Abstract
Acute rhinosinusitis in children is typically caused by viral or bacterial infections. However, methicillin-resistant Staphylococcus aureus (MRSA) is increasingly linked to recurrence and severe complications, including orbital involvement. We present a case of a 6-year-old boy with periorbital swelling, proptosis, and fever following upper respiratory symptoms. Imaging revealed pansinusitis with a subperiosteal orbital abscess. He was treated empirically with intravenous ceftriaxone and metronidazole, followed by endoscopic sinus surgery. Intraoperative cultures confirmed MRSA, leading to a switch to vancomycin. The patient recovered fully without complications. This case illustrates the clinical challenges posed by MRSA sinusitis and emphasises its public health implications. Integrating antimicrobial stewardship, promoting community hygiene, ensuring early diagnostics and healthcare access, and enhancing epidemiological surveillance can play a pivotal role in reducing the burden of MRSA-related complications in children.
1. Introduction
Acute rhinosinusitis (ARS) is prevalent in pediatric populations, typically resolving without major issues [1]. However, serious complications such as orbital or intracranial infections can arise despite appropriate antibiotic therapy. The microbiological etiology of acute rhinosinusitis has been extensively studied, identifying Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis as the predominant pathogens globally [1]. Recently, there has been a notable increase in methicillin-resistant Staphylococcus aureus (MRSA) associated with acute and chronic sinusitis [2]. This article presents a case of community-acquired MRSA sinusitis in a 6-year-old boy, complicated by a subperiosteal orbital abscess (SPOA).
2. Case Presentation
A 6-year-old boy with no significant medical history was referred to our facility due to left eye swelling and pain that had persisted for four days, following a day of rubbing his left eye (Figure 1). He also exhibited fever, upper respiratory tract infection symptoms, and lethargy for one week prior to admission. Before arriving at our hospital, he had received treatment at a private clinic, where he was prescribed oral antibiotics. He did not report any double vision, blurred vision, impaired color vision, or other symptoms indicative of intracranial involvement. The patient underwent a formal ophthalmologic assessment, which revealed normal intraocular pressures of 19 mmHg in the right eye and 20 mmHg in the left eye. Visual acuity using Snellen chart was recorded as 3/3 for distance and N5 for near vision in both eyes.

Figure 1.
Initial presentation with proptosis of the left eye, periorbital swelling, erythema.
Upon examination, the patient appeared lethargic, with proptosis of the left eye, periorbital swelling, erythema, and restricted eye movement. The pupils were bilaterally reactive. A mucopurulent discharge was observed coming from his left nostril (Figure 2). A high-resolution CT scan revealed a complete opacification of the left ethmoidal, maxillary, and sphenoidal sinuses, with rim enhancement seen within. A soft tissue density is present in the left nasal cavity with obliteration of the osteomeatal complex. There was associated erosion of the left lamina papyracea. Fat stranding is seen involving the left medial extraconal space with a rim enhancing collection located at the left subperiosteal region. This causes lateral displacement of the medial rectus muscle (Figure 3). A diagnosis of acute bacterial sinusitis with a subperiosteal abscess was established. He was initiated on intravenous ceftriaxone and metronidazole.
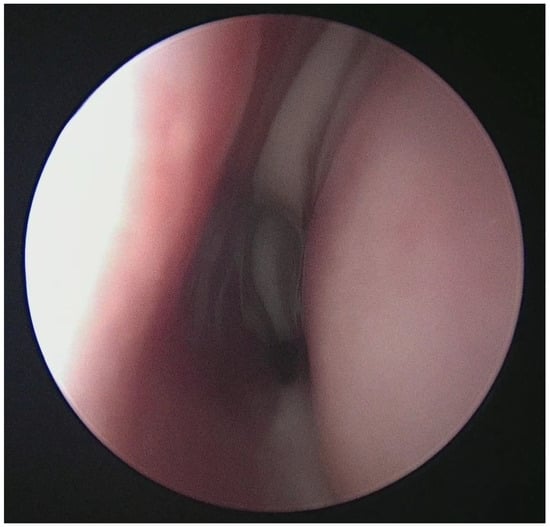
Figure 2.
Mucopurulent discharge in nasal cavity upon nasoendoscopic examination.
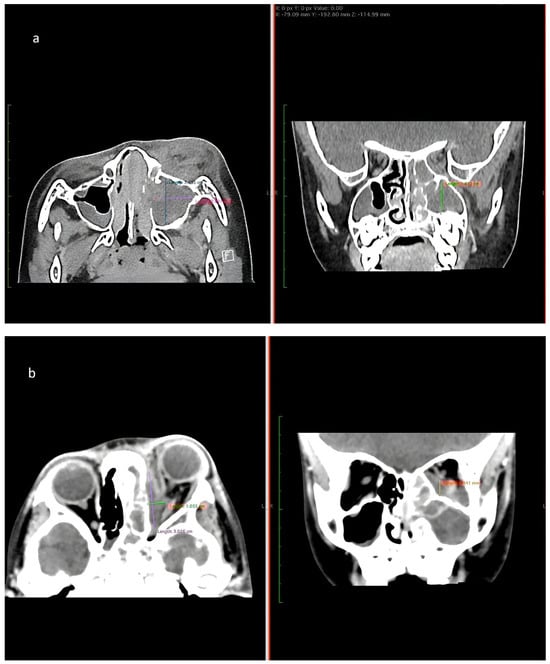
Figure 3.
(a) CT of paranasal sinus shows intrasinus collection collectively measures approximately 2.5 cm × 2.0 cm × 1.9 cm (Anteroposterior × Width × Craniocaudal). (b) CT image shows rim-enhancing collection at the left subperiosteal region measuring 3.0 cm × 1.0 cm × 1.8 cm (Anteroposterior × Width × Craniocaudal).
The following day, he underwent endoscopic sinus surgery with drainage of subperiosteal abscess under general anesthesia. Intraoperatively, pus was observed in the left maxillary sinus and subperiosteal area (Figure 4). Postoperatively, his general condition improved; however, tissue and pus cultures obtained from the left maxillary sinus subsequently grew methicillin-resistant Staphylococcus aureus (MRSA). In response, his antibiotic regimen was adjusted to intravenous vancomycin, as recommended by the infectious disease specialist.
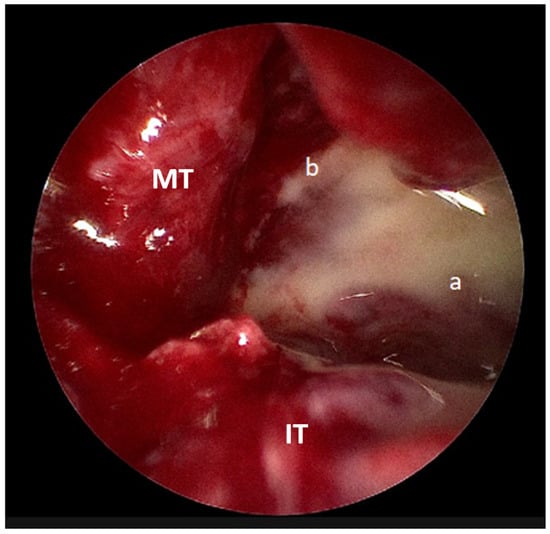
Figure 4.
Intraoperative endoscopic picture showing pus draining from the (a) maxillary sinus and (b) subperiosteal region (IT: inferior turbinate, MT: middle turbinate).
The patient’s eye condition improved significantly following the drainage of pus. After two weeks of intravenous vancomycin therapy, he was discharged home with a prescription for oral trimethoprim-sulfamethoxazole (Bactrim) 80 mg twice daily for two weeks. At a follow-up appointment two weeks post-discharge, the patient had made a complete recovery without any complications.
3. Discussion
Sinusitis, defined as the inflammation of the mucosal lining of one or more paranasal sinuses, can be categorized based on the duration of clinical symptoms into three types: acute (less than 30 days), subacute (30 to 90 days), and chronic (more than 90 days) [3]. Acute sinusitis may be caused by viral, bacterial, or fungal infections, as well as by environmental irritants and allergies [3]. Common pathogens in the pediatrics population globally associated with this condition include Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Streptococcus pyogenes and Staphylococcus aureus [3]. Emerging data from regions such as Japan and Taiwan indicate MRSA prevalence rates as high as 15.6–25.0% among S. aureus isolates in otolaryngologic infections [4]. These findings reflect microbial trends and underlying public health determinants, such as antibiotic prescribing practices, infection control measures, and regional differences in surveillance. Inadequate empirical coverage for MRSA can delay effective treatment, potentially leading to life-threatening complications, including orbital or intracranial spreads as demonstrated in this case [5,6].
A retrospective cohort study conducted at a tertiary care children’s hospital analyzed data from pediatric patients diagnosed with complicated ARS [6]. The findings indicated that among the 89 children examined, all bacterial isolates identified were MRSA. Additional studies have similarly reported cases of MRSA-associated sinusitis; in these cases, patients were administered antibiotics, albeit not specifically tailored to the identified organism. Notably, the resolution of sinusitis was achieved through the combined approach of antibiotic therapy and surgical intervention. These findings, which are summarized in Table 1, highlight the clinical importance of MRSA in pediatric sinusitis and emphasize the necessity for appropriate antibiotic coverage alongside surgical management to effectively address these infections.

Table 1.
Literature review of article for MRSA sinusitis.
From a public health perspective, this case highlights several issues. First, the early and accurate identification of resistant pathogens remains critical, especially in pediatric populations, where signs may be subtle and rapid progression. Although usually self-limiting, it is essential to recognize the potential for acute MRSA sinusitis to lead to serious complications, considering the significant risk of morbidity and mortality linked with such complications [9]. Antibiotics are a primary treatment for bacterial sinusitis, with empirical regimens such as amoxicillin-clavulanate or cephalosporins typically administered prior to obtaining culture and sensitivity results [10]. The initial antibiotic treatment for acute sinusitis is unlikely to target MRSA. Hence, the risk of morbidity may be significantly heightened in these cases. Systemic antibiotic therapy with vancomycin remains a cornerstone for treating serious MRSA infections in children, including sinusitis, due to its efficacy against MRSA strains [11].
The role of screening for MRSA in sinusitis is not well established. However, the benefits of MRSA nasal screening have been explored and it is primarily used to predict MRSA infections in other respiratory tract infections. It has demonstrated a high negative predictive value (NPV), allowing for the de-escalation of empirical anti-MRSA therapy when the screening result is negative [12]. In this instance, the patient first received intravenous ceftriaxone and was later switched to vancomycin based on tissue culture results. The recommended duration of antibiotic therapy ranges from 7 to 14 days but may be adjusted based on the patient’s clinical condition [3]. In hospitalized children with complicated MRSA infections, intravenous vancomycin remains the recommended first line therapy. A total treatment duration of 7 to 14 days is generally effective; however, in cases requiring prolonged therapy, an initial course of intravenous antibiotics followed by oral agents may be considered. This approach should be individualized based on the patient’s clinical response [13].
Second, the rise in complicated sinus infections caused by MRSA reflects the broader challenge of antimicrobial resistance (AMR), a global public health priority. Orbital infections are a rare complication of acute sinusitis in the pediatric population. Several risk factors have been identified that increase the likelihood of developing orbital complications, including older age, clinical signs such as proptosis and fever, ethmoid sinus involvement, a shorter duration of symptoms, and the presence of MRSA or anaerobic bacteria [1,14]. One significant risk factor is the age of the child. Studies have shown that children older than 5 years are more likely to present with severe orbital complications and may require surgical intervention despite having received pre-hospital antibiotics [15]. This case exemplifies the limitations of standard empiric antibiotic regimens in the face of evolving resistance patterns. It reinforces the need for enhanced local epidemiological data to inform clinical guidelines and optimize empirical therapy.
Third, the case underscores the importance of timely access to specialized care and diagnostic imaging. For children presenting with periorbital cellulitis, it is essential to rule out infections from adjacent paranasal sinuses using a contrast-enhanced CT (CECT) scan, even without ear, nose, and throat symptoms. The most widely accepted classification system for orbital complications is that of Chandler et al. Subperiosteal orbital abscesses (SPOA) classified as Chandler grade 3 typically present as a pus collection in the space between the periorbita and the lamina papyracea adjacent to the infected paranasal sinuses [2]. Though rare, SPOA can progress rapidly, leading to potential permanent visual impairment [15].
Hence, the importance of timely drainage of MRSA abscesses and their outcomes is highly dependent on early surgical intervention. The incidence of MRSA SPOA has been rising and is associated with a higher incidence of orbital complications compared to infections caused by other organisms [6,16]. This may suggest that MRSA-related infections exhibit a more aggressive clinical course compared to infections caused by other microorganisms, although definitive evidence is currently lacking. Therefore, further research is warranted to elucidate the pathogenicity and clinical outcomes associated with MRSA infections.
Finally, in parallel with effective treatment, preventing MRSA sinusitis in the pediatric population is critical in reducing disease burden and healthcare utilization. Preventive strategies involve a multiple approach centered on household-level hygiene, community-level prevention strategies and environmental control. Regular handwashing with soap and water is fundamental, while the use of antibacterial soap may further reduce MRSA colonization among household members. Avoiding the sharing of personal items such as towels, ointments, and lotions also helps prevent cross-transmission. Daily bathing has been associated with a lower risk of colonization [17]. Environmental hygiene is equally important, with routine cleaning of frequently touched surfaces serving to limit household contamination.
In relation to healthcare settings, rigorous cleaning and disinfection of patient rooms and medical equipment should be consistently practiced. Additionally, strict contact precautions should be implemented when caring for patients colonized or infected with MRSA to prevent cross-transmission. For children identified as MRSA carriers, decolonization protocols using intranasal mupirocin and antiseptic body washes like chlorhexidine have shown efficacy in reducing colonization and subsequent infection risk [17,18]. Effective prevention of MRSA transmission within healthcare facilities requires a structured, multitiered strategy. Institutions should begin by establishing MRSA prevention as a critical organizational priority. This includes the routine assessment of infection data to guide tailored interventions, the implementation of targeted control measures, and the continuous evaluation of outcomes to monitor their effectiveness. Patient education is also crucial; clinicians should advise patients on methods to reduce transmission risk and maintain personal hygiene. In daily practice, healthcare workers must perform meticulous hand hygiene with soap and water or alcohol-based hand sanitizers before and after each patient encounter. Incorporating these preventive strategies into household, healthcare facilities, and community practices may significantly reduce the incidence of MRSA-related complications in pediatric sinusitis [13].
Summarized in Table 2 are the key takeaways derived from this case and relevant literature. These points serve as practical guidance for clinicians managing similar cases and emphasize important considerations in diagnosis, treatment, and prevention [13,17,18].

Table 2.
Key Clinical Takeaways for MRSA-Associated Complicated Infections in Pediatric Patients.
4. Conclusions
This case not only illustrates the growing clinical relevance of MRSA in pediatric sinusitis and its potential to cause severe complications but also emphasizes its public health implications. Prompt recognition, timely surgical intervention, and targeted antibiotic therapy, particularly with agents effective against MRSA, are critical for favorable outcomes. Given the rising incidence of community-acquired MRSA, especially in regions with high prevalence, incorporating MRSA coverage into empirical treatment regimens for complicated sinusitis may be warranted. Moreover, preventive strategies focusing on hygiene, environmental sanitation, and decolonization in at-risk children should be emphasized as part of broader public health efforts to mitigate MRSA transmission and its complications.
Author Contributions
Conceptualization, A.F.J. and F.S.R.; methodology, A.F.J. and F.S.R.; resources, A.F.J., F.S.R. and F.D.Z.; writing—original draft preparation, F.S.R.; writing—review and editing, A.F.J.; visualization, F.S.R.; supervision, A.F.J. and F.D.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
In line with institutional policy at the authors’ institutions, single case reports that do not involve a clinical trial or systematic research are exempt from institutional review board (IRB) oversight. Therefore, ethical approval was not required for this case report.
Informed Consent Statement
Written informed consent has been obtained from the patient’s parent (legal guardian) to publish this paper.
Data Availability Statement
The data supporting the findings of this case report are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MRSA | methicillin-resistant Staphylococcus aureus |
| AMR | antimicrobial resistance |
| SPOA | subperiosteal orbital abscesses |
| ARS | Acute rhinosinusitis |
References
- Nocon, C.C.; Baroody, F.M. Acute rhinosinusitis in children. Curr. Allergy Asthma Rep. 2014, 14, 443. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Huo, J.; Liu, C.; Fu, Y.; Li, J. Infantile orbital abscess caused by methicillin-resistant Staphylococcus aureus: A case report and literature review. Front. Pediatr. 2023, 11, 1272852. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.K.; Hon, K.L.; Chu, W.C. Acute bacterial sinusitis in children: An updated review. Drugs Context 2020, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.H.; Hung, P.K. Methicillin-resistant Staphylococcus aureus infections in acute rhinosinusitis. Laryngoscope 2006, 116, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Liao, S.; Durand, M.L.; Cunningham, M.J. Sinogenic orbital and subperiosteal abscesses: Microbiology and methicillin-resistant Staphylococcus aureus incidence. Otolaryngol. Head Neck Surg. 2010, 143, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Mulvey, C.L.; Kiell, E.P.; Rizzi, M.D.; Buzi, A. The Microbiology of Complicated Acute Sinusitis among Pediatric Patients: A Case Series. Otolaryngol. Head Neck Surg. 2019, 160, 712–719. [Google Scholar] [CrossRef] [PubMed]
- Whitby, C.R.; Kaplan, S.L.; Mason, E.O., Jr.; Carrillo-Marquez, M.; Lamberth, L.B.; Hammerman, W.A.; Hultén, K.G. Staphylococcus aureus sinus infections in children. Int. J. Pediatr. Otorhinolaryngol. 2011, 75, 118–121. [Google Scholar] [CrossRef] [PubMed]
- Hamill, C.S.; Sykes, K.J.; Harrison, C.J.; Weatherly, R.A. Infection rates of MRSA in complicated pediatric rhinosinusitis: An up to date review. Int. J. Pediatr. Otorhinolaryngol. 2018, 104, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.S.; Cunnion, K.M. Acute MRSA sinusitis with intracranial extension and marginal vancomycin susceptibility. Case Rep. Pediatr. 2013, 2013, 153239. [Google Scholar] [CrossRef]
- Richards, N.; Tiedeken, S.D.; Chang, C.C. Medical Management of Acute Rhinosinusitis in Children and Adults. In Diseases of the Sinuses: A Comprehensive Textbook of Diagnosis and Treatment; Springer: New York, NY, USA, 2013; pp. 359–371. [Google Scholar]
- Avedissian, S.N.; Rhodes, N.J.; Shaffer, C.L.; Tran, L.; Bradley, J.S.; Le, J. Antimicrobial Prescribing for Treatment of Serious Infections Caused by Staphylococcus aureus and Methicillin-Resistant Staphylococcus aureus in Pediatrics: An Expert Review. Expert Rev. Anti-Infect. Ther. 2021, 19, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.L.; Daley, M.J.; Givens Merkel, K.; Rose, D.T. Clinical Utility of Methicillin-Resistant Staphylococcus aureus Nasal Screening for Antimicrobial Stewardship: A Review of Current Literature. Pharmacotherapy 2018, 38, 1216–1228. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Bayer, A.; Cosgrove, S.E.; Daum, R.S.; Fridkin, S.K.; Gorwitz, R.J.; Kaplan, S.L.; Karchmer, A.W.; Levine, D.P.; Murray, B.E.; et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin. Infect. Dis. 2011, 52, e18–e55, Erratum in Clin. Infect. Dis. 2011, 53, 319. [Google Scholar] [CrossRef] [PubMed]
- Trivić, A.; Cevik, M.; Folić, M.; Krejovic-Trivić, S.; Rubino, S.; Micić, J.; Stevanović, G.; Milovanović, J.; Jotić, A.; Barać, A. Management of Orbital Complications of Acute Rhinosinusitis in Pediatric Patients: A 15-Year Single-Center Experience. Pediatr. Infect. Dis. J. 2019, 38, 994–998. [Google Scholar] [CrossRef] [PubMed]
- Soon, V.T. Pediatric subperiosteal orbital abscess secondary to acute sinusitis: A 5-year review. Am. J. Otolaryngol. 2011, 32, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Ang, T.; Cameron, C.; Tong, J.Y.; Wilcsek, G.; Tan, J.; Patel, S.; Selva, D. Methicillin-resistant Staphylococcus aureus-associated orbital cellulitis: A case series. Int. Ophthalmol. 2023, 43, 2925–2933. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Humphreys, H.; Grundmann, H.; Skov, R.; Lucet, J.C.; Cauda, R. Prevention and control of methicillin-resistant Staphylococcus aureus. Clin. Microbiol. Infect. 2009, 15, 120–124. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kao, C.M.; Fritz, S.A. Infection prevention-how can we prevent transmission of community-onset methicillin-resistant Staphylococcus aureus? Clin. Microbiol. Infect. 2025, 31, 166–172. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).