Actinomyces in Pregnancy: A Rare and Silent Cause of Preterm Delivery—Case Report
Abstract
1. Introduction
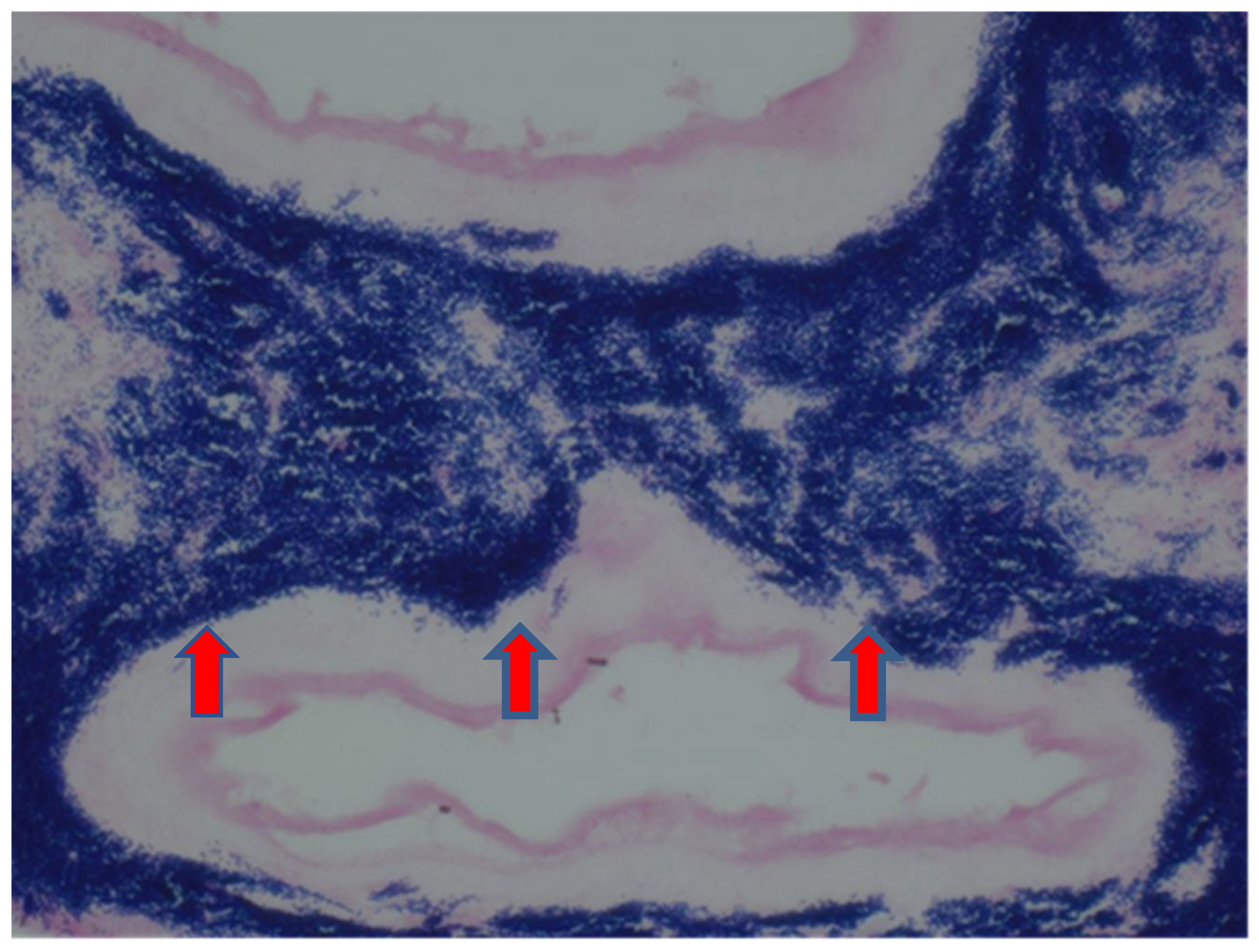
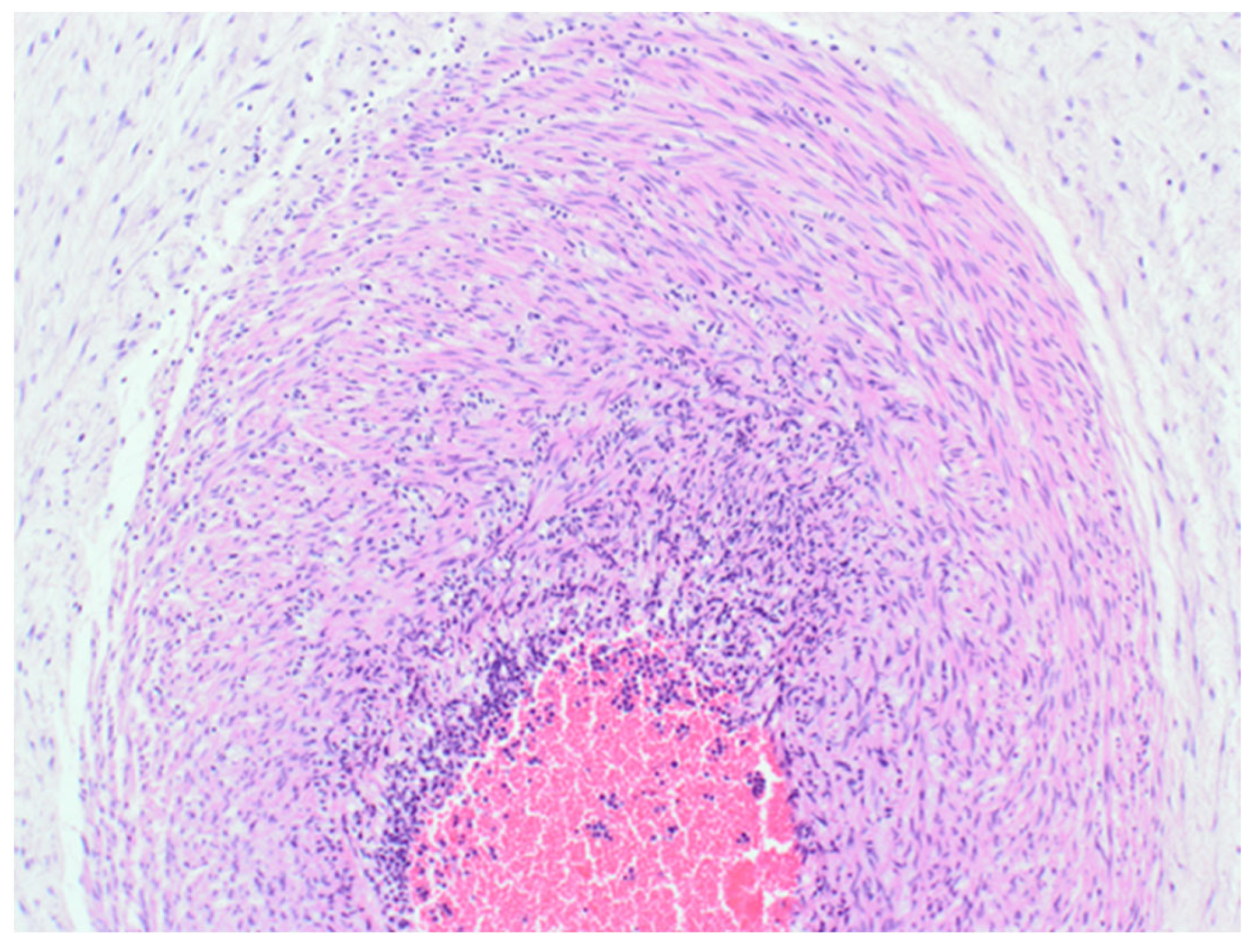
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rueda, M.S.; Hefter, Y.; Stone, B.; Hahn, A.; Jantausch, B. A Premature Infant With Neonatal Actinomyces odontolyticus Sepsis. J. Pediatr. Infect. Dis. Soc. 2021, 10, 533–535. [Google Scholar] [CrossRef] [PubMed]
- Ong, H.-C.; Ling, A.C.-K.; Ng, D.S.-W.; Ng, R.-X.; Wong, P.-L.; Omar, S.F.S. Case report: Actinomyces naeslundii complicating preterm labour in a trisomy-21 pregnancy. ID Cases 2021, 23, e01051. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Cavoretto, P.I.; Barros, F.C.; Romero, R.; Papageorghiou, A.T.; Kennedy, S.H. Etiologically Based Functional Taxonomy of the Preterm Birth Syndrome. Clin. Perinatol. 2024, 51, 475–495. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ye, Z.; Miao, Q.; Xu, H.; Pang, W. Actinomyces meyeri-induced brain abscess in pregnancy: A case report. BMC Neurol. 2023, 23, 401. [Google Scholar] [CrossRef] [PubMed]
- Gajdács, M.; Urbán, E. The Pathogenic Role of Actinomyces spp. and Related Organisms in Genitourinary Infections: Discoveries in the New, Modern Diagnostic Era. Antibiotics 2020, 9, 524. [Google Scholar] [CrossRef] [PubMed]
- Alsohime, F.; Assiri, R.A.; Al-Shahrani, F.; Bakeet, H.; Elhazmi, M.; Somily, A.M. Premature labor and neonatal sepsis caused by Actinomyces neuii. J. Infect. Public Health 2019, 12, 282–284. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, A.; Tabb, D.; Hagan, L. Preterm Labor Caused by Hemolysis, Elevated Liver Enzymes, Low Platelet Count (HELLP) Syndrome and Postpartum Infection Complicated with Actinomyces Species: A Case Report. Am. J. Case Rep. 2018, 19, 1350–1353. [Google Scholar] [CrossRef] [PubMed]
- Neuz-Zaragoza, W.; Sanfeliu, I. Acute necritizing chorioaminionitis caused by Actinomyces Neuii. Enfermedades Infecc. Y Microbiol. Clínica 2022, 40, 455–464. [Google Scholar]
- Wong, V.K.; Turmezei, T.D.; Weston, V.C. Actinomycosis. BMJ 2011, 343, d6099. [Google Scholar] [CrossRef] [PubMed]
- Gajdács, M.; Urbán, E.; Terhes, G. Microbiological and Clinical Aspects of Cervicofacial Actinomyces Infections: An Overview. Dent. J. 2019, 7, 85. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Youm, J.; Kim, J.H.; Jee, B.C. Actinomyces-like organisms in cervical smears: The association with intrauterine device and pelvic inflammatory diseases. Obstet. Gynecol. Sci. 2014, 57, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Ohuma, E.O.; Moller, A.-B.; Bradley, E.; Chakwera, S.; Hussain-Alkhateeb, L.; Lewin, A.; Okwaraji, Y.B.; Mahanani, W.R.; Johansson, E.W.; Lavin, T.; et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: A systematic analysis. Lancet 2023, 402, 1261–1271, Erratum in Lancet 2024, 403, 618. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.-R.; Tsai, C.-C.; Chan, J.Y.H.; Lee, W.-C.; Wu, K.L.H.; Tain, Y.-L.; Hsu, T.-Y.; Cheng, H.-H.; Huang, H.-C.; Huang, C.-H.; et al. A Higher Abundance of Actinomyces spp. in the Gut Is Associated with Spontaneous Preterm Birth. Microorganisms 2023, 11, 1171. [Google Scholar] [CrossRef] [PubMed]
- Kahle, P.J.; Mellinger, G.T. Renal actinomycosis in pregnancy; report of a case. Urol. Cutan. Rev. 1949, 53, 720–723. [Google Scholar] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Idaewor, P.E.; Ozua, P.; Jaiyesimi, R.A.K.; Al-Zawi, A.S.A. Actinomyces in Pregnancy: A Rare and Silent Cause of Preterm Delivery—Case Report. Reprod. Med. 2025, 6, 7. https://doi.org/10.3390/reprodmed6010007
Idaewor PE, Ozua P, Jaiyesimi RAK, Al-Zawi ASA. Actinomyces in Pregnancy: A Rare and Silent Cause of Preterm Delivery—Case Report. Reproductive Medicine. 2025; 6(1):7. https://doi.org/10.3390/reprodmed6010007
Chicago/Turabian StyleIdaewor, Philip E., Peter Ozua, Rotimi A. K. Jaiyesimi, and Abdalla SAAD Abdalla Al-Zawi. 2025. "Actinomyces in Pregnancy: A Rare and Silent Cause of Preterm Delivery—Case Report" Reproductive Medicine 6, no. 1: 7. https://doi.org/10.3390/reprodmed6010007
APA StyleIdaewor, P. E., Ozua, P., Jaiyesimi, R. A. K., & Al-Zawi, A. S. A. (2025). Actinomyces in Pregnancy: A Rare and Silent Cause of Preterm Delivery—Case Report. Reproductive Medicine, 6(1), 7. https://doi.org/10.3390/reprodmed6010007





