Abstract
Burns are an actual problem of modern medicine. Oxidative stress, microcirculation, and hemostasis disorders are important links in the pathogenesis of burn disease. It is shown that these processes are significantly influenced by the point effect of low-intensity (LI) electromagnetic radiation (EMR) of the millimeter (MM) and submillimeter (subMM) ranges. However, the final opinion on the advantages of a particular range has not been formed. We have given a comparative assessment of the results of the effects of various frequency-energy parameters of microwaves on the indicators of adaptive reactions in rats under experimental thermal trauma and viscoelastic properties of blood in the case of burn disease.
1. Introduction
The problem of burn injuries has been actualized all over the world against the background of increased man-made disasters and local military conflicts [1,2,3]. Experience shows a close relationship between the quality of medical care in the acute period (from the first hours to the next 5–7 days from the moment of injury) and the outcomes of burn injury. This has encouraged the search for innovative technologies for early rehabilitation of burned patients [4]. Burns of the IIIA degree, in which the epidermis and partially the dermis die in the wound [5,6], lead to local and systemic pathological changes, the development of severe dysmetabolic changes, microcirculation disorders, and inhibition of the body’s protective reactions. This requires the use of combination therapy [7,8,9].
Modern local and general effects on the body by physical factors in burns should activate adaptive-compensatory reactions with the participation of the sympathoadrenal system, which plays a leading role in the process of adaptation of the body [10]. Despite the successes achieved, this problem remains very relevant and has acquired interdisciplinary significance [11,12].
Currently, microwave therapy is actively developing and using portable devices that generate EMR with a noise spectrum evenly distributed in the frequency range of 50–170 GHz [13]. In the interaction of the human body and animals with subMM EMR, the resonant absorption frequencies correspond to the maximum therapeutic efficiency and can vary over time depending on the state of the biological object and the nature of external influence [14]. The simplest way to achieve a therapeutic effect using MM and subMM EMR is to use sources with broadband frequency tuning or broadband sources of “white noise” with a power level of at least 10–18 W/(cm2∙Hz) at resonant frequencies. This method provides the maximum possible value of therapeutic efficacy for each organism with minimal doses of EMR exposure [15]. It has been shown that microwaves have a homeostatic effect on metabolic, microcirculatory, and hemostasiological disorders, especially at frequencies containing the molecular spectrum of radiation and absorption of NO and O2, as these molecules are involved in most biochemical reactions [16,17,18,19].
The optimal way to deliver EMR to the body is the impact on the acupuncture points (APs). This is explained by their biophysical features due to the increased concentration of extraneuronal transmitters [20,21]. Correlations between disorders of body functions under external EMR influences and biophysical characteristics of acupuncture points were experimentally investigated and a scheme of bioresonance interaction was constructed [22].
However, the use of microwave puncture therapy in the early rehabilitation of patients with burns has not been practically studied. In this regard, the assessment of the effectiveness of irradiation of APs by microwaves with different frequency characteristics is particularly relevant. The criteria for this assessment can be the dynamics of microcirculation, the level of oxidative enzymes, and indicators of viscoelastic properties of blood [23,24]. This paper analyzed the nature and degree of influence of various broadband bands of subMM and MM ranges of LI EMR on the induction of metabolic, vascular, and hemostasiological adaptive reactions in the acute period of experimental thermal trauma in vivo and in vitro. The differences were determined by comparing the data obtained with the indicators of intact animals and rats with contact thermal burn (CThB) without subsequent irradiation.
2. Materials and Methods
The experiments were carried out on 25 male Wistar rats weighing 310–360 g in accordance with the requirements of bioethics and the Rules of Laboratory Practice (GLP), the Geneva Convention for the Protection of Animals “International Guidelines for Biomedical Research involving Animals” (Geneva, 1990), Order No. 267 of the Ministry of Health of the Russian Federation dated 19 June 2003 “On approval of the rules of laboratory practice.” The study was approved by the Local Ethics Committee of the Volga Research Medical University of the Ministry of Health of the Russian Federation in accordance with the provisions of the Helsinki Declaration of 1975, revised in 2008. The animals were kept under the same conditions, and a free drinking regime and standard nutrition were observed until the end of the experiment.
We used a model of a grade IIIA contact thermal burn, which was applied under intramuscular anesthesia from a combination of “Zoletil-100” (“Virbacsanteanimale,” France), at a dose of 10 mL/kg, and “Xylavet” (“Interchemie,” the Netherlands), at a dose of 10 mg/kg, on the depilated surface of the animal’s back on an area of 20% of the body surface by a single three-second contact of an isolated skin area with a thermal heating element [25]. The rats were randomly divided into four groups of equal number (n = 4): 2 control groups and 2 experimental groups. Intact rats (control 1) and animals with contact thermal burn without subsequent irradiation (control 2) served as controls.
The rats of the experimental groups immediately after coming out of anesthesia began to receive a course of daily noncontact (0.5 cm above the skin surface) microwave exposure over the center of the occipital protuberance in the projection of the AP GV.14. Radiation power—1.0 McW, power density—0.05 McW/cm2, exposure—10 min. The exposure was carried out from the first to the seventh day after application of the drug. During the procedure, the animals were placed in a special pencil case.
Radiation sources: certified device “Amfit-0.2/10-01” (frequency range 53.57…78.33 GHz), developed by the limited liability company “Phystech” (Lobachevsky University, Nizhny Novgorod, Russia); experimental noise signal generator (frequency range 130.0–170.0 GHz), developed by IFM RAS (Nizhniy Novgorod, Russia). The noise mode of EMR allows the body to adjust to the resonance with the desired frequency, and the radiation parameters used are 3 times higher than the threshold sensitivity of cells, which minimizes possible side-effects.
Animals of the 3rd group (experiment 3) were irradiated with EMR MM 53.57–78.33 GHz, which does not contain the frequencies of messenger molecules. Animals of the 4th group (experiment 4) received the exposure to EMR subMM 130.0–170.0 GHz (contains molecular spectrum of radiation and absorption of O2 and NO). The animals were removed from the experiment under anesthesia after decapitation after the seventh radiation session.
For the biochemical analysis of the enzymatic activity, blood stabilized with sodium citrate (1:9) was used. The activity of free radical oxidation processes in plasma and red blood cells was studied by the method of induced biochemiluminescence (BHL) on the device BHL-06 (N. Novgorod), coupled with an IBM computer. The BHL-06 device is designed for recording light fluxes that occur in biological samples as a result of enzymatic and chemical processes. The following parameters of the chemiluminogram were evaluated: tg2a—an indicator that characterizes the rate of decline in free radical oxidation processes in plasma—total antioxidant activity (TAA); the chemiluminescence light sum for 30 s (S) is an indicator that reflects the potential ability of a biological object to perform lipid peroxidation (LPO). The intensity of the LPO was determined by the level of malonic dialdehyde (MDA) and activity of the superoxide dismutase (SOD) [26]. The activities of catalase and lactate dehydrogenase (LDH) in the direct (LDHdir) and reverse (LDHrev) reactions, and glutathione reductase (GR) and glucose-6-phosphate dehydrogenase (Gl-6-fDH) were determined by the spectrophotometric method [27].
The dynamics of microblood flow in the border area of the burn injury was monitored before the injury and on the 7-th day after contact thermal burn under combined anesthesia according to the Laser Doppler flowmetry (LDF) method [28]. The integral MI, which characterizes the degree of perfusion of the tissue volume per unit of time, was evaluated using a laser blood flow analyzer LAKK-M (“Lazma”, Russia) with the use of a wavelet analysis, which allows us to evaluate the components of microvessel tonus based on the values of the amplitudes of microcirculation fluctuations [29].
The study of the state of the hemostasis system was carried out using the thromboelastography method in whole citrated blood against the background of irradiation with low-intensity broadband EMR with different frequency characteristics. Blood samples from 29 patients with burns on an area of at least 20% of the body surface were irradiated (15 men aged 42 ± 3 years and 14 women 51 ± 4 years old). Blood sampling was performed under standard conditions: in the morning, on an empty stomach, from the cubital vein. The obtained blood samples were divided into three groups, which were then irradiated with low-intensity microwave EMR with different broadband frequency ranges.
For 11 blood samples, the source of LI EMP was the range of 53.57–78.33 GHz; in 18 cases, the exposure was carried out with an experimental generator of a subMM noise signal of 130.0–170.0 GHz, which contains the molecular emission and absorption spectra (MSEA) of an oxygen molecule (O2) and nitric oxide molecule (NO). The effect of LI EMR on citrated blood samples with a volume of 340 μL placed in a disposable cuvette was carried out in the direct irradiation mode with an exposure of 5 and 30 min.
The study of the viscoelastic properties of whole blood was carried out according to the standard technique of thromboelastography. Measurement of thromboelastographic parameters was carried out on samples of citrated blood with the addition of a coalin activator (TEG mode—citrated kaolin). All indicators of the kinetics of coagulation obtained using this program were obtained, and the TEG indicators were subjected to statistical analysis: R, K, α, MA, G. Indicators: R— initiation of thrombosis (initiation); K—amplification (amplification); angle α—propagation (distribution) characterizes, in general, the state of the coagulation system and clearly correlates with the main phases of thrombus formation of the modern cellular-base model of blood coagulation; MA is the maximum amplitude; and G is the density of the blood clot.
To test statistical hypotheses, the Student’s t-test and Mann–Whitney U-test were used. The critical value of the significance level was taken equal to 0.05. Quantitative data are presented as M ± σ, as well as the median and the first and third quartile Me (Q1; Q3). Statistical data processing was carried out using the Statistica 6.0 software (Stat Soft, Inc., Tulsa, OK, USA)
3. Results
The study of biochemical parameters of oxidative and energy metabolism in animals of the second control group against the background of contact thermal burn in the absence of radiation revealed the development of oxidative stress. This was confirmed by statistically significant differences in the studied parameters compared to intact rats (p < 0.05). This was manifested in the activation of free radical oxidation in the blood (an increase in the concentration of MDA in red blood cells by 20%, in plasma by 11%, the S index—by 42% in plasma, and by 7% in red blood cells) and a decrease in the specific activity of antioxidant enzymes (SOD, catalase, GR, Gl-6-fDH) in red blood cells and TAA in blood plasma. Decreases in the activity of LDHdir and LDHrev by 39% and 30%, respectively, against the background of contact thermal burn (compared with intact animals) led to lactic acidosis and, as a result, the development of hypoxia.
The general dynamics of the indicators of the antioxidant and energy systems under the influence of course irradiation of rats with different frequency ranges under the conditions of experimental burn injury is presented in Table 1.

Table 1.
Dynamics of indicators of antioxidant and energy systems in groups.
From the presented data, it follows that a 7-day course of daily exposure to broadband LI EMR on APs in the skin projection of the center for the vegetative regulation of animals with experimental thermal trauma at frequencies of 130.0–170.0 GHz led to a decrease in the intensity of LPO in blood plasma. Thus, the S index remained significantly higher than the control values of intact rats by 14.84% (p = 0.001), and that of the concentration of MDA in erythrocytes was higher by 70.25% under the influence of subMM EMR in the frequency range of 130.0–170.0 GHz, where NO and O2 MSEA are present.
Under the influence of subMM EMR with frequency spectra of 130.0–170.0 GHz, the activity of SOD and TAA in four experimental groups was significantly reduced compared to intact rats (control 1). The red blood cells of these animals had increased peroxide resistance, which increased their resistance in the fight against active oxygen forms formed against the background of thermal trauma.
A parallel study of the dynamics of MI showed a decrease in tissue perfusion by 21% compared to intact animals (Figure 1) during the contact thermal burn without subsequent irradiation (control 2). This is natural for the pathogenesis of thermal trauma.
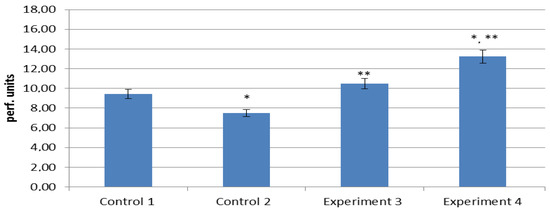
Figure 1.
The level of the microcirculation indicator (MI) in the experimental treatment of thermal trauma. *—differences are statistically significant compared to intact rats (p < 0.05); **—differences are statistically significant compared to CThB controls (p < 0.05).
The intensity of blood flow in the animals from the three experimental groups compared with the rats of the second control group (contact thermal burn without treatment) significantly (p < 0.05) increased by 29% and exceeded the normal parameters of the animals of the first control group by only 11%.
The greatest increase in the level of tissue perfusion was observed in rats exposed to subMM EMR in the ranges of 130.0–170.0 GHz. The microcirculation indicator was comparable in the four experimental groups. A significant increase of 39% compared to control 1 and 73% compared to control 2 was recorded in the four experimental groups. This fact confirms the vasodilatation effect of nitric oxide, which is included in the frequency ranges.
The analysis of the dynamics of factors of active and passive regulation of microcirculation was carried out to assess the mechanisms of development of adaptive vascular reactions against the background of EMR irradiation. The application of contact thermal burn affected the state of microhemodynamics, initiating the centralization of blood circulation. This was confirmed by the inhibition of local hemodynamics (a decrease in the endothelial, neurogenic, and myogenic ranges by 44%, 45%, and 32% respectively) (Figure 2), as well as intensive activation of the systemic (an increase in respiratory by 416% and cardiac by 340% components) regulation of microcirculation in relation to intact animals (Figure 3) (p < 0.05). This trend continued in the experimental groups.
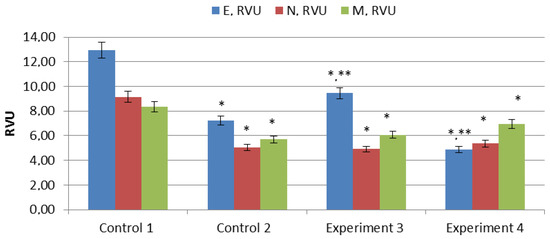
Figure 2.
Dynamics of factors of active regulation of microcirculation under the influence of different EMR ranges of MM and subMM on animals in the CThB state. Note: E—endothelial factor, M—myogenic factor, N—neurogenic factor, *—differences are statistically significant compared to intact rats (p < 0.05); **—differences are statistically significant compared to CThB controls (p < 0.05).
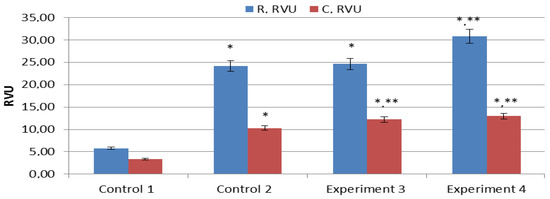
Figure 3.
Dynamics of passive factors of regulation under various factors of influence on a burn wound. Note: R—respiratory factor, C—cardiac component, *—differences are statistically significant compared to intact rats (p < 0.05); **—differences are statistically significant compared to CThB controls (p < 0.05).
The greatest increase in fluctuations in the ranges of endothelial (by 23%) and cardiac (by 15%) frequencies in relation to the control group (2) (p < 0.05) was observed in the three experimental groups under the influence of EMR MM 53.57–78.33 GHz.
The factors of active regulation underwent noticeable changes compared to the control (2) values (a decrease in the endothelial component by 32% and an increase in the myogenic component by 22%), and the factors of passive regulation increased according to the respiratory and cardiac components by 21% and 20%, respectively (p < 0.05), in group 4 under the influence of EMR subMM 130.0–170.0 GHz.
The effect of low-intensity microwaves of the millimeter range on the viscoelastic properties of the blood of heavily burned patients has been experimentally confirmed. Analysis of studies carried out in vitro showed that exposure to a broadband range of 53.57–78.33 GHz had a potentiating effect on the initiation (R) and enhancement (k) phases of blood coagulation, both at 5 and 30 min of exposure. At the same time, the effect of this radiation range on the propagation phase (α) and mechanical properties of the blood clot (MA and G) was not recorded (Table 2).

Table 2.
Dependence of the dynamics of the viscoelastic properties of blood on the EMM spectrum and exposure to radiation.
Irradiation of blood samples with EMR with a frequency range of 130.0–170.0 GHz, which contains MSEA of oxygen and nitric oxide, both at 5 and 30 min of exposure, caused a shortening of the R interval, which indicated an activating effect on the initiation phase. At the same time, after 5 min of exposure, no effect on the phases of propagation and enhancement of blood coagulation was revealed, while lengthening the irradiation time to 30 min caused a decrease in the activity of the coagulation cascade. This was evidenced by the prolonged time of initial thrombus formation (k) and a decrease in the rate of clot formation (α). Irradiation with this spectrum also affected the properties of the formed clot: exposure for 5 min contributed to an increase in the clot density (MA, G); with an increase in the exposure to 30 min, its decrease (MA, G) was noted. These changes demonstrate the dose-dependent effect of EMR at the frequencies of the MSEA of oxygen and nitric oxide on the viscoelastic properties of blood: the potentiating effect as a result of 5 min of irradiation is replaced by inhibition of the activity of the hemostasis system after 30 min of exposure (Table 2).
4. Discussion
Daily exposure to LI EMR for 7 days on animals with experimental thermal trauma led to the activation of energy metabolism in erythrocytes, most pronounced in the frequency range of EMR 130.0–170.0 GHz, contributing to the utilization of lactic acid. This is probably due to the increased activity of LDH due to the interaction of NO contained in the frequency spectrum of this range with the sulfate groups of the active center of this enzyme. According to biochemiluminescence and MDA concentration data, LPO indicators in animals exposed to broadband EMR of 53.57–78.33 GHz demonstrated a statistically significant antioxidant effect, manifested in a significant decrease in the activity of the LPO process in plasma and erythrocytes and increases in TAA and the activity of antioxidant enzymes. Compared with intact rats, the indicators of the pro-oxidant system were increased, and the antioxidant system was reduced. This confirms the results of previous studies [18].
The important results of the study were the absence of a negative effect of all EMR ranges on the processes of lipid peroxidation and antioxidant protection in the experimental groups. Exposure to EMR 130.0–170.0 GHz with frequency ranges of emission and absorption of nitric oxide and oxygen compared to EMR 53.57–78.33 GHz had a more pronounced antioxidant effect associated with increases in TAA and the enzymatic activities of SOD, catalase, GR, and glucose-6-phosphate dehydrogenase. The effect of EMR 130.0–170.0 GHz had a pronounced stimulating effect on the energy metabolism of erythrocytes, manifested in an increase in LDH activity, and had a normalizing effect on the enzymatic activity of FRO in the blood and the activities of GR and glucose-6-phosphate dehydrogenase.
The effect of EMR 130.0–170.0 GHz had a pronounced stimulating effect on the energy metabolism of erythrocytes, manifested in an increase in LDH activity, and had a normalizing effect on the enzymatic activity of FRO in the blood and the activities of GR and glucose-6-phosphate dehydrogenase. This also led to a decrease in active regulation factors. Thus, the chains of interaction of various indicators of LPO, factors, and components of microcirculation systems in the process of adaptation of the body to acute thermal stress were demonstrated. The role of nitric oxide as an endogenous vasodilator and neurotransmitter was shown, which statistically significantly positively modified the state of oxidative blood metabolism and the main estimated indicators of vascular reactions, which indirectly confirms the readaptive possibilities of microwaves in the early post-burn period.
Irradiation of EMR with a range of 130.0–170.0 GHz, which contains the molecular spectrum of radiation and absorption of NO and O2, also led to a decrease in the indicators of active regulation, which coincides with the data of other researchers on the decisive role of NO in the development of adaptive vascular reactions and confirms our preliminary results [30]. However, the pronounced normalizing effect noted not only by us when working at frequencies of 130.0–170.0 GHz in the case of burn disease cannot be interpreted unambiguously, taking into account the possible overstrain of the hypothalamic–pituitary–adrenal system. The possibility of inversion of the physiological reaction with a subsequent decrease in adaptive energy has been noted [31,32], which requires the continuation of the studies initiated and the development of differentiated indications for the inclusion of microwave therapy in the complex rehabilitation of patients with thermal injuries.
The EMR of 130.0–170.0 GHz was characterized by a dual effect on the viscoelastic properties of blood, which was manifested by activation of the initial stage of coagulation and normalization of the density of the blood clot characterizing the end point of coagulation. One of the possible reasons for the potentiating effect of this type of radiation may be the fact that oxygen affects the activity of coagulation, fibrinolysis, as well as the regulation of effector cells such as platelets, endothelial cells, erythrocytes, neutrophils, mast cells, monocytes, and fibroblasts. The effect of EMR on the hemostasiological profile may be associated with a change in the functional activity of transport proteins, enzymes that determine biochemical processes, as well as biomacromolecules embedded in membranes in response to their conformational rearrangement in the process of increasing the dose of EMR exposure [33]. In our study, this was manifested by a decrease in the viscoelastic properties of blood in patients with burn injury with an increase in the exposure to EMR of 130.0–170.0 GHz from 5 to 30 min.
5. Conclusions
The results of this study allow us to expand the understanding of the degree and mechanism of the physiopunctural effect of various low-intensity ranges of microwave EMR on the development of protective metabolic and vascular reactions of the body in vivo. The modifying effect on the state of the hemostasis system in the process of adaptation of the body to acute stress was demonstrated.
Author Contributions
Conceptualization, A.G.P.; methodology, A.G.S., P.V.P. and M.V.P.; validation, A.G.S., P.V.P. and M.V.P.; resources, V.V. and A.V.K.; writing—original draft preparation, A.G.P.; writing—review and editing, A.G.S., P.V.P. and M.V.P.; project administration, A.G.P. All authors have read and agreed to the published version of the manuscript.
Funding
The work was carried out within the framework of the scientific research Reg. No. 121030100012-9 “Experimental and clinical justification of the use of innovative technologies of medical rehabilitation using physical factors.
Institutional Review Board Statement
The animal study protocol was approved by the Ethics Committee of Privolzhsky Research Medical University of the Ministry of Health of the Russian Federation (protocol 75/13 14 July 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
No applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript.
References
- Shabanov, V.E.; Savvin, Y.U.N.; Alekseev, A.A.; Krutikov, M.G.; Bobrovnikov, A.E.; Demenko, V.V. Klinicheskie Rekomendacii po Okazaniyu Medicinskoj Pomoshchi Postradavshim s Termicheskoj Travmoj v Chrezvychajnyh Situaciyah; Zashchita: Moscow, Russia, 2016; p. 240. [Google Scholar]
- Sidel’nikov, V.O.; Cygan, V.N.; Zinov’ev, E.V. Boevye Ozhogovye Porazheniya; SpecLit: Saint-Petersburg, Russia, 2019; p. 247. [Google Scholar]
- Van Lieshout, E.M.; Van Yperen, D.T.; Van Baar, M.E.; Polinder, S.; Boersma, D.; Cardon, A.Y.; De Rijcke, P.A.; Guijt, M.; Klem, T.M.; Lansink, K.W.; et al. Epidemiology of injuries, treatment (costs) and outcome in patients with burns admitted to the hospital with or without a dedicated burn center (Burn-Pro): Protocol of a multicenter prospective observational study. BMJ 2018, 8, 023709. [Google Scholar] [CrossRef] [PubMed]
- Alekseev, A.A.; Bobrovnikov, A.E.; Bogdanov, V.V. Evaluation of the effectiveness of innovative technologies for the treatment of burn victims. Med. Alfavit 2020, 13, 44–47. [Google Scholar] [CrossRef]
- Ubbink, D.T.; Brolmann, F.E.; Go, P.M.; Vermeule, N.H. Evidence-based care for acute wounds: A perspective. Adv. Wound Care 2015, 4, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Agadzhanova, K.V. Burns: Classification and treatment approaches depending on the severity. Colloquium-J. 2020, 1, 4. [Google Scholar]
- Bobrovnikov, A.E.; Alekseev, A.A. Personalized technologies for local treatment of burn wounds. Lechenie I Profil. 2017, 3, 75–78. [Google Scholar]
- Saeidinia, A.A.; Keihanian, F.; Lashari, A.P.; Lahiji, H.G.; Mobayyen, M.; Heidarzade, A.; Golchan, J. Healing of partial-thickness burn wounds with local treatment: A randomized controlled comparison of silver sulfadiazine and santiderma. Medicina 2017, 96, 61–68. [Google Scholar]
- Fayazov, A.D.; Tulyaganov, D.B.; Kamilov, U.R.; Ruzimuratov, D.A. Modern methods of local treatment of burn wounds. Vestn. Ekstrennoj Med. 2019, 12, 43–47. [Google Scholar]
- Tapbergenov, S.O.; Tapbergenov, T.S.; Sovetov, B.S. Funkcional’nye i Metabolicheskie Effekty Simpato-Adrenalovoj Sistemy i Stress; Akademiya Estestvoznaniya: Moscow, Russia, 2019; p. 138. [Google Scholar]
- Podoinitsyna, M.G.; Cepelev, A.V.; Stepanov, V.L. Clinical efficacy of magnetic laser therapy for skin burns. Zabajkal’skij Med. Vestn. 2015, 2, 99–102. [Google Scholar]
- Bailey, J.K.; Blackstone, B.N.; De Bruler, D.M.; Kim, J.Y.; Baumann, M.E.; McFanrland, K.L.; Imeokpana, F.O.; Supp, D.M.; Powell, H.M. Effects of early combinatorial processing of autologous split-thickness skin grafts in the Duroc red pig model using a pulsed dye laser and a fractional CO2 laser. Lazern. Hir. 2018, 50, 78–87. [Google Scholar]
- Moskvin, S.V.; Khadartsev, A.A. EHF-Laser Therapy; Publishing house “Triad”: Tver, Russia, 2016; p. 168. [Google Scholar]
- Vaks, V.L.; Anfertev, V.A.; Balakirev, V.Y.; Basov, S.A.; Domracheva, E.G.; Illyuk, A.V.; Kupriyanov, P.V.; Pripolzin, S.I.; Chernyaeva, M.B. High resolution terahertz spectroscopy for analytical applications. Phys. Usp. 2020, 63, 708–720. [Google Scholar] [CrossRef]
- KVCh-Terapija s Nizkointensivnym Shumovym Izlucheniem; Balchugov, V.A., Poljakova, A.G., Anisimov, S.I., Kornauchov, A.V.N., Eds.; NGU: Novgorod, Russia, 2002; p. 192. [Google Scholar]
- Kiryanova, V.V.; Zharova, E.N.; Bagraev, N.T.; Reukov, A.S.; Loginova, S.V. Prospects of application of electromagnetic waves of the terahertz range in physiotherapy (retrospective review). Physiother. Balneol. Rehabil. 2016, 4, 209–215. [Google Scholar] [CrossRef]
- Deryugina, A.V.; Talamanova, M.N.; Hlamova, Y.U.N.; Kuvaeva, S.S.; Shabalin, M.A.; Oshevenskij, L.V.; Cvetkov, A.I.; Glavin, M.Y. Adaptive reactions of red blood cells under the action of electromagnetic radiation of the terahertz range. Mezhdunarodnyj Nauchno-Issledovatel’skij Zhurnal 2017, 1–2, 6–8. [Google Scholar]
- Soloveva, A.G.; Polyakova, A.G.; Peretyagin, P.V.; Didenko, N.V. The influence of terahertz radiation on biochemical metabolism of blood in the experiment. EPJ Web Conf. 2018, 195, 32–33. [Google Scholar] [CrossRef][Green Version]
- Lukin, S.Y.; Soldatov, Y.P.; Stogov, M.V. Complex correction of pathophysiological disorders in orthopedic and traumatological patients with the use of electromagnetic waves of the terahertz range at the frequencies of nitric oxide radiation. Vopr. Kurortol. Fizioter. I Lech. Fiz. Kul’tury 2018, 95, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Polyakova, A.G. Microwave Reflexotherapy in the Complex Rehabilitation of Patients with Traumatological and Orthopedic Profile Textbook Nizhny; PIMU: Novgorod, Russia, 2020; p. 56. [Google Scholar]
- Spasova, N.V.; Razumov, A.N.; Lyubovcev, V.B. The role of acupuncture points in the interaction of the human body with the interplanetary electromagnetic field. Vestn. Vosstanov. Med. 2007, 4, 103–104. [Google Scholar]
- Savin, L.A.; Panov, G.A.; Makashova, E.S. Neurophysiological changes that occur during the reflexotherapy procedure. Refleksoterapiya I Komplement. Med. 2017, 4, 25–26. [Google Scholar]
- Parshina, S.S.; Afanasyeva, T.N.; Vodolagin, A.V.; Petrova, V.D.; Ushakov VYu Kaplanova, T.I.; Potapova, M.V.; Ramazanova, Z.G. Terahertz therapy at frequencies of the molecular spectrum of nitric oxide: Results and prospects of clinical use. Sarat. Nauchno-Med. Zhurnal 2019, 15, 800–806. [Google Scholar]
- Subbotina, T.I.; Yashin, A.A. Effects of interaction of electromagnetic fields with biosystems. Vestn. Novyh Med. Tekhnologij Elektron. Zhurnal 2018, 4, 1–20. [Google Scholar]
- Peretyagin, P.V.; Solov’eva, A.G.; Luzan, A.S.; Vorob’ev, E.V.; Didenro, N.V. Ustrojstvo Dlya Esperimental’nogo Modelirovaniya Termicheskoj Travmy Kozhi. RU Patent 179 126 U1 MПK A61B 18/04, 26 April 2018. [Google Scholar]
- Sirota, T.V. A new approach to the study of the epinephrine auto-oxidation reaction: The possibility of polarographic determination of the activity of superoxide dismutase and the antioxidant properties of various drugs. Biomed. Him. 2012, 58, 77–87. [Google Scholar]
- Sibgatullina, G.V.; Haertdinova, L.R.; Gumerova, E.A.; Akulov, A.N.; Kostyukova, Y.U.A.; Nikonorova, N.A.; Rumyanceva, N.I. Metody Opredeleniya Redoks-Statusa Kul’tiviruemyh Kletok Rastenij:Uchebno-Metodicheskoe Posobie; Kazanskij (Privolzhskij) Federal’nyj Universitet: Kazan, Russia, 2011; p. 61. [Google Scholar]
- Kozlov, V.I.; Azolov, G.A.; Gurova, O.A.; Litvin, F.B. Lazernaya Dopplerovskaya Floumetriya v Ocenke Sostoyaniya i Rasstrojstv Mikrocirkulyacii Krovi. Metodicheskoe Posobie; RUDN GNC Lazer. Med.: Moscow, Russia, 2012; p. 32. [Google Scholar]
- Krupatkin, A.I.; Sidorov, V.V. Funkcional’naya Diagnostika Sostoyaniya Mikrocirkulyatorno-Tkanevyh Sistem: Kolebaniya, Informaciya, Nelinejnost’; Rukovodstvo Dlya Vrachej; Knizhnyj dom “LIBROKOM”: Moscow, Russia, 2013; p. 496. [Google Scholar]
- Martusevich, A.K.; Peretyagin, S.P.; Samodelkin, A.G.; Solov’eva, A.G.; Martusevich, A.A.; Ivashchenko, M.N. Biomedicina Oksida Azota (NO): Funkcional’no-Metabolicheskie Aspekty; Nizhegorodskaya Gosudarstvennaya Sel’skohozyajstvennaya Akademiya: Nizhny Novgorod, Russia, 2017; p. 261. [Google Scholar]
- Ushakova, T.A. Adaptation to Burn Injury: Problems and Prospects. Kombustiologiya 2009, 39. Available online: http://combustiolog.ru/journal/adaptatsiya-k-ozhogovoj-travme-problemy-i-perspektivy/ (accessed on 17 January 2022).
- Dmitriev, G.I.; Aref’ev, I.Y.U.; Korotkova, N.L.; Belousov, S.S.; Poyato, T.V.; Men’shenina, E.G.; Poluakova, A.G. Improving the rehabilitation of patients with the consequences of burn injury. Med. Al’manah 2010, 2, 225–228. [Google Scholar]
- Ivanov, D.V.; Lischuk, A.N.; Borisova, O.N. Effects of low-energy electromagnetic radiation of high frequencies when exposed to cells (literature review). Bulletin of New Medical Technologies. Electron. Ed. 2020, 3, 143–152. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).