Management of Intracranial Hemorrhage in the Setting of Mechanical Heart Valve Replacement Therapy
Abstract
1. Introduction
2. Development of Normal Heart Valves
3. Dysfunction of the Heart Valves
4. Mechanical and Bioprosthetic Heart Valves
5. Complications of Artificial Heart Valves
6. Mechanical Heart Valves Background
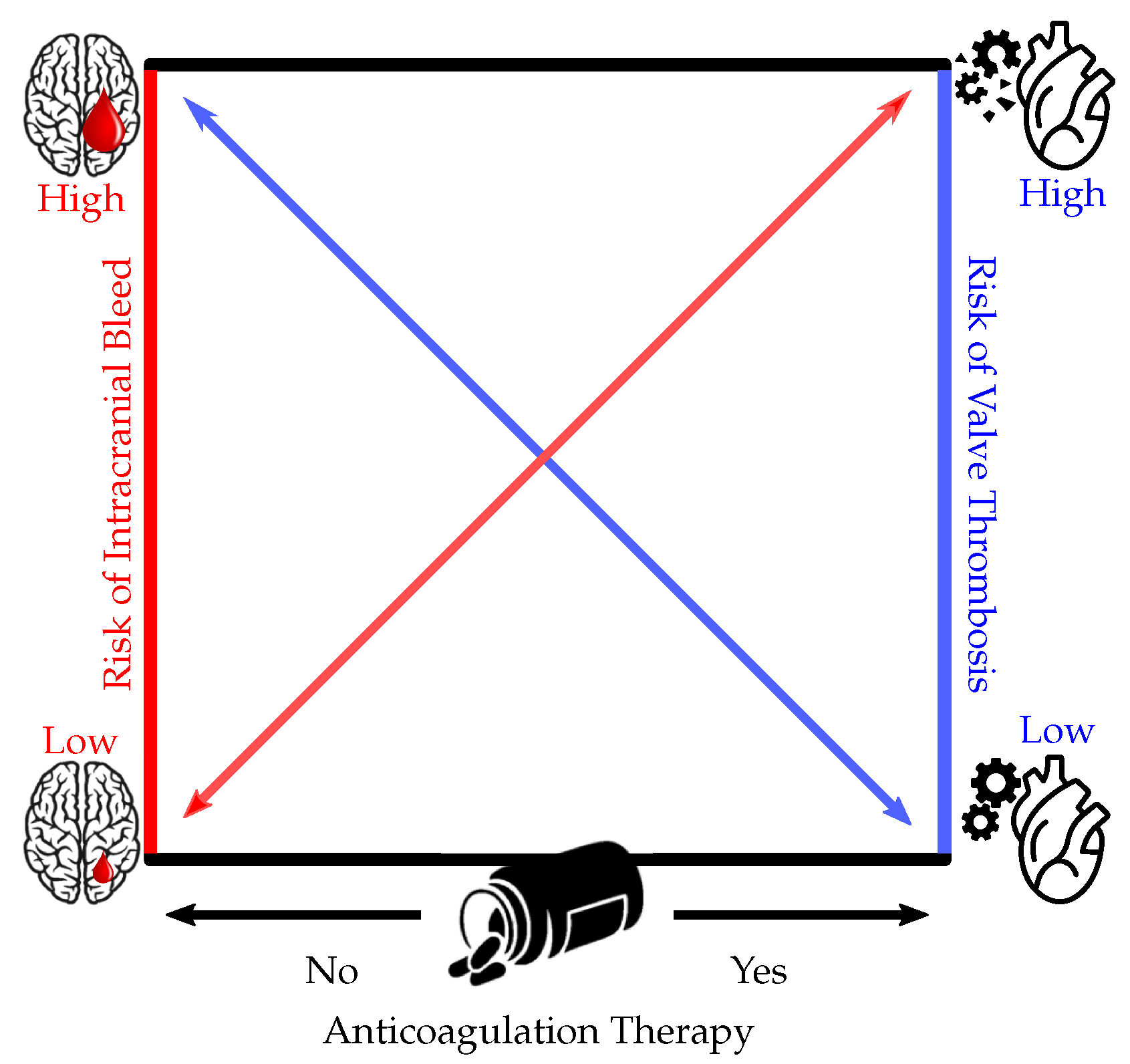
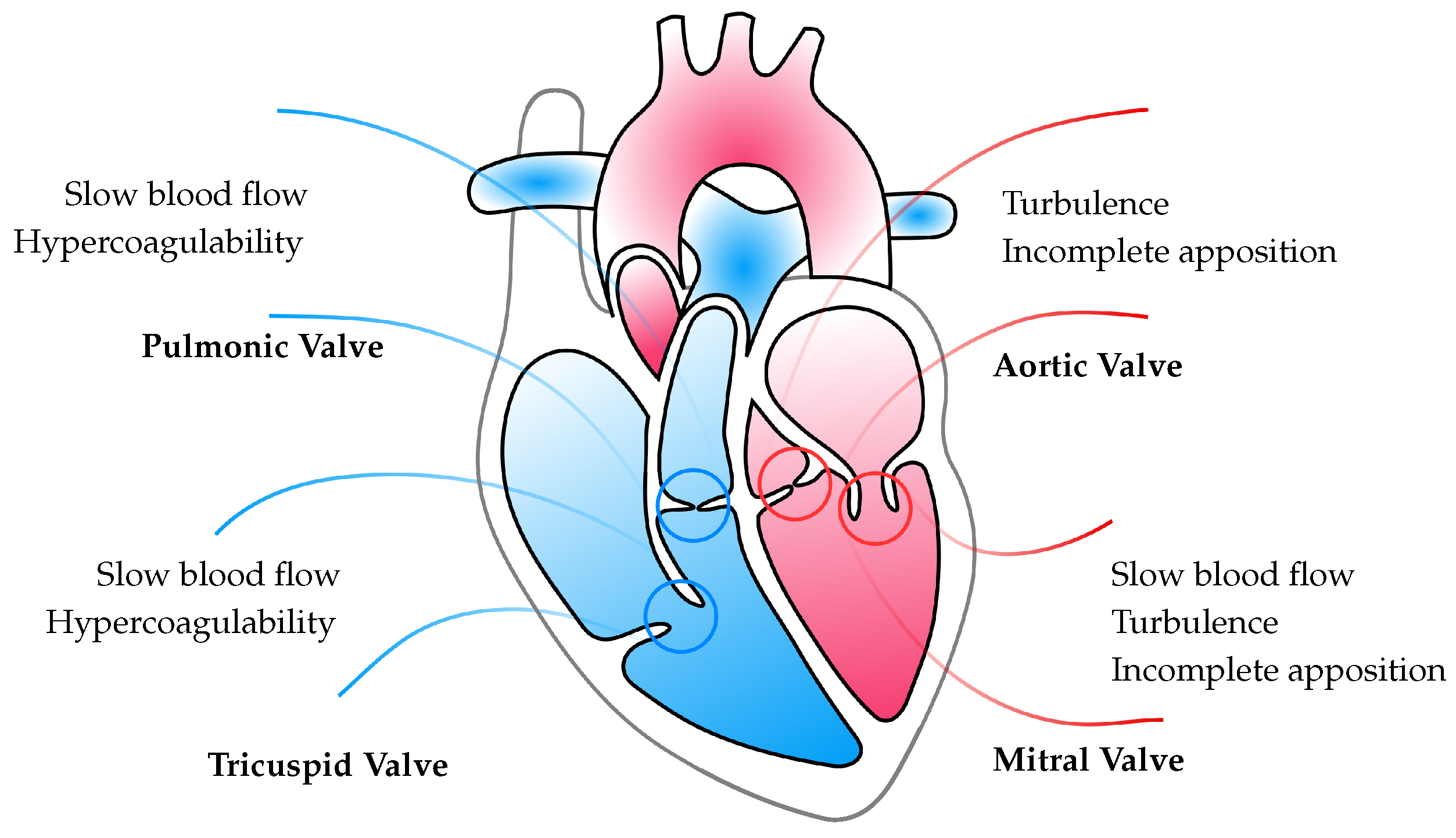
7. Thromboembolism and the Need for Anticoagulation
8. Anticoagulants and Their Reversal Agents
9. Efficacy of Different Anticoagulant Regiments with Mechanical Heart Valves
10. Risk for Intracranial Hemorrhage with Anticoagulants and Its Management
11. Discussion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| US | United States |
| ICH | Intracranial Hemorrhage |
| AV | Atrioventricular |
| TAVR | Transcatheter Aortic Valve Replacement |
| IV | Intravenous |
| TMVR | Transcatheter Mitral Valve Replacement |
| FFP | Fresh Frozen Plasma |
| PCC | Prothrombin Complex Concentrates |
| LMWH | Low Molecular Weight Heparins |
| ACS | Acute Coronary Syndrome |
| PCI | Percutaneous Coronary Intervention |
| CABG | Coronary Artery Bypass Graft |
| INR | International Normalized Ratio |
| VARC | Valve Academic Research Consortium |
| BVD | Bioprosthetic Valve Dysfunction |
| BVF | Bioprosthetic Valve Failure |
| AVA | Aortic Valve Area |
| DVI | Doppler Velocity Index |
| AR | Aortic Regurgitation |
| VTE | Venous Thromboembolism |
References
- Aluru, J.S.; Barsouk, A.; Saginala, K.; Rawla, P.; Barsouk, A. Valvular Heart Disease Epidemiology. Med. Sci. 2022, 10, 32. [Google Scholar] [CrossRef] [PubMed]
- Dangas, G.D.; Weitz, J.I.; Giustino, G.; Makkar, R.; Mehran, R. Prosthetic Heart Valve Thrombosis. J. Am. Coll. Cardiol. 2016, 68, 2670–2689. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, S.M.; Ziai, W.C.; Cordonnier, C.; Dowlatshahi, D.; Francis, B.; Goldstein, J.N.; Hemphill, J.C.; Johnson, R.; Keigher, K.M.; Mack, W.J.; et al. 2022 Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke 2022, 53, e282–e361. [Google Scholar] [CrossRef] [PubMed]
- Combs, M.D.; Yutzey, K.E. Heart Valve Development. Circ. Res. 2009, 105, 408–421. [Google Scholar] [CrossRef]
- Spicer, D.E.; Bridgeman, J.M.; Brown, N.A.; Mohun, T.J.; Anderson, R.H. The anatomy and development of the cardiac valves. Cardiol. Young 2014, 24, 1008–1022. [Google Scholar] [CrossRef]
- MacGrogan, D.; Münch, J.; de la Pompa, J.L. Notch and interacting signalling pathways in cardiac development, disease, and regeneration. Nat. Rev. Cardiol. 2018, 15, 685–704. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, E.J.; Bischoff, J. Heart Valve Development. Circ. Res. 2004, 95, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.J.; Lin, C.Y.; Chen, C.H.; Zhou, B.; Chang, C.P. Partitioning the heart: Mechanisms of cardiac septation and valve development. Development 2012, 139, 3277–3299. [Google Scholar] [CrossRef]
- Hinton, R.B.; Yutzey, K.E. Heart Valve Structure and Function in Development and Disease. Annu. Rev. Physiol. 2011, 73, 29–46. [Google Scholar] [CrossRef]
- Zuñiga, L.F.F.; Cerón, Y.S.M.; Salazar, L. Structural remodelling of the heart valves extracellular matrix during embryo development. Anat. Histol. Embryol. 2020, 50, 206–211. [Google Scholar] [CrossRef]
- Rabkin-Aikawa, E.; Mayer, J.E.; Schoen, F.J. Heart Valve Regeneration. In Advances in Biochemical Engineering/Biotechnology; Springer: Berlin/Heidelberg, Germany, 2005; pp. 141–179. [Google Scholar] [CrossRef]
- Vitartaitė, M.; Vaičiulytė, D.; Venclovienė, J.; Širvinskas, E.; Bukauskienė, R.; Jakuška, P.; Vimantaitė, R. Risk Factors Associated with an Increased Risk of Deep Sternal Wound Infections in Patients After Coronary Artery Bypass Grafting and Heart Defect Surgery. Heart Surg. Forum 2021, 24, E741–E745. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, O.; Omran, J.; Al-Dadah, A.; Enezate, T. Outcomes of transcatheter aortic valve replacement in patients with mitral valve regurgitation. Adv. Interv. Cardiol. 2019, 15, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Pope, J.E.; Deer, T.R.; Falowski, S.M. A Retrospective, Single-Center, Quantitative Analysis of Adverse Events in Patients Undergoing Spinal Stenosis with Neurogenic Claudication Using a Novel Percutaneous Direct Lumbar Decompression Strategy. J. Pain Res. 2021, 14, 1909–1913. [Google Scholar] [CrossRef]
- Stephan, P.J.; Henry, A.C.; Hebeler, R.F.; Whiddon, L.; Roberts, W.C. Comparison of Age, Gender, Number of Aortic Valve Cusps, Concomitant Coronary Artery Bypass Grafting, and Magnitude of Left Ventricular-Systemic Arterial Peak Systolic Gradient in Adults Having Aortic Valve Replacement for Isolated Aortic Valve Stenosis. Am. J. Cardiol. 1997, 79, 166–172. [Google Scholar] [CrossRef]
- Bosse, Y.; Miqdad, A.; Fournier, D.; Pepin, A.; Pibarot, P.; Mathieu, P. Refining Molecular Pathways Leading to Calcific Aortic Valve Stenosis by Studying Gene Expression Profile of Normal and Calcified Stenotic Human Aortic Valves. Circ. Cardiovasc. Genet. 2009, 2, 489–498. [Google Scholar] [CrossRef]
- Hinton, R.B.; Lincoln, J.; Deutsch, G.H.; Osinska, H.; Manning, P.B.; Benson, D.W.; Yutzey, K.E. Extracellular Matrix Remodeling and Organization in Developing and Diseased Aortic Valves. Circ. Res. 2006, 98, 1431–1438. [Google Scholar] [CrossRef] [PubMed]
- Rabkin-Aikawa, E.; Farber, M.; Aikawa, M.; Schoen, F.J. Dynamic and reversible changes of interstitial cell phenotype during remodeling of cardiac valves. J. Heart Valve Dis. 2004, 13, 841–847. [Google Scholar]
- Liu, A.C.; Joag, V.R.; Gotlieb, A.I. The Emerging Role of Valve Interstitial Cell Phenotypes in Regulating Heart Valve Pathobiology. Am. J. Pathol. 2007, 171, 1407–1418. [Google Scholar] [CrossRef]
- Helms, A.S.; Bach, D.S. Heart Valve Disease. Prim. Care Clin. Off. Pract. 2013, 40, 91–108. [Google Scholar] [CrossRef]
- Supino, P.G.; Borer, J.S.; Preibisz, J.; Bornstein, A. The Epidemiology of Valvular Heart Disease: A Growing Public Health Problem. Heart Fail. Clin. 2006, 2, 379–393. [Google Scholar] [CrossRef]
- Holst, K.A.; Said, S.M.; Nelson, T.J.; Cannon, B.C.; Dearani, J.A. Current Interventional and Surgical Management of Congenital Heart Disease. Circ. Res. 2017, 120, 1027–1044. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.Y.; Higgins, A.; Desai, M.Y. Bicuspid aortic valve: Basics and beyond. Clevel. Clin. J. Med. 2018, 85, 779–784. [Google Scholar] [CrossRef] [PubMed]
- Mrsic, Z.; Hopkins, S.P.; Antevil, J.L.; Mullenix, P.S. Valvular Heart Disease. Prim. Care Clin. Off. Pract. 2018, 45, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Iung, B.; Vahanian, A. Epidemiology of valvular heart disease in the adult. Nat. Rev. Cardiol. 2011, 8, 162–172. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.G. Etiology of valvular heart disease. Curr. Opin. Cardiol. 1996, 11, 98–113. [Google Scholar] [CrossRef]
- Hollenberg, S.M. Valvular heart disease in adults: Etiologies, classification, and diagnosis. FP Essent. 2017, 457, 11–16. [Google Scholar]
- Reineke, D.; Gisler, F.; Englberger, L.; Carrel, T. Mechanical versus biological aortic valve replacement strategies. Expert Rev. Cardiovasc. Ther. 2016, 14, 423–430. [Google Scholar] [CrossRef]
- Flameng, W. Bio-artificial organs: Cardiac applications. Verh. K. Acad. Geneeskd. Belg. 2004, 66, 246–252. [Google Scholar]
- Harter, K.; Levine, M.; Henderson, S. Anticoagulation Drug Therapy: A Review. West. J. Emerg. Med. 2015, 16, 11–17. [Google Scholar] [CrossRef]
- Boroumand, M.; Goodarzynejad, H. Monitoring of anticoagulant therapy in heart disease: Considerations for the current assays. J. Tehran Heart Cent. 2010, 5, 57–68. [Google Scholar]
- Neumann, P.J.; Weinstein, M.C. The Diffusion of New Technology: Costs and Benefits to Health Care. In The Changing Economics of Medical Technology; Institute of Medicine (US) Committee on Technological Innovation in Medicine: Washington, DC, USA; National Academies Press (US): Washington, DC, USA, 1991; Chapter 2. [Google Scholar]
- Álamo, B.S.; Moi, L.; Bajema, I.; Faurshou, M.; Flossmann, O.; Hauser, T.; Hruskova, Z.; Jayne, D.; Luqmani, R.; Mahr, A.; et al. Long-term outcomes and prognostic factors for survival of patients with ANCA-associated vasculitis. Nephrol. Dial. Transplant. 2023, gfac320. [Google Scholar] [CrossRef]
- Kostyunin, A.E.; Yuzhalin, A.E.; Rezvova, M.A.; Ovcharenko, E.A.; Glushkova, T.V.; Kutikhin, A.G. Degeneration of Bioprosthetic Heart Valves: Update 2020. J. Am. Heart Assoc. 2020, 9, e018506. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, C.C.; Komninou, M.A.; Badria, A.F.; Korossis, S.; Koutsoukos, P.; Mavrilas, D. Calcification Assessment of Bioprosthetic Heart Valve Tissues Using an Improved In Vitro Model. IEEE Trans. Biomed. Eng. 2020, 67, 2453–2461. [Google Scholar] [CrossRef] [PubMed]
- Glower, D.D. Commentary: Biologic versus mechanical valves: Wandering in the dark. J. Thorac. Cardiovasc. Surg. 2019, 158, 715. [Google Scholar] [CrossRef] [PubMed]
- Capodanno, D.; Petronio, A.S.; Prendergast, B.; Eltchaninoff, H.; Vahanian, A.; Modine, T.; Lancellotti, P.; Sondergaard, L.; Ludman, P.F.; Tamburino, C.; et al. Standardized definitions of structural deterioration and valve failure in assessing long-term durability of transcatheter and surgical aortic bioprosthetic valves: A consensus statement from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) endorsed by the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. J. Cardio-Thorac. Surg. 2017, 52, 408–417. [Google Scholar] [CrossRef]
- Mendelson, K.; Schoen, F.J. Heart Valve Tissue Engineering: Concepts, Approaches, Progress, and Challenges. Ann. Biomed. Eng. 2006, 34, 1799–1819. [Google Scholar] [CrossRef]
- Malvindi, P.G.; Luthra, S.; Olevano, C.; Salem, H.; Kowalewski, M.; Ohri, S. Aortic valve replacement with biological prosthesis in patients aged 50–69 years. Eur. J. Cardio-Thorac. Surg. 2020, 59, 1077–1086. [Google Scholar] [CrossRef]
- David, T. How to Decide Between a Bioprosthetic and Mechanical Valve. Can. J. Cardiol. 2021, 37, 1121–1123. [Google Scholar] [CrossRef]
- Alkady, H.; Saber, A.; Abouramadan, S.; Elnaggar, A.; Nasr, S.; Mahmoud, E. Mitral valve replacement in mitral stenosis; the problem of small left ventricle. J. Cardiothorac. Surg. 2020, 15. [Google Scholar] [CrossRef]
- Stocco, F.; Fabozzo, A.; Bagozzi, L.; Cavalli, C.; Tarzia, V.; D’Onofrio, A.; Lorenzoni, G.; Chiminazzo, V.; Gregori, D.; Gerosa, G. Biological versus mechanical aortic valve replacement in non-elderly patients: A single-centre analysis of clinical outcomes and quality of life. Interact. CardioVasc. Thorac. Surg. 2020, 32, 515–521. [Google Scholar] [CrossRef]
- Pibarot, P.; Herrmann, H.C.; Wu, C.; Hahn, R.T.; Otto, C.M.; Abbas, A.E.; Chambers, J.; Dweck, M.R.; Leipsic, J.A.; Simonato, M.; et al. Standardized Definitions for Bioprosthetic Valve Dysfunction Following Aortic or Mitral Valve Replacement. J. Am. Coll. Cardiol. 2022, 80, 545–561. [Google Scholar] [CrossRef] [PubMed]
- Head, S.J.; Çelik, M.; Kappetein, A.P. Mechanical versus bioprosthetic aortic valve replacement. Eur. Heart J. 2017, 38, 2183–2191. [Google Scholar] [CrossRef] [PubMed]
- Azari, S.; Rezapour, A.; Omidi, N.; Alipour, V.; Tajdini, M.; Sadeghian, S.; Bragazzi, N.L. A systematic review of the cost-effectiveness of heart valve replacement with a mechanical versus biological prosthesis in patients with heart valvular disease. Heart Fail. Rev. 2019, 25, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Diaz, R.; Hernandez-Vaquero, D.; Alvarez-Cabo, R.; Avanzas, P.; Silva, J.; Moris, C.; Pascual, I. Long-term outcomes of mechanical versus biological aortic valve prosthesis: Systematic review and meta-analysis. J. Thorac. Cardiovasc. Surg. 2019, 158, 706–714.e18. [Google Scholar] [CrossRef]
- Tao, E.; Wan, L.; Wang, W.; Luo, Y.; Zeng, J.; Wu, X. The prognosis of infective endocarditis treated with biological valves versus mechanical valves: A meta-analysis. PLoS ONE 2017, 12, e0174519. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Wang, W. Bioprosthetic vs. Mechanical Mitral Valve Replacement for Rheumatic Heart Disease in Patients Aged 50–70 Years. Front. Cardiovasc. Med. 2022, 9, 904958. [Google Scholar] [CrossRef]
- Lameijer, H.; van Slooten, Y.J.; Jongbloed, M.R.; Oudijk, M.A.; Kampman, M.A.; van Dijk, A.P.; Post, M.C.; Mulder, B.J.; Sollie, K.M.; van Veldhuisen, D.J.; et al. Biological versus mechanical heart valve prosthesis during pregnancy in women with congenital heart disease. Int. J. Cardiol. 2018, 268, 106–112. [Google Scholar] [CrossRef]
- Kytö, V.; Ahtela, E.; Sipilä, J.; Rautava, P.; Gunn, J. Mechanical versus biological valve prosthesis for surgical aortic valve replacement in patients with infective endocarditis. Interact. CardioVasc. Thorac. Surg. 2019, 29, 386–392. [Google Scholar] [CrossRef]
- Palacios, A.R.; Menéndez, J.L.; Hycka, J.M.; García, M.M.; Barca, L.V.; Marzal, A.F.; Pérez, R.M.; de Anquín, E.O.; Andrade, I.G.; Hernández, T.C.; et al. Which type of valve should we use in tricuspid position? Long-term comparison between mechanical and biological valves. J. Cardiovasc. Surg. 2017, 58, 739–746. [Google Scholar] [CrossRef]
- Lubiszewska, B.; Rozanski, J.; Szufladowicz, M.; Szaroszyk, W.; Hoffman, P.; Ksiezycka, E.; Rydlewska-Sadowska, W.; Ruzyllo, W. Mechanical valve replacement in congenital heart disease in children. J. Heart Valve Dis. 1999, 8, 74–79. [Google Scholar]
- Hettich, I.; Deutsch, M.A.; Badiu, C.; Krane, M.; Lange, R.; Bleiziffer, S.; Kottmaier, M. Quality of Life and Anxiety in Younger Patients after Biological versus Mechanical Aortic Valve Replacement. Thorac. Cardiovasc. Surg. 2016, 65, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Pragt, H.; van Melle, J.P.; Javadikasgari, H.; Seo, D.M.; Stulak, J.M.; Knez, I.; Hörer, J.; Muñoz-Guijosa, C.; Dehaki, M.G.; Shin, H.J.; et al. Mechanical valves in the pulmonary position: An international retrospective analysis. J. Thorac. Cardiovasc. Surg. 2017, 154, 1371–1378.e1. [Google Scholar] [CrossRef] [PubMed]
- Toma, M.; Singh-Gryzbon, S.; Frankini, E.; Wei, Z.A.; Yoganathan, A.P. Clinical Impact of Computational Heart Valve Models. Materials 2022, 15, 3302. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.M.; O’Brien, S.M.; Wu, C.; Sikora, J.A.H.; Griffith, B.P.; Gammie, J.S. Isolated aortic valve replacement in North America comprising 108,687 patients in 10 years: Changes in risks, valve types, and outcomes in the Society of Thoracic Surgeons National Database. J. Thorac. Cardiovasc. Surg. 2009, 137, 82–90. [Google Scholar] [CrossRef]
- Chiang, Y.P.; Chikwe, J.; Moskowitz, A.J.; Itagaki, S.; Adams, D.H.; Egorova, N.N. Survival and Long-term Outcomes Following Bioprosthetic vs Mechanical Aortic Valve Replacement in Patients Aged 50 to 69 Years. JAMA 2014, 312, 1323. [Google Scholar] [CrossRef]
- Isaacs, A.J.; Shuhaiber, J.; Salemi, A.; Isom, O.W.; Sedrakyan, A. National trends in utilization and in-hospital outcomes of mechanical versus bioprosthetic aortic valve replacements. J. Thorac. Cardiovasc. Surg. 2015, 149, 1262–1269.e3. [Google Scholar] [CrossRef]
- Beckmann, A.; Meyer, R.; Lewandowski, J.; Markewitz, A.; Blaßfeld, D.; Böning, A. German Heart Surgery Report 2021: The Annual Updated Registry of the German Society for Thoracic and Cardiovascular Surgery. Thorac. Cardiovasc. Surg. 2022, 70, 362–376. [Google Scholar] [CrossRef] [PubMed]
- Tillquist, M.N.; Maddox, T. Cardiac crossroads: Deciding between mechanical or bioprosthetic heart valve replacement. Patient Prefer. Adherence 2011, 5, 91–99. [Google Scholar] [CrossRef]
- Myers, P.O.; Mokashi, S.A.; Horgan, E.; Borisuk, M.; Mayer, J.E.; del Nido, P.J.; Baird, C.W. Outcomes after mechanical aortic valve replacement in children and young adults with congenital heart disease. J. Thorac. Cardiovasc. Surg. 2019, 157, 329–340. [Google Scholar] [CrossRef]
- Javadikasgari, H.; Chemtob, R.A.; Gillinov, A.M.; Pettersson, G.B.; Lowry, A.M.; Desai, M.Y.; Svensson, L.G.; Blackstone, E.H.; Wierup, P. Outcomes of mitral valve re-replacement for bioprosthetic structural valve deterioration. J. Thorac. Cardiovasc. Surg. 2022, 163, 1804–1812.e5. [Google Scholar] [CrossRef]
- Van Geldorp, M.W.; Jamieson, W.E.; Kappetein, A.P.; Ye, J.; Fradet, G.J.; Eijkemans, M.J.; Grunkemeier, G.L.; Bogers, A.J.; Takkenberg, J.J. Patient outcome after aortic valve replacement with a mechanical or biological prosthesis: Weighing lifetime anticoagulant-related event risk against reoperation risk. J. Thorac. Cardiovasc. Surg. 2009, 137, 881–886.e5. [Google Scholar] [CrossRef] [PubMed]
- Dangas, G.D.; Tijssen, J.G.; Wöhrle, J.; Søndergaard, L.; Gilard, M.; Möllmann, H.; Makkar, R.R.; Herrmann, H.C.; Giustino, G.; Baldus, S.; et al. A Controlled Trial of Rivaroxaban after Transcatheter Aortic-Valve Replacement. N. Engl. J. Med. 2020, 382, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Guimarães, P.O.; Pokorney, S.D.; Lopes, R.D.; Wojdyla, D.M.; Gersh, B.J.; Giczewska, A.; Carnicelli, A.; Lewis, B.S.; Hanna, M.; Wallentin, L.; et al. Efficacy and safety of apixaban vs warfarin in patients with atrial fibrillation and prior bioprosthetic valve replacement or valve repair: Insights from the ARISTOTLE trial. Clin. Cardiol. 2019, 42, 568–571. [Google Scholar] [CrossRef] [PubMed]
- Gerfer, S.; Djordjevic, I.; Eghbalzadeh, K.; Mader, N.; Wahlers, T.; Kuhn, E. Direct oral anticoagulation in atrial fibrillation and heart valve surgery—A meta-analysis and systematic review. Ther. Adv. Cardiovasc. Dis. 2022, 16, 175394472210939. [Google Scholar] [CrossRef]
- Karchmer, A.W.; Longworth, D.L. Infections of intracardiac devices. Infect. Dis. Clin. N. Am. 2002, 16, 477–505. [Google Scholar] [CrossRef]
- Lakkas, L.; Serim, B.D.; Fotopoulos, A.; Iakovou, I.; Doumas, A.; Korkmaz, U.; Michalis, L.K.; Sioka, C. Infection of cardiac prosthetic valves and implantable electronic devices: Early diagnosis and treatment. Acta Cardiol. 2021, 76, 569–575. [Google Scholar] [CrossRef]
- Heimberger, T.; RJ, D. Infections of prosthetic heart valves and cardiac pacemakers. Infect. Dis. Clin. N. Am. 1989, 3, 221–245. [Google Scholar] [CrossRef]
- Mateos Gaitán, R.; Boix-Palop, L.; Muñoz García, P.; Mestres, C.A.; Marín Arriaza, M.; Pedraz Prieto, Á.; de Alarcón Gonzalez, A.; Gutiérrez Carretero, E.; Hernández Meneses, M.; Goenaga Sánchez, M.Á.; et al. Infective endocarditis in patients with cardiac implantable electronic devices: A nationwide study. Europace 2020, 22, 1062–1070. [Google Scholar] [CrossRef]
- Anantha-Narayanan, M.; Reddy, Y.N.V.; Sundaram, V.; Murad, M.H.; Erwin, P.J.; Baddour, L.M.; Schaff, H.V.; Nishimura, R.A. Endocarditis risk with bioprosthetic and mechanical valves: Systematic review and meta-analysis. Heart 2020, 106, 1413–1419. [Google Scholar] [CrossRef]
- Galar, A.; Weil, A.A.; Dudzinski, D.M.; Muñoz, P.; Siedner, M.J. Methicillin-resistant Staphylococcus aureus prosthetic valve endocarditis: Pathophysiology, epidemiology, clinical presentation, diagnosis, and management. Clin. Microbiol. Rev. 2019, 32, e00041-18. [Google Scholar] [CrossRef]
- Maraj, R.; Jacobs, L.E.; Ioli, A.; Kotler, M.N. Evaluation of hemolysis in patients with prosthetic heart valves. Clin. Cardiol. 1998, 21, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Soccio, M.; D’Ambrosio, C.; De Caterina, R. Hemolysis following valve surgery. Ital. Heart J. Suppl. 2003, 4, 807–813. [Google Scholar] [PubMed]
- Simard, T.; Thangarasa, T.; Di Santo, P.; Labinaz, A.; Hibbert, B. The balloon impasse sign in percutaneous transvenous mitral valvuloplasty. Oxf. Med. Case Rep. 2020, 2020, omaa062. [Google Scholar] [CrossRef] [PubMed]
- Wenn, P.; Zeltser, R. Aortic Valve Disease. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Sharma, R.; Pellerin, D.; Gaze, D.C.; Mehta, R.L.; Gregson, H.; Streather, C.P.; Collinson, P.O.; Brecker, S.J. Mitral annular calcification predicts mortality and coronary artery disease in end stage renal disease. Atherosclerosis 2007, 191, 348–354. [Google Scholar] [CrossRef]
- Calabrò, P.; Gragnano, F.; Niccoli, G.; Marcucci, R.; Zimarino, M.; Spaccarotella, C.; Renda, G.; Patti, G.; Andò, G.; Moscarella, E.; et al. Antithrombotic Therapy in Patients Undergoing Transcatheter Interventions for Structural Heart Disease. Circulation 2021, 144, 1323–1343. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, L.; Amna, D.; Bukhari, S.S.H.; Javaid, R.; Sidiqui, R. Incidence and Different Risk Factors of Cardiac Surgery Associated Acute Kidney Injury. Pak. Armed Forces Med J. 2021, 70, S814–S818. [Google Scholar] [CrossRef]
- Hathcock, J.J. Flow Effects on Coagulation and Thrombosis. Arterioscler. Thromb. Vasc. Biol. 2006, 26, 1729–1737. [Google Scholar] [CrossRef]
- Madukauwa-David, I.D.; Sadri, V.; Midha, P.A.; Babaliaros, V.; Sharma, R.; Makkar, R.; Yoganathan, A.P. Might Coronary Flow Influence Transcatheter Heart Valve Neo-Sinus Thrombosis? Circ. Cardiovasc. Interv. 2019, 12, e008005. [Google Scholar] [CrossRef]
- Hollenhorst, M.A.; Battinelli, E.M. Thrombosis, Hypercoagulable States, and Anticoagulants. Prim. Care Clin. Off. Pract. 2016, 43, 619–635. [Google Scholar] [CrossRef]
- Hollander, K.; Joshi, B. Bioprosthetic valve thrombosis in carcinoid heart disease. Ann. Card. Anaesth. 2019, 22, 79–82. [Google Scholar] [CrossRef]
- Kronborg, J.; Svelander, F.; Eriksson-Lidbrink, S.; Lindström, L.; Homs-Pons, C.; Lucor, D.; Hoffman, J. Computational Analysis of Flow Structures in Turbulent Ventricular Blood Flow Associated With Mitral Valve Intervention. Front. Physiol. 2022, 13, 806534. [Google Scholar] [CrossRef]
- Hatoum, H.; Lilly, S.; Maureira, P.; Crestanello, J.; Dasi, L.P. The hemodynamics of transcatheter aortic valves in transcatheter aortic valves. J. Thorac. Cardiovasc. Surg. 2021, 161, 565–576.e2. [Google Scholar] [CrossRef]
- Kalińczuk, Ł.; Zieliński, K.; Witkowski, A.; Mintz, G.S. Incomplete apposition of a transcatheter aortic valve replacement frame associated with late subclinical leaflet thrombosis. Kardiol. Pol. 2020, 78, 1289–1290. [Google Scholar] [CrossRef] [PubMed]
- Leguay, D.; Duval, S.; Leroux, M.; Monnier, A.; Davienne, Y.; Brasselet, C. Thrombose de valve post-TAVI. Ann. Cardiol. D’Angéiologie 2017, 66, 447–452. [Google Scholar] [CrossRef]
- Dasi, L.P.; Simon, H.A.; Sucosky, P.; Yoganathan, A.P. Fluid Mechanics of Artificial Heart Valves. Clin. Exp. Pharmacol. Physiol. 2009, 36, 225–237. [Google Scholar] [CrossRef]
- Gopal, S.; Hauser, J.; Mahboobi, S. Mechanical Aortic Valve Replacement. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Melton, N.; Soleimani, B.; Dowling, R. Current Role of the Total Artificial Heart in the Management of Advanced Heart Failure. Curr. Cardiol. Rep. 2019, 21, 142. [Google Scholar] [CrossRef]
- Lee, H.S.; Tsukiya, T.; Homma, A.; Taenaka, Y.; Tatsumi, E.; Takano, H. Closing behavior of the mechanical heart valve in a total artificial heart. J. Artif. Organs 2003, 6, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Becker, R.C. Bridging Anticoagulation with Mechanical Heart Valves: Current Guidelines and Clinical Decisions. Curr. Cardiol. Rep. 2020, 22. [Google Scholar] [CrossRef] [PubMed]
- Pagnesi, M.; Moroni, F.; Beneduce, A.; Giannini, F.; Colombo, A.; Weisz, G.; Latib, A. Thrombotic Risk and Antithrombotic Strategies After Transcatheter Mitral Valve Replacement. JACC Cardiovasc. Interv. 2019, 12, 2388–2401. [Google Scholar] [CrossRef]
- Hammermeister, K.E.; Sethi, G.K.; Henderson, W.G.; Oprian, C.; Kim, T.; Rahimtoola, S. A Comparison of Outcomes in Men 11 Years after Heart-Valve Replacement with a Mechanical Valve or Bioprosthesis. N. Engl. J. Med. 1993, 328, 1289–1296. [Google Scholar] [CrossRef]
- Yao, H.; Miyamoto, T.; Mukai, S.; Yamamura, M.; Tanaka, H.; Nakagawa, T.; Ryomoto, M.; Inai, Y.; Yoshioka, Y.; Kaji, M. Long-term results of mitral valve replacement: Biological xenograft versus mechanical valves. J. Artif. Organs 2003, 6, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Bluestein, D.; Yin, W.; Affeld, K.; Jesty, J. Flow-induced platelet activation in mechanical heart valves. J. Heart Valve Dis. 2004, 13, 501–508. [Google Scholar] [PubMed]
- Wei, Z.A.; Sonntag, S.J.; Toma, M.; Singh-Gryzbon, S.; Sun, W. Computational Fluid Dynamics Assessment Associated with Transcatheter Heart Valve Prostheses: A Position Paper of the ISO Working Group. Cardiovasc. Eng. Technol. 2018, 9, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Roudaut, R.; Serri, K.; Lafitte, S. Thrombosis of prosthetic heart valves: Diagnosis and therapeutic considerations. Heart 2007, 93, 137–142. [Google Scholar] [CrossRef]
- Allen, A.L.; Lucas, J.; Parra, D.; Spoutz, P.; Kibert, J.L.; Ragheb, B.; Chia, L.; Sipe, A. Shifting the Paradigm: A Population Health Approach to the Management of Direct Oral Anticoagulants. J. Am. Heart Assoc. 2021, 10, e022758. [Google Scholar] [CrossRef] [PubMed]
- VHA Directive 1108.16. In Anticoagulation Therapy Management; Pharmacy Benefits Management Services and Office of Patient Care Services, Veterans Health Administration, Department of Veterans Affairs: West Haven, CT, USA, 2021.
- Lim, W.Y.; Lloyd, G.; Bhattacharyya, S. Mechanical and surgical bioprosthetic valve thrombosis. Heart 2017, 103, 1934–1941. [Google Scholar] [CrossRef] [PubMed]
- Zbroński, K.; Sabiniewicz, R.; Scisło, P.; Siennicka, A.; Kochman, J.; Huczek, Z. Percutaneous retrograde paramitral leak closure through a mechanical aortic valve. Kardiol. Pol. 2019, 77, 482–483. [Google Scholar] [CrossRef]
- Takeshita, M.; Arai, H.; Nagaoka, E.; Mizuno, T. Papillary muscle relocation and annular repositioning for functional tricuspid regurgitation. JTCVS Tech. 2020, 3, 162–165. [Google Scholar] [CrossRef]
- Flameng, W.; Herijgers, P.; Bogaerts, K. Recurrence of Mitral Valve Regurgitation After Mitral Valve Repair in Degenerative Valve Disease. Circulation 2003, 107, 1609–1613. [Google Scholar] [CrossRef]
- Praz, F.; Brugger, N.; Kassar, M.; Hunziker, L.; Moschovitis, A.; Stortecky, S.; Reineke, D.; Pilgrim, T.; Windecker, S. Interventional treatment of mitral valve regurgitation: An alternative to surgery? Swiss Med. Wkly. 2019, 149, w20023. [Google Scholar] [CrossRef]
- Zeballos-Palacios, C.L.; Hargraves, I.G.; Noseworthy, P.A.; Branda, M.E.; Kunneman, M.; Burnett, B.; Gionfriddo, M.R.; McLeod, C.J.; Gorr, H.; Brito, J.P.; et al. Developing a Conversation Aid to Support Shared Decision Making: Reflections on Designing Anticoagulation Choice. Mayo Clin. Proc. 2019, 94, 686–696. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.J.; Singer, D.E.; Glynn, R.J.; Blackley, S.; Zhou, L.; Liu, J.; Dube, G.; Oertel, L.B.; Schneeweiss, S. Prediction Score for Anticoagulation Control Quality Among Older Adults. J. Am. Heart Assoc. 2017, 6, e006814. [Google Scholar] [CrossRef] [PubMed]
- Umerah, C.; Momodu, I. Anticoagulation. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Yee, J.; Kaide, C. Emergency Reversal of Anticoagulation. West. J. Emerg. Med. 2019, 20, 770–783. [Google Scholar] [CrossRef] [PubMed]
- Kornhall, L.; Wikander, D.; Strandberg, K.; Berntorp, E.; Schött, U. ROTEM and vitro reversal of warfarin with APCC. J. Cardiovasc. Med. Cardiol. 2019, 6, 6–11. [Google Scholar] [CrossRef]
- Gulseth, M.P. Overview of direct oral anticoagulant therapy reversal. Am. J. Health-Syst. Pharm. 2016, 73, s5–s13. [Google Scholar] [CrossRef] [PubMed]
- Simon, E.M.; Streitz, M.J.; Sessions, D.J.; Kaide, C.G. Anticoagulation Reversal. Emerg. Med. Clin. N. Am. 2018, 36, 585–601. [Google Scholar] [CrossRef]
- Ansell, J.E.; Laulicht, B.E.; Bakhru, S.H.; Hoffman, M.; Steiner, S.S.; Costin, J.C. Ciraparantag safely and completely reverses the anticoagulant effects of low molecular weight heparin. Thromb. Res. 2016, 146, 113–118. [Google Scholar] [CrossRef]
- Desai, N.R.; Cornutt, D. Reversal agents for direct oral anticoagulants: Considerations for hospital physicians and intensivists. Hosp. Pract. 2019, 47, 113–122. [Google Scholar] [CrossRef]
- Antoniou, S. Rivaroxaban for the treatment and prevention of thromboembolic disease. J. Pharm. Pharmacol. 2015, 67, 1119–1132. [Google Scholar] [CrossRef]
- Clark, N.P. Role of the anticoagulant monitoring service in 2018: Beyond warfarin. Hematol. Am. Soc. Hematol. Educ. Program 2018, 2018, 348–352. [Google Scholar] [CrossRef]
- Verheugt, F.W.A. Anticoagulant management in the cardiovascular setting. Fundam. Clin. Pharmacol. 2012, 26, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Czuprynska, J.; Patel, J.P.; Arya, R. Current challenges and future prospects in oral anticoagulant therapy. Br. J. Haematol. 2017, 178, 838–851. [Google Scholar] [CrossRef] [PubMed]
- Leow, A.S.T.; Sia, C.H.; Tan, B.Y.Q.; Loh, J.P.Y. A meta-summary of case reports of non-vitamin K antagonist oral anticoagulant use in patients with left ventricular thrombus. J. Thromb. Thrombolysis 2018, 46, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Von Vajna, E.; Alam, R.; So, T.Y. Current Clinical Trials on the Use of Direct Oral Anticoagulants in the Pediatric Population. Cardiol. Ther. 2016, 5, 19–41. [Google Scholar] [CrossRef] [PubMed]
- Lauffenburger, J.C.; Farley, J.F.; Gehi, A.K.; Rhoney, D.H.; Brookhart, M.A.; Fang, G. Effectiveness and Safety of Dabigatran and Warfarin in Real-World US Patients With Non-Valvular Atrial Fibrillation: A Retrospective Cohort Study. J. Am. Heart Assoc. 2015, 4, e001798. [Google Scholar] [CrossRef]
- Fonseca, J.P.; Pereiro, T.; dos Santos, D.P.; Correia, J.M.; Capelo, J.; Carragoso, A. Successful Management of Prosthetic Valve Brucella Endocarditis with Antibiotherapy Alone. Eur. J. Case Rep. Intern. Med. 2018, 5, 000808. [Google Scholar] [CrossRef]
- McGettigan, P.; Henry, D. Use of Non-Steroidal Anti-Inflammatory Drugs That Elevate Cardiovascular Risk: An Examination of Sales and Essential Medicines Lists in Low-, Middle-, and High-Income Countries. PLoS Med. 2013, 10, e1001388. [Google Scholar] [CrossRef]
- Nopp, S.; Kraemmer, D.; Ay, C. Factor XI Inhibitors for Prevention and Treatment of Venous Thromboembolism: A Review on the Rationale and Update on Current Evidence. Front. Cardiovasc. Med. 2022, 9, 903029. [Google Scholar] [CrossRef]
- Weitz, J.I.; Bauersachs, R.; Becker, B.; Berkowitz, S.D.; Freitas, M.C.S.; Lassen, M.R.; Metzig, C.; Raskob, G.E. Effect of Osocimab in Preventing Venous Thromboembolism Among Patients Undergoing Knee Arthroplasty. JAMA 2020, 323, 130. [Google Scholar] [CrossRef]
- Desborough, M.; Oakland, K.; Landoni, G.; Crivellari, M.; Doree, C.; Estcourt, L.; Stanworth, S. Desmopressin for treatment of platelet dysfunction and reversal of antiplatelet agents: A systematic review and meta-analysis of randomized controlled trials. J. Thromb. Haemost. 2017, 15, 263–272. [Google Scholar] [CrossRef]
- Vijayan, V.; Rachel, T. Pregnancy outcomes compared in women with mechanical heart valve replacements anticoagulated with warfarin and enoxaparin in pregnancy. Med. J. Malays. 2012, 67, 591–594. [Google Scholar]
- Saksena, D.; Muralidharan, S.; Mishra, Y.K.; Kanhere, V.; Mohanty, B.B.; Srivastava, C.P.; Mange, J.; Puranik, M.; Nair, M.P.; Goel, P.; et al. Anticoagulation management in patients with valve replacement. J. Assoc. Physicians India 2018, 66, 59–74. [Google Scholar] [PubMed]
- Gerfer, S.; Grandoch, M.; Wahlers, T.C.; Kuhn, E.W. Factor Xa Inhibitors for Patients after Mechanical Heart Valve Replacement? Thorac. Cardiovasc. Surg. 2023, 71, 189–194. [Google Scholar] [CrossRef]
- Eikelboom, J.W.; Connolly, S.J.; Brueckmann, M.; Granger, C.B.; Kappetein, A.P.; Mack, M.J.; Blatchford, J.; Devenny, K.; Friedman, J.; Guiver, K.; et al. Dabigatran versus Warfarin in Patients with Mechanical Heart Valves. N. Engl. J. Med. 2013, 369, 1206–1214. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.C.; Davidson, M.J.; Lamy, A.; Eikelboom, J.W. Antithrombotic management of patients with prosthetic heart valves: Current evidence and future trends. Lancet 2009, 374, 565–576. [Google Scholar] [CrossRef]
- Kovacs, M.J.; Wells, P.S.; Anderson, D.R.; Lazo-Langner, A.; Kearon, C.; Bates, S.M.; Blostein, M.; Kahn, S.R.; Schulman, S.; Sabri, E.; et al. Postoperative low molecular weight heparin bridging treatment for patients at high risk of arterial thromboembolism (PERIOP2): Double blind randomised controlled trial. BMJ 2021, 373, n1205. [Google Scholar] [CrossRef]
- Puskas, J.D.; Gerdisch, M.; Nichols, D.; Fermin, L.; Rhenman, B.; Kapoor, D.; Copeland, J.; Quinn, R.; Hughes, G.C.; Azar, H.; et al. Anticoagulation and Antiplatelet Strategies After On-X Mechanical Aortic Valve Replacement. J. Am. Coll. Cardiol. 2018, 71, 2717–2726. [Google Scholar] [CrossRef]
- Pengo, V.; Palareti, G.; Cucchini, U.; Molinatti, M.; Bono, R.D.; Baudo, F.; Ghirarduzzi, A.; Pegoraro, C.; Iliceto, S. Low-Intensity Oral Anticoagulant Plus Low-Dose Aspirin During the First Six Months Versus Standard-Intensity Oral Anticoagulant Therapy After Mechanical Heart Valve Replacement: A Pilot Study of Low-Intensity Warfarin and Aspirin in Cardiac Prostheses (LIWACAP). Clin. Appl. Thromb. 2007, 13, 241–248. [Google Scholar] [CrossRef]
- Turpie, A.; Gent, M.; Laupacis, A.; Latour, Y.; Gunstensen, J.; Basile, F.; Klimek, M.; Hirsh, J. A Comparison of Aspirin with Placebo in Patients Treated with Warfarin after Heart-Valve Replacement. N. Engl. J. Med. 1993, 329, 524–529. [Google Scholar] [CrossRef]
- Barnes, G.D. Combining antiplatelet and anticoagulant therapy in cardiovascular disease. Hematology 2020, 2020, 642–648. [Google Scholar] [CrossRef]
- Schaefer, J.K.; Errickson, J.; Gu, X.; Alexandris-Souphis, T.; Ali, M.A.; Haymart, B.; Kaatz, S.; Kline-Rogers, E.; Kozlowski, J.H.; Krol, G.D.; et al. Assessment of an Intervention to Reduce Aspirin Prescribing for Patients Receiving Warfarin for Anticoagulation. JAMA Netw. Open 2022, 5, e2231973. [Google Scholar] [CrossRef] [PubMed]
- Larson, E.A.; German, D.M.; Shatzel, J.; DeLoughery, T.G. Anticoagulation in the cardiac patient: A concise review. Eur. J. Haematol. 2018, 102, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Dauphin, C.; Legault, B.; Jaffeux, P.; Motreff, P.; Azarnoush, K.; Joly, H.; Geoffroy, É.; Aublet-Cuvelier, B.; Camilleri, L.; Lusson, J.R.; et al. Comparison of INR stability between self-monitoring and standard laboratory method: Preliminary results of a prospective study in 67 mechanical heart valve patients. Arch. Cardiovasc. Dis. 2008, 101, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Li, C.; Shen, J.; Wu, K.; Li, Y.; Liu, K.; Zhang, F.; Zhang, Z.; Li, Y.; Han, J.; et al. New Internet-Based Warfarin Anticoagulation Management Approach After Mechanical Heart Valve Replacement: Prospective, Multicenter, Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e29529. [Google Scholar] [CrossRef]
- Heneghan, C.; Ward, A.; Perera, R.; Bankhead, C.; Fuller, A.; Stevens, R.; Bradford, K.; Tyndel, S.; Alonso-Coello, P.; Ansell, J.; et al. Self-monitoring of oral anticoagulation: Systematic review and meta-analysis of individual patient data. Lancet 2012, 379, 322–334. [Google Scholar] [CrossRef]
- Mair, H.; Sachweh, J.; Sodian, R.; Brenner, P.; Schmoeckel, M.; Schmitz, C.; Reichart, B.; Daebritz, S. Long-term self-management of anticoagulation therapy after mechanical heart valve replacement in outside trial conditions. Interact. CardioVasc. Thorac. Surg. 2011, 14, 253–257. [Google Scholar] [CrossRef]
- Matchar, D.B.; Jacobson, A.; Dolor, R.; Edson, R.; Uyeda, L.; Phibbs, C.S.; Vertrees, J.E.; Shih, M.C.; Holodniy, M.; Lavori, P. Effect of Home Testing of International Normalized Ratio on Clinical Events. N. Engl. J. Med. 2010, 363, 1608–1620. [Google Scholar] [CrossRef]
- Zhang, L.; Zheng, X.; Long, Y.; Wu, M.; Chen, Y.; Yang, J.; Liu, Z.; Zhang, Z. D-dimer to guide the intensity of anticoagulation in Chinese patients after mechanical heart valve replacement: A randomized controlled trial. J. Thromb. Haemost. 2017, 15, 1934–1941. [Google Scholar] [CrossRef]
- McLintock, C. Anticoagulant choices in pregnant women with mechanical heart valves: Balancing maternal and fetal risks—The difference the dose makes. Thromb. Res. 2013, 131, S8–S10. [Google Scholar] [CrossRef]
- Adilova, L.R.; Shifman, E.M.; Adamian, L.V.; Liashko, E.S.; Tiul’kina, E.E. Anticoagulant therapy in pregnant women with mechanical prosthetic heart valves. Review of international clinical guidelines. Anesteziol. Reanimatol. 2013, 6, 62–66. [Google Scholar]
- Quinn, J.; Klemperer, K.V.; Brooks, R.; Peebles, D.; Walker, F.; Cohen, H. Use of high intensity adjusted dose low molecular weight heparin in women with mechanical heart valves during pregnancy: A single-center experience. Haematologica 2009, 94, 1608–1612. [Google Scholar] [CrossRef] [PubMed]
- Saeed, C.R.; Frank, J.B.; Pravin, M.; Aziz, R.H.; Serasheini, M.; Dominique, T.G. A Prospective Trial Showing the Safety of Adjusted-Dose Enoxaparin for Thromboprophylaxis of Pregnant Women With Mechanical Prosthetic Heart Valves. Clin. Appl. Thromb. 2010, 17, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Park, N.H.; Keum, D.Y.; Choi, S.Y.; Kwon, K.Y.; Cho, C.H. Low Molecular Weight Heparin Treatment in Pregnant Women with a Mechanical Heart Valve Prosthesis. J. Korean Med. Sci. 2007, 22, 258. [Google Scholar] [CrossRef] [PubMed]
- Santos, F.D.; Baris, L.; Varley, A.; Cornette, J.; Allam, J.; Steer, P.; Swan, L.; Gatzoulis, M.; Roos-Hesselink, J.; Johnson, M.R. Mechanical heart valves and pregnancy: Issues surrounding anticoagulation. Experience from two obstetric cardiac centres. Obstet. Med. 2020, 14, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Seshadri, N.; Goldhaber, S.Z.; Elkayam, U.; Grimm, R.A.; Groce, J.B.; Heit, J.A.; Spinler, S.A.; Turpie, A.G.; Bosker, G.; Klein, A.L. The clinical challenge of bridging anticoagulation with low-molecular-weight heparin in patients with mechanical prosthetic heart valves: An evidence-based comparative review focusing on anticoagulation options in pregnant and nonpregnant patients. Am. Heart J. 2005, 150, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.D.; Su, Y.J.; Chen, B.Y.; Cui, J.J.; Zhang, Z.L.; Xu, Q.; Gu, Z.C. The optimal anticoagulant therapy for mechanical heart valves in a gallbladder cancer patient with hepatic metastases. Medicine 2018, 97, e12368. [Google Scholar] [CrossRef] [PubMed]
- Yates, S.; Sarode, R. Reversal of Anticoagulant Effects in Patients with Intracerebral Hemorrhage. Curr. Neurol. Neurosci. Rep. 2014, 15, 504. [Google Scholar] [CrossRef]
- Kuramatsu, J.B.; Sembill, J.A.; Gerner, S.T.; Sprügel, M.I.; Hagen, M.; Roeder, S.S.; Endres, M.; Haeusler, K.G.; Sobesky, J.; Schurig, J.; et al. Management of therapeutic anticoagulation in patients with intracerebral haemorrhage and mechanical heart valves. Eur. Heart J. 2018, 39, 1709–1723. [Google Scholar] [CrossRef]
- AlKherayf, F.; Xu, Y.; Westwick, H.; Moldovan, I.D.; Wells, P.S. Timing of anticoagulant re-initiation following intracerebral hemorrhage in mechanical heart valves: Survey of neurosurgeons and thrombosis experts. Clin. Neurol. Neurosurg. 2017, 154, 23–27. [Google Scholar] [CrossRef]
- Romualdi, E.; Micieli, E.; Ageno, W.; Squizzato, A. Oral anticoagulant therapy in patients with mechanical heart valve and intracranial haemorrhage. A systematic review. Thromb. Haemost. 2009, 101, 290–297. [Google Scholar]
- Wijdicks, E.F.; Schievink, W.I.; Brown, R.D.; Mullany, C.J. The Dilemma of Discontinuation of Anticoagulation Therapy for Patients with Intracranial Hemorrhage and Mechanical Heart Valves. Neurosurgery 1998, 42, 769–772. [Google Scholar] [CrossRef]
- Shah, R.; Shah, D.; Koganti, S.; Davies, R. Intracerebral haemorrhage, anticoagulation and mechanical heart valves: What should I do next? Case Rep. 2013, 2013, bcr2013008639. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, M. Anticoagulant-Associated Intracerebral Hemorrhage. Semin. Neurol. 2010, 30, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Kuramatsu, J.B.; Gerner, S.T.; Schellinger, P.D.; Glahn, J.; Endres, M.; Sobesky, J.; Flechsenhar, J.; Neugebauer, H.; Jüttler, E.; Grau, A.; et al. Anticoagulant Reversal, Blood Pressure Levels, and Anticoagulant Resumption in Patients With Anticoagulation-Related Intracerebral Hemorrhage. JAMA 2015, 313, 824. [Google Scholar] [CrossRef] [PubMed]
- Bashline, M.J.; Chaudhary, R.; Wong, T.C.; Okonkwo, D.O.; Aiyer, A. Examining the Duration and Safety of Withholding Anticoagulation After an Intracerebral Hemorrhage in Patients With Mechanical Heart Valves. Am. J. Cardiol. 2022, 177, 164–166. [Google Scholar] [CrossRef]
- Colantino, A.; Jaffer, A.K.; Brotman, D.J. Resuming anticoagulation after hemorrhage: A practical approach. Clevel. Clin. J. Med. 2015, 82, 245–256. [Google Scholar] [CrossRef]
- Flaherty, M.L.; Tao, H.; Haverbusch, M.; Sekar, P.; Kleindorfer, D.; Kissela, B.; Khatri, P.; Stettler, B.; Adeoye, O.; Moomaw, C.J.; et al. Warfarin use leads to larger intracerebral hematomas. Neurology 2008, 71, 1084–1089. [Google Scholar] [CrossRef]
- Flibotte, J.J.; Hagan, N.; O’Donnell, J.; Greenberg, S.M.; Rosand, J. Warfarin, hematoma expansion, and outcome of intracerebral hemorrhage. Neurology 2004, 63, 1059–1064. [Google Scholar] [CrossRef]
- Oguz, M.; Ayaz, A.; Adin, M.E. Warfarin-associated intracranial haemorrhage in pregnant woman with double mechanical valve replacement: A case presentation. BMC Cardiovasc. Disord. 2020, 20. [Google Scholar] [CrossRef]
- Maingi, M.; Glynn, M.F.; Scully, H.E.; Graham, A.F.; Floras, J.S. Spontaneous spinal epidural hematoma in a patient with a mechanical aortic valve taking warfarin. Can. J. Cardiol. 1995, 11, 429–432. [Google Scholar]
- Eikelboom, J.W.; Bosch, J.; Hart, R.G. Rapid reversal of haematoma expansion associated with vitamin K antagonists. Lancet Neurol. 2016, 15, 535–537. [Google Scholar] [CrossRef] [PubMed]
- Steiner, T.; Poli, S.; Griebe, M.; Hüsing, J.; Hajda, J.; Freiberger, A.; Bendszus, M.; Bösel, J.; Christensen, H.; Dohmen, C.; et al. Fresh frozen plasma versus prothrombin complex concentrate in patients with intracranial haemorrhage related to vitamin K antagonists (INCH): A randomised trial. Lancet Neurol. 2016, 15, 566–573. [Google Scholar] [CrossRef]
- AlKherayf, F.; Xu, Y.; Gandara, E.; Westwick, H.; Moldovan, I.D.; Wells, P.S. Timing of vitamin K antagonist re-initiation following intracranial hemorrhage in mechanical heart valves: Systematic review and meta-analysis. Thromb. Res. 2016, 144, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Wan, A.; Butcher, K.; Hodgson, M.; Schultz, K.; Bungard, T.J. Warfarin Reinitiation After Intracranial Hemorrhage: A Case Series of Heart Valve Patients. Can. J. Neurol. Sci./J. Can. Des Sci. Neurol. 2019, 47, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Becattini, C.; Sembolini, A.; Paciaroni, M. Resuming anticoagulant therapy after intracerebral bleeding. Vasc. Pharmacol. 2016, 84, 15–24. [Google Scholar] [CrossRef] [PubMed]
| Mechanical | Bioprosthetic | |
|---|---|---|
| Percentage of use [56,57,58,59] | ≈20% | ≈80% |
| Durability [60] | up to 30 years | up to 15 years |
| Need for Replacement/Repair [61,62] | Lower Risk | Higher Risk |
| Morbidity/Mortality with Reoperation [63] | Higher Risk | Lower Risk |
| Thromboembolism [2,64] | Higher Risk | Lower Risk |
| Anticoagulation [65,66] | Lifelong | 3+ months |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, S.; Syed, F.; Toma, M. Management of Intracranial Hemorrhage in the Setting of Mechanical Heart Valve Replacement Therapy. Appl. Mech. 2023, 4, 644-667. https://doi.org/10.3390/applmech4020033
Khan S, Syed F, Toma M. Management of Intracranial Hemorrhage in the Setting of Mechanical Heart Valve Replacement Therapy. Applied Mechanics. 2023; 4(2):644-667. https://doi.org/10.3390/applmech4020033
Chicago/Turabian StyleKhan, Sahar, Faiz Syed, and Milan Toma. 2023. "Management of Intracranial Hemorrhage in the Setting of Mechanical Heart Valve Replacement Therapy" Applied Mechanics 4, no. 2: 644-667. https://doi.org/10.3390/applmech4020033
APA StyleKhan, S., Syed, F., & Toma, M. (2023). Management of Intracranial Hemorrhage in the Setting of Mechanical Heart Valve Replacement Therapy. Applied Mechanics, 4(2), 644-667. https://doi.org/10.3390/applmech4020033






