Pre-Operative Anxiety Related to Major Urogynecologic Surgery: Insights from Perioperative Survey Data in Maine
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility
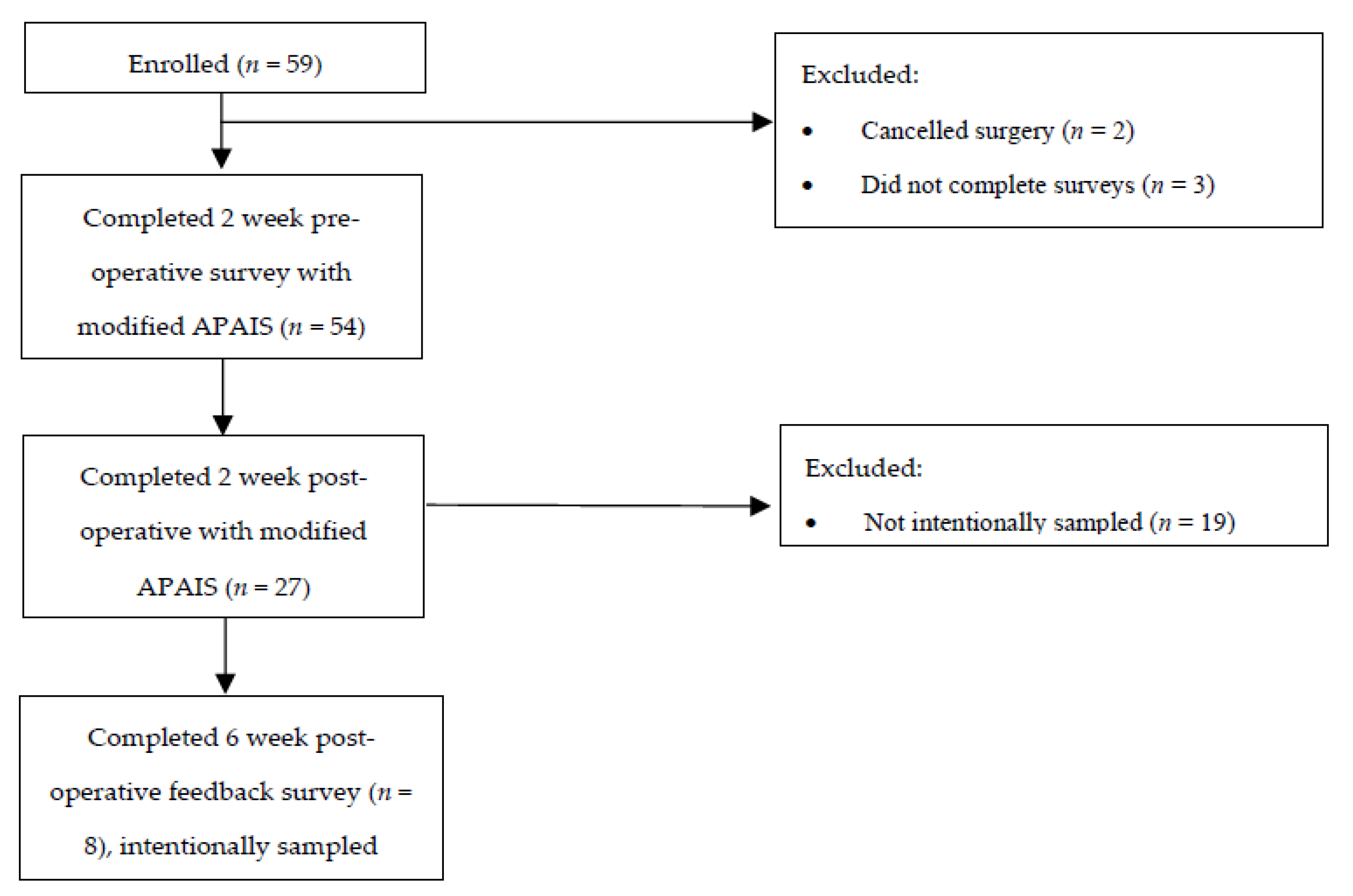
2.2. Enrollment
2.3. Sample Size Estimates
2.4. Data Collection
2.5. Data Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oliphant, S.S.; Jones, K.A.; Wang, L.; Bunker, C.H.; Lowder, J.L.M. Trends over time with commonly performed obstetric and gynecologic inpatient procedures. Obstet. Gynecol. 2010, 116, 926–931. [Google Scholar] [CrossRef]
- Geynisman-Tan, J.; Kenton, K. Surgical Updates in the Treatment of Pelvic Organ Prolapse. Rambam Maimonides Med. J. 2017, 8, e0017. [Google Scholar] [CrossRef]
- Ocalan, R.; Akin, C.; Disli, Z.K.; Kilinc, T.; Ozlugedik, S. Preoperative anxiety and postoperative pain in patients undergoing septoplasty. Belg. ENT 2015, 11, 19–23. [Google Scholar]
- Raichle, K.A.; Osborne, T.L.; Jensen, M.P.; Ehde, D.M.; Smith, D.G.; Robinson, L.R. Preoperative state anxiety, acute postoperative pain, and analgesic use in persons undergoing lower limb amputation. Clin. J. Pain 2015, 31, 699–706. [Google Scholar] [CrossRef]
- Ali, A.; Altun, D.; Oguz, B.H.; Ilhan, M.; Demircan, F.; Koltka, K. The effect of preoperative anxiety on postoperative analgesia and anesthesia recovery in patients undergoing laparoscopic cholecystectomy. J. Anesth. 2014, 28, 222–227. [Google Scholar] [CrossRef]
- Williams, J.B.; Alexander, K.P.; Morin, J.-F.; Langlois, Y.; Noiseux, N.; Perrault, L.P.; Smolderen, K.; Arnold, S.V.; Eisenberg, M.J.; Pilote, L.; et al. Preoperative anxiety as a predictor of mortality and major morbidity in patients aged >70 years undergoing cardiac surgery. Am. J. Cardiol. 2013, 111, 137–142. [Google Scholar] [CrossRef]
- Guo, P. Preoperative education interventions to reduce anxiety and improve recovery among cardiac surgery patients: A review of randomised controlled trials. J. Clin. Nurs. 2015, 24, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Carr, E.; Brockbank, K.; Allen, S.; Strike, P. Patterns and frequency of anxiety in women undergoing gynaecological surgery. J. Clin. Nurs. 2006, 15, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Pinar, G.; Kurt, A.; Gungor, T. The efficacy of preoperative instruction in reducing anxiety following gyneoncological surgery: A case control study. World J. Surg. Oncol. 2013, 9, 38. [Google Scholar] [CrossRef] [PubMed]
- Oliphant, S.S.; Lowder, J.L.; Ghetti, C.; Zyczynski, H.M. Effect of a preoperative self-catheterization video on anxiety: A randomized controlled trial. Int. Urogynecol. J. 2013, 24, 419–424. [Google Scholar] [CrossRef]
- Zhang, L.; Hao, L.-J.; Hou, X.-L.; Wu, Y.-L.; Jing, L.-S.; Sun, R.-N. Preoperative anxiety and postoperative pain in patients with laparoscopic hysterectomy. Front. Psychol. 2021, 12, 727250. [Google Scholar] [CrossRef]
- Larouche, M.; Brotto, L.A.; Koenig, N.A.B.; Lee, T.; Cundiff, G.W.; Geoffrion, R. Depression, anxiety, and pelvic floor symptoms before and after surgery for pelvic floor dysfunction. Female Pelvic Med. Reconstr. Surg. 2020, 26, 67–72. [Google Scholar] [CrossRef]
- Concato, J.; Peduzzi, P.; Holford, T.R.; Feinstein, A.R. Importance of events per independent variable in proportional hazard analysis. I. Background, goals, and general strategy. J. Clin. Epidemiol. 1995, 48, 1495–1501. [Google Scholar] [CrossRef]
- Peduzzi, P.; Concato, J.; Feinstein, A.R.; Holford, T.R. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J. Clin. Epidemiol. 1995, 48, 1503–1510. [Google Scholar] [CrossRef]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]
- The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 4 August 2021).
- Merman, N.; van Dam, F.S.; Muller, M.J.; Oosting, H. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth. Analg. 1996, 82, 445–451. [Google Scholar]
- Vergara-Romero, M.; Morales-Asencio, J.M.; Morales-Fernández, A.; Canca-Sanchez, J.C.; Rivas-Ruiz, F.; Reinaldo-Lapuerta, J.A. Validation of the Spanish version of the Amsterdam Preoperative Anxiety and Information Scale (APAIS). Health Qual. Life Outcomes 2017, 15, 120. [Google Scholar] [CrossRef]
- Song, B.; Yang, Y.; Teng, X.; Li, Y.; Bai, W.; Zhu, J. Use of pre-operative anxiety score to determine the precise dose of butorphanol for intra-operative sedation under regional anesthesia: A double-blinded randomized trial. Exp. Ther. Med. 2019, 18, 3885–3892. [Google Scholar] [CrossRef] [PubMed]
- Jovanovic, K.; Kalezic, N.; Grujicic, S.S.; Zivaljevic, V.; Jovanovic, M.; Savic, M.; Bukumiric, Z.; Dragas, M.; Sladojevic, M.; Trailovi, R.; et al. Translation and validation of the Amsterdam preoperative anxiety and information scale (APAIS) in Serbia. Brain Behav. 2022, 12, e2462. [Google Scholar] [CrossRef] [PubMed]
- Moss, C.; Pandya, P.R.; Yanek, L.; Lovejoy, D.; Muñiz, K.; Chen, C.C.G.; Blomquist, J.; Jacobs, S.; Powell, A.; Handa, V.L.; et al. The impact of anxiety on postoperative pain following pelvic reconstructive surgery. Int. Urogynecol. J. 2023, 34, 1551–1557. [Google Scholar] [CrossRef] [PubMed]
- Billiquist, E.J.; Michelfelder, A.; Brincat, C.; Brubaker, L.; Fitzgerald, C.M.; Mueller, E.R. Pre-operative guided imagery in female pelvic medicine and reconstructive surgery: A randomized trial. Int. Urogynecological J. 2018, 29, 1117–1122. [Google Scholar] [CrossRef]
- Chan, J.; Yeam, C.T.; Kee, H.M.; Tan, C.W.; Sultana, R.; Sia, A.T.H.; Sng, B.L. The use of pre-operative virtual reality to reduce anxiety in women undergoing gynecological surgeries: A prospective cohort study. BMC Anesthesiol. 2020, 20, 261. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.; McEnroe-Petitte, D.M. Influence of music on preoperative anxiety and physiological parameters in women undergoing gynecological surgery. Clin. Nurs. 2016, 25, 157–173. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Barnes, H.; Westbay, L.; Wolff, B.; Shannon, M.; Adams, W.; Acevedo-Alvarez, M.; Mueller, E.R.; Pham, T.T. Preoperative music listening in pelvic reconstructive surgery: A randomized trial. J. Am. Urogynecol. Soc. 2021, 27, 469–473. [Google Scholar] [CrossRef]
- Reynaud, D.; Bouscaren, N.; Lenclume, V.; Boukerrou, M. Comparing the effects of self selected music versus predetermined music on patient anxiety prior to gynaecological surgery: The MUANX randomized controlled trial. Trials 2021, 22, 535. [Google Scholar] [CrossRef]
- Liu, X.; Ren, J.-H.; Jiang, S.-S.; Tan, Y.; Ma, S.-G.; Huang, Y. Expressive arts therapy combined with progressive muscle relaxation following music for perioperative patients with gynecological malignancies: A pilot study. Evid.-Based Complement. Altern. Med. 2022, 2022, 6211581. [Google Scholar] [CrossRef]
- Jakobsen, C.; Blom, L.; Brondbjerg, M.; Lenler-Petersen, P. Effect of metoprolol and diazepam on preoperative anxiety. Anaesthesia 1990, 45, 40–43. [Google Scholar] [CrossRef]
- Joseph, T.; Krishna, H.M.; Kamath, S. Premedication with gabapentin, alprazolam or a placebo for abdominal hysterectomy: Effect on preoperative anxiety, postoperative pain and morphine consumption. Indian J. Anesth. 2014, 58, 694–699. [Google Scholar]
- Wunsch, J.; Klausenitz, C.; Janner, H.; Hesse, T.; Mustea, A.; Hahnenkamp, K.; Petersmann, A.; Usichenko, T.I. Auricular acupuncture for treatment of preoperative anxiety in patients scheduled for ambulatory gynaecological surgery: A prospective controlled investigation with a non-randomised arm. Acupunct. Med. 2018, 36, 222–227. [Google Scholar] [CrossRef]
- Bang, Y.; Lee, J.-H.; Kim, C.S.; Lee, Y.-Y.; Min, J.-J. Anxiolytic effects of chewing gum during preoperative fasting and patient-centered outcomes in female patients undergoing elective gynaecological surgery: A randomized controlled study. Sci. Rep. 2022, 12, 4165. [Google Scholar] [CrossRef]
| Variables | Completed Pre-Op Survey | Completed Post-Op Survey |
|---|---|---|
| Sample size | 54 | 27 |
| Age (years) | 62.0 (median, IQR: 53.8, 69.3) | 62 yo (median, IQR 50.5, 69) |
| Race * |
|
|
| Education highest level completed |
|
|
| Employment * |
|
|
| Income ** |
|
|
| Marital status |
|
|
| Ever diagnosed with mental health condition * |
|
|
| Other health conditions | 51 (91%) | 23 (85.5%) |
| Any prior surgery *** | Yes: 47 (94%) None: 3 (6%) | Yes: 21 (91.3%) None: 2 (8.7%) |
| Completed Pre-Op Survey Score [IQR] | Completed Post-Op Survey Score [IQR] | |
|---|---|---|
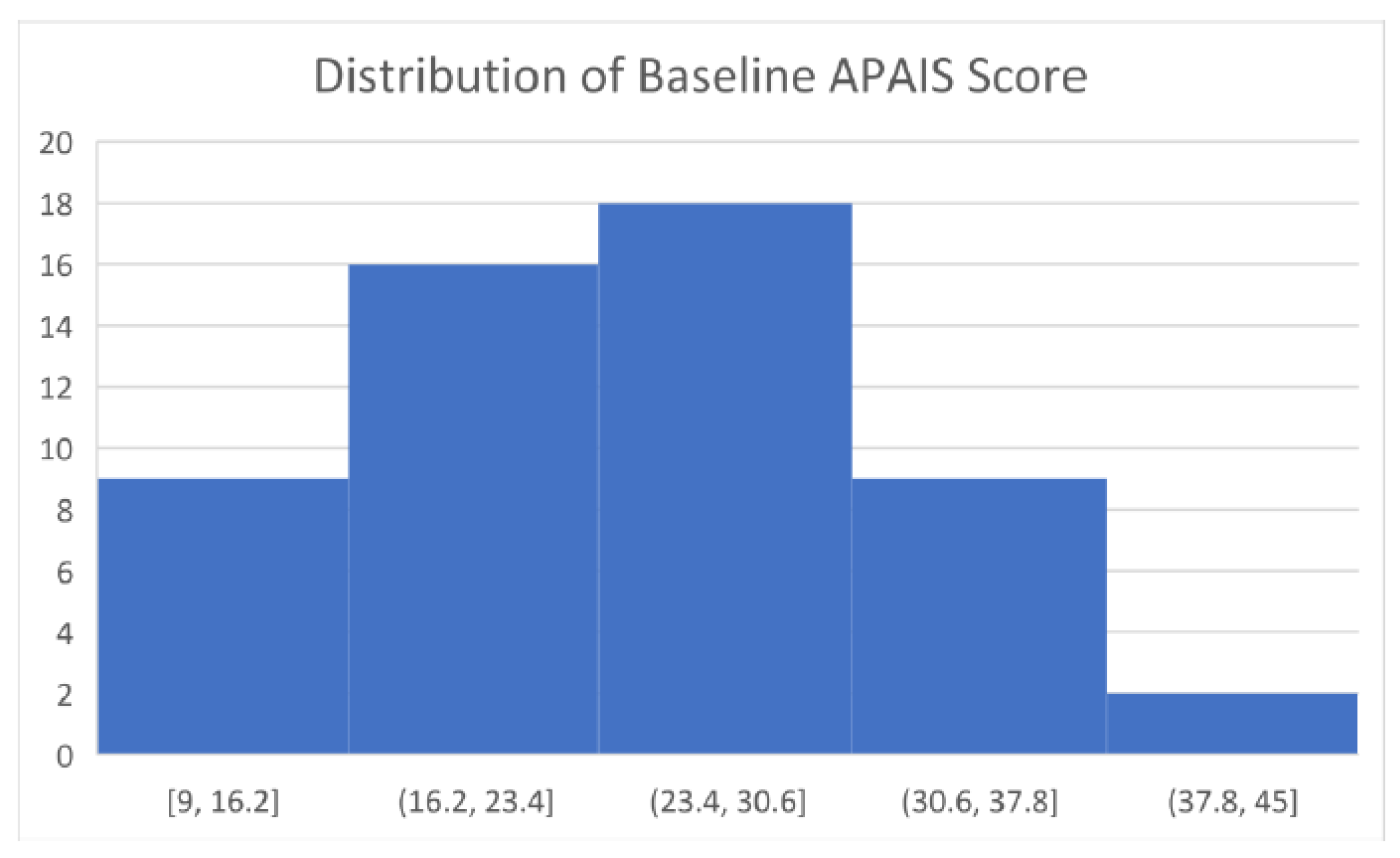
| Baseline APAIS Score | 24 [19.25, 29.75] | 24 [21.5, 29] |
| Complication | Frequency, n (%) |
|---|---|
| Urinary incontinence | 8 (14.8%) |
| Urinary retention | 3 (5.6%) |
| Urinary tract infection | 4 (7.4%) |
| Deep vein thrombosis/Pulmonary Embolism | 1 (1.8%) |
| Vaginal bleeding | 2 (3.7%) |
| Wound-related issue | 2 (3.7%) |
| Recurrent prolapse | 4 (7.4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaonga, N.N.; Courbron, Y.; Holmgren, E.; Konzal, E.; Williams, W.; Brandes, M.; Foust-Wright, C. Pre-Operative Anxiety Related to Major Urogynecologic Surgery: Insights from Perioperative Survey Data in Maine. Reprod. Med. 2024, 5, 23-31. https://doi.org/10.3390/reprodmed5010003
Kaonga NN, Courbron Y, Holmgren E, Konzal E, Williams W, Brandes M, Foust-Wright C. Pre-Operative Anxiety Related to Major Urogynecologic Surgery: Insights from Perioperative Survey Data in Maine. Reproductive Medicine. 2024; 5(1):23-31. https://doi.org/10.3390/reprodmed5010003
Chicago/Turabian StyleKaonga, Nadi Nina, Yanghee Courbron, Emmy Holmgren, Eliot Konzal, Whitney Williams, Mary Brandes, and Caroline Foust-Wright. 2024. "Pre-Operative Anxiety Related to Major Urogynecologic Surgery: Insights from Perioperative Survey Data in Maine" Reproductive Medicine 5, no. 1: 23-31. https://doi.org/10.3390/reprodmed5010003
APA StyleKaonga, N. N., Courbron, Y., Holmgren, E., Konzal, E., Williams, W., Brandes, M., & Foust-Wright, C. (2024). Pre-Operative Anxiety Related to Major Urogynecologic Surgery: Insights from Perioperative Survey Data in Maine. Reproductive Medicine, 5(1), 23-31. https://doi.org/10.3390/reprodmed5010003







