The Early Childhood Development of Pediatric Burn Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection: Demographic and Clinical Characteristics
2.3. Data Collection: Dutch Development Instrument
2.4. Statistical Analyses
3. Results
3.1. Study Population
3.2. Dutch Development Instrument
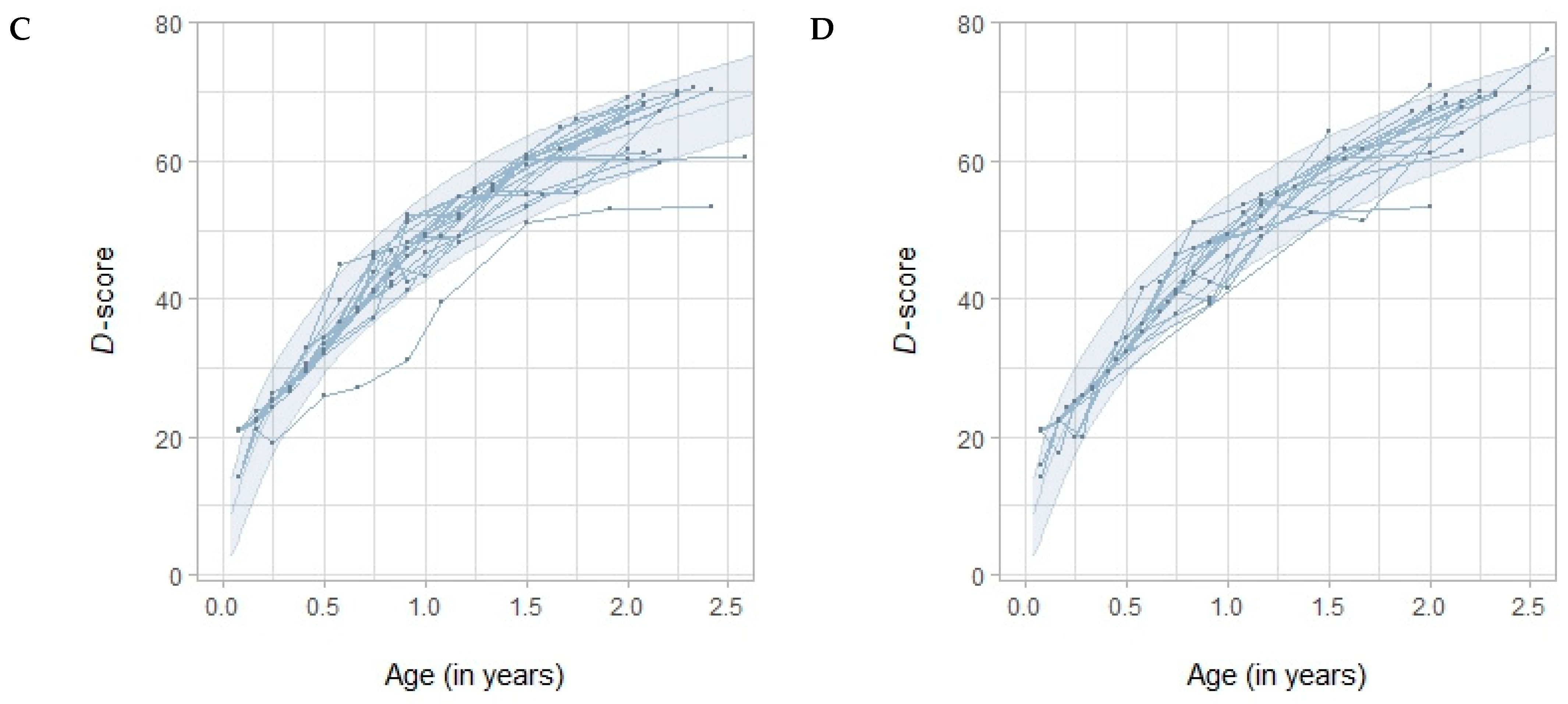
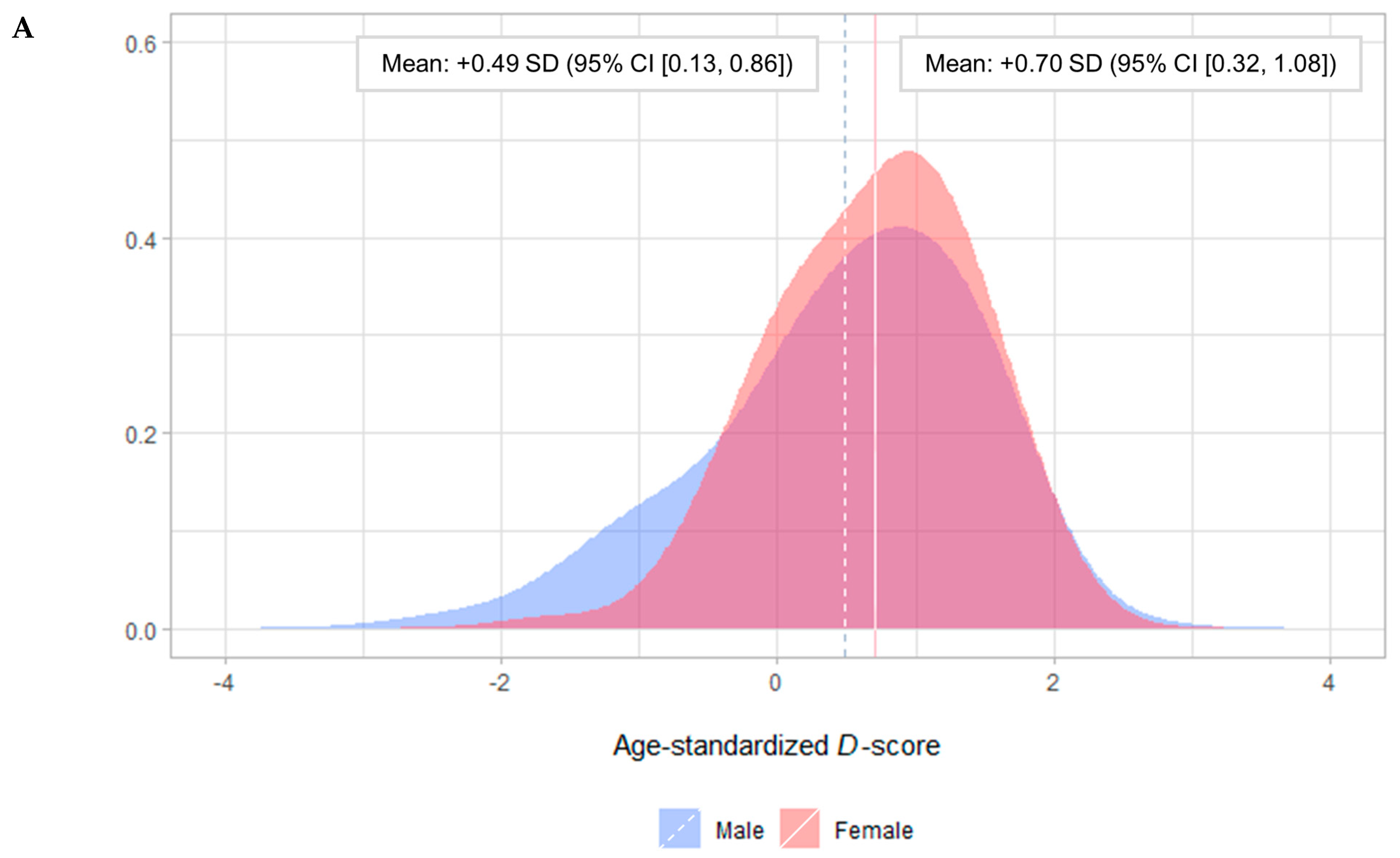
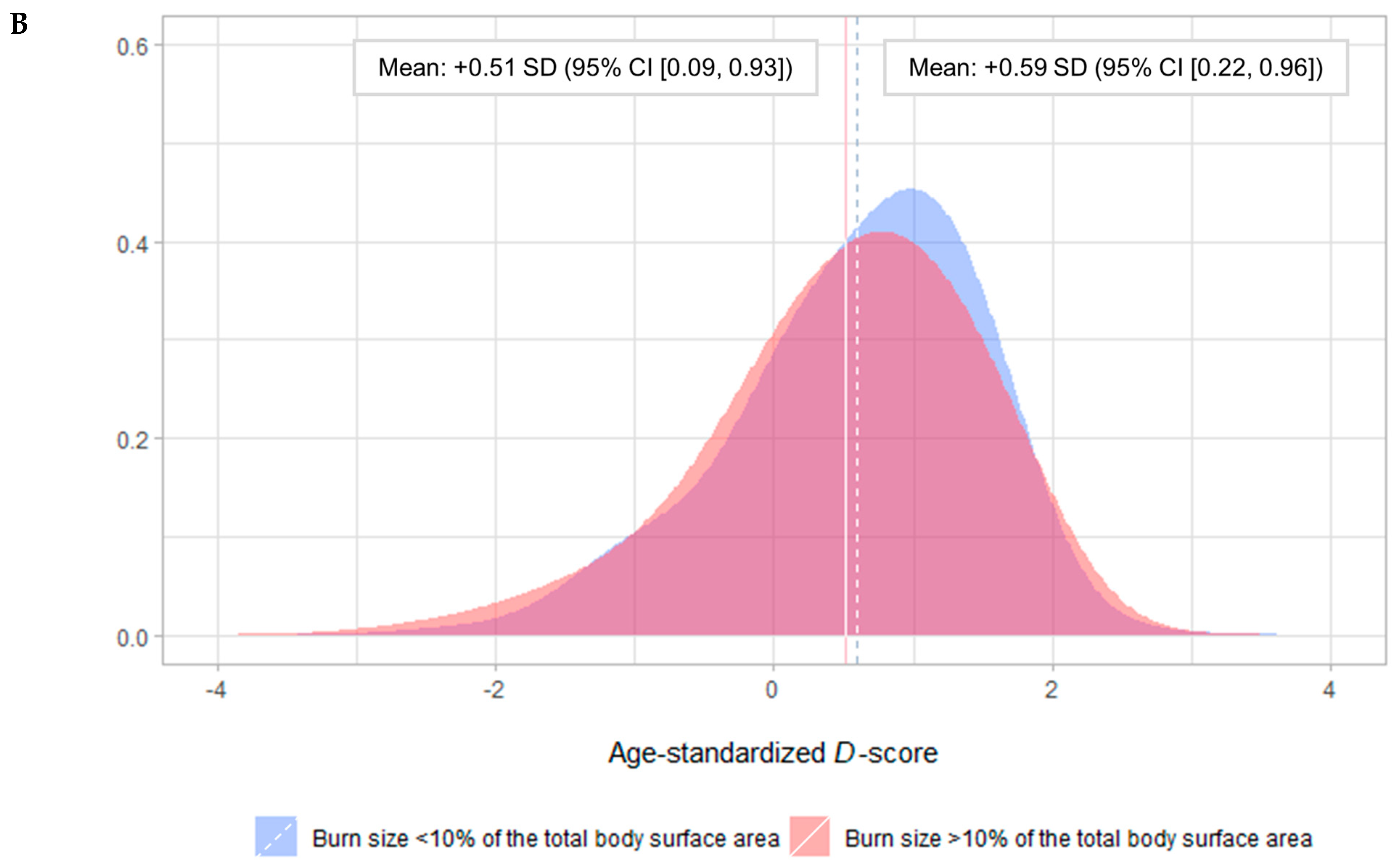
3.3. D-Score
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Fact Sheet: Burns; WHO: Geneva, Switzerland, 2023; p. 1. [Google Scholar]
- Vloemans, A.F.P.M.; Dokter, J.; Van Baar, M.E.; Nijhuis, I.; Beerthuizen, G.I.J.M.; Nieuwenhuis, M.K.; Kuijper, E.C.; Middelkoop, E.M. Epidemiology of children admitted to the Dutch burn centres. Changes in referral influence admittance rates in burn centres. Burns 2011, 37, 1161–1167. [Google Scholar] [CrossRef]
- Dokter, J.; Vloemans, A.F.; Beerthuizen, G.I.J.M.; Van der Vlies, C.H.; Boxma, H.; Breederveld, R.; Tuinebreijer, W.E.; Middelkoop, E.; van Baar, M.E. Epidemiology and trends in severe burns in the Netherlands. Burns 2014, 40, 1406–1414. [Google Scholar] [CrossRef]
- Van Zoonen, E.E.; Van Baar, M.E.; Van Schie, C.H.; Koppes, L.L.; Verheij, R.A. Burn injuries in primary care in the Netherlands: Risk factors and trends. Burns 2022, 48, 440–447. [Google Scholar] [CrossRef]
- Black, M.M.; Walker, S.P.; Fernald, L.C.; Andersen, C.T.; DiGirolamo, A.M.; Lu, C.; McCoy, D.C.; Fink, G.; Shawar, Y.R.; Shiffman, J.; et al. Early childhood development coming of age: Science through the life course. Lancet 2017, 389, 77–90. [Google Scholar] [CrossRef]
- Agran, P.F.; Anderson, C.; Winn, D.; Trent, R.; Walton-Haynes, L.; Thayer, S. Rates of Pediatric Injuries by 3-Month Intervals for Children 0 to 3 Years of Age. Pediatrics 2003, 111, e683–e692. [Google Scholar] [CrossRef]
- Peck, M.D. Epidemiology of burns throughout the world. Part I: Distribution and risk factors. Burns 2011, 37, 1087–1100. [Google Scholar] [CrossRef]
- Rivara, F.P. Developmental and Behavioral Issues in Childhood Injury Prevention. J. Dev. Behav. Pediatr. 1995, 16, 362–370. [Google Scholar] [CrossRef]
- van Zoonen, E.E.; Pijpe, A.; van Baar, M.E.; Nieuwenhuis, M.K.; van Schie, C.H.; Trommel, N.; Hartlief, G.; Beemsterboer-Haagsman, M.G.; Meij-de Vries, A. Aetiology of severe burn incidents in children under 5 years of age in the Netherlands: A prospective cohort study. Burns 2022, 48, 713–722. [Google Scholar] [CrossRef]
- Capitani, E.; Lorenzini, C.; Biuzzi, A.; Alaimo, L.; Nante, N. Factors influencing the first thousand days of life. The importance of Nurturing Care. J. Prev. Med. Hyg. 2023, 64, E172–E177. [Google Scholar]
- Shonkoff, J.P.; Garner, A.S.; Committee on Psychosocial Aspects of Child Family Health; Committee on Early Childhood Adoption Dependent Care; Section on Developmental Behavioral Pediatrics. The Lifelong Effects of Early Childhood Adversity and Toxic Stress. Pediatrics 2012, 129, e232–e246. [Google Scholar] [CrossRef]
- Pinquart, M.; Shen, Y. Behavior Problems in Children and Adolescents with Chronic Physical Illness: A Meta-Analysis. J. Pediatr. Psychol. 2011, 36, 1003–1016. [Google Scholar] [CrossRef]
- Patenaude, A.F.; Kupst, M.J. Psychosocial Functioning in Pediatric Cancer. J. Pediatr. Psychol. 2005, 30, 9–27. [Google Scholar] [CrossRef]
- Pinquart, M.; Teubert, D. Academic, Physical, and Social Functioning of Children and Adolescents with Chronic Physical Illness: A Meta-analysis. J. Pediatr. Psychol. 2012, 37, 376–389. [Google Scholar] [CrossRef]
- Nijhof, S.L.; Vinkers, C.H.; van Geelen, S.M.; Duijff, S.N.; Achterberg, E.M.; Van Der Net, J.; Veltkamp, R.C.; Grootenhuis, M.A.; van de Putte, E.M.; Hillegers, M.H.; et al. Healthy play, better coping: The importance of play for the development of children in health and disease. Neurosci. Biobehav. Rev. 2018, 95, 421–429. [Google Scholar] [CrossRef]
- Bakker, A.; Maertens, K.J.; Van Son, M.J.; Van Loey, N.E. Psychological consequences of pediatric burns from a child and family perspective: A review of the empirical literature. Clin. Psychol. Rev. 2013, 33, 361–371. [Google Scholar] [CrossRef]
- Gorga, D.; Johnson, J.; Bentley, A.; Silverberg, R.; Glassman, M.; Madden, M.; Yurt, R.; Nagler, W. The physical, functional, and developmental outcome of pediatric burn survivors from 1 to 12 months postinjury. J. Burn Care Rehabil. 1999, 20, 171–178; discussion 170. [Google Scholar]
- Nayeb-Hashemi, N.; Rosenberg, M.; Rosenberg, L.; Sharp, S.; Thomas, C.; Holzer, C., III; McCauley, R.; Herndon, D.; Meyer, W., III. Skull burns resulting in calvarial defects: Cognitive and affective outcomes. Burns 2009, 35, 237–246. [Google Scholar] [CrossRef]
- Folio, M.R.; Fewell, R. Peabody developmental motor scales and activity cards. Adapt. Phys. Act. Q 1984, 1, 173–178. [Google Scholar]
- Coons, C.; Denver Developmental Materials Inc. John F. Kennedy Child Development Centre. The Home Screening Questionnaire Reference Manual; Denver Developmental Materials [for] J.F.K. Development Center: Denver, CO, USA, 1981. [Google Scholar]
- Frankenburg, W.K.; Denver Developmental Materials Inc. Denver II Technical Manual; Denver Developmental Materials: Denver, CO, USA, 1990. [Google Scholar]
- Kazis, L.E.; Lee, A.F.; Rose, M.; Liang, M.H.; Li, N.C.; Ren, X.S.; Sheridan, R.; Gilroy-Lewis, J.; Stoddard, F.; Hinson, M.; et al. Recovery curves for pediatric burn survivors advances in patient-oriented outcomes. JAMA Pediatr. 2016, 170, 534–542. [Google Scholar] [CrossRef]
- Kazis, L.E.; Liang, M.H.; Lee, A.; Ren, X.S.; Phillips, C.B.; Hinson, M.; Calvert, C.; Cullen, M.; Beth Daugherty, M.; Goodwin, C.W.; et al. The Development, Validation, and Testing of a Health Outcomes Burn Questionnaire for Infants and Children 5 years of Age and Younger: American Burn Association/Shriners Hospitals for Children. J. Burn Care Rehabil. 2002, 23, 196–207. [Google Scholar] [CrossRef]
- Cuijpers, M.D.; van de Sande, P.J.; Cords, C.I.; Scholten-Jaegers, S.M.; van Zuijlen, P.P.; Baartmans, M.G.; Pijpe, A. The Effect of Burns on Children’s Growth Trajectory: A Nationwide Cohort Study. J. Burn Care Res. 2023, 44, 1083–1091. [Google Scholar] [CrossRef] [PubMed]
- Dunnink, G. Standpunt Bereik van de Jeugdgezondheidszorg; Rijksinstituut voor Volksgezondheid en Milieu RIVM: Bilthoven, The Netherlands, 2010. [Google Scholar]
- Van Buuren, S.; Eekhout, I. Child development with the D-score: Turning milestones into measurement. Gates Open Res. 2021, 5, 81. [Google Scholar] [CrossRef]
- Eekhout, I.; van Buuren, S. Child development with the D-score: Tuning instruments to unity. Gates Open Res. 2022, 5, 86. [Google Scholar] [CrossRef]
- Fernald, L.C.; Prado, E.; Kariger, P.; Raikes, A. A Toolkit for Measuring Early Childhood Development in Low and Middle-Income Countries; World Bank: Washington, DC, USA, 2017. [Google Scholar]
- McCray, G.; McCoy, D.; Kariger, P.; Janus, M.; Black, M.M.; Chang, S.M.; Tofail, F.; Eekhout, I.; Waldman, M.; Van Buuren, S.; et al. The creation of the Global Scales for Early Development (GSED) for children aged 0–3 years: Combining subject matter expert judgements with big data. BMJ Glob. Health 2023, 8, e009827. [Google Scholar] [CrossRef] [PubMed]
- Van Buuren, S.; Eekhout, I.; Huizing, A. GitHub: D-Score for Child Development; Routledge: Abingdon, UK, 2023. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2022. [Google Scholar]
- Jacobusse, G.; van Buuren, S.; Verkerk, P.H. An interval scale for development of children aged 0–2 years. Stat. Med. 2006, 25, 2272–2283. [Google Scholar] [CrossRef]
- Jacobusse, G.; van Buuren, S. Computerized adaptive testing for measuring development of young children. Stat. Med. 2007, 26, 2629–2638. [Google Scholar] [CrossRef] [PubMed]
- Herngreen, W.P.; Reerink, J.D.; van Noord-Zaadstra, B.M.; Verloover-Vanhorick, S.P.; Ruys, J.H. SMOCC: Design of a Representative Cohort-study of Live-born Infants in the Netherlands. Eur. J. Public Health 1992, 2, 117–122. [Google Scholar] [CrossRef]
- Daltroy, L.H.; Liang, M.H.; Phillips, C.B.; Daugherty, M.B.; Hinson, M.; Jenkins, M.; McCauley, R.W.M., III; Munster, A.; Pidcock, F.; Reilly, D. American Burn Association/Shriners Hospitals for Children Burn Outcomes Questionnaire. J. Burn Care Rehabil. 2000, 21, 29–39. [Google Scholar] [CrossRef]
- Nederlands Jeugdinstituut. Nederlands Jeugdinstituut: Van Wiechenonderzoek (VWO); Nederlands Jeugdinstituut: Utrecht, The Netherlands, 2023. [Google Scholar]

| Sex, n (%) | ||
| Male | 25 | (66.0)% |
| Female | 13 | (34.0%) |
| Age at the time of injury, median (IQR) | 1.0 | (1.0–2.0) |
| Burn size, median (IQR) | 6.0 | (4.5–11.9) |
| Burn size, n (%) | ||
| ≤10.0% TBSA | 20 | (52.6%) |
| >10.0% TBSA | 18 | (47.4%) |
| Extent of full-thickness burn, median (IQR) | 0.0 | (0.0–0.0) |
| Etiology, n (%) | ||
| Scald | 34 | (89.5%) |
| Contact | 2 | (5.2%) |
| Fat | 2 | (5.2%) |
| Hospital admission in days, median (IQR) | 7.5 | (3.0–12.5) |
| Mechanical ventilation, n (%) | 1 | (2.6%) |
| Reconstructive surgery, n (%) | 1 | (2.6%) |
| Pre-existing developmental delay, n (%) | 1 | (2.6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuijpers, M.D.; Akkerman, M.; Baartmans, M.G.A.; van Zuijlen, P.P.M.; Pijpe, A. The Early Childhood Development of Pediatric Burn Patients. Eur. Burn J. 2024, 5, 145-154. https://doi.org/10.3390/ebj5020012
Cuijpers MD, Akkerman M, Baartmans MGA, van Zuijlen PPM, Pijpe A. The Early Childhood Development of Pediatric Burn Patients. European Burn Journal. 2024; 5(2):145-154. https://doi.org/10.3390/ebj5020012
Chicago/Turabian StyleCuijpers, Maxime D., Moniek Akkerman, Martin G. A. Baartmans, Paul P. M. van Zuijlen, and Anouk Pijpe. 2024. "The Early Childhood Development of Pediatric Burn Patients" European Burn Journal 5, no. 2: 145-154. https://doi.org/10.3390/ebj5020012
APA StyleCuijpers, M. D., Akkerman, M., Baartmans, M. G. A., van Zuijlen, P. P. M., & Pijpe, A. (2024). The Early Childhood Development of Pediatric Burn Patients. European Burn Journal, 5(2), 145-154. https://doi.org/10.3390/ebj5020012






