Cholesterol Granuloma of the Frontal Sinus Complicated by Mycetoma: A Rare Case Report
Abstract
1. Introduction
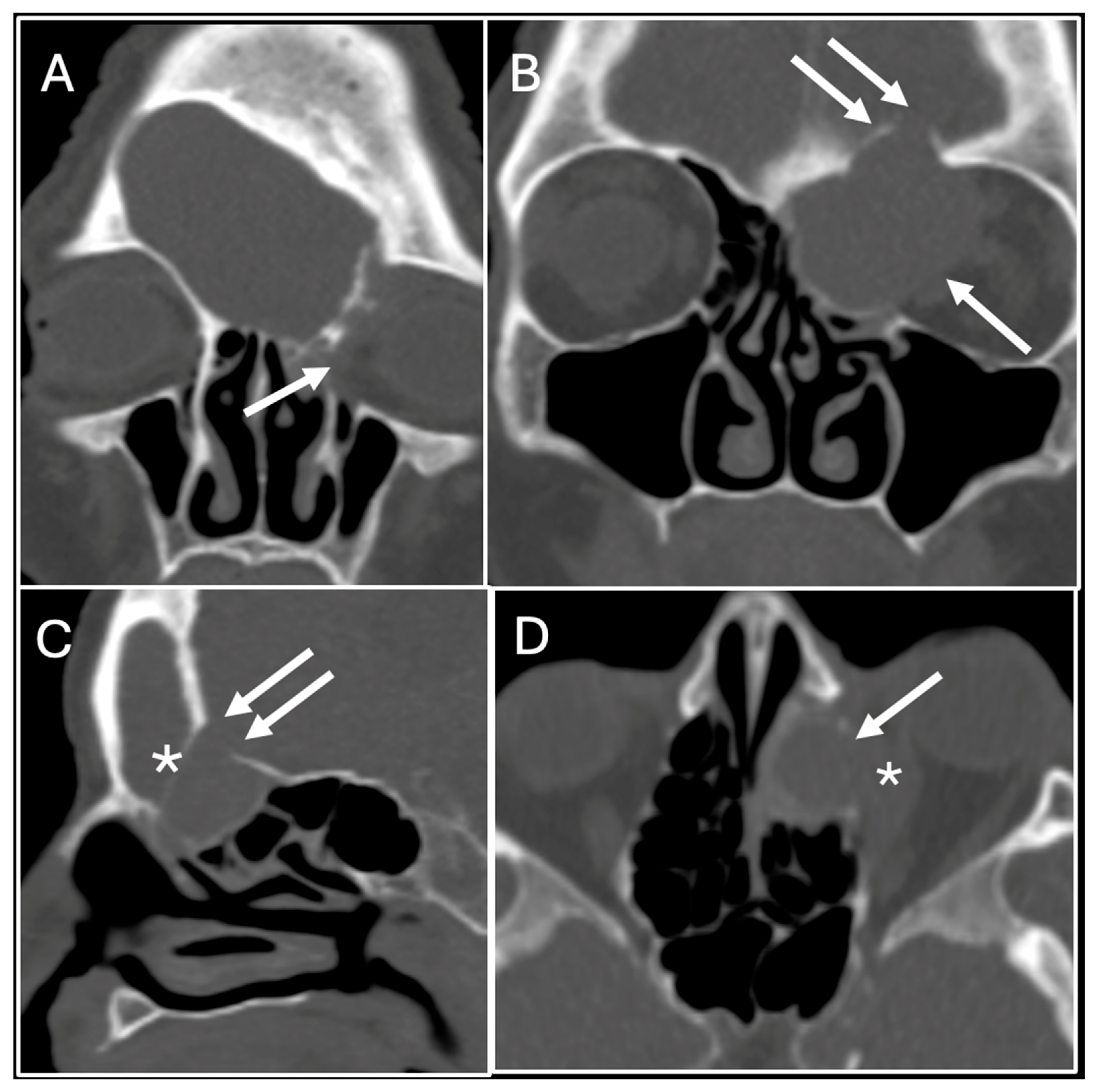
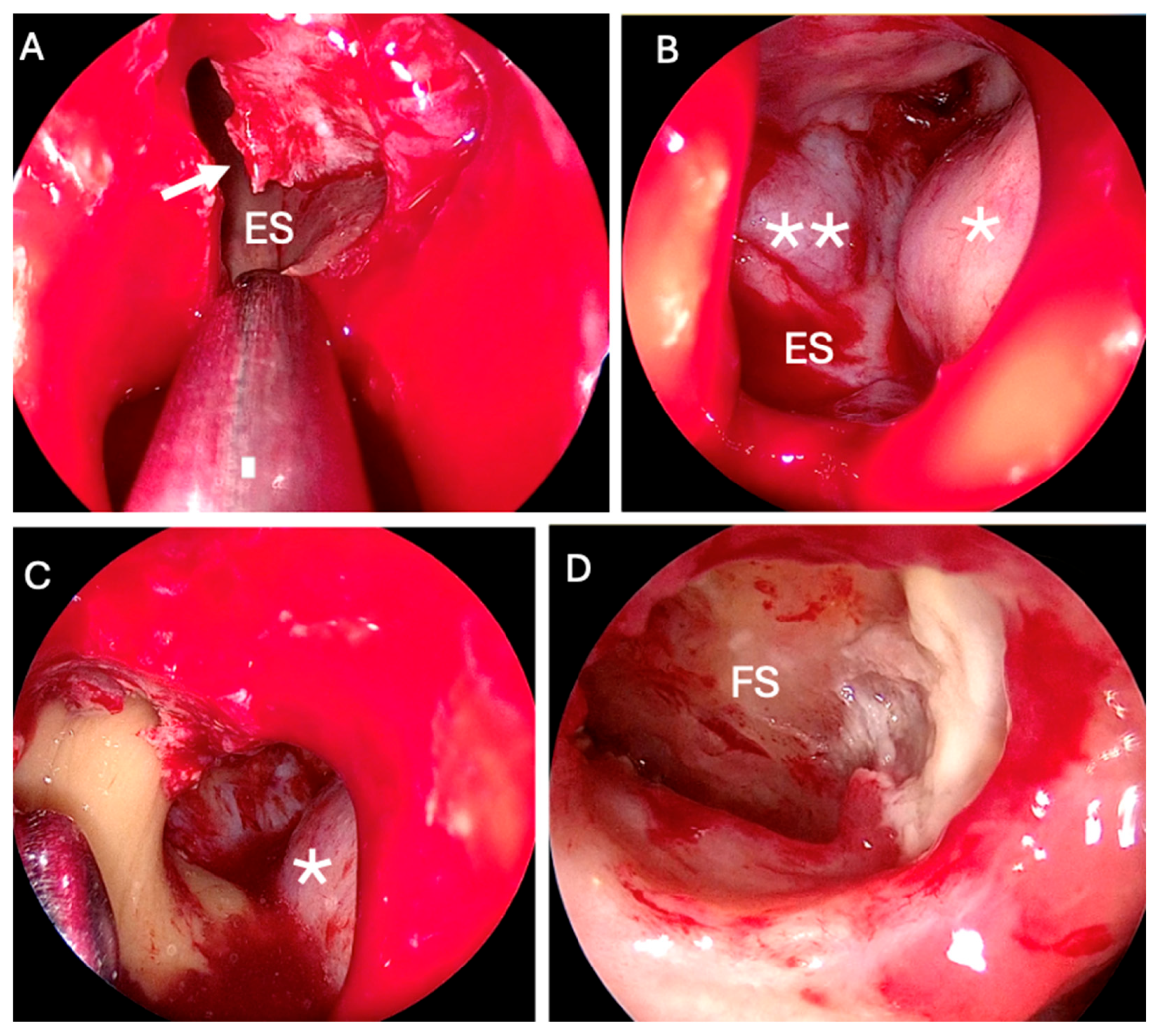
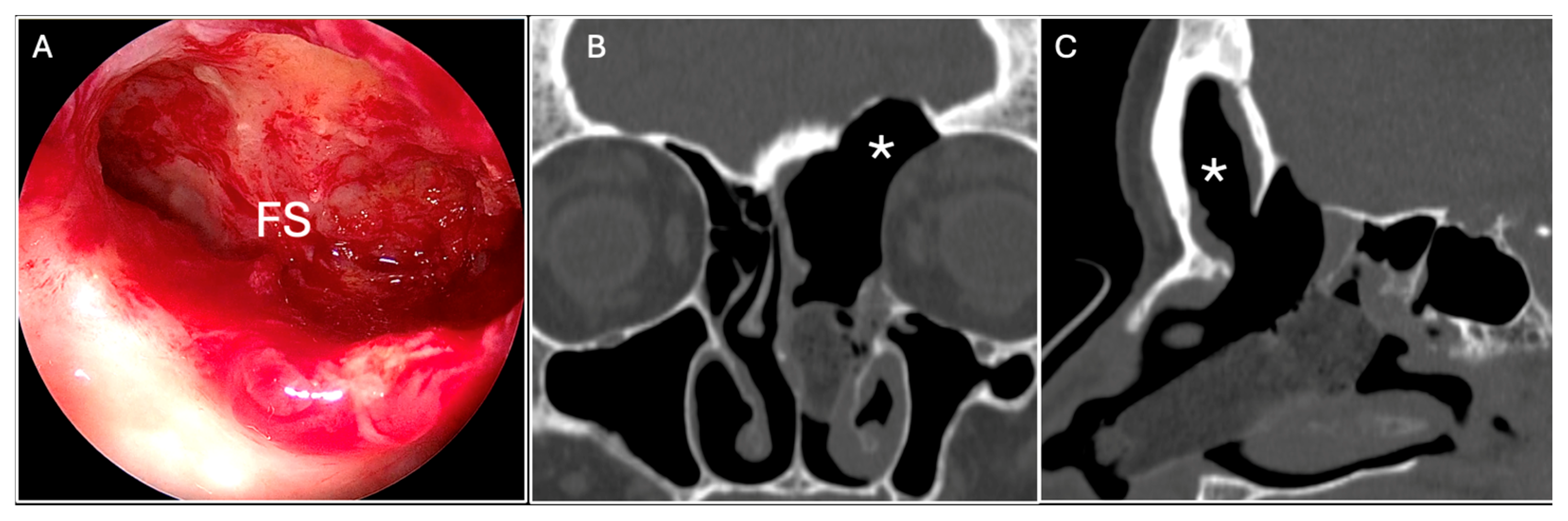
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ESS | Endoscopic Sinus Surgery |
| CT | Computed Tomography |
| MRI | Magnetic Resonance Imaging |
| CSF | Cerebrospinal Fluid |
| FB | Fungus Ball |
References
- Isaacson, B. Cholesterol Granuloma and Other Petrous Apex Lesions. Otolaryngol. Clin. N. Am. 2015, 48, 361–373. [Google Scholar] [CrossRef]
- Jackler, R.K.; Cho, M. A new theory to explain the genesis of petrous apex cholesterol granuloma. Otol. Neurotol. 2003, 24, 96–106. [Google Scholar] [CrossRef]
- Li, K.L.; Agarwal, V.; Moskowitz, H.S.; Abuzeid, W.M. Surgical approaches to the petrous apex. World J. Otorhinolaryngol. Head Neck Surg. 2020, 6, 106–114. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ochiai, H.; Yamakawa, Y.; Fukushima, T.; Nakano, S.; Wakisaka, S. Large cholesterol granuloma arising from the frontal sinus-case report. Neurol. Med. Chir. 2001, 41, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Durgam, A.; Batra, P.S. Paranasal sinus cholesterol granuloma: Systematic review of diagnostic and management aspects. Int. Forum Allergy Rhinol. 2013, 3, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Wershoven, N.; Miller, C.; Gibson, P.; Ciolino, A.; Rimash, T. Bilateral cholesterol granulomas of the maxillary sinus with review of the literature. SAGE Open Med. Case Rep. 2022, 10, 2050313X221116711. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lin, J.I.; Tseng, C.H.; Marsidi, P.J.; Bais, V.C. Cholesterol granuloma of right testis. Urology 1979, 14, 522–523. [Google Scholar] [CrossRef] [PubMed]
- Grignon, D.J.; Kirk, M.E.; Haines, D.S. Cholesterol granulomas in lymph nodes draining a benign ovarian neoplasm. Arch. Pathol. Lab Med. 1985, 109, 1124–1126. [Google Scholar] [PubMed]
- Amer, A.F.; Walia, H.S.; Madda, J.P. Cholesterol granuloma of the peritoneum. Can. J. Surg. 1990, 33, 410–413. [Google Scholar] [PubMed]
- Mafee, M.F.; Kumar, A.; Heffner, D.K. Epidermoid cyst (cholesteatoma) and cholesterol granuloma of the temporal bone and epidermoid cysts affecting the brain. Neuroimaging Clin. N. Am. 1994, 4, 561–578. [Google Scholar] [CrossRef] [PubMed]
- Nativ, O.; Mor, Y.; Nass, D.; Leibovitch, I.; Goldwasser, B. Cholesterol granuloma of the tunica vaginalis mimicking a neoplasm. Isr. J. Med. Sci. 1995, 31, 235–236. [Google Scholar] [PubMed]
- Fariña Pérez, L.A.; Menéndez, P.; Macho, V. Hydrocele and cholesterol granuloma of the tunica vaginalis simulating a tumor in echography. Actas Urol. Esp. 1998, 22, 70–73. (In Spanish) [Google Scholar] [PubMed]
- Schultz, R.; Mattila, J.; Gappa, M.; Verronen, P. Development of progressive pulmonary interstitial and intra-alveolar cholesterol granulomas (PICG) associated with therapy-resistant chronic systemic juvenile arthritis (CJA). Pediatr. Pulmonol. 2001, 32, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Mendonça, R.; Peron, C.S.; Stefani, M.A.; Gallo, P. Cerebral cholesterol granuloma: Case report. Arq. Neuropsiquiatr. 2007, 65, 540–541. [Google Scholar] [CrossRef] [PubMed]
- Paluzzi, A.; Gardner, P.; Fernandez-Miranda, J.C.; Pinheiro-Neto, C.D.; Scopel, T.F.; Koutourousiou, M.; Snyderman, C.H. Endoscopic endonasal approach to cholesterol granulomas of the petrous apex: A series of 17 patients: Clinical article. J. Neurosurg. 2012, 116, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, T.R.; Sinha, S.K.; Kejriwal, N.K. A rare case of cholesterol granuloma in the anterior mediastinum. Heart Lung Circ. 2013, 22, 303–304. [Google Scholar] [CrossRef] [PubMed]
- Young Sa, Y.J.; Hwang, S.J.; Sim, S.B.; Lee, S.H.; Moon, S.W.; Park, C.B. Cholesterol granuloma: A rare benign rib tumor. Ann. Thorac. Surg. 2013, 95, 1801–1803. [Google Scholar] [CrossRef]
- Unal, D.; Kilic, M.; Erkinuresin, T.; Demirbas, M.; Coban, S.; Aydos, M.M. Cholesterol granuloma of the paratesticular tissue: A case report. Can. Urol. Assoc. J. 2015, 9, 390–392. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Raghavan, D.; Lee, T.C.; Curtin, H.D. Cholesterol Granuloma of the Petrous Apex: A 5-Year Review of Radiology Reports with Follow-Up of Progression and Treatment. J. Neurol. Surg. B Skull Base 2015, 76, 266–271. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, M.; Tie, H.T.; Wang, C.L.; Wu, Q.C. Pulmonary interstitial cholesterol crystals associated with diffuse lung cysts in adult: A case report and literature review. J. Cardiothorac. Surg. 2016, 19, 11. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nam, G.; Singer, T.M.; Lourenco, A.P.; Wang, Y. Cholesteroloma of the breast: A 10 year retrospective review of 79 cases with radiology correlation. Breast J. 2019, 25, 1177–1181. [Google Scholar] [CrossRef] [PubMed]
- Eba, S.; Tanaka, R.; Watanabe, T.; Watanabe, Y.; Notsuda, H.; Suzuki, T.; Hirama, T.; Oishi, H.; Niikawa, H.; Noda, M.; et al. Anterior Mediastinal Cholesterin Granuloma Associated with Bilateral Pleurisy and Pericarditis. Kyobu Geka 2021, 74, 1059–1062. (In Japanese) [Google Scholar] [PubMed]
- Hassen, S.S.; Ali, G.A.; Ahmed, A.O.; Goravey, W. Cholesterol Granuloma: An Underrecognized Cause of Benign Lung Granuloma. Eur. J. Case Rep. Intern. Med. 2022, 9, 003264. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vinciguerra, A.; Turri-Zanoni, M.; Verillaud, B.; Guichard, J.P.; Spirito, L.; Karligkiotis, A.; Castelnuovo, P.; Herman, P. Typical and Atypical Symptoms of Petrous Apex Cholesterol Granuloma: Association with Radiological Findings. J. Clin. Med. 2022, 11, 4297. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yan, J.; Cai, Y.; Liu, R.; Lin, J.; Li, J. Cholesterol Granuloma of the Orbit. J. Craniofacial Surg. 2015, 26, 124–126. [Google Scholar] [CrossRef]
- Sia, D.I.T.; Davis, G.; Selva, D. Recurrent orbitofrontal cholesterol granuloma: A case report. Orbit 2012, 31, 184–186. [Google Scholar] [CrossRef]
- Arat, Y.O.; Chaudhry, I.A.; Boniuk, M. Orbitofrontal cholesterol granuloma: Distinct diagnostic features and management. Ophthalmic Plast Reconstr. Surg. 2003, 19, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Khalatbari, M.R.; Moharamzad, Y. Recurrent orbitofrontal cholesterol granuloma in pediatric patient: Case report and review of the literature. Childs Nerv. Syst. 2012, 28, 291–296. [Google Scholar] [CrossRef]
- Shrirao, N.; Mukherjee, B.; Krishnakumar, S.; Biswas, J. Cholesterol granuloma: A case series & review of literature. Graefes Arch. Clin. Exp. Ophthalmol. 2016, 254, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Ren, M.; Wang, W.; Li, R.; Zhang, L.; Liu, L. Orbitofrontal cholesterol granuloma masquerading as frontal sinus mucoceles: Report of two cases. BMC Ophthalmol. 2023, 23, 98. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ugga, L.; Stilo, S.; Napolitano, P.; Guadagno, E.; Iuliano, A.; Del Basso de Caro, M.L.; Elefante, A. Orbitofrontal cholesterol granuloma: Case report and review of the literature. Quant. Imaging Med. Surg. 2017, 7, 373–377. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Deep, N.L.; Chaaban, M.R.; Chaudhry, A.L.; Woodworth, B.A. Frontal sinus cholesterol granuloma: Case report. Allergy Rhinol. 2014, 5, 36–38. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yokoi, H.; Yamanaka, H.; Matsumoto, Y.; Kawada, M.; Fujiwara, M.; Ohara, A.; Saito, K. Modified Lothrop (Draf III) procedure for the treatment of a recurrent orbitofrontal cholesterol granuloma: A case report. SAGE Open Med. Case Rep. 2020, 8, 2050313X20907809. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Selva, D.; Lai, T.; Krishnan, S. Orbitofrontal cholesterol granuloma: Percutaneous endoscopic-assisted curettage. J. Laryngol. Otol. 2003, 117, 892–894. [Google Scholar] [CrossRef]
- Selva, D.; Phipps, S.E.; O’Connell, J.X.; White, V.A.; Rootman, J. Pathogenesis of orbital cholesterol granuloma. Clin. Exp. Ophthalmol. 2003, 31, 78–82. [Google Scholar] [CrossRef]
- Ong, L.Y.; McNab, A.A. Recurrent orbital cholesterol granuloma. Orbit 2008, 27, 119–121. [Google Scholar] [CrossRef]
- Kim, Y.K.; Kim, H.J.; Kim, H.Y.; Cha, J.; Lee, J.Y.; Chung, S.K.; Dhong, H.J.; Song, M.; Kim, S.T. Extrasinonasal infiltrative process associated with a sinonasal fungus ball: Does it mean invasive fungal sinusitis? Diagn. Interv. Radiol. 2016, 22, 347–353. [Google Scholar] [CrossRef]
- Fadda, G.L.; Allevi, F.; Rosso, C.; Martino, F.; Pipolo, C.; Cavallo, G.; Felisati, G.; Saibene, A.M. Treatment of Paranasal Sinus Fungus Ball: A Systematic Review and Meta-Analysis. Ann. Otol. Rhinol. Laryngol. 2021, 130, 1302–1310. [Google Scholar] [CrossRef] [PubMed]
- Popko, M.; Broglie, M.A.; Holzmann, D. Isolated fungus ball mimicking mucocele or frontal sinus tumour: A diagnostic pitfall. J. Laryngol. Otol. 2010, 124, 1111–1115. [Google Scholar] [CrossRef] [PubMed]
- DeShazo, R.D.; O’Brien, M.; Chapin, K.; Soto-Aguilar, M.; Swain, R.; Lyons, M.; Bryars, W.C., Jr.; Alsip, S. Criteria for the diagnosis of sinus mycetoma. J. Allergy Clin. Immunol. 1997, 99, 475–485. [Google Scholar] [CrossRef] [PubMed]
- Fadda, G.L.; Succo, G.; Moretto, P.; Veltri, A.; Castelnuovo, P.; Bignami, M.; Cavallo, G. Endoscopic Endonasal Surgery for Sinus Fungus Balls: Clinical, Radiological, Histopathological, and Microbiological Analysis of 40 Cases and Review of the Literature. Iran. J. Otorhinolaryngol. 2019, 31, 35–44. [Google Scholar] [PubMed] [PubMed Central]

| Authors | Site | No. Cases |
|---|---|---|
| Lin J. I. et al. [7] (1979) | Testis | 1 |
| Grignon D. J. et al. [8] (1985) | Lymph nodes | 1 |
| Amer A. F. et al. [9] (1990) | Peritoneum | 1 |
| Mafee M. F. et al. [10] (1994) | Brain | 7 |
| Nativ O. et al. [11] (1995) | Testis | 1 |
| Fariña Pérez L. A. et al. [12] (1998) | Testis | 1 |
| Schultz R. et al. [13] (2001) | Lung | 1 |
| Mendonça R. et al. [14] (2007) | Brain | 1 |
| Paluzzi A. et al. [15] (2012) | Petrous apex | 17 |
| Krishnan T. R. et al. [16] (2013) | Mediastinum | 1 |
| Young Sa Y. J. et al. [17] (2013) | Bone (rib) | 1 |
| Unal D. et al. [18] (2015) | Testis | 1 |
| Raghavan D. et al. [19] (2015) | Petrous apex | 18 |
| Zhang M. et al. [20] (2016) | Lung | 1 |
| Nam G. et al. [21] (2019) | Breast | 79 |
| Eba S. et al. [22] (2021) | Mediastinum | 1 |
| Hassen S. S. et al. [23] (2022) | Lung | 1 |
| Vinciguerra A. et al. [24] (2022) | Petrous apex | 29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rustichelli, C.; Serrone, A.; Cavallo, G.; Maniaci, A.; Fadda, G.L. Cholesterol Granuloma of the Frontal Sinus Complicated by Mycetoma: A Rare Case Report. Sinusitis 2025, 9, 15. https://doi.org/10.3390/sinusitis9020015
Rustichelli C, Serrone A, Cavallo G, Maniaci A, Fadda GL. Cholesterol Granuloma of the Frontal Sinus Complicated by Mycetoma: A Rare Case Report. Sinusitis. 2025; 9(2):15. https://doi.org/10.3390/sinusitis9020015
Chicago/Turabian StyleRustichelli, Chiara, Alessandro Serrone, Giovanni Cavallo, Antonino Maniaci, and Gian Luca Fadda. 2025. "Cholesterol Granuloma of the Frontal Sinus Complicated by Mycetoma: A Rare Case Report" Sinusitis 9, no. 2: 15. https://doi.org/10.3390/sinusitis9020015
APA StyleRustichelli, C., Serrone, A., Cavallo, G., Maniaci, A., & Fadda, G. L. (2025). Cholesterol Granuloma of the Frontal Sinus Complicated by Mycetoma: A Rare Case Report. Sinusitis, 9(2), 15. https://doi.org/10.3390/sinusitis9020015










