Travel during Pregnancy: A Web-Based Survey of People Who Have Been Pregnant within the Past 10 Years
Abstract
1. Introduction
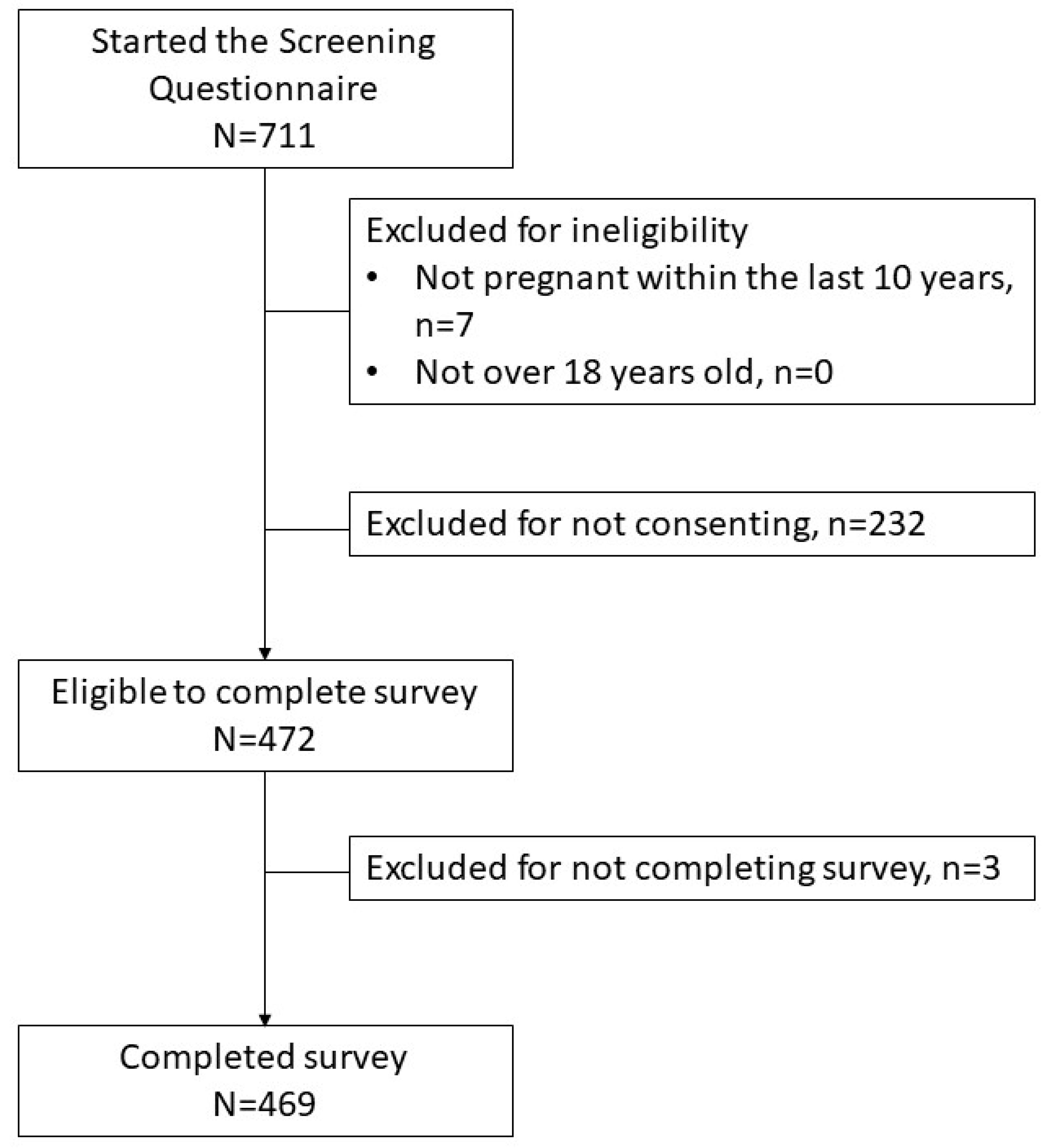
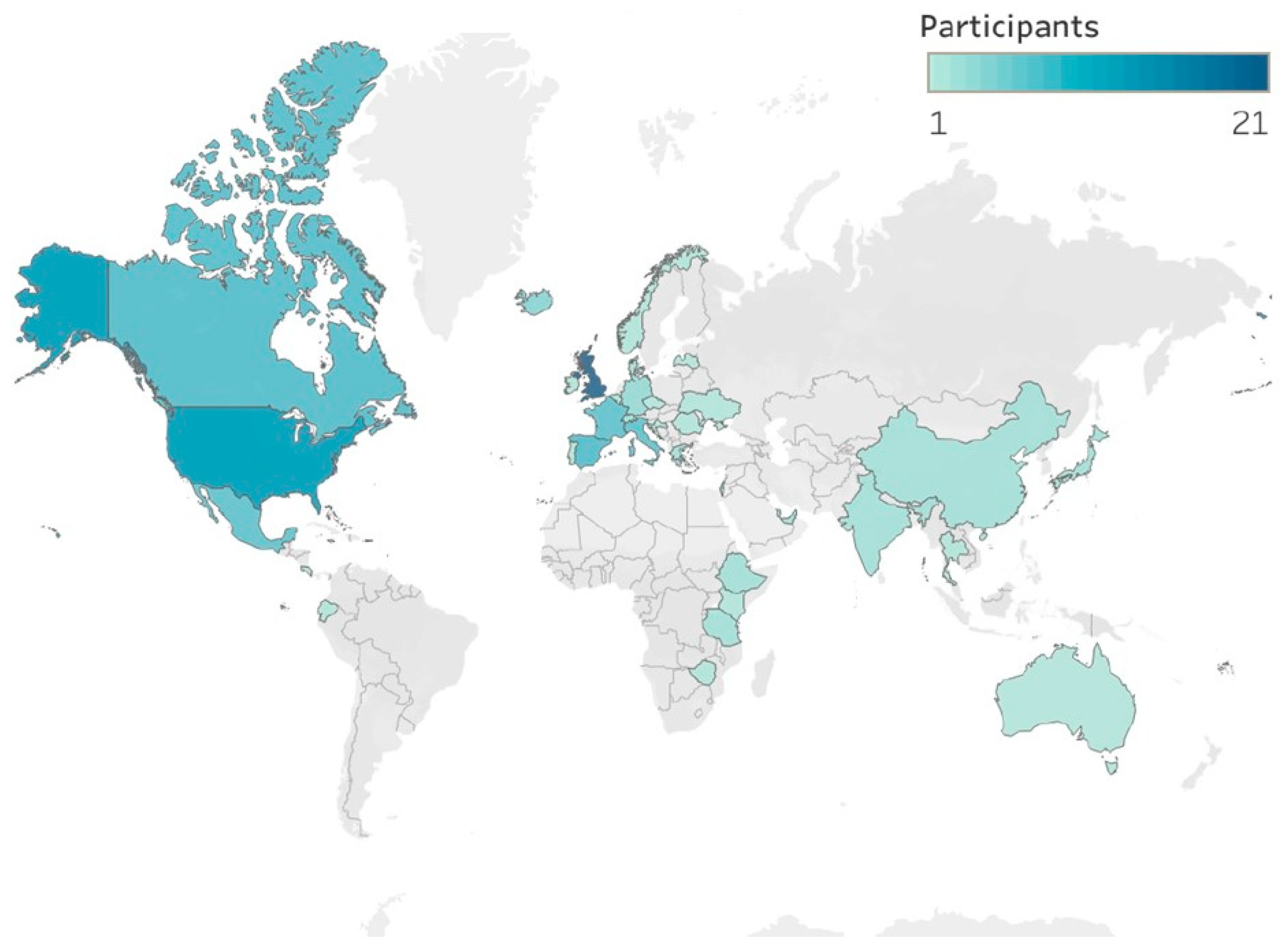
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jones, C.A.; Chan, C. Bon Voyage: An Update on Safe Travel in Pregnancy. J. Obstet. Gynaecol. Can. 2014, 36, 1101–1106. [Google Scholar] [CrossRef]
- Melidosian, L.; Evans, E.; Stewart, K.; Antony, K.M. Travel during pregnancy: A study of postpartum women in Madison, Wisconsin. WMJ 2019, 118, 114–119. [Google Scholar] [PubMed]
- Antony, K.M.; Gupta, V.K.; Hoppe, K.K.; Quamme, T.; Feldman, N.; Stewart, K. Travel during Pregnancy: Results from an Ultrasound Unit-Based Questionnaire. WMJ 2017, 116, 49–54. [Google Scholar]
- Antony, K.M.; Ehrenthal, D.; Evensen, A.; Iruretagoyena, J.I. Travel during Pregnancy: Considerations for the Obstetric Provider. Obstet. Gynecol. Surv. 2017, 72, 97–115. [Google Scholar] [CrossRef]
- VJaeger, V.K.; Tschudi, N.; Rüegg, R.; Hatz, C.; Bühler, S. The elderly, the young and the pregnant traveler—A retrospective data analysis from a large Swiss Travel Center with a special focus on malaria prophylaxis and yellow fever vaccination. Travel Med. Infect. Dis. 2015, 13, 475–484. [Google Scholar] [CrossRef]
- Lagerberg, R.E. Malaria in Pregnancy: A Literature Review. J. Midwifery Women’s Health 2008, 53, 209–215. [Google Scholar] [CrossRef]
- Rice, M.E.; Galang, R.R.; Roth, N.M.; Ellington, S.R.; Moore, C.A.; Valencia-Prado, M.; Ellis, E.M.; Tufa, A.J.; Taulung, L.A.; Alfred, J.M.; et al. Vital signs: Zika-associated birth defects and neurodevelopmental abnormalities possibly associated with congenital zika virus infection—U.S. Territories and freely associated states, 2018. Morb. Mortal. Wkly. Rep. 2018, 67, 858–867. [Google Scholar] [CrossRef]
- Lindsay, S.; Ansell, J.; Selman, C.; Cox, V.; Hamilton, K.; Walraven, G. Effect of pregnancy on exposure to malaria mosquitoes. Lancet 2000, 355, 1972. [Google Scholar] [CrossRef]
- Ansell, J.; Hamilton, K.; Pinder, M.; Walraven, G.; Lindsay, S. Short-range attractiveness of pregnant women to Anopheles gambiae mosquitoes. Trans. R. Soc. Trop. Med. Hyg. 2002, 96, 113–116. [Google Scholar] [CrossRef]
- Sholapurkar, S.L.; Gupta, A.N.; Mahajan, R.C. Clinical course of malaria in pregnancy—A prospective controlled study from India. Trans. R. Soc. Trop. Med. Hyg. 1988, 82, 376–379. [Google Scholar] [CrossRef]
- World Health Organization Division of Control of Tropical Diseases. Severe and Complicated Malaria. Trans. R. Soc. Trop. Med. Hyg. 1990, 84 (Suppl. S2), 1–65. [Google Scholar] [CrossRef]
- McGregor, I.A. Epidemiology, malaria, and pregnancy. Am. J. Trop. Med. Hyg. 1984, 33, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Smereck, J. Malaria in pregnancy: Update on emergency management. J. Emerg. Med. 2011, 40, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, E.; Hidalgo, L.; Chedraui, P. The effect of malarial infection on maternal-fetal outcome in Ecuador. J. Matern. Fetal. Neonatal Med. 2005, 18, 101–105. [Google Scholar] [CrossRef]
- Ducarme, G.; Thuillier, C.; Wernet, A.; Bellier, C.; Luton, D. Malaria in pregnant woman masquerading as HELLP syndrome. Am. J. Perinatol. 2009, 27, 171–172. [Google Scholar] [CrossRef]
- Newman, R.D.; Hailemariam, A.; Jimma, D.; Degifie, A.; Kebede, D.; Rietveld, A.E.C.; Nahlen, B.L.; Barnwell, J.W.; Steketee, R.W.; Parise, M.E. Burden of malaria during pregnancy in areas of stable and unstable transmission in Ethiopia during a nonepidemic year. J. Infect. Dis. 2003, 187, 1765–1772. [Google Scholar] [CrossRef]
- Singh, N.; Saxena, A.; Chand, S.K.; Valecha, N.; Sharma, V.P. Studies on malaria during pregnancy in a tribal area of central India (Madhya Pradesh). Southeast Asian J. Trop. Med. Public Health 1998, 29, 10–17. [Google Scholar]
- de Barros Miranda-Filho, D.; Martelli, C.M.T.; de Alencar Ximenes, R.A.; Araújo, T.V.B.; Rocha, M.A.W.; Ramos, R.C.F.; Dhalia, R.; de Oliveira França, R.F.; de Azevedo Marques Júnior, E.T.; Rodrigues, L.C. Initial description of the presumed congenital Zika syndrome. Am. J. Public Health 2016, 106, 598–600. [Google Scholar] [CrossRef]
- Costello, A.; Dua, T.; Duran, P.; Gülmezoglu, M.; Oladapo, O.T.; Perea, W.; Pires, J.; Ramon-Pardo, P.; Rollins, N.; Saxena, S. Defining the syndrome associated with congenital Zika virus infection. Bull. World Health Organ. 2016, 94, 406. [Google Scholar] [CrossRef]
- Pomar, L.; Musso, D.; Malinger, G.; Vouga, M.; Panchaud, A.; Baud, D. Zika virus during pregnancy: From maternal exposure to congenital Zika virus syndrome. Prenat. Diagn. 2019, 39, 420–430. [Google Scholar] [CrossRef]
- Freitas, D.A.; Souza-Santos, R.; Carvalho, L.M.A.; Barros, W.B.; Neves, L.M.; Brasil, P.; Wakimoto, M.D. Congenital Zika syndrome: A systematic review. PLoS ONE 2020, 15, e0242367. [Google Scholar] [CrossRef] [PubMed]
- Puntasecca, C.J.; King, C.H.; LaBeaud, A.D. Measuring the global burden of Chikungunya and Zika viruses: A systematic review. PLoS Negl. Trop. Dis. 2021, 15, e0009055. [Google Scholar] [CrossRef] [PubMed]
- DeSisto, C.L.; Wallace, B.; Simeone, R.M.; Polen, K.; Ko, J.Y.; Meaney-Delman, D.; Ellington, S.R. Risk for Stillbirth among Women with and without COVID-19 at Delivery Hospitalization—United States, March 2020–September 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1640–1645. [Google Scholar] [CrossRef]
- Kasehagen, L.; Byers, P.; Taylor, K.; Kittle, T.; Roberts, C.; Collier, C.; Rust, B.; Ricaldi, J.N.; Green, J.; Zapata, L.B.; et al. COVID-19—Associated Deaths after SARS-CoV-2 Infection during Pregnancy—Mississippi, 1 March 2020–6 October 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1646–1648. [Google Scholar] [CrossRef] [PubMed]
- Zambrano, L.D.; Ellington, S.; Strid, P.; Galang, R.R.; Oduyebo, T.; Tong, V.T.; Woodworth, K.R.; Nahabedian, J.F.; Azziz-Baumgartner, E.; Gilboa, S.M.; et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status—United States, 22 January–3 October 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1641–1647. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Squiers, L.; Lynch, M.; Dolina, S.; Ray, S.; Kelly, B.; Herrington, J.; Turner, M.; Chawla, D.; Becker-Dreps, S.; Stamm, L.; et al. Zika and travel in the news: A content analysis of US news stories during the outbreak in 2016–2017. Public Health 2019, 168, 164–167. [Google Scholar] [CrossRef]
- Chandrasekaran, N.; Marotta, M.; Taldone, S.; Curry, C. Perceptions of Community Risk and Travel during Pregnancy in an –Area of Zika Transmission. Cureus 2017, 9, 7–10. [Google Scholar] [CrossRef]
- Gallivan, M.; Oppenheim, B.; Madhav, N.K. Using social media to estimate Zika’s impact on tourism: #babymoon, 2014–2017. PLoS ONE 2019, 14, e0212507. [Google Scholar] [CrossRef]
- United Nations Development Programme. A Socio-Economic Impact Assessment of the Zika Virus in Latin America and the Caribbean with a Focus on Brazil, Colombia and Suriname. 2017. Available online: https://www.undp.org/publications/socio-economic-impact-assessment-zika-virus-latin-america-and-caribbean?utm_source=EN&utm_medium=GSR&utm_content=US_UNDP_PaidSearch_Brand_English&utm_campaign=CENTRAL&c_src=CENTRAL&c_src2=GSR&gclid=Cj0KCQjwkOqZBhDNARIsAAC (accessed on 9 March 2022).
- Chibber, R.; Al-Sibai, M.H.; Qahtani, N. Adverse outcome of pregnancy following air travel: A myth or a concern? Aust. N. Z. J. Obstet. Gynaecol. 2006, 46, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Bühler, S.; Rüegg, R.; Steffen, R.; Hatz, C.; Jaeger, V.K. A profile of travelers—An analysis from a large Swiss travel clinic. J. Travel Med. 2014, 21, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Centers for Disease Control and Prevention: Zika Virus: Zika Travel Information. Available online: https://wwwnc.cdc.gov/travel/page/zika-travel-information (accessed on 4 May 2019).
- Centers for Disease Control and Prevention. COVID-19 Travel Recommendations by Destination. COVID-19 Travel Recommendations by Destination. Available online: https://www.cdc.gov/coronavirus/2019-ncov/travelers/map-and-travel-notices.html (accessed on 24 February 2022).
- Better Homes & Gardens (Ed.) Better Homes and Gardens Baby Book: A Handbook for Parents by the Better Homes & Gardens Child Care and Training Department, 5th ed.; Meredith Publishing Company: Des Moines, IA, USA, 1951. [Google Scholar]
- Ram, H.S.; Ram, S.; Miller, N.; Rosental, Y.S.; Chodick, G. Air travel during pregnancy and the risk of adverse pregnancy outcomes as gestational age and weight at birth: A retrospective study among 284,069 women in Israel between the years 2000 to 2016. PLoS ONE 2020, 15, e0228639. [Google Scholar] [CrossRef]
- Freeman, M.; Ghidini, A.; Spong, C.Y.; Tchabo, N.; Bannon, P.Z.; Pezzullo, J.C. Does air travel affect pregnancy outcome? Arch. Gynecol. Obstet. 2003, 269, 274–277. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. Prediction and prevention of spontaneous preterm birth. ACOG Practice Bulletin No. 234. Obstet. Gynecol. 2021, 138, e65–e90. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 200: Early pregnancy loss. Obstet. Gynecol. 2018, 132, e197–e207. [Google Scholar] [CrossRef]
- Aw, B.; Boraston, S.; Botten, D.; Cherniwchan, D.; Fazal, H.; Kelton, T.; Libman, M.; Saldanha, C.; Saldanha, C.; Stowe, B. Travel Medicine: What’s Involved? When to Refer? Can. Fam. Physician 2014, 60, 1091–1103. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4264804/ (accessed on 10 August 2016).
| Characteristic | No Domestic Travel | Domestic Travel | p * | ||
|---|---|---|---|---|---|
| N = 79 | N = 390 | ||||
| Age (mean, SD) | 34.8 (3.9) | 34.3 (3.7) | 0.290 | ||
| Advanced maternal age (n, %) | 32 (40.5) | 144 (36.9) | 0.549 | ||
| Race (n, %) | |||||
| White/Caucasian | 59 (74.7) | 319 (82.6) | 0.005 | ||
| African American | 3 (3.8) | 12 (3.1) | |||
| American Indian or Alaskan Native | 0 (0) | 2 (0.5) | |||
| Asian | 7 (8.9) | 41 (10.6) | |||
| Native Hawaiian or other Pacific Islander | 1 (1.3) | 0 (0) | |||
| From multiple races | 4 (5.1) | 6 (1.6) | |||
| Other or prefer not to answer | 5 (6.3) | 6 (1.6) | |||
| Hispanic or Latina (n, %) | 7 (9.0) | 28 (7.2) | 0.600 | ||
| Marital status (n, %) | |||||
| Currently married or living with partner | 79 (100.0) | 380 (97.4) | 0.150 | ||
| Currently widowed, divorced, separated, or never married/not living with partner | 0 (0) | 10 (2.6) | |||
| Highest educational level (n, %) | |||||
| High school or less than high school | 0 (0) | 3 (0.8) | 0.078 | ||
| Some or completed college | 19 (24.1) | 56 (14.4) | |||
| Graduate degree | 60 (76.0) | 331 (84.9) | |||
| Annual Income (n, %) | |||||
| <$50,000 | 10 (12.7) | 43 (11.0) | 0.010 | ||
| $50,000–149,999 | 29 (36.7) | 84 (21.5) | |||
| $150,000 or more | 40 (50.6) | 263 (67.4) | |||
| Residence † (n, %) | 0.032 | ||||
| Urban | 35 (44.3) | 121 (31.3) | |||
| Suburban | 41 (51.9) | 214 (55.3) | |||
| Rural | 3 (3.8) | 45 (11.6) | |||
| Other | 0 (0) | 7 (1.8) | |||
| Born in the United States † (n, %) | 62 (78.5) | 328 (84.8) | 0.169 | ||
| Parents born in the United States (n, %) | 50 (64.1) | 279 (72.3) | 0.147 | ||
| Primary household language English (n, %) | 67 (84.8) | 353 (91.7) | 0.057 | ||
| Medical comorbidities (n, %) | |||||
| Tobacco use | 0 (0) | 1 (0.26) | 0.651 | ||
| Diabetes | 5 (6.3) | 34 (8.8) | 0.469 | ||
| Hypertension | 11 (13.9) | 52 (13.4) | 0.908 | ||
| Thyroid disease | 6 (7.6) | 29 (7.5) | 0.975 | ||
| Asthma | 3 (3.8) | 32 (8.3) | 0.165 | ||
| Seizures | 0 (0) | 1 (0.3) | 0.652 | ||
| Body mass index ≥ 30 kg/m2 | 10 (12.7) | 75 (19.2) | 0.167 | ||
| Obstetric characteristics (n, %) | |||||
| Gravidity (median, IQR) | 3 (2–3) | 2 (2–3) | 0.151 | ||
| Gravida 1 ‡ | 12 (15.2) | 75 (19.5) | 0.382 | ||
| Gravida 2 | 26 (32.9) | 142 (36.9) | |||
| Gravida 3 or greater | 41 (51.9) | 168 (43.6) | |||
| First pregnancy (n, %) | 24 (30.4) | 129 (33.1) | 0.641 | ||
| Prior miscarriage | 34 (43.0) | 144 (36.9) | 0.307 | ||
| Twin pregnancy | 1 (1.3) | 8 (2.1) | 0.635 | ||
| Characteristic | No International or Non-Contiguous Travel | International or Non-Contiguous Travel | p † | ||
|---|---|---|---|---|---|
| N = 353 | N = 114 * | ||||
| Age (mean, SD) | 34.2 (3.6) | 34.8 (3.8) | 0.201 | ||
| Advanced maternal age (n, %) | 120 (33.9) | 55 (48.2) | 0.006 | ||
| Race (n, %) | |||||
| White/Caucasian | 298 (85.1) | 79 (69.3) | |||
| African American | 9 (2.6) | 6 (5.3) | |||
| American Indian or Alaskan Native | 1 (0.3) | 1 (0.9) | 0.020 | ||
| Asian | 28 (8.0) | 20 (17.5) | |||
| Native Hawaiian or other Pacific Islander | 1 (0.3) | 0 (0) | |||
| From multiple races | 6 (1.7) | 4 (3.5) | |||
| Other or prefer not to answer | 7 (2.1) | 4 (3.5) | |||
| Hispanic or Latina (n, %) | 25 (7.1) | 10 (8.8) | 0.551 | ||
| Marital status (n, %) | |||||
| Currently married or living with partner | 346 (98.0) | 112 (98.2) | 0.877 | ||
| Currently widowed, divorced, separated, or never married/not living with partner | 7 (2.0) | 2 (1.8) | |||
| Highest educational level (n, %) | |||||
| High school or less than high school | 2 (0.6) | 0 (0) | 0.665 | ||
| Some or completed college | 58 (16.4) | 17 (14.9) | |||
| Graduate degree | 293 (83.0) | 97 (85.1) | |||
| Annual Income (n, %) | |||||
| <$50,000 | 36 (10.2) | 16 (14.0) | 0.431 | ||
| $50,000–149,999 | 84 (23.8) | 29 (25.4) | |||
| $150,000 or more | 233 (66.0) | 69 (60.5) | |||
| Residence (n, %) | 0.024 | ||||
| Urban | 109 (31.1) | 47 (41.2) | |||
| Suburban | 199 (56.7) | 55 (48.2) | |||
| Rural | 40 (11.4) | 8 (7.0) | |||
| Other | 3 (0.8) | 4 (3.5) | |||
| Born in the United States ‡ (n, %) | 302 (86.0) | 87 (76.3) | 0.015 | ||
| Parents born in the United States (n, %) | 265 (75.7) | 63 (55.8) | <0.001 | ||
| Primary household language English (n, %) | 322 (92.3) | 97 (85.1) | 0.023 | ||
| Medical comorbidities (n, %) | |||||
| Tobacco use | 1 (0.3) | 0 (0) | 0.568 | ||
| Diabetes | 31 (8.8) | 8 (7.1) | 0.559 | ||
| Hypertension | 52 (14.8) | 11 (9.6) | 0.161 | ||
| Thyroid disease | 26 (7.4) | 9 (7.9) | 0.864 | ||
| Asthma | 31 (8.9) | 4 (3.5) | 0.059 | ||
| Seizures | 1 (0.3) | 0 (0) | 0.566 | ||
| Body mass index ≥ 30 kg/m2 | 72 (20.4) | 13 (11.4) | 0.030 | ||
| Obstetric characteristics (n, %) | |||||
| Gravidity (median, IQR) | 2 (2–3) | 2 (1–3) | 0.018 | ||
| Gravida 1 | 56 (16.0) | 31 (27.4) | 0.026 | ||
| Gravida 2 | 130 (37.1) | 37 (32.7) | |||
| Gravida 3or greater | 164 (46.9) | 45 (39.8) | |||
| First pregnancy (n, %) | 105 (29.8) | 48 (42.1) | 0.014 | ||
| Prior miscarriage | 140 (39.7) | 38 (33.3) | 0.227 | ||
| Twin pregnancy | 5 (1.4) | 4 (3.5) | 0.162 | ||
| Complication | No Domestic Travel | Domestic Travel | p | No International Travel | International Travel | p |
|---|---|---|---|---|---|---|
| N = 79 | N = 390 | N = 353 | N = 114 | |||
| Preterm birth * | 9 (11.4) | 29 (7.6) | 0.257 | 30 (8.6) | 8 (7.1) | 0.610 |
| Miscarriage † | 8 (10.3) | 7 (1.8) | <0.001 | 12 (3.4) | 3 (2.7) | 0.697 |
| Fetal anomalies ‡ | 3 (3.8) | 13 (3.4) | 0.833 | 13 (3.7) | 3 (2.6) | 0.579 |
| Venous thromboembolism § | 0 (0) | 1 (0.3) | 0.652 | 0 (0) | 1 (0.9) | 0.077 |
| Reason | Domestic Travel, n (%) | International Travel, n (%) |
|---|---|---|
| N = 390 * | N = 114 | |
| Work | 118 (30.4) | 32 (34.8) |
| Leisure/vacation | 355 (91.3) | 88 (94.6) |
| Family | 300 (77.1) | 73 (78.5) |
| Pregnancy or medical | 10 (2.6) | 2 (2.2) |
| Family emergency or unplanned travel | 28 (7.2) | 2 (2.2) |
| Characteristics | Domestic Travel, n (IQR) | International Travel, n (IQR) |
|---|---|---|
| N = 390 | N = 114 | |
| Duration by car travel, (hours) median (IQR) | 5 (3–8) | 3.5 (2–7) |
| Duration by air travel, (hours) median (IQR) | 4 (3–5) | 7 (5–12) |
| Number of trips, median (IQR, min-max) | 3 (2–4, 1–5) | 1 (1–1, 1–5) |
| Discussion Items | Domestic Travelers n = 390 | International Travelers n = 114 | |
|---|---|---|---|
| Participant discussed travel plans with OB provider | 170 (44.2) | 69 (61.1) | |
| Obstetric provider initiated the conversation and asked about travel * | 6 (3.6) | 2 (2.9) | |
| Obstetric provider’s recommendations about travel * | |||
| Generally supportive of travel plans * | 126 (74.1) | 55 (79.7) | |
| Discouraged travel * | 9 (5.3) | 3 (4.4) | |
| Discussed risks and benefits, left decision to pregnant person * | 35 (20.6) | 11 (15.9) | |
| Obstetric provider discussed risks and benefits of travel? | |||
| Risks of blood clots related to immobility | 97 (78.2) | 38 (86.4) | |
| Risk of food or water borne illness | 20 (16.1) | 14 (31.8) | |
| Risk of other illnesses | 35 (28.2) | 17 (38.6) | |
| Obstetric provider recommended the following | |||
| Frequent ambulation * | 127 (74.7) | 46 (66.7) | |
| Hydrating * | 130 (76.5) | 48 (69.6) | |
| Steps to avoid food and water borne illnesses *, ‡ | 26 (15.3) | 14 (20.3) | |
| Steps to avoid mosquito borne illnesses *, ‡ | 42 (25.0) | 22 (31.9) | |
| Obstetric provider reviewed the following | |||
| Signs of blood clots * | 83 (48.8) | 30 (43.5) | |
| Symptoms of travel related illnesses * | 28 (16.5) | 15 (21.7) | |
| Whether Zika was a concern *, ‡ | 40 (23.6) | 21 (30.4) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nechval, L.H.; Antony, K.M. Travel during Pregnancy: A Web-Based Survey of People Who Have Been Pregnant within the Past 10 Years. Reprod. Med. 2023, 4, 166-179. https://doi.org/10.3390/reprodmed4030016
Nechval LH, Antony KM. Travel during Pregnancy: A Web-Based Survey of People Who Have Been Pregnant within the Past 10 Years. Reproductive Medicine. 2023; 4(3):166-179. https://doi.org/10.3390/reprodmed4030016
Chicago/Turabian StyleNechval, Lada H., and Kathleen M. Antony. 2023. "Travel during Pregnancy: A Web-Based Survey of People Who Have Been Pregnant within the Past 10 Years" Reproductive Medicine 4, no. 3: 166-179. https://doi.org/10.3390/reprodmed4030016
APA StyleNechval, L. H., & Antony, K. M. (2023). Travel during Pregnancy: A Web-Based Survey of People Who Have Been Pregnant within the Past 10 Years. Reproductive Medicine, 4(3), 166-179. https://doi.org/10.3390/reprodmed4030016







