The History of the Discovery of Ectopic Epithelial Cells in Lower Peritoneal Organs: The So-Called Mucosal Invasion
Abstract
:1. Introduction
2. Early Descriptions
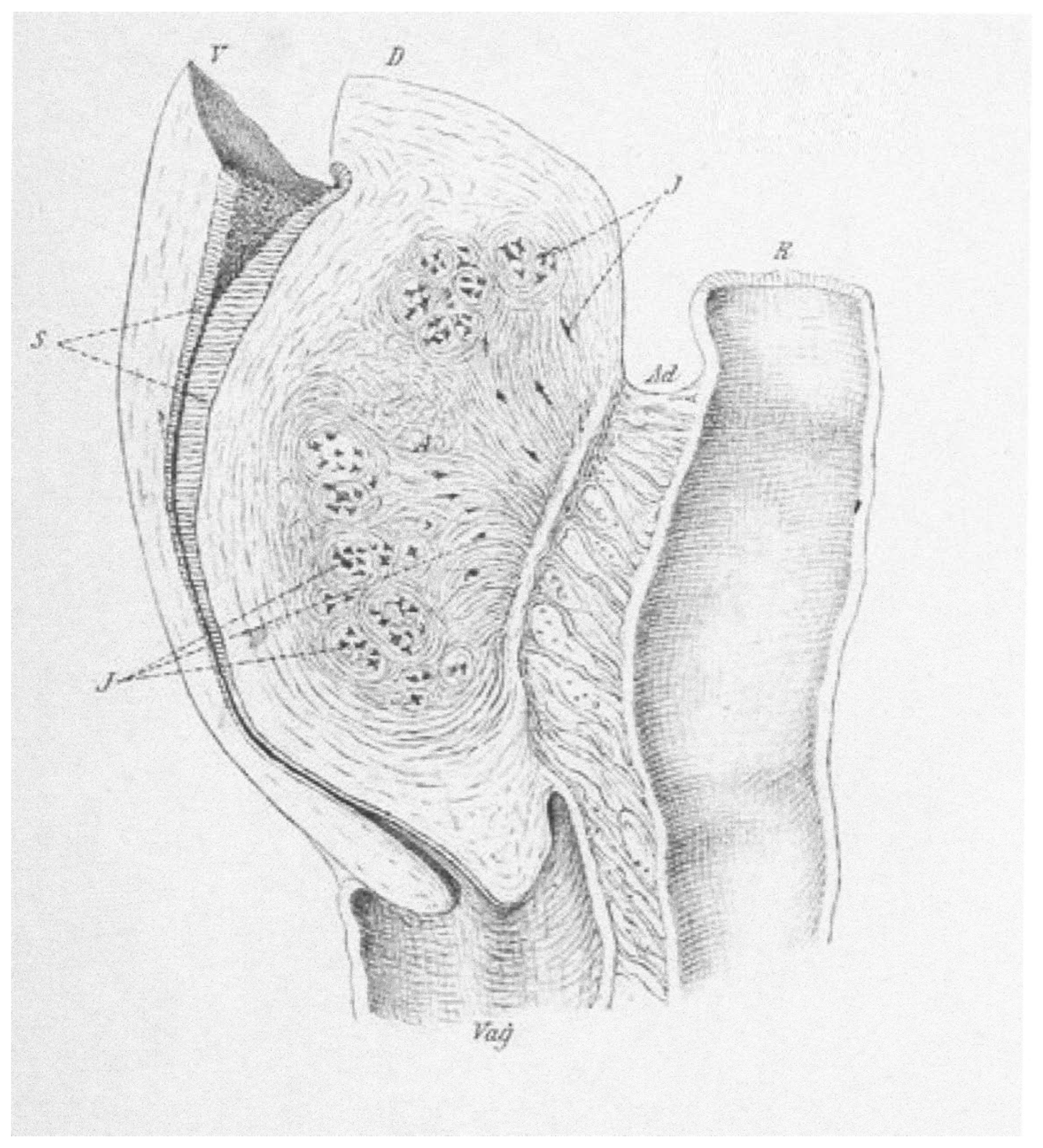
3. The Term Adenomyoma
- Hard: predominately made of muscle tissue.
- Cystic: containing visible cystic spaces and equal glandular and muscle tissue.
- Soft: predominately made of glandular tissue.
- Telangiectatic: soft, very vascular growths that are almost devoid of cysts.
4. The Search for the Origin of Mucosal Invasions
5. Introducing the Term Adenomyosis
6. Identification of Endometriosis
6.1. The Ovarian Endometrioma
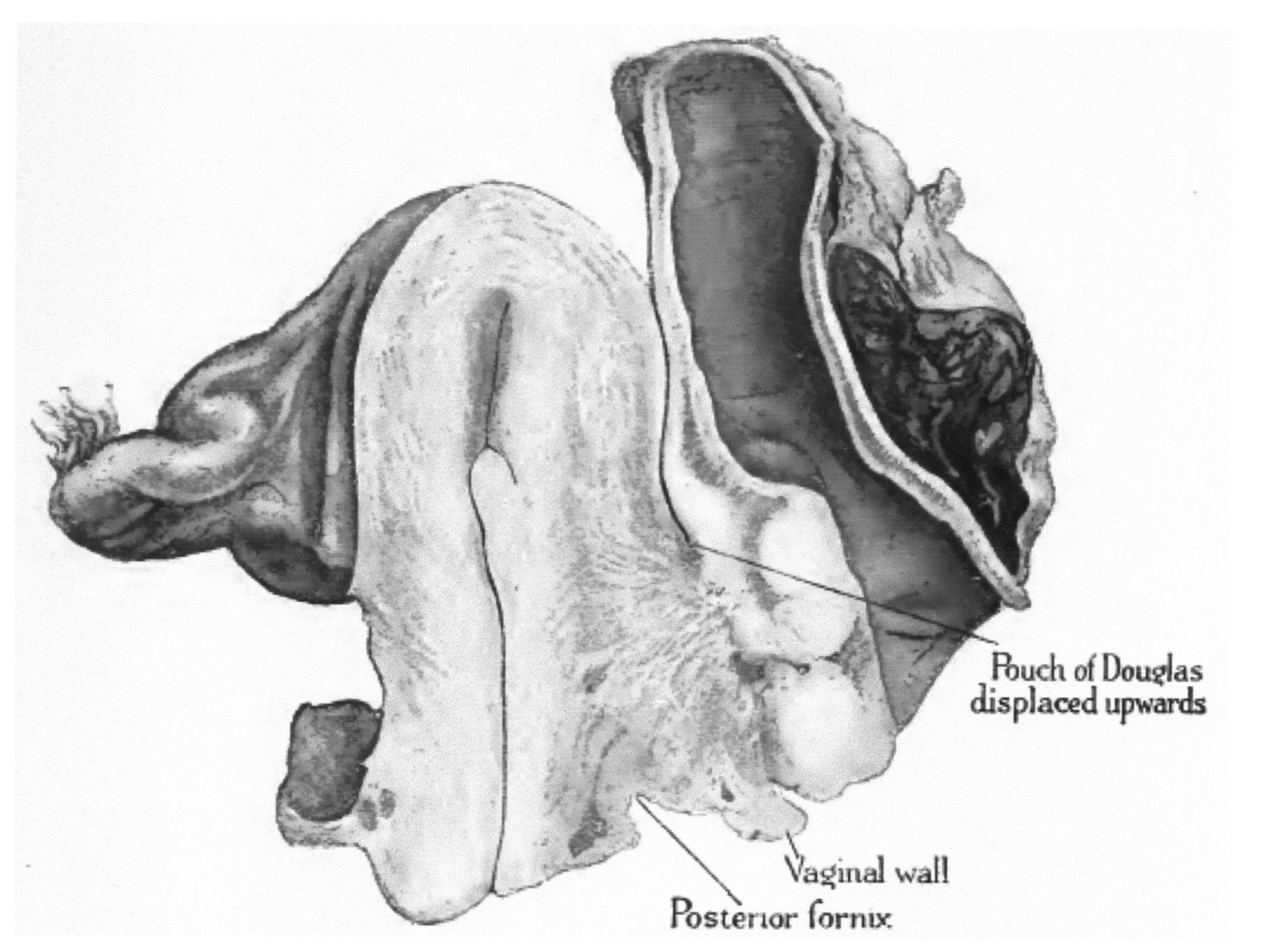
6.2. Deep, Infiltrating Endometriotic Nodules
6.3. Superficial Peritoneal Lesions
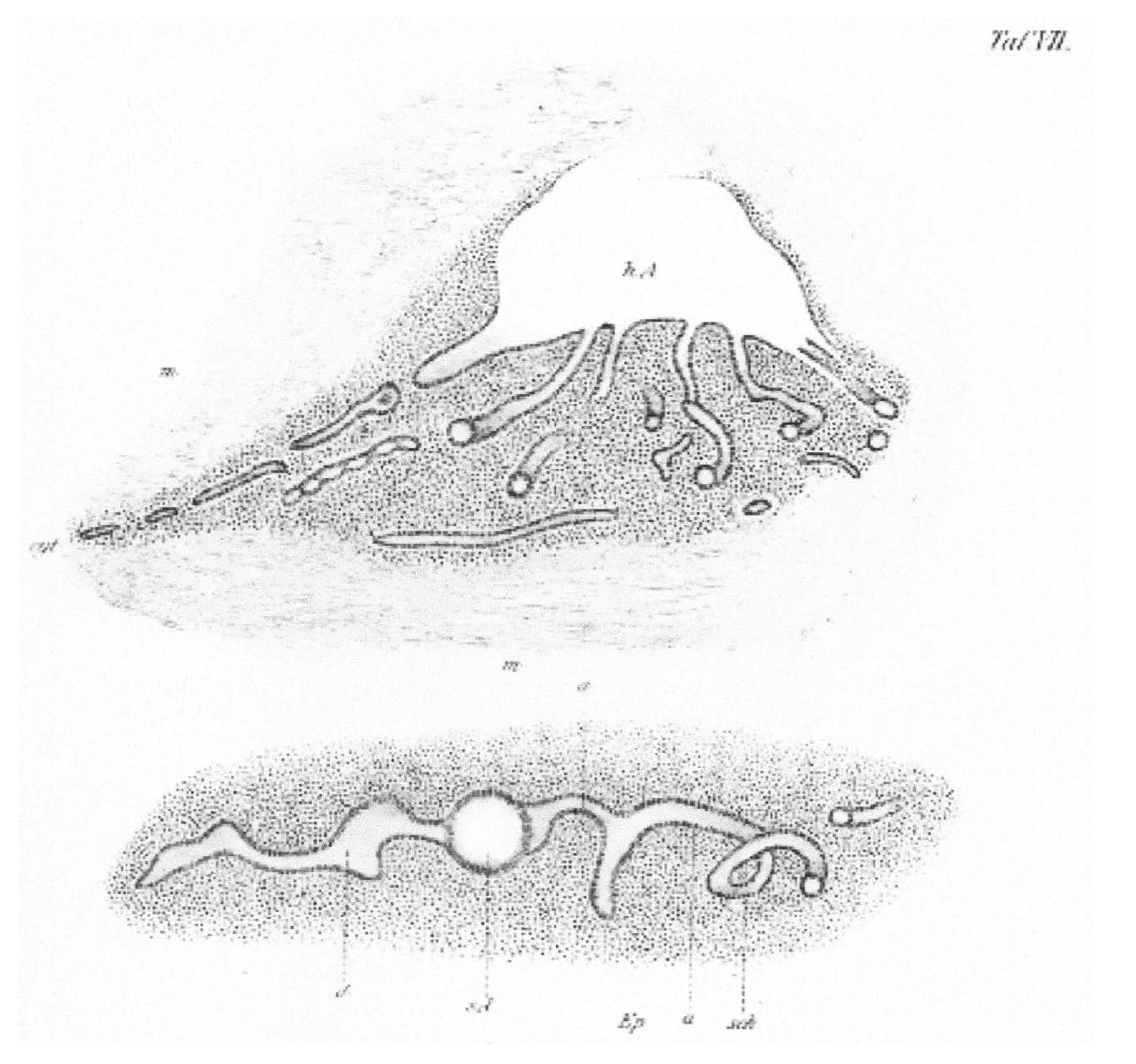
7. Tubal Adenomyosis
8. Other Types of Epithelia Present in Lower Peritoneal Organs
8.1. Müllerianosis and Mixed Endometrial-Myometrial Lesions
8.2. Endosalpingiosis
8.3. Endocervicosis
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Reverón, R.R. Marcello Malpighi (1628–1694), Founder of Microanatomy. Int. J. Morphol. 2011, 29, 399–402. [Google Scholar] [CrossRef] [Green Version]
- Hooke, R. Micrographia; The Royal Society: London, UK, 1665. [Google Scholar]
- Schleiden, M.J. Beiträge zur Phytogenesis. In Archiv Anatomie, Physiologie und Wissenschaftliche Medicin; Müller, J., Ed.; Viet: Berlin, Germany, 1838; pp. 137–176. [Google Scholar]
- Schwann, T. Mikroskopische Untersuchungen über die Übereinstimmung in der Struktur und dem Wachsthum der Thiere und Pflanzen; Verlag der Sander’schen Buchhandlung: Berlin, Germany, 1839. [Google Scholar]
- Wolff, C.F. Theoria Generationis; Halae ad Salam, Litteris Hendelianis: Halle (Saale), Germany, 1759. [Google Scholar]
- Pander, H.C. Beiträge zur Entwickelungsgeschichte des Hühnchens im Eye; Bronner: Vista, CA, USA, 1817. [Google Scholar]
- von Baer, K.E.; O’Malley, C.D. On the Genesis of the Ovum of Mammals and of Man; Isis: Oxford, UK, 1956; Volume 47, pp. 117–153. [Google Scholar]
- Müller, J. Bildungsgeschichte der Genitalien aus Anatomischen Untersuchungen an Embryonen des Menschen und der Thiere; Arnz: Düsseldorf, Germany, 1830. [Google Scholar]
- Grünwald, P. Zur entwicklungsmechanik des urogenitalsystems beim huhn. Wilhelm Roux Arch. Entwickl. Mech. Org. 1937, 136, 786–813. [Google Scholar] [CrossRef]
- Grünwald, P. The relation of the growing Müllerian duct to the Wolffian duct and its importance for the genesis of malformations. Anat. Rec. 1941, 81, 1–19. [Google Scholar] [CrossRef]
- Guioli, S.; Sekido, R.; Lovell-Badge, R. The origin of the Müllerian duct in chick and mouse. Dev. Biol. 2007, 302, 389–398. [Google Scholar] [CrossRef] [Green Version]
- Engelmann, G.J. The Mucous Membrane of the Uterus, with Special Reference to the Development and Structure of the Deciduae; William Wood and Co.: New York, NY, USA, 1875. [Google Scholar]
- Cullen, T.S. The distribution of adenomyomata containing uterine mucosa. Am. J. Obstet. Dis. Women Child. 1919, 80, 130–138. [Google Scholar]
- Cullen, T.S. The distribution of adenomyomas containing uterine mucosa. Arch. Surg. 1920, 1, 215–283. [Google Scholar] [CrossRef] [Green Version]
- Nezhat, C.; Nezhat, F.; Nezhat, C. Endometriosis: Ancient disease, ancient treatments. Fertil. Steril. 2012, 98, S1–S62. [Google Scholar] [CrossRef] [PubMed]
- Benagiano, G.; Lippi, D.; Brosens, I. Endometriosis: Ancient or Modern Disease? Indian J. Med. Res. 2015, 141, 69–71. [Google Scholar] [CrossRef] [Green Version]
- Knapp, V.J. How old is endometriosis? Late 17th- and 18th-century European descriptions of the disease. Fertil. Steril. 1999, 72, 10–14. [Google Scholar] [PubMed]
- Schrön, D.C. Disputatio Inauguralis Medica de Ulceribus Uteri; [Inaugural Medical Thesis on Ulcers of the Uterus]; Crause, R.W., Ed.; Literis Krebsianis: Jena, Germany, 1960; pp. 6–17. [Google Scholar]
- Crellius, J.F. Tumorem Fundo Uteri Externe Adhaerentem Describit; [Tumor Adhering to the Uterus Fundus is Described]; Ordinis Medici in Academia Vitembergensis: Würtemberg, Germany, 1739. [Google Scholar]
- Rokitansky, C.A. Manual of Pathological Anatomy (1849); Adlar: London, UK, 1854. [Google Scholar]
- Rokitansky, C. Über Uterusdrüsen-Neubildung in Uterus- und Ovarial-Sarcomen; [On the neoplasm of uterus glands on uterine and ovarian sarcomas]; Zeitschr Gesellschaft Aerzte: Wien, Austria, 1860; Volume 16, pp. 577–581. [Google Scholar]
- Wells, T. Diseases of the Ovaries. Their Diagnosis and Treatment; J & A Churchill: London, UK, 1872. [Google Scholar]
- Gusserow, A. Die Neubildungen des Uterus; [The Neoplasms of the Uterus]; Verlag von Ferdinand Enke: Stuttgart, Germany, 1886. [Google Scholar]
- Lockyer, C. Fibroids and Allied Tumours (Myoma and Adenomyoma); MacMillan: London, UK, 1918. [Google Scholar]
- Babeș, V. Über epitheliale Geschwulste in Uterusmyomem. [About epithelial tumors in uterine fibroids]. Allgem. Wiener. Med Ztschr. 1882, 27, 36–48. [Google Scholar]
- Diesterweg, B. Ein Fall von Cystofibrom uteri verum; [A case of cystofibroma uteri verum]. Zeitschr. Geburtshilfe. 1883, 9, 191–195. [Google Scholar]
- von Recklinghausen, F. Über Adenomyome des Uterus und der Tuba. [About the adenomyomas of the uterus and tube]. Wiener Klin. Wochenschr. 1895, 29, 530. [Google Scholar]
- von Recklinghausen, F. Die Adenomyomata und Cystadenomata der Uterus und Tubenwandung: Ihre Abkunft von Resten des Wolffischen Körpers; [The adenomyomas and cystadenomas of the uterus and tube wall: Their origin from remnants of the Wolffian body]; August Hirschwald Verlag: Berlin, Germany, 1896. [Google Scholar]
- Cullen, T. Adenomyoma of the round ligament. John’s Hopkins Hosp. Bull. 1896, 7, 112–117. [Google Scholar]
- Pick, L. Ein neuer Typus des voluminösen paroophoralen Adenomyoms—Zugleich über eine bisher nicht bekannte Geschwulst Form der Gebärmutter (Adenomyoma psammopapillare) und über totale Verdoppelung des Eileiters [A new type of voluminous paroophoral adenomyoma—At the same time about a previously unknown tumor form of the uterus (adenomyoma psammopapillare) and about total doubling of the fallopian tubes]. Archiv Gynäkol. 1897, 54, 117–206. [Google Scholar]
- Rolly, F. Über einen fall von adenomyoma uteri mit übergang in karcinom und metastasenbildung. [About a case of uterine adenomyoma with transition to carcinoma and metastasis]. Archiv Pathol. Anat. Physiol. Klin. Med. 1897, 150, 555–582. [Google Scholar] [CrossRef]
- Ivanoff, N.S. Drüsiges cystenhaltiges Uterusfibromyom compliciert durch Sarcom und Carcinom (Adenofibromyoma cysticum sarcomatodes carcinomatosum) [Uterine fibromyoma containing glandular cysts (Adenofibromyoma cysticum sarcomatodes carcinomatosum)]. Monatssch. Gebursthilfe Gynäkol. 1898, 7, 295–300. [Google Scholar]
- Cullen, T.S. Adenomyoma of the Uterus; Saunders: London, UK, 1908. [Google Scholar]
- Breus, C. Über Wahre epitel Fürende Cysten Bildung in Uterus Myomen; [Over the formation of true epithelial cysts in uterine myomas]; Franz Deuticke: Vienna, Austria, 1894. [Google Scholar]
- Schröder, O. Über Cystofibroide des Uterus Speciell Über Einen Fall von Intra-Uterinen Cystofibroid; [On the cystofibroids of the uterus]; Universitäts-Buchdrucker: Strasburg, France, 1873. [Google Scholar]
- Heer, O. Über Fibrocysten des Uterus; [Over the Cystic Fibroids of the uterus]; Druck von Zürcher und Furrer: Zürich, Switzerland, 1874. [Google Scholar]
- Grosskopf, C. Zur Kenntniss der Cystomyome des Uterus; [On knowledge of the cystomyomas of the uterus]; Druckerei der" Bayerischen Landeszeitung: Munich, Germany, 1884. [Google Scholar]
- Fritsch, H. Die Krankheiten der Frauen, fur Ärzte und Studirende; [The Diseases of Women, for Doctors and Students]; Verlag von Friedrich Werden: Berlin, Germany, 1892. [Google Scholar]
- Schröder, C. Das adenom des uterus [The adenoma of the uterus]. Ztschr. Geburtshilfe Gynäkol. 1877, 1, 189–219. [Google Scholar]
- Kolb, J.M. Pathologische Anatomie der weiblichen Sexualorgane; [Pathological Anatomy of the Female Sexual Organs]; Wilhelm Braumüller: Vienna, Austria, 1864. [Google Scholar]
- Röhrig, A. Erfahrungen über verlauf und prognose der uterusfibromyome [Experience with the course and prognosis of uterine fibromyomas]. Zeitschr. Geburtshilfe Gynäkol. 1880, 5, 265–316. [Google Scholar]
- Cullen, T.S. Adeno-Myome des Uterus [Uterine Adenomyomas]; Verlag von August Hirschwald: Berlin, Germany, 1903. [Google Scholar]
- von Lockstaedt, P. Über Vorkommen und Bedeutung von Drüsenschläuchen in den Myomen des Uterus [About the occurrence and importance of glandular tubes in the fibroids of the uterus]. Monatssch. Geburtshilfe Gynäkol. 1898, 7, 188–232. [Google Scholar]
- Kelly, H.A.; Cullen, T.S. Myomata of the Uterus; Saunders: London, UK, 1909. [Google Scholar]
- Kossman, R. Die Abstammung der Drüseneinschlüsse in der Uterus und der Tuben [The lineage of the glandular inclusions in the uterus and tubes]. Archiv Gynäkol. 1897, 54, 359–381. [Google Scholar]
- Meyer, R. Über eine adenomatose Wucherung der Serosa in einer Bauchnarde [On an adenomatous growth of the serosa around silk ligatures]. Zeitschr Gebursthilfe Gynäkol. 1903, 49, 32–41. [Google Scholar]
- Novak, E. Pelvic endometriosis. Spontaneous rupture of endometrial cysts, with a report of three cases. Am. J. Obstet. Gynecol. 1931, 22, 826–837. [Google Scholar] [CrossRef]
- von Franqué, O. Salpingitis nodosa isthmica und Adenomyoma tubae. Zeitschr Gebursthilfe Gynäkol. 1900, 42, 41–54. [Google Scholar]
- Baldy, J.M.; Longcope, W.T. Adenomyomata of the Uterus. Am. J. Obstet. Dis. Women Child. 1903, 45, 78–92. [Google Scholar]
- Schickele, G. Die lehre von den Mesonephrischen Geschülsten [The teaching of the Mesonephric Schools]. Zentralbl. Allg. Pathol. Anat. 1904, 15, 261–302. [Google Scholar]
- Meyer, R. Anatomie und histigenese der myome und fibrome [Anatomy and histogenesis of myoma and fibroma]. In Handbuch der Gynäkologie; von Verlag, J.F., Ed.; Bergmann: Weisbaden, Germany, 1907; pp. 413–486. [Google Scholar]
- Waldeyer, W. Eierstock und Ei. Ein Beitrag zur Anatomie und Entwicklungeschichte der Sexualorgane [Ovary and Egg. A Contribution to the Anatomy and Developmental History of the Sexual Organs]; Verlag von Wilhelm Engelmann: Leipzig, Germany, 1870. [Google Scholar]
- Marchand, J. Beiträge zur Kenntnis der Ovarialtumoren [Contributions to the Knowledge of Ovarian Tumors]. Habilitation Thesis, Habilitationsschrift, Halle, Germany, 1879. [Google Scholar]
- Williams, J.W. Papillomatous tumours of the ovary. Johns Hopkins Hosp. Rep. 1894, 3, 1–84. [Google Scholar]
- Frommel, R. Das Oberflächenpapillom des Eierstocks, seine Histogenese und, seine Stellung zum papillären Flimmerepithelcystom [The surface papilloma of the ovary, its histogenesis and its position in relation to the papillary ciliated epithelial cystoma]. Zeitschr Geburtsh Gynäkol. 1890, 19, 44–72. [Google Scholar]
- Bailey, K.V. The etiology, classification and life history of tumours of the ovary and other female pelvic organs containing aberrant Müllerian elements, with suggested nomenclature. J. Obstet. Gynaecol. Br. Emp. 1924, 31, 539–579. [Google Scholar] [CrossRef]
- Sampson, J.A. Inguinal endometriosis (often reported as endometrial tissue in the groin, adenomyoma in the groin, and adenomyoma of the round ligament). Am. J. Obstet. Gynecol. 1925, 10, 462–503. [Google Scholar] [CrossRef]
- Blair Bell, W. Endometrioma and Endometriomyoma of the Ovary. J. Obstet. Gynaecol. 1922, 29, 443–446. [Google Scholar] [CrossRef] [Green Version]
- Frankl, O. Adenomyosis uteri. Am. J. Obstet. Gynecol. 1925, 10, 680–684. [Google Scholar] [CrossRef]
- Emge, L.A. The elusive adenomyosis of the uterus. Its historical past and its present state of recognition. Am. J. Obstet. Gynecol. 1962, 83, 1541–1563. [Google Scholar] [CrossRef]
- Sampson, J.A. Metastatic or embolic endometriosis, due to the menstrual dissemination of endometrial tissue into the venous circulation. Am. J. Pathol. 1927, 3, 93–109. [Google Scholar] [PubMed]
- Halban, J. Zur Diagnose der Adenomyosis und der Adenomyome der Gebärmutter [Towards diagnosing adenomyosis and adenomyomas of the uterus]. Zentralbl. Gynäkol. 1933, 57, 961–963. [Google Scholar]
- Taussig, F.S. A study of the lymph glands in cancer of the cervix and cancer of the vulva. Am. J. Obstet. Gynecol. 1938, 36, 819–832. [Google Scholar] [CrossRef]
- Bird, C.C.; McElin, T.W.; Manalo-Estrella, P. The elusive adenomyosis of the uterus—Revisited. Am. J. Obstet. Gynecol. 1972, 112, 583–593. [Google Scholar] [CrossRef]
- Hricak, H.; Alpers, C.; Crooks, L.E.; Sheldon, P.E. Magnetic resonance imaging of the female pelvis: Initial experience. Am. J. Roentgenol. 1983, 141, 1119–1128. [Google Scholar] [CrossRef]
- Tamai, K.; Togashi, K.; Ito, T.; Morisawa, N.; Fujiwara, T.; Koyama, T. MR imaging findings of adenomyosis: Correlation with histopathologic features and diagnostic pitfalls. Radiographics 2005, 25, 21–40. [Google Scholar] [CrossRef]
- Habiba, M.; Gordts, S.; Bazot, M.; Brosens, I.; Benagiano, G. Exploring challenges for a new classification of adenomyosis. Reprod. BioMed Online 2020, 40, 569–581. [Google Scholar] [CrossRef]
- Sampson, J.A. Peritoneal endometriosis due to menstrual dissemination of endometrial tissue into the peritoneal cavity. Am. J. Obstet. Gynecol. 1927, 14, 422–469. [Google Scholar] [CrossRef]
- Batt, R.E. A History of Endometriosis; Springer: Brelin/Heidelberg, Germany, 2011. [Google Scholar]
- Batt, R.E. The history of endometriosis (commentary). Gynecol. Obstet Invest. 2014, 78, 10–11. [Google Scholar] [CrossRef] [PubMed]
- Russell, W.W. Aberrant portions of the Müllerian duct found in an ovary. Johns Hopkins Hosp. Bull. 1899, 10, 8–10. [Google Scholar] [CrossRef]
- Semmelink, H.B.; De Josselin de Jong, R. Beitrag mit Kenntnis der Adenomyome des Weiblichen genitalapparates [Contributon to the knowledge of adenomyoma]. Monatsschr. Geburtshilfe Gynäkol. 1905, 22, 234–251. [Google Scholar]
- Sitzenfrei, A. Das Übergreifen der Adenomyome des Uterus auf den Mastdarm. Zugleich ein Beitrag zur Klinik und Histogenese der Adenomyositis uteri et recti und des adenomyoma recti [The spread of adenomyomas of the uterus onto the rectum. At the same time a contribution to the clinical picture and histogenesis of adenomyositis uteri et recti and adenomyoma recti]. Zeitschr Geburst Gynäkol. 1909, 64, 538–580. [Google Scholar]
- Savage, S. Haematoma of the ovary and its pathological connections with the ripening and the retrogression of the Graafian follicle. Br. Gynaecol. J. 1906, 21, 285–305. [Google Scholar]
- Casler, D.B. A unique, diffuse uterine tumor, really an adenomyoma, with stróma, but no glands. Menstruation after complete hysterectomy due to uterine mucosa remaining in the ovary. Trans Am. Gynecol. Soc. 1919, 44, 69–84. [Google Scholar]
- Smith, R.R. Hemorrhage into the pelvic cavity other that of ectopic pregnancy. Am. J. Obstet. Gynaecol. 1920, 1, 240–242. [Google Scholar] [CrossRef] [Green Version]
- Norris, C.C. Ovary containing endometrium. Am. J. Obstet. Gynecol. 1921, 1, 831–834. [Google Scholar]
- Donald, A. The Clinical Aspects of Adenomyomata of the Female Pelvic Organs. Proc. R. Soc. Med. 1923, 16, 82–92. [Google Scholar] [CrossRef] [Green Version]
- Pick, L. Über neubildungen am genitale bei zwittern, nebst Beiträgen zur Lehre von den adenomen des hodens und eierstockes [About new formations on the genitals in hermaphrodites, as well as contributions to the theory of adenomas of the testicle and ovary]. Arch. Gynäkol. 1905, 76, 191–281. [Google Scholar] [CrossRef]
- Sampson, J.A. Perforating hemorrhagic (chocolate) cysts of the ovary. Arch. Surg. 1921, 3, 245–323. [Google Scholar] [CrossRef] [Green Version]
- Sampson, J.A. The life history of ovarian hematomas (hemorrhagic cysts) of endometrial (Müllerian) type. Arch. Surg. 1922, 5, 217–280. [Google Scholar] [CrossRef] [Green Version]
- Schultze, B.S. Über die pathologische anteflexion der gebärmutter und die parametritis posterior [About the pathological anteflexion of the uterus and the parametritis posterior]. Arch. Gynäkol. 1875, 8, 134–180. [Google Scholar] [CrossRef]
- Schultze, B.S. Pathologie und Therapie der Lageveränderungen der Gebärmutter; [Pathology and Therapy of Changes in the Position of the Uterus]; Verlag von august Hirschwald: Berlin, Germany, 1881. [Google Scholar]
- Meyer, R. Über entzündliche heterotope Epithelwucherungen im weiblichen Genitalgebiete und über eine bis in die Wurzel des Mesocolon ausgedehnte benigne Wucherung des Darmepithels [About inflammatory heterotopic epithelial growths in the female genital tract and a benign growth of the intestinal epithelium extending to the root of the mesocolon]. Virchows. Arch. 1909, 195, 487–537. [Google Scholar]
- Eden, T.W.; Lockyer, C. Gynaecology for Student and Practitioners; New York, The Macmillan Company: New York, NY, USA, 1916. [Google Scholar]
- Kleinhans, T. Beitrag zur Lehre von den adenomyomen des weiblichen Genitaltraktus [Contribution to the study of adenomyomas of the female genital trac]. Z. Geburtshilfe Gynäkol. 1904, 52, 266–287. [Google Scholar]
- Lockyer, C. Adenomyoma of the recto-uterine and recto-vaginal septa. Proc. R. Soc. Med. 1913, 6, 112–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pfannenstiel, H.J. Über die Adenomyome des Genitalstranges [About the adenomyomas of the genital tract]. Verhandl Deutsch Gesellsch. Gynäkol. 1897, 7, 195–199. [Google Scholar]
- von Herff, O. Über cystomyome und adenomyome der scheide [About cystomyomas and adenomyomas of the vagina]. Verh. Dtsch. Gesellsch Gynäkol 1897, 7, 189–195. [Google Scholar]
- Pick, L. Die Adenomyome der leistengegend und des hinteren scheidengewölbes, ihre Stellung zu den paroophoralen adenomyomen der Uterus- und tubenwandung v. Recklinghausen’s [The adenomyomas of the inguinal region and the posterior vaginal vault, their position in relation to the paroophoral adenomyomas of the uterine and tube wall of von Recklinghausen’s]. Arch Gynäkol. 1899, 57, 461–509. [Google Scholar]
- Meckel, J.F. Handbuch der Pathologischen Anatomie; [Handbook of Pathological Anatomy]; Carl Heinrich Reclam: Leipzig, Germany, 1818. [Google Scholar]
- Rokitansky, C. Lehrbuch der Pathologischen Anatomie; [Textbook of Pathological anatomy]; Wilhelm Braumüller: Vienna, Austria, 1861. [Google Scholar]
- Förster, A. Handbuch der Speciellen Pathologischen Anatomie; [Handbook of Special Pathological Anatomy]; Leopold Voss: Leipzig, Austria, 1854. [Google Scholar]
- Kelbs, E. Handbuch der Pathologishen Anatomie; [Handbook of pathological anatomy]; Verlag von August Hirschwald: Berlin, Germany, 1876. [Google Scholar]
- Chiari, H. Zur pathologischen anatomie des Eileitercatarrhs [On the pathological anatomy of fallopian tube secretions]. Pager Zeitschrift Heilkunde 1887, 8, 457–464. [Google Scholar]
- Meyer, R. Über adenomatöse schleimhautwucherungen in der uterus- und tubenwand und ihre pathologisch-anatomische bedeutung [About adenomatous mucous membrane growths in the uterus and tube walls and their pathological-anatomical significance]. Virchows Arch. 1903, 172, 394–409. [Google Scholar] [CrossRef]
- Rabinovitz, M. The pathogenesis of adenomyosalpingitis (salpingitis nodosa). Report of ten cases. Am. J. Obstet. Dis. Women Child. 1917, 76, 711–752. [Google Scholar]
- Habiba, M.; Brosens, I.; Benagiano, G. Müllerianosis, Endocervicosis, and Endosalpingiosis of the Urinary Tract: A Literature Review. Reprod. Sci. 2018, 12, 1607–1618. [Google Scholar] [CrossRef] [PubMed]
- Oliver, J. An accessory uterus distended with menstrual fluid enucleated from the substance of the right broad ligament. Lancet 1912, 179, 1609. [Google Scholar] [CrossRef]
- Cranstoun, G. Cystic Adenomyoma of Uterus. Proc. R. Soc. Med. 1922, 15, 8–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peterson, C.J.; Strickler, J.G.; Gonzalez, R.; Dehner, L.P. Uterus-like mass of the small intestine. Heterotopia or monodermal teratoma? Am. J. Surg. Pathol. 1990, 14, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Rougier, A.; Vital, C.; Caillaud, P. Uterus-like mass of the conus medullaris with associated tethered cord. Neurosurgery. 1993, 33, 328–331. [Google Scholar] [CrossRef] [PubMed]
- McDougal, R.A.; Roth, L.M. Ovarian adenomyoma associated with an endometriotic cyst. South Med. J. 1986, 79, 640–642. [Google Scholar] [CrossRef]
- Sisodia, S.M.; Khan, W.A.; Goel, A. Ovarian ligament adenomyoma: Report of a rare entity with review of the literature. J. Obstet. Gynaecol. Res. 2012, 38, 724–728. [Google Scholar] [CrossRef]
- Torres, D.; Parker, L.; Moghadamfalahi, M.; Sanders, M.A.; Metzinger, D.S. Clear cell adenocarcinoma arising in an adenomyoma of the broad ligament. Int. J. Surg. Pathol. 2015, 23, 140–143. [Google Scholar] [CrossRef]
- Ulm, M.A.; Robins, D.B.; Thorpe, E.M.; Reed, M.E. Endometrioid adenocarcinoma in an extrauterine adenomyoma. Obstet Gynecol. 2014, 124, 445–448. [Google Scholar] [CrossRef] [PubMed]
- Clement, P.B.; Young, R.H. Endocervicosis of the urinary bladder: A report of six cases of a benign mullerian lesion that may mimic adenocarcinoma. Am. J. Surg. Pathol. 1992, 16, 533–542. [Google Scholar] [CrossRef]
- Batt, R.E.; Yeh, J. Müllerianosis: Four developmental (embryonic) mullerian diseases. Reprod. Sci. 2013, 20, 1030–1037. [Google Scholar] [CrossRef]
- Signorile, P.G.; Baldi, F.; Bussani, R.; D’Armiento, M.; de Falco, M.; Baldi, A. Ectopic endometrium in human foetuses is a common event and sustains the theory of müllerianosis in the pathogenesis of endometriosis, a disease that predisposes to cancer. J. Exp. Clin. Cancer Res. 2009, 28, 49–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sampson, J.A. Postsalpingectomy endometriosis (endosalpingiosis). Am. J. Obstet. Gynecol. 1930, 20, 443–480. [Google Scholar] [CrossRef]
- Gallan, A.J.; Antic, T. Benign Müllerian glandular inclusions in men undergoing pelvic lymph node dissection. Hum. Pathol. 2016, 57, 136–139. [Google Scholar] [CrossRef]
- Yang, M.; Lia, Y.; Chen, M.; Chen, J.; Kung, F.T. Uterine endosalpingiosis: Case report and review of the literature. Taiwan, J. Obstet. Gynecol. 2019, 58, 324–327. [Google Scholar] [CrossRef] [PubMed]
- Campenot, J.F.; Grice, G.; Auge, B.; Michael Quigley, M. Pathologic quiz case: A woman with chronic pelvic pain. Endocervicosis. Arch. Pathol. Lab. Med. 2005, 129, e109–e110. [Google Scholar] [CrossRef]
- Heretis, J.; Stamatiou, K.; Papadimitriou, V.; Giannikaki, E.; Stathopoulos, E.; Sofras, F. Endocervicosis of the bladder: Report of a case and review of the current literature. Int. J. Clin. Exp. Pathol. 2009, 2, 91–94. [Google Scholar]
- Cheah, P.L.; Looi, L.M.; Lee, G.E.; Teoh, K.H.; Mun, K.S.; Nazarina, A.R. Unusual finding of endocervical-like mucinous epithelium in continuity with urothelium in endocervicosis of the urinary bladder. Diagn. Pathol. 2011, 23, 6–56. [Google Scholar] [CrossRef] [Green Version]
| Author | Landmark Contribution |
|---|---|
| Marcello Malpighi | 17th century introduction of microscopy to biology |
| Caspar Friedrich Wolff | 1774 thesis “Theoria Generationis” considered the father of embryology |
| Johannes Peter Müller | 1830 described the early stages of the formation of female internal genital organs von Lockstaedt P |
| Daniel Schrön | 1690 perhaps an early description of endometriosis |
| Joannes Fridericus Crellius | 1739 perhaps an early description of endometriotic cyst |
| Carl Rokitansky | 1849 reference to a chocolate-containing cyst of the ovary 1860 described neoformation of mucosal tissue in the uterus |
| Babeș (Victor Babesiu) | 1882 perhaps the first description of a fibroid containing epithelium |
| Carl Breus | 1894 refers to the distinction between cystic lesions based on the presence or absence of mucosal lining |
| Paul von Lockstaedt | 1898 describes glands within fibroids |
| Cuthbert Lockyer | 1913 describes adenomyoma of the rectovaginal septum 1918 critical publication on myoma and adenomyoma |
| Friedrich von Recklinghausen | 1895, 1896 Important contribution advocation Wolffian theory |
| Robert Meyer | 1903, 1907, 1909 Important contributions: aberrant glands develop in response to a sequence of inflammation, induration and epithelial hypertrophy |
| Thomas Cullen | 1895 presented his first case of adenomyoma 1903, 1908, 1919, 1920 critical publications in the field advocates mucosal origin |
| Kenneth Vernon Bailey | 1924 description of ovarian lesions |
| Oskar Frankl | 1925 advocates ‘adenomyosis’ for uterine lesions |
| John Alberton Sampson | Advocates ‘endometriosis’ 1921, 1925, 1927 important contributions to the study of endometriosis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Habiba, M.; Lippi, D.; Benagiano, G. The History of the Discovery of Ectopic Epithelial Cells in Lower Peritoneal Organs: The So-Called Mucosal Invasion. Reprod. Med. 2021, 2, 68-84. https://doi.org/10.3390/reprodmed2020008
Habiba M, Lippi D, Benagiano G. The History of the Discovery of Ectopic Epithelial Cells in Lower Peritoneal Organs: The So-Called Mucosal Invasion. Reproductive Medicine. 2021; 2(2):68-84. https://doi.org/10.3390/reprodmed2020008
Chicago/Turabian StyleHabiba, Marwan, Donatella Lippi, and Giuseppe Benagiano. 2021. "The History of the Discovery of Ectopic Epithelial Cells in Lower Peritoneal Organs: The So-Called Mucosal Invasion" Reproductive Medicine 2, no. 2: 68-84. https://doi.org/10.3390/reprodmed2020008
APA StyleHabiba, M., Lippi, D., & Benagiano, G. (2021). The History of the Discovery of Ectopic Epithelial Cells in Lower Peritoneal Organs: The So-Called Mucosal Invasion. Reproductive Medicine, 2(2), 68-84. https://doi.org/10.3390/reprodmed2020008







