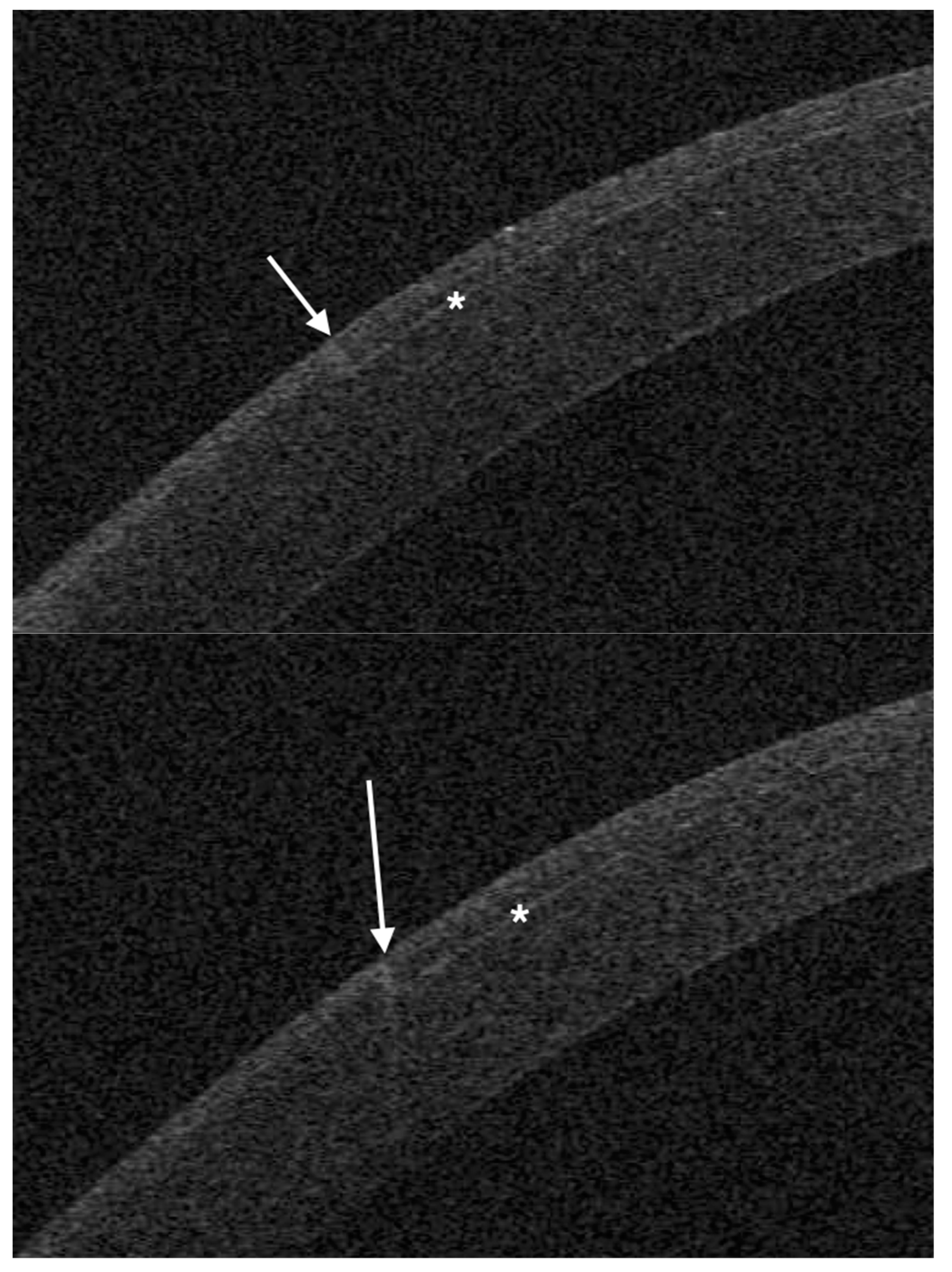
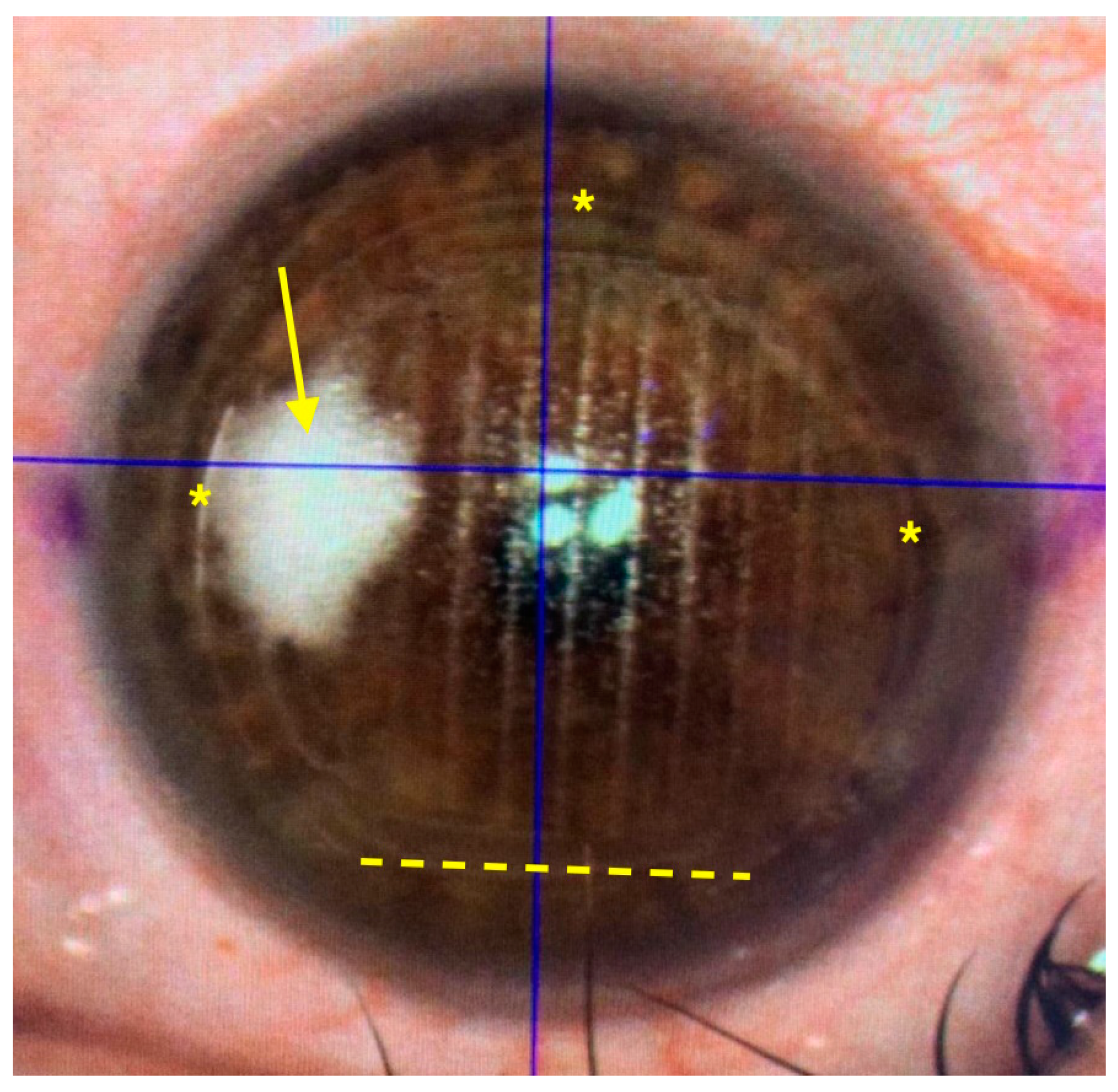
Creation of a Corneal Flap for Laser In Situ Keratomileusis Using a Three-Dimensional Femtosecond Laser Cut: Clinical and Optical Coherence Tomography Features
Abstract
1. Introduction
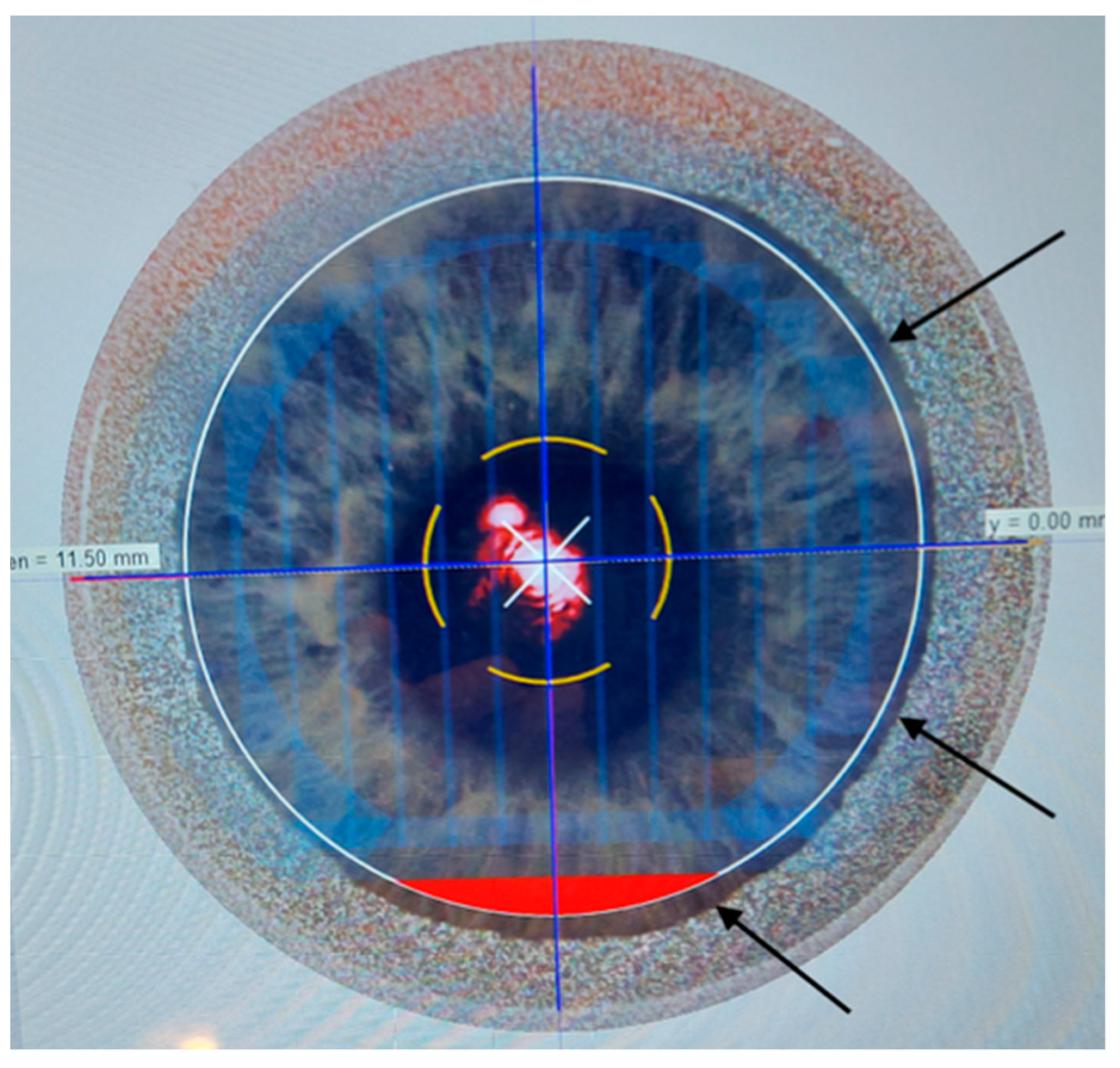
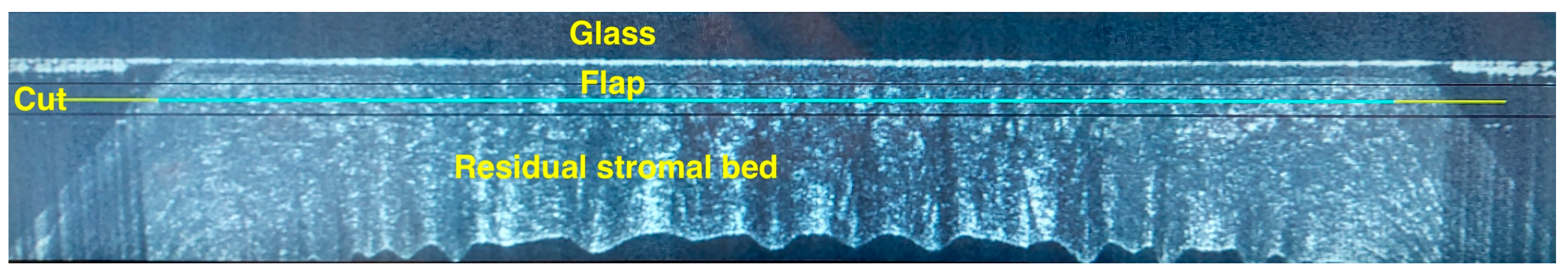
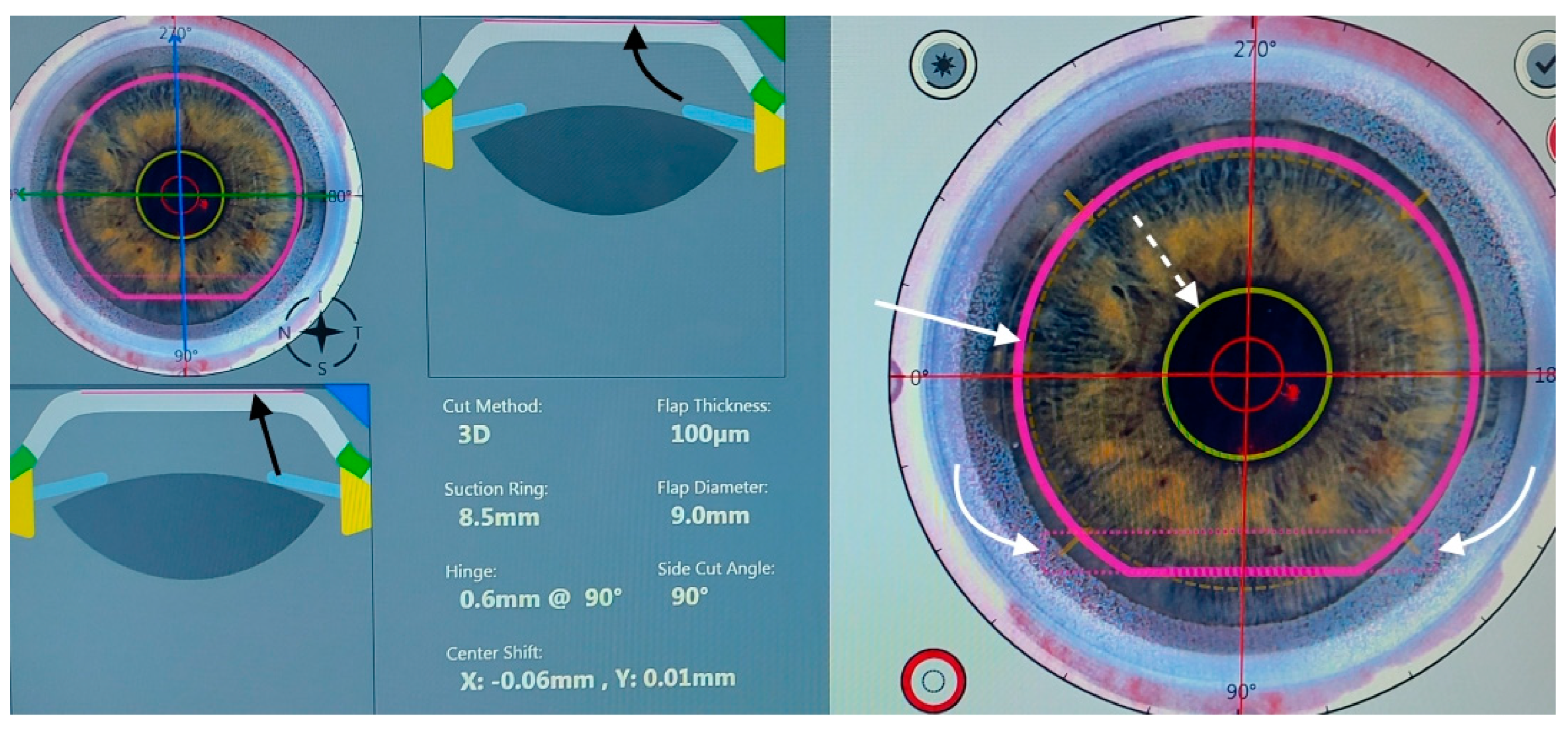
2. Materials and Methods
- (a)
- Myopia or compound myopic astigmatism with spherical equivalent (SE) −1 to −12 diopters (D), with at least 18 months of refractive stability, and a refractive astigmatism ≤ 3 D.
- (b)
- Age: between 25 and 50 years;
- (c)
- General health status: absence of collagen vascular disease; no pregnancy;
- (d)
- Ocular disease: no previous surgery; absence of scars or epithelial irregularities; absence of macular or lens abnormality; no topical treatment for ocular hypertension; absence of dry eye symptoms; non-invasive tear film break-up time ≥ 10 s (MS-39, Costruzione Strumenti Oftalmici, Florence, Italy); lacrimal fluid osmolarity ≤300 mOsm/l (I-PEN, Imedpharma, St. Laurent, QC, Canada);
- (e)
- Corneal features on OCT and Placido topography (MS-39): central pachymetry ≥480 µm; regular posterior elevation; anterior and posterior tangential topography; no signs of ectasia;
- (f)
- Corrected distance visual acuity (CDVA) ≥ 20/40 Snellen;
- (g)
- Minimum follow-up: 1 month from treatment.
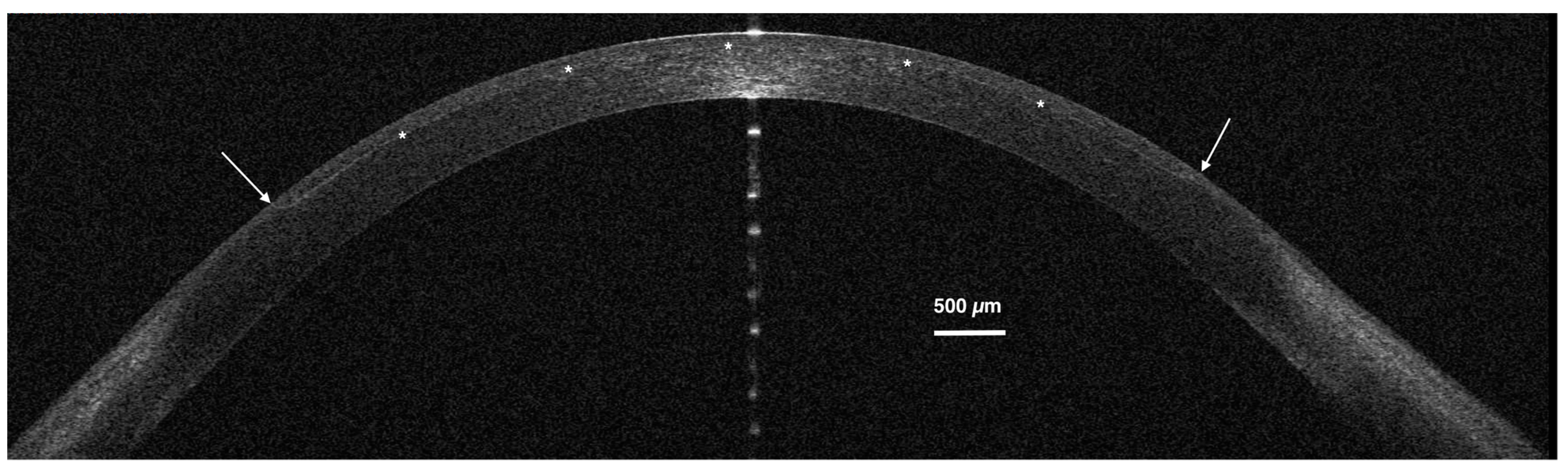
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CDVA | corrected distance visual acuity |
| LASIK | laser in situ keratomileusis |
| OBL | opaque bubble layer |
| OCT | optical coherence tomography |
| UDVA | uncorrected distance visual acuity |
References
- Ang, M.; Gatinel, D.; Reinstein, D.Z.; Mertens, E.; del Barrio, J.L.A.; Alió, J.L. Refractive surgery beyond 2020. Eye 2021, 35, 362–382. [Google Scholar] [CrossRef] [PubMed]
- Kymionis, G.D.; Kankariya, V.P.; Plaka, A.D.; Reinstein, D.Z. Femtosecond laser technology in corneal refractive surgery: A review. J. Refract. Surg. 2012, 28, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Clare, G.; Moore, T.C.B.; Grills, C.; Leccisotti, A.; Moore, J.E.; Schallhorn, S. Early flap displacement following LASIK. Ophthalmology 2011, 118, 1760–1765. [Google Scholar] [CrossRef] [PubMed]
- Jhanji, V.; Chan, T.C.; Li, W.Y.; Lim, R.R.; Yu, M.C.; Law, K.; Yi, P.; Yip, Y.W.; Wang, Y.; Ng, T.K.; et al. Conventional versus inverted sidecut flaps for femtosecond laser-assisted LASIK: Laboratory and clinical evaluation. J. Refract. Surg. 2017, 33, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Knox Cartwright, N.E.; Tyrer, J.R.; Jaycock, P.D.; Marshall, J. Effects of variation in depth and side cut angulations in lasik and thin-flap LASIK using a femtosecond laser: A biomechanical study. J. Refract. Surg. 2012, 28, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Yip, Y.W.Y.; Yu, M.C.Y.; Jhanji, V. Randomized, contralateral eye study to evaluate the effect of standard and inverted side-cut angle on corneal biomechanical properties during femtosecond laser-assisted in situ keratomileusis. Acta Ophthalmol. 2014, 92, e437–e442. [Google Scholar] [CrossRef]
- Taha, S.; Azzam, S.; Anis, M.; Zaazou, C.; Hosny, M. Verification and measurement of the side-cut angle of corneal flap in patients undergoing LASIK surgery using FS 200 kHz femtosecond laser system versus conventional mechanical microkeratome. Clin. Ophthalmol. 2019, 13, 985–992. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, D.; Rhee, K.I. Flap thickness reproducibility in laser in situ keratomileusis with a femtosecond laser: Optical coherence tomography measurement. J. Cataract. Refract. Surg. 2008, 34, 132–136. [Google Scholar] [CrossRef]
- Leccisotti, A.; Fields, S.V.; De Bartolo, G. Femtosecond-LASIK retreatments after primary myopic photorefractive keratectomy. Cornea 2023, 42, 675–679. [Google Scholar] [CrossRef]
- Knorz, M.C.; Vossmerbaeumer, U. Comparison of flap adhesion strength using the Amadeus microkeratome and the IntraLase iFS femtosecond laser in rabbits. J. Refract. Surg. 2008, 24, 875–878. [Google Scholar]
- Kung, J.S.; Sáles, C.S.; Manche, E.E. Corneal sensation and dry eye symptoms after conventional versus inverted side-cut femtosecond LASIK: A prospective randomized study. Ophthalmology 2014, 121, 2311–2316. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Sun, X.Y.; Shen, D.; Wang, X.R.; Ji, Y.Q.; Zhang, C.N. Comparison of healing patterns of different side-cut angulations after FS-LASIK. Int. J. Ophthalmol. 2021, 14, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Feng, Y.; Stojanovic, A.; Jankov, M.R., 2nd; Wang, Q. IntraLase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: A systematic review and meta-analysis. J. Refract. Surg. 2012, 28, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Vetter, J.M.; Holzer, M.P.; Teping, C.; Weingärtner, W.E.; Gericke, A.; Stoffelns, B.; Pfeiffer, N.; Sekundo, W. Intraocular pressure during corneal applanation: Comparison among four femtosecond lasers in porcine eyes. J. Refract. Surg. 2011, 27, 427–433. [Google Scholar] [CrossRef]
- Cameron, B.D.; Sara, N.A.; Strominger, M.B. Laser in situ keratomileusis-induced optic neuropathy. Ophthalmology 2001, 108, 660–665. [Google Scholar] [CrossRef]
- Arevalo, J.F.; Azar-Arevalo, O. Retinal detachment in myopic eyes after laser in situ keratomileusis. Am. J. Ophthalmol. 2000, 129, 825–826. [Google Scholar] [CrossRef]
- Mirshahi, A.; Kohnen, T. Effect of microkeratome suction during LASIK on ocular structures. Ophthalmology 2005, 112, 645–649. [Google Scholar] [CrossRef]
- Strohmaier, C.; Christian Runge, C.; Orang Seyeddain, O. Profiles of intraocular pressure in human donor eyes during femtosecond laser procedures—A comparative study. Investig. Ophthalmol. Vis. Sci. 2013, 54, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Farjo, A.A.; Sugar, A.; Schallhorn, S.C.; Majmudar, P.A.; Tanzer, D.J.; Trattler, W.B.; Cason, J.B.; Donaldson, K.E.; Kymionis, G.D. Femtosecond lasers for LASIK flap creation: A report by the American Academy of Ophthalmology. Ophthalmology 2013, 120, e5–e20. [Google Scholar] [CrossRef]
- Marino, G.K.; Santhiago, M.R.; Wilson, S.E. OCT study of the femtosecond laser opaque bubble layer. J. Refract. Surg. 2017, 33, 18–22. [Google Scholar] [CrossRef]
- He, X.; Li, S.M.; Zhai, C.; Zhang, L.; Wang, Y.; Song, X.; Wang, Y. Flap-making patterns and corneal characteristics influence opaque bubble layer occurrence in femtosecond laser-assisted laser in situ keratomileusis. BMC Ophthalmol. 2022, 22, 300. [Google Scholar] [CrossRef] [PubMed]
- Melki, S.A.; Azar, D.T. LASIK complications: Etiology, management, and prevention. Surv. Ophthalmol. 2001, 46, 95–116. [Google Scholar] [CrossRef] [PubMed]
- Leccisotti, A.; Fields, S.V.; De Bartolo, G.; Malandrini, A. Traumatic flap complications after femtosecond LASIK. Cornea 2022, 41, 604–608. [Google Scholar] [CrossRef]
- Asano-Kato, N.; Toda, I.; Hori-Komai, Y.; Takano, Y.; Tsubota, K. Epithelial ingrowth after laser in situ keratomileusis: Clinical features and possible mechanisms. Am. J. Ophthalmol. 2002, 134, 801–807. [Google Scholar] [CrossRef] [PubMed]

| Parameter | 2D | 3D | p Value (95% CI) |
|---|---|---|---|
| Age (years) | 36.4 (±4.5) | 37.2 (±6.1) | 0.27 § (−1.85 to 0.25) |
| Male/female (% males) | 74/126 (37) | 68/132 (34) | |
| Right/left eye (% right) | 94/106 (47) | 85/115 (43) | |
| Suction time (s) | 31.1 (±3.3) | 36.3 (±4.2) | 0 § * (−5.9 to −4.6) |
| Angle of sidecut (degrees) | 21 (±5) | 92 (±3) | |
| Opaque bubble layer | 2 | 9 | 0.03 ^ * |
| Folds | 13 | 7 | 0.25 ^ |
| Diffuse lamellar keratitis | 1 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leccisotti, A.; Fields, S.V.; De Bartolo, G.; Crudale, C.; Posarelli, M. Creation of a Corneal Flap for Laser In Situ Keratomileusis Using a Three-Dimensional Femtosecond Laser Cut: Clinical and Optical Coherence Tomography Features. Optics 2024, 5, 267-276. https://doi.org/10.3390/opt5020019
Leccisotti A, Fields SV, De Bartolo G, Crudale C, Posarelli M. Creation of a Corneal Flap for Laser In Situ Keratomileusis Using a Three-Dimensional Femtosecond Laser Cut: Clinical and Optical Coherence Tomography Features. Optics. 2024; 5(2):267-276. https://doi.org/10.3390/opt5020019
Chicago/Turabian StyleLeccisotti, Antonio, Stefania V. Fields, Giuseppe De Bartolo, Christian Crudale, and Matteo Posarelli. 2024. "Creation of a Corneal Flap for Laser In Situ Keratomileusis Using a Three-Dimensional Femtosecond Laser Cut: Clinical and Optical Coherence Tomography Features" Optics 5, no. 2: 267-276. https://doi.org/10.3390/opt5020019
APA StyleLeccisotti, A., Fields, S. V., De Bartolo, G., Crudale, C., & Posarelli, M. (2024). Creation of a Corneal Flap for Laser In Situ Keratomileusis Using a Three-Dimensional Femtosecond Laser Cut: Clinical and Optical Coherence Tomography Features. Optics, 5(2), 267-276. https://doi.org/10.3390/opt5020019






