Evidence-Based Management of Burns: A Narrative Review of Evolving Practices
Abstract
1. Introduction
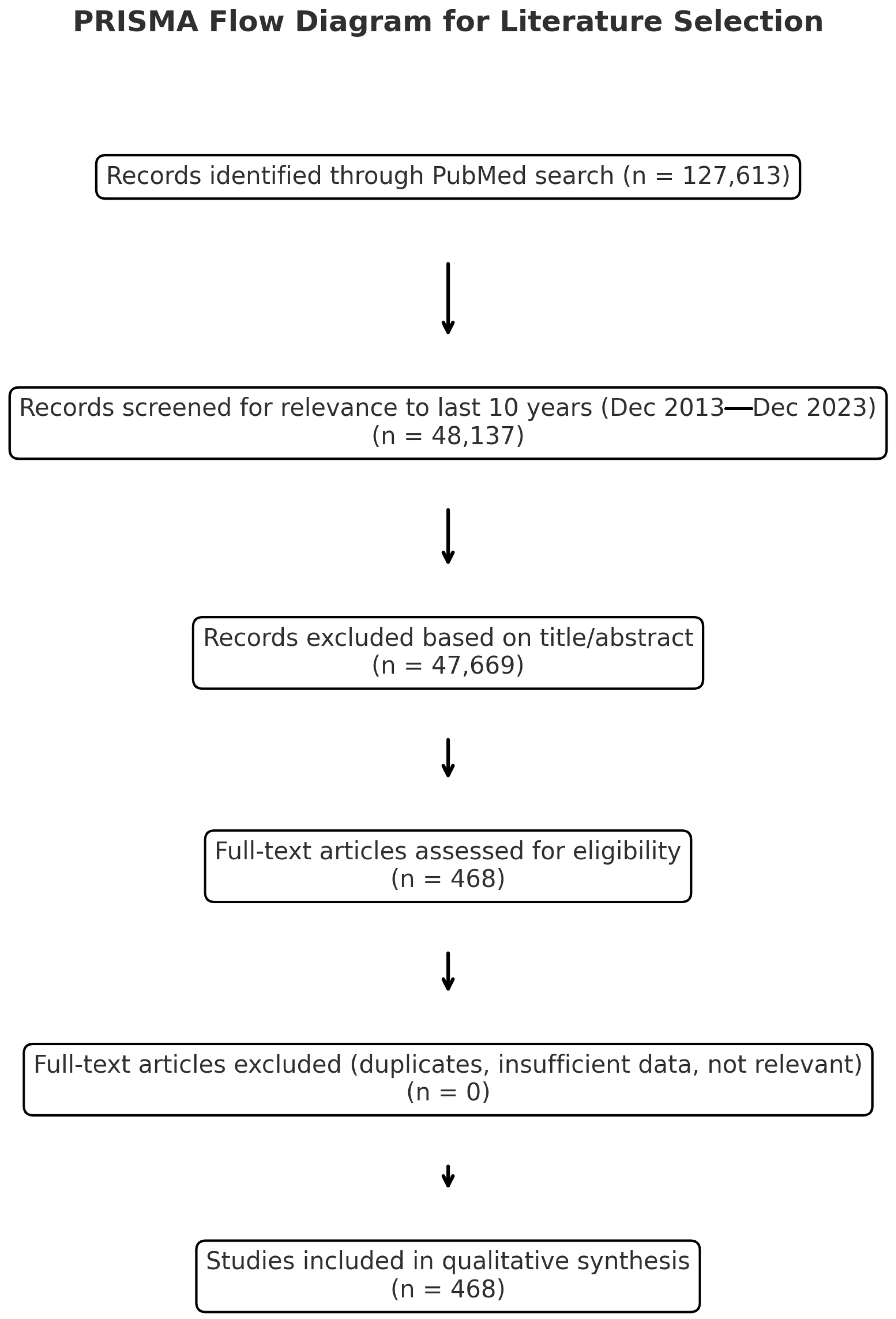
2. Materials and Methods
3. Review
3.1. Pharmacological Adjuncts in Burn Recovery
3.1.1. Oxandrolone
3.1.2. Propranolol
3.1.3. Chemical Venous Thromboembolism Prophylaxis
3.1.4. Tranexamic Acid
3.1.5. Summary
3.2. Debridement Innovations
3.2.1. Bromelain-Based Enzymatic Debridement
3.2.2. Summary
3.3. Skin Replacement and Regenerative Technologies
3.3.1. Epidermal Cell Sprays
3.3.2. Dermal Substitutes
3.3.3. Cultured Bilayered Skin Equivalents
3.3.4. Summary
3.4. Energy and Metabolic Modulation
3.4.1. Indirect Calorimetry and Metabolic Modulation
3.4.2. Summary
3.5. Scar Modulation and Functional Recovery
3.5.1. Fractional CO2 Laser Therapy
3.5.2. Rehabilitation and Functional Recovery
3.5.3. Summary
3.6. Emerging Technologies and Future Directions
3.6.1. 3D Bioprinting and Tissue Engineering
3.6.2. Artificial Intelligence and Digital Burn Assessment
3.6.3. Precision Burn Care
3.6.4. Summary
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 3D | 3 Dimensional |
| CO2 | Carbon dioxide |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| AAS | Anabolic Androgen Steroids |
| TBSA | Total Body Surface Area |
| RCT | Randomised Control Trial |
| FDA | Food and Drug Administration |
| VTE | Venous thromboembolism |
| TXA | Tranexamic Acid |
| STSG | Split Thickness Skin Graft |
| BTM | Biodegradable Temporizing Matrix |
| NPWT | Negative Pressure Wound Therapy |
| rhGH | Recombinant Human Growth Hormone |
| IGF-1 | Insulin Growth Factor 1 |
| IGFBP-3 | Insulin Growth Factor Binding Protein 3 |
| PROM | Patient Reported Outcome Measure |
| POSAS | Patient and Observer Scar Assessment Scale |
| AI | Artificial Intelligence |
| COVID-19 | Coronavirus Disease 2019 |
References
- Yakupu, A.; Zhang, J.; Dong, W.; Song, F.; Dong, J.; Lu, S. The epidemiological characteristic and trends of burns globally. BMC Public Health 2022, 22, 1596. [Google Scholar] [CrossRef]
- Radzikowska-Buchner, E.; Lopuszynska, I.; Flieger, W.; Tobiasz, M.; Maciejewski, R.; Flieger, J. An Overview of Recent Developments in the Management of Burn Injuries. Int. J. Mol. Sci. 2023, 24, 16357. [Google Scholar] [CrossRef]
- Ring, J.; Heinelt, M.; Sharma, S.; Letourneau, S.; Jeschke, M.G. Oxandrolone in the Treatment of Burn Injuries: A Systematic Review and Meta-analysis. J. Burn. Care Res. 2020, 41, 190–199. [Google Scholar] [CrossRef]
- Shahrokhi, S.; Jeschke, M.G. Metabolic and Nutritional Support. Surg. Clin. N. Am. 2023, 103, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Hirche, C.; Kreken Almeland, S.; Dheansa, B.; Fuchs, P.; Governa, M.; Hoeksema, H.; Korzeniowski, T.; Lumenta, D.B.; Marinescu, S.; Martinez-Mendez, J.R.; et al. Eschar removal by bromelain based enzymatic debridement (Nexobrid®) in burns: European consensus guidelines update. Burns 2020, 46, 782–796. [Google Scholar] [CrossRef] [PubMed]
- Ter Horst, B.; Chouhan, G.; Moiemen, N.S.; Grover, L.M. Advances in keratinocyte delivery in burn wound care. Adv. Drug Deliv. Rev. 2018, 123, 18–32. [Google Scholar] [CrossRef]
- Lou, J.; Zhu, X.; Xiang, Z.; Song, J.; Huang, N.; Jin, G.; Cui, S.; Fan, Y.; Li, J. Efficacy of Acellular Dermal Matrix in Improving Clinical Outcomes in Pediatric Burns: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Pediatr. Surg. 2025, 60, 162270. [Google Scholar] [CrossRef] [PubMed]
- Abouzeid, C.; Friedstat, J.; Goldstein, R.; Chacon, K.L.; Mehta, A.; Sheridan, R.L.; Schulz, J.T.; Kazis, L.; Goverman, J.; Ryan, C.M.; et al. Fractional CO2 Laser for Burn Scars: A Comparison of Patient-Reported Outcomes Between Those with and without Laser Treatment. J. Burn. Care Res. 2024, 45, 1505–1512. [Google Scholar] [CrossRef]
- Partain, K.P.; Fabia, R.; Thakkar, R.K. Pediatric burn care: New techniques and outcomes. Curr. Opin. Pediatr. 2020, 32, 405–410. [Google Scholar] [CrossRef]
- Gus, E.I.; Shahrokhi, S.; Jeschke, M.G. Anabolic and anticatabolic agents used in burn care: What is known and what is yet to be learned. Burns 2020, 46, 19–32. [Google Scholar] [CrossRef]
- Kopel, J.; Sorensen, G.; Griswold, J. A Reappraisal of Oxandrolone in Burn Management. J. Pharm. Technol. 2022, 38, 232–238. [Google Scholar] [CrossRef]
- Ojeda, S.; Blumenthal, E.; Stevens, P.; Andersen, C.R.; Robles, L.; Herndon, D.N.; Meyer, W.J., 3rd. The Safety and Efficacy of Propranolol in Reducing the Hypermetabolic Response in the Pediatric Burn Population. J. Burn. Care Res. 2018, 39, 963–969. [Google Scholar] [CrossRef]
- Bhatti, A.; Shah, S.; Shahzaib, M.; Nadeem, M.A.; Shaikh, A.; Rehman, H.U.; Rizvi, S.S.; Khan, M.; Singh, J.D.; Mahfooz, F.; et al. The Effectiveness and Safety of Beta Antagonists in Patients with Burns: An Updated Meta-Analysis. Am. Surg. 2025, 91, 772–783. [Google Scholar] [CrossRef]
- Fernando, S.M.; Tran, A.; Cheng, W.; Sadeghirad, B.; Arabi, Y.M.; Cook, D.J.; Moller, M.H.; Mehta, S.; Fowler, R.A.; Burns, K.E.A.; et al. VTE Prophylaxis in Critically Ill Adults: A Systematic Review and Network Meta-analysis. Chest 2022, 161, 418–428. [Google Scholar] [CrossRef]
- Greenhalgh, D.G.; Hill, D.M.; Burmeister, D.M.; Gus, E.I.; Cleland, H.; Padiglione, A.; Holden, D.; Huss, F.; Chew, M.S.; Kubasiak, J.C.; et al. Surviving Sepsis After Burn Campaign. Burns 2023, 49, 1487–1524. [Google Scholar] [CrossRef]
- Fijany, A.J.; Givechian, K.B.; Zago, I.; Olsson, S.E.; Boctor, M.J.; Gandhi, R.R.; Pekarev, M. Tranexamic acid in burn surgery: A systematic review and meta-analysis. Burns 2023, 49, 1249–1259. [Google Scholar] [CrossRef]
- Vermaak, P.V.; D’Asta, F.; Provins, J.; Farr, M.; Wilson, Y.T. Thromboprophylaxis in adult and paediatric burn patients: A survey of practice in the United Kingdom. Burns 2019, 45, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, B.; Fischer, S.; Pieper, D.; Mathes, T.; Kneser, U.; Hirche, C. Evidence and Trends in Burn Wound Debridement: An Evidence Map. Plast. Surg. 2020, 28, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Norbury, W.; Herndon, D.N.; Tanksley, J.; Jeschke, M.G.; Finnerty, C.C. Infection in Burns. Surg. Infect. 2016, 17, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Kwa, K.A.A.; Goei, H.; Breederveld, R.S.; Middelkoop, E.; van der Vlies, C.H.; van Baar, M.E. A systematic review on surgical and nonsurgical debridement techniques of burn wounds. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 1752–1762. [Google Scholar] [CrossRef]
- De Freitas, L.R.; Udoma-Udofa, O.C.; Reginato, P.H.; Mitsui, H.C.; Provinciatto, H.; Torres, F.C. Bromelain-Based Enzymatic Debridement Versus Standard of Care in Deep Burn Injuries: A Systematic Review and Meta-Analysis. J. Burn. Care Res. 2025, 46, 123–131. [Google Scholar] [CrossRef]
- Grunzweig, K.A.; Ascha, M.; Kumar, A.R. Fibrin tissue sealant and minor skin grafts in burn surgery: A systematic review and meta-analysis. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 871–883. [Google Scholar] [CrossRef] [PubMed]
- Haug, V.; Tapking, C.; Panayi, A.C.; Veeramani, A.; Knoedler, S.; Tchiloemba, B.; Abdulrazzak, O.; Kadakia, N.; Bonaventura, B.; Culnan, D.; et al. Outcome comparison of the most commonly employed wound coverage techniques in patients with massive burns >/=50% TBSA—A systematic review and meta-analysis. Burns 2024, 50, 107210. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers 2020, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- Peirce, S.C.; Carolan-Rees, G. ReCell® Spray-On Skin System for Treating Skin Loss, Scarring and Depigmentation after Burn Injury: A NICE Medical Technology Guidance. Appl. Health Econ. Health Policy 2019, 17, 131–141. [Google Scholar] [CrossRef]
- Cooper-Jones, B.; Visintini, S. A Noncultured Autologous Skin Cell Spray Graft for the Treatment of Burns. In CADTH Issues in Emerging Health Technologies; CADTH Horizon Scans: Ottawa, ON, Canada, 2016; pp. 1–11. [Google Scholar]
- Widjaja, W.; Tan, J.; Maitz, P.K.M. Efficacy of dermal substitute on deep dermal to full thickness burn injury: A systematic review. ANZ J. Surg. 2017, 87, 446–452. [Google Scholar] [CrossRef]
- van den Bosch, A.S.; Verwilligen, R.A.F.; Pijpe, A.; Bosma, E.; van der Vlies, C.H.; Lucas, Y.; Burchell, G.L.; van Zuijlen, P.P.M.; Middelkoop, E.; National Burn Care, E.; et al. Outcomes of dermal substitutes in burns and burn scar reconstruction: A systematic review and meta-analysis. Wound Repair. Regen. 2024, 32, 960–978. [Google Scholar] [CrossRef]
- Phillips, G.S.A.; Nizamoglu, M.; Wakure, A.; Barnes, D.; El-Muttardi, N.; Dziewulski, P. The Use of Dermal Regeneration Templates for Primary Burns Surgery in a UK Regional Burns Centre. Ann. Burn. Fire Disasters 2020, 33, 245–252. [Google Scholar]
- Grande, P.K.; Hill, D.; McElfresh, J.; Velamuri, R.; Liu, X. Systematic Review and Meta-analysis of Biodegradable Temporizing Matrix Application for Complex Wound Reconstruction. J. Burn. Care Res. 2025, 46, 82–89. [Google Scholar] [CrossRef]
- Domaszewska-Szostek, A.P.; Krzyzanowska, M.O.; Czarnecka, A.M.; Siemionow, M. Local Treatment of Burns with Cell-Based Therapies Tested in Clinical Studies. J. Clin. Med. 2021, 10, 396. [Google Scholar] [CrossRef]
- Varkey, M.; Visscher, D.O.; van Zuijlen, P.P.M.; Atala, A.; Yoo, J.J. Skin bioprinting: The future of burn wound reconstruction? Burns Trauma 2019, 7, 4. [Google Scholar] [CrossRef]
- Mrazek, A.A.; Simpson, P.; Lee, J.O. Nutrition in Pediatric Burns. Semin. Plast. Surg. 2024, 38, 125–132. [Google Scholar] [CrossRef]
- Heyland, D.K.; Wibbenmeyer, L.; Pollack, J.; Friedman, B.; Turgeon, A.F.; Eshraghi, N.; Jeschke, M.G.; Belisle, S.; Grau, D.; Mandell, S.; et al. A Randomized Trial of Enteral Glutamine for Treatment of Burn Injuries. N. Engl. J. Med. 2022, 387, 1001–1010. [Google Scholar] [CrossRef]
- Greenhalgh, D.G. Management of Burns. N. Engl. J. Med. 2019, 380, 2349–2359. [Google Scholar] [CrossRef]
- Kivi, M.K.; Jafarzadeh, A.; Hosseini-Baharanchi, F.S.; Salehi, S.; Goodarzi, A. The efficacy, satisfaction, and safety of carbon dioxide (CO2) fractional laser in combination with pulsed dye laser (PDL) versus each one alone in the treatment of hypertrophic burn scars: A single-blinded randomized controlled trial. Lasers Med. Sci. 2024, 39, 69. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.J.; Williams, E.A.; Pham, C.H.; Collier, Z.J.; Dang, J.; Yenikomshian, H.A.; Gillenwater, T.J. Fractional CO2 laser treatment for burn scar improvement: A systematic review and meta-analysis. Burns 2021, 47, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.J.; Lei, Y.; Gold, M.H.; Tan, J. Efficacy of pulsed dye laser combined with fractional CO2 laser in the treatment of pediatric burn scars. Lasers Surg. Med. 2023, 55, 464–470. [Google Scholar] [CrossRef]
- Sohrabi, C.; Goutos, I. The use of botulinum toxin in keloid scar management: A literature review. Scars Burn. Heal. 2020, 6, 2059513120926628. [Google Scholar] [CrossRef]
- Legemate, C.M.; Spronk, I.; Mokkink, L.B.; Middelkoop, E.; Polinder, S.; van Baar, M.E.; van der Vlies, C.H. Evaluation of measurement properties of health-related quality of life instruments for burns: A systematic review. J. Trauma Acute Care Surg. 2020, 88, 555–571. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.H.; Rowland, R.; Kennedy, G.T.; Campbell, C.; Joe, V.C.; Chin, T.L.; Burmeister, D.M.; Christy, R.J.; Durkin, A.J. Review of machine learning for optical imaging of burn wound severity assessment. J. Biomed. Opt. 2024, 29, 020901. [Google Scholar] [CrossRef]
- Taib, B.G.; Karwath, A.; Wensley, K.; Minku, L.; Gkoutos, G.V.; Moiemen, N. Artificial intelligence in the management and treatment of burns: A systematic review and meta-analyses. J. Plast. Reconstr. Aesthet. Surg. 2023, 77, 133–161. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Burns Association. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neriamparambil, A.J.; Sawhney, R.; Wong, W.L. Evidence-Based Management of Burns: A Narrative Review of Evolving Practices. Eur. Burn J. 2025, 6, 59. https://doi.org/10.3390/ebj6040059
Neriamparambil AJ, Sawhney R, Wong WL. Evidence-Based Management of Burns: A Narrative Review of Evolving Practices. European Burn Journal. 2025; 6(4):59. https://doi.org/10.3390/ebj6040059
Chicago/Turabian StyleNeriamparambil, Anna Jolly, Raja Sawhney, and Wei Lun Wong. 2025. "Evidence-Based Management of Burns: A Narrative Review of Evolving Practices" European Burn Journal 6, no. 4: 59. https://doi.org/10.3390/ebj6040059
APA StyleNeriamparambil, A. J., Sawhney, R., & Wong, W. L. (2025). Evidence-Based Management of Burns: A Narrative Review of Evolving Practices. European Burn Journal, 6(4), 59. https://doi.org/10.3390/ebj6040059






