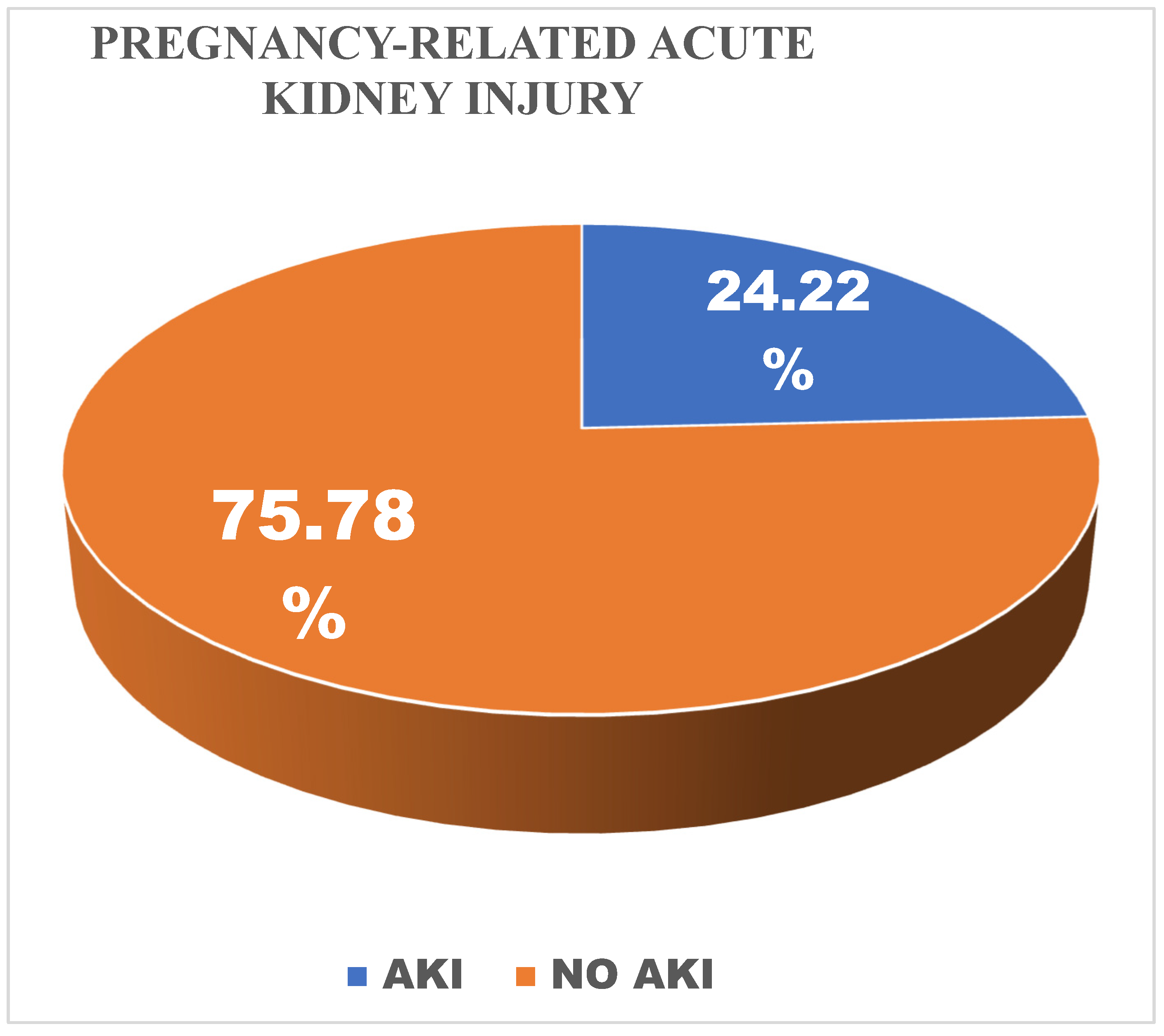
3.2. Distribution of PRAKI and Stages Among Women Who Developed Acute Kidney Injury
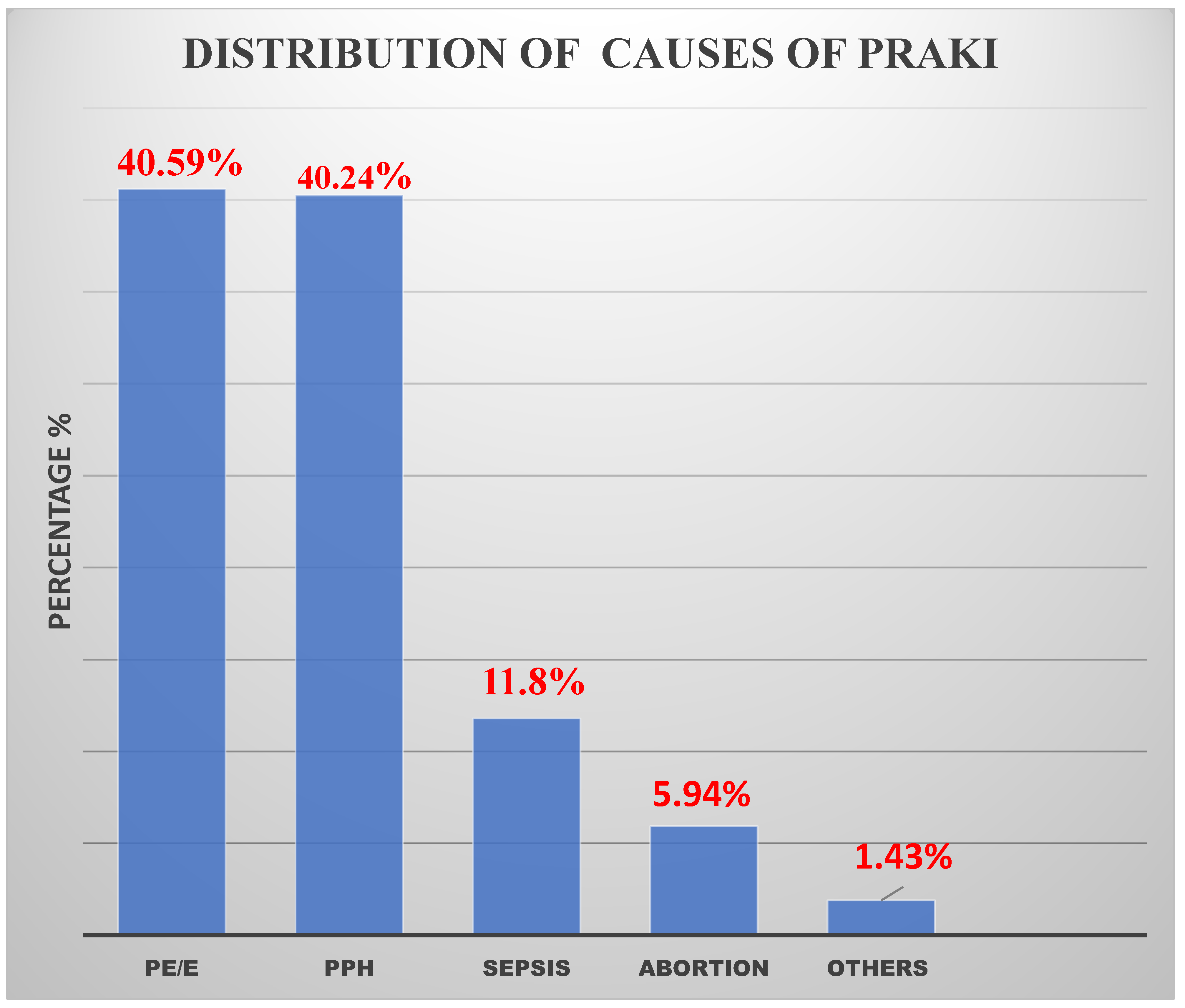
3.3. Distribution of Causes of Pregnancy-Related Acute Kidney Injury
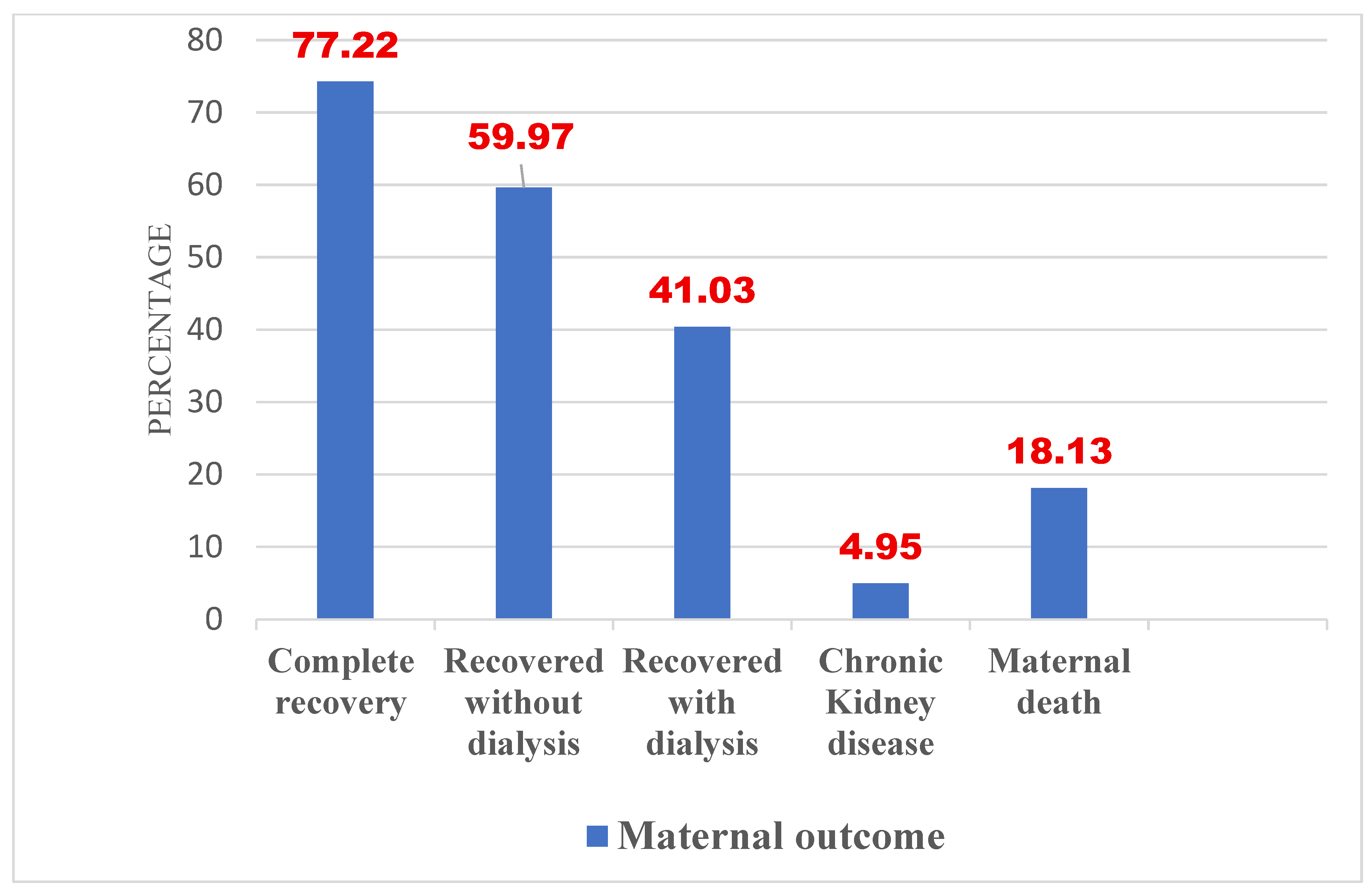
3.4. Maternal Outcomes of Patients Who Developed PRAKI
3.5. Factors Associated with the Development of Acute Kidney Injury Among High-Risk Women
4. Discussion
4.1. Conclusions and Implications
4.2. Study Strengths and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AKI | Acute kidney injury |
| BMC | Bugando Medical Centre |
| CKD | Chronic Kidney Disease |
| HELLP | Hemolysis, Elevated Liver enzymes, and Low Platelets |
| ICU | Intensive Care Unit |
| PPH | Postpartum hemorrhage |
| PRAKI | Pregnancy-related acute kidney injury |
References
- Cerdá, J.; Bagga, A.; Kher, V.; Chakravarthi, R.M. The contrasting characteristics of acute kidney injury in developed and developing countries. Nat. Clin. Pract. Nephrol. 2008, 4, 138–153. [Google Scholar] [CrossRef] [PubMed]
- Gaber, T.Z.; Shemies, R.S.; Baiomy, A.A.; Aladle, D.A.; Mosbah, A.; Abdel-hady, E.S.; Sayed-Ahmed, N.; Sobh, M. Acute kidney injury during pregnancy and puerperium: An Egyptian hospital-based study. J. Nephrol. 2021, 34, 1611–1619. [Google Scholar] [CrossRef] [PubMed]
- Ruggajo, P.; Appollo, E.; Bramania, P.; Basil, T.; Furia, F.; Mngumi, J. Prevalence, Risk Factors and Short-term Outcomes of Acute Kidney Injury in Women with Obstetric Complications in Dar es Salaam, Tanzania. Tanzan. Med. J. 2022, 33, 14–29. [Google Scholar]
- Liu, D.; He, W.; Li, Y.; Xiong, M.; Wang, L.; Huang, J.; Jia, L.; Yuan, S.; Nie, S. Epidemiology of acute kidney injury in hospitalized pregnant women in China. BMC Nephrol. 2019, 20, 67. [Google Scholar] [CrossRef] [PubMed]
- Ndaboine, E.M.; Kihunrwa, A.; Rumanyika, R.; Im, H.B.; Massinde, A.N. Maternal and perinatal outcomes among eclamptic patients admitted to Bugando Medical Centre, Mwanza, Tanzania. Afr. J. Reprod. Health 2012, 16, 35–41. [Google Scholar] [PubMed]
- Prakash, J.; Ganiger, V. Acute kidney injury in pregnancy-specific disorders. Indian J. Nephrol. 2017, 27, 258–270. [Google Scholar] [CrossRef] [PubMed]
- Shalaby, A.S.; Shemies, R.S. Pregnancy-related acute kidney injury in the African continent: Where do we stand? A systematic review. J. Nephrol. 2022, 35, 2175–2189. [Google Scholar] [CrossRef] [PubMed]
- Hildebrand, A.M.; Liu, K.; Shariff, S.Z.; Ray, J.G.; Sontrop, J.M.; Clark, W.F.; Hladunewich, M.A.; Garg, A.X. Characteristics and outcomes of AKI treated with dialysis during pregnancy and the postpartum period. J. Am. Soc. Nephrol. 2015, 26, 3085–3091. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ma, X.; Zheng, J.; Liu, X.; Yan, T. Pregnancy outcomes in patients with acute kidney injury during pregnancy: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2017, 17, 235. [Google Scholar] [CrossRef] [PubMed]
- Prakash, J.; Kumar, H.; Sinha, D.; Kedalaya, P.; Pandey, L.; Srivastava, P.; Raja, R.; Usha. Acute renal failure in pregnancy in a developing country: Twenty years of experience. Ren. Fail. 2006, 28, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Njau, M.; Mujuni, F.; Matovelo, D.; Ndaboine, E.; Kiritta, R.; Rudovick, L. Acute Kidney Injury: Magnitude and Predictors of Maternal Outcomes among Pre-Eclamptic and Eclamptic Women in Mwanza, Tanzania. East Afr. Health Res. J. 2025, 8, 372. [Google Scholar]
- Shija, K.; Ibrahim, H.; Jumbe, S.; Lugoba, B.; Kibusi, S.M.; Chandika, A. Clinical Presentation and Treatment Outcomes of Pregnancy-Related Acute Kidney Injury among Pregnant Women Admitted at the Benjamin Mkapa Hospital in Tanzania. Open J. Nephrol. 2024, 14, 157–175. [Google Scholar] [CrossRef]
- Cooke, W.R.; Hemmilä, U.K.; Craik, A.L.; Mandula, C.J.; Mvula, P.; Msusa, A.; Dreyer, G.; Evans, R. Incidence, aetiology and outcomes of obstetric-related acute kidney injury in Malawi: A prospective observational study. BMC Nephrol. 2018, 19, 25. [Google Scholar] [CrossRef] [PubMed]
- Ismael, K.S.; Warda, O.; Elshamy, M.; Abdelhafez, M.S. Pregnancy Related Acute Kidney Injury: A Single Tertiary Care Center Experience. Evid. Based Women’s Health J. 2024, 14, 32–38. [Google Scholar] [CrossRef]
- Awowole, I.O.; Omitinde, O.S.; Arogundade, F.A.; Bola-Oyebamiji, S.B.; Adeniyi, O.A. Pregnancy-related acute kidney injury requiring dialysis as an indicator of severe adverse maternal morbidity at a tertiary center in Southwest Nigeria. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 225, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Guillén, A.O.; Shemies, R.S.; Ankawi, G.A.; Jesudason, S.; Piccoli, G.B. Women should not die of pregnancy-related acute kidney injury (PRAKI): Revealing the underwater iceberg of maternal health. J. Nephrol. 2024, 37, 543–546. [Google Scholar] [CrossRef] [PubMed]
- Waziri, B.; Umar, I.A.; Magaji, A.; Umelo, C.C.; Nalado, A.M.; Wester, C.W.; Aliyu, M.H. Risk factors and outcomes associated with pregnancy-related acute kidney injury in a high-risk cohort of women in Nigeria. J. Nephrol. 2024, 37, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Piccoli, G.B.; Chatrenet, A.; Cataldo, M.; Torreggiani, M.; Attini, R.; Masturzo, B.; Cabiddu, G.; Versino, E.; Kidney and Pregnancy Study Group of the Italian Society of Nephrology. Adding creatinine to routine pregnancy tests: A decision tree for calculating the cost of identifying patients with CKD in pregnancy. Nephrol. Dial. Transplant. 2023, 38, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Rage, H.I.; Jha, P.K.; Hashi, H.A.; Abdillahi, N.I. Pregnancy-Related AKI: A Tertiary Care Hospital Experience in Somaliland. Kidney Int. Rep. 2023, 8, 388. [Google Scholar] [CrossRef] [PubMed]
- Kumari, P.; Trivedi, K.; Banerjee, S.; Sharma, A.; Sinha, T.; Boipai, P.; Kumari, S. Study on Incidence of Pregnancy-related Acute Kidney Injury and Its Associated Risk Factors and Outcomes: In Preponderant Tribal State of India. Ann. Afr. Med. 2025, 24, 304–309. [Google Scholar] [CrossRef] [PubMed]

| Stage | Serum Creatinine | Urine Output |
|---|---|---|
| 1 | 1.5–1.9 times baseline OR ≥ 0.3 mg/dL (≥26.5 mmol/L) increase | <0.5 mL/kg/h for 6–12 h |
| 2 | 2.0–2.9 times baseline | <0.5 mL/kg/h for ≥12 h |
| 3 | 3.0 times baseline OR Increase in serum creatinine to ≥353.6 mmol/L) OR Initiation of renal replacement therapy OR, In patients <18 years, decrease in eGFR to <35 mL/min per 1.73 m | <0.3 mL/kg/h for ≥24 h OR Anuria for ≥12 h |
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Age category | ||
| 18–24 years | 103 | 24.50 |
| 25–34 years | 210 | 50.00 |
| ≥35 years | 107 | 25.50 |
| Referral status | ||
| Self-referral | 212 | 50.60 |
| Referral from other | 207 | 49.40 |
| Residence | ||
| Urban | 293 | 69.80 |
| Rural | 127 | 30.20 |
| Education | ||
| Informal education | 15 | 3.57 |
| Primary education | 163 | 38.80 |
| Secondary education | 175 | 41.67 |
| College education | 67 | 15.95 |
| Occupation | ||
| Employed | 68 | 16.19 |
| Unemployed | 52 | 12.38 |
| Farm worker | 146 | 34.76 |
| Entrepreneur | 154 | 36.67 |
| Marital status | ||
| Single | 23 | 5.48 |
| Married | 395 | 94.05 |
| Divorced | 2 | 0.48 |
| Parity | ||
| 0 | 17 | 4.05 |
| 1 | 137 | 32.62 |
| 2–4 | 189 | 45.00 |
| 5+ | 77 | 18.33 |
| Mode of delivery | ||
| Vaginal delivery | 181 | 43.1 |
| Caesarean section | 239 | 56.9 |
| Ward admitted | ||
| General | 236 | 56.19 |
| HDU | 149 | 35.48 |
| HDU then general | 5 | 1.19 |
| ICU | 30 | 7.14 |
| Aki status | ||
| No AKI | 316 | 75.2 |
| AKI | 104 | 24.8 |
| Pulse rate per minute | ||
| <100 | 325 | 77.4 |
| >100 | 95 | 22.6 |
| Temperature | ||
| <37.7 | 404 | 96.2 |
| >37.7 | 16 | 3.8 |
| Variable | Bivariate | Multivariate | ||
|---|---|---|---|---|
| COR [95% CI] | p-Value | AOR [95% CI] | p-Value | |
| Age group | ||||
| <25 | 1 | 1 | ||
| 25–34 | 0.56 (0.33–0.96) | 0.033 | 1.09 (0.55–2.17) | 0.794 |
| 35+ | 0.72 (0.39–1.31) | 0.276 | 0.896 (0.36–2.24) | 0.815 |
| Residence | ||||
| Rural | 1 | 1 | ||
| Urban | 0.19 (0.12–0.30) | <0.0001 | 0.34 (0.18–0.62) | 0.001 |
| Education | ||||
| Informal/Primary | 1 | 1 | ||
| Secondary | 0.26 (0.16–0.44) | <0.0001 | 0.67 (0.33–1.37) | 0.271 |
| College | 0.09 (0.03–0.26) | <0.0001 | 0.22 (0.05–0.98) | 0.048 |
| Occupation | ||||
| Employed | 1 | 1 | ||
| Entrepreneur | 1.30 (0.52–3.24) | 0.572 | 0.66 (0.20–2.16) | 0.488 |
| Farm worker | 6.99 (2.30–16.32) | <0.0001 | 0.87 (0.23–3.30) | 0.836 |
| Unemployed | 2.61 (0.95–7.21) | 0.063 | 0.81 (0.21–3.12) | 0.759 |
| Marital status | ||||
| Divorced | 1 | NA | ||
| Married | 0.41 (0.17–0.96) | 0.039 | 0.58 (0.21–1.61) | 0.294 |
| Single | NA | NA | ||
| Ward admitted | ||||
| General | 1 | 1 | ||
| HDU | 5.23 (3.08–8.88) | <0.0001 | 3.66 (2.04–6.56) | <0.0001 |
| HDU then general | 5.63 (0.90–35.31) | 0.065 | 2.86 (0.38–21.71) | 0.310 |
| ICU | 16.88 (7.11–40.09) | <0.0001 | 10.5 (4.07–27.12) | <0.0001 |
| Parity | ||||
| <5 | 1 | 1 | ||
| 5+ | 2.39 (1.41–4.06) | 0.001 | 1.60 (0.72–3.56) | 0.252 |
| Mode of delivery | ||||
| Caesarean section | 1 | |||
| Vaginal delivery | 0.69 (0.44–1.076) | 0.102 | 1.19 (0.69–2.06) | 0.533 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernard, K.; Mujuni, F.; Matovelo, D.; Ndaboine, E.; Kiritta, R.; Rudovick, L. Exploring Pregnancy-Related Acute Kidney Injury: Risk Factors and Maternal Outcomes in High-Risk Women in Mwanza, Tanzania. Reprod. Med. 2025, 6, 20. https://doi.org/10.3390/reprodmed6030020
Bernard K, Mujuni F, Matovelo D, Ndaboine E, Kiritta R, Rudovick L. Exploring Pregnancy-Related Acute Kidney Injury: Risk Factors and Maternal Outcomes in High-Risk Women in Mwanza, Tanzania. Reproductive Medicine. 2025; 6(3):20. https://doi.org/10.3390/reprodmed6030020
Chicago/Turabian StyleBernard, Kahibi, Fridolin Mujuni, Dismas Matovelo, Edgar Ndaboine, Richard Kiritta, and Ladius Rudovick. 2025. "Exploring Pregnancy-Related Acute Kidney Injury: Risk Factors and Maternal Outcomes in High-Risk Women in Mwanza, Tanzania" Reproductive Medicine 6, no. 3: 20. https://doi.org/10.3390/reprodmed6030020
APA StyleBernard, K., Mujuni, F., Matovelo, D., Ndaboine, E., Kiritta, R., & Rudovick, L. (2025). Exploring Pregnancy-Related Acute Kidney Injury: Risk Factors and Maternal Outcomes in High-Risk Women in Mwanza, Tanzania. Reproductive Medicine, 6(3), 20. https://doi.org/10.3390/reprodmed6030020






