Outcomes of Patients with Amputation following Electrical Burn Injuries
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics
3.2. Amputation Rate and Total Body Surface Area (TBSA) (%) Burnt
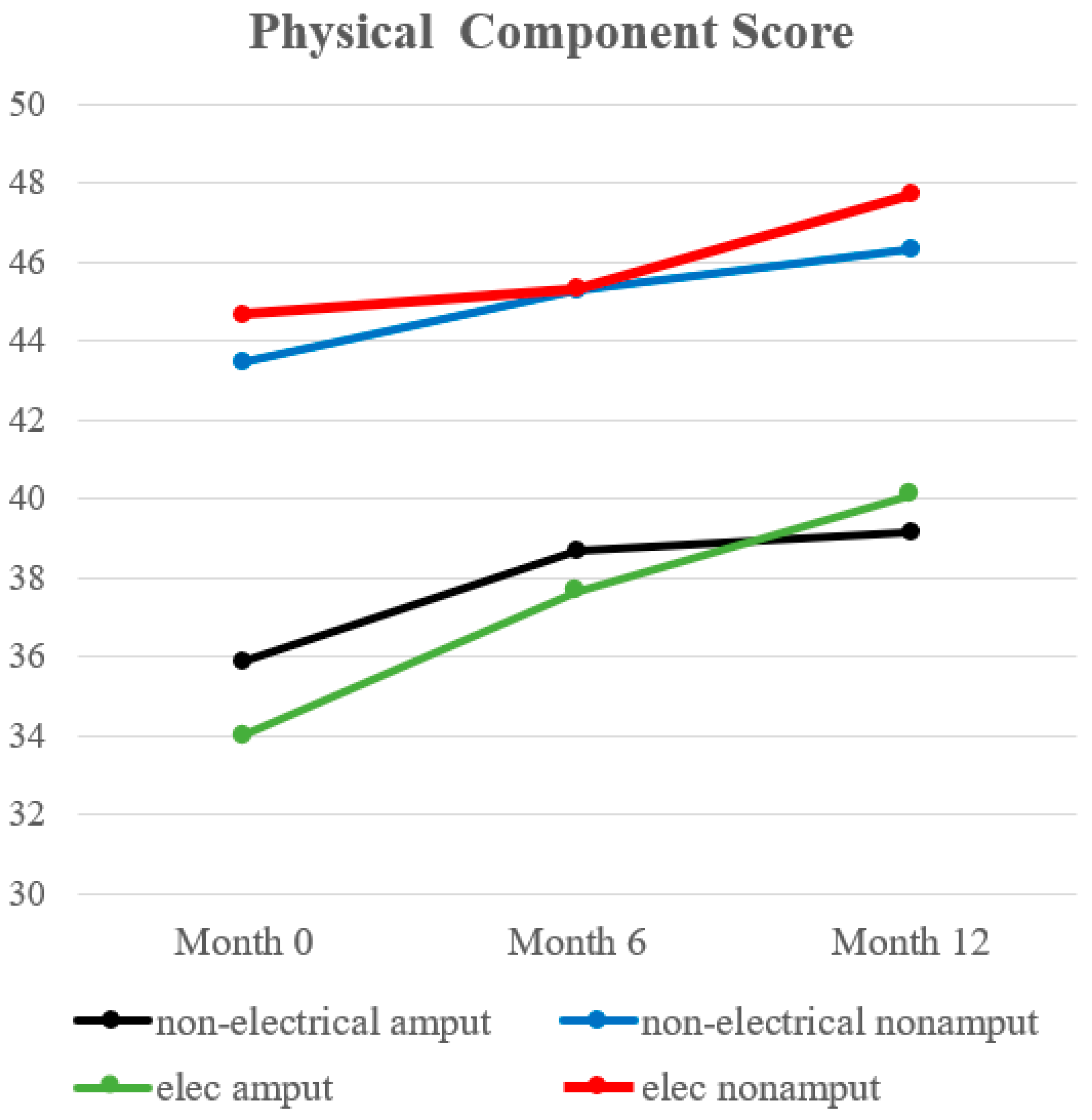
3.3. Physical Component Score (PCS)
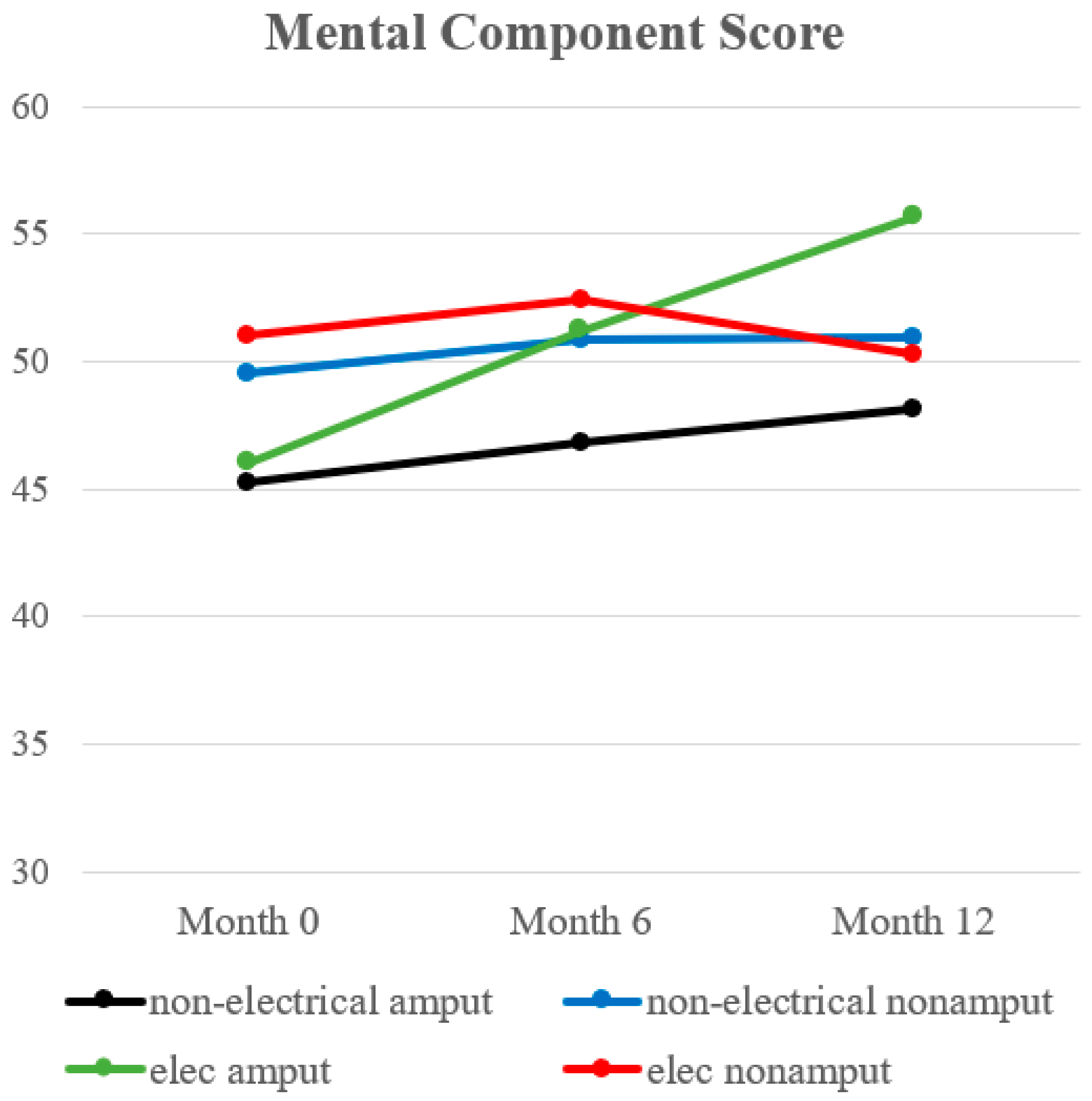
3.4. Mental Component Score (MCS)
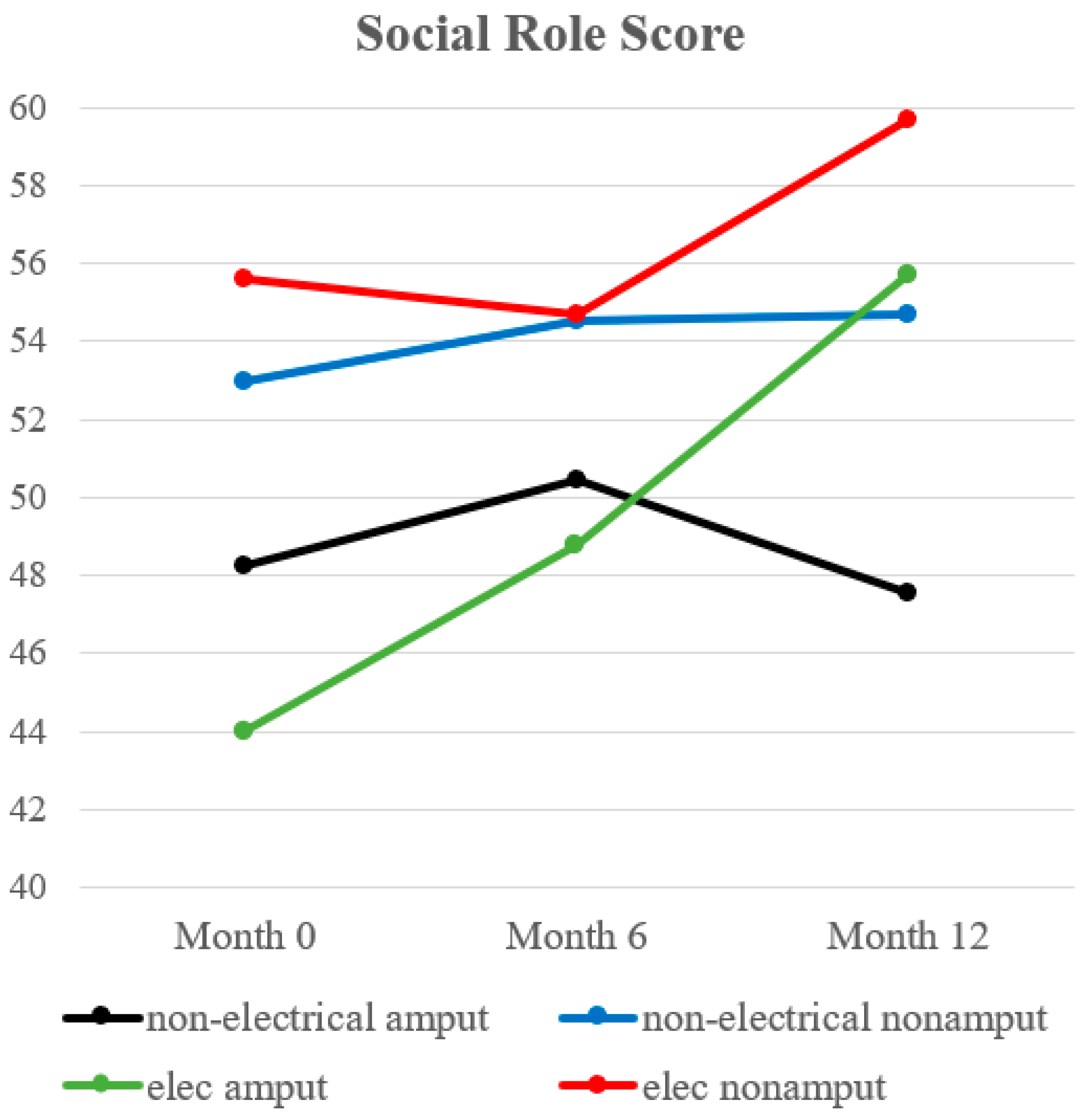
3.5. Social Participation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xie, W.G. Prevention and treatment of electrical burn injury: Much progresses achieved yet further efforts still needed. Zhonghua Shao Shang Za Zhi 2017, 33, 728–731. [Google Scholar] [CrossRef] [PubMed]
- Shih, J.G.; Shahrokhi, S.; Jeschke, M.G. Review of Adult Electrical Burn Injury Outcomes Worldwide: An Analysis of Low-Voltage vs High-Voltage Electrical Injury. J. Burn. Care Res. 2017, 38, e293–e298. [Google Scholar] [CrossRef] [PubMed]
- Evers, L.H.; Bhavsar, D.; Mailander, P. The biology of burn injury. Exp. Dermatol. 2010, 19, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Koumbourlis, A.C. Electrical injuries. Crit. Care Med. 2002, 30 (Suppl. 11), S424–S430. [Google Scholar] [CrossRef]
- Sanford, A.; Gamelli, R.L. Lightning and thermal injuries. Handb. Clin. Neurol. 2014, 120, 981–986. [Google Scholar] [CrossRef]
- Tondel, M.; Blomqvist, A.; Jakobsson, K.; Nilsson, T.; Persson, B.; Thomee, S.; Gunnarsson, L.G. Immediate and delayed outcomes after electrical injury. A guide for clinicians. Lakartidningen 2016, 113, D7CL. [Google Scholar]
- Wesner, M.L.; Hickie, J. Long-term sequelae of electrical injury. Can. Fam. Physician 2013, 59, 935–939. [Google Scholar] [PubMed]
- Docking, P. Electrical burn injuries. Accid. Emerg. Nurs. 1999, 7, 70–76. [Google Scholar] [CrossRef]
- Kowalske, K.; Holavanahalli, R.; Helm, P. Neuropathy after burn injury. J. Burn. Care Rehabil. 2001, 22, 353–357. [Google Scholar] [CrossRef]
- Holavanahalli, R.K.; Helm, P.A.; Kowalske, K.J. Long-term outcomes in patients surviving large burns: The skin. J. Burn. Care Res. 2010, 31, 631–639. [Google Scholar] [CrossRef]
- Kuwabara, T.; Fukushima, T.; Makino, K.; Kondo, H. Epileptic seizure, cataract, and tongue atrophy during the 8 years after electrical brain injury. Intern. Med. 2009, 48, 1179–1182. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, D.B.; Nelson, M. Rehabilitation concerns in electrical burn patients: A review of the literature. J. Trauma. 1988, 28, 808–812. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers 2020, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- Ashfaq, A.; Lashari, U.G.; Saleem, S.; Naveed, S.; Meraj, H.; Waqas, A. Exploring Symptoms of Post-traumatic Stress Disorders and Perceived Social Support among Patients with Burn Injury. Cureus 2018, 10, e2669. [Google Scholar] [CrossRef] [PubMed]
- Ohrtman, E.A.; Shapiro, G.D.; Simko, L.C.; Dore, E.; Slavin, M.D.; Saret, C.; Amaya, F.; Lomelin-Gascon, J.; Ni, P.; Acton, A.; et al. Social Interactions and Social Activities After Burn Injury: A Life Impact Burn Recovery Evaluation (LIBRE) Study. J. Burn. Care Res. 2018, 39, 1022–1028. [Google Scholar] [CrossRef] [PubMed]
- Ross, E.; Crijns, T.J.; Ring, D.; Coopwood, B. Social factors and injury characteristics associated with the development of perceived injury stigma among burn survivors. Burns 2021, 47, 692–697. [Google Scholar] [CrossRef]
- Baumgartner, R. Rehabilitation following amputation. Ther. Umsch. 1989, 46, 441–448. [Google Scholar]
- Dash, S.; Arumugam, P.K.; Muthukumar, V.; Kumath, M.; Sharma, S. Study of clinical pattern of limb loss in electrical burn injuries. Injury 2021, 52, 1925–1933. [Google Scholar] [CrossRef]
- Stockly, O.R.; Wolfe, A.E.; Espinoza, L.F.; Simko, L.C.; Kowalske, K.; Carrougher, G.J.; Gibran, N.; Bamer, A.M.; Meyer, W.; Rosenberg, M.; et al. The impact of electrical injuries on long-term outcomes: A Burn Model System National Database study. Burns 2020, 46, 352–359. [Google Scholar] [CrossRef]
- Bartley, C.N.; Atwell, K.; Purcell, L.; Cairns, B.; Charles, A. Amputation Following Burn Injury. J. Burn. Care Res. 2019, 40, 430–436. [Google Scholar] [CrossRef]
- Amtmann, D.; McMullen, K.; Bamer, A.; Fauerbach, J.A.; Gibran, N.S.; Herndon, D.; Schneider, J.C.; Kowalske, K.; Holavanahalli, R.; Miller, A.C. National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Review of Program and Database. Arch. Phys. Med. Rehabil. 2020, 101, S5–S15. [Google Scholar] [CrossRef] [PubMed]
- Hays, R.D.; Spritzer, K.L.; Schalet, B.D.; Cella, D. PROMIS((R))-29 v2.0 profile physical and mental health summary scores. Qual. Life Res. 2018, 27, 1885–1891. [Google Scholar] [CrossRef] [PubMed]
- Huppe, M.; Schneider, K.; Casser, H.R.; Knille, A.; Kohlmann, T.; Lindena, G.; Nagel, B.; Nelles, J.; Pfingsten, M.; Petzke, F. Characteristic values and test statistical goodness of the Veterans RAND 12-Item Health Survey (VR-12) in patients with chronic pain: An evaluation based on the KEDOQ pain dataset. Schmerz 2021, 36, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Selim, A.J.; Rothendler, J.A.; Qian, S.X.; Bailey, H.M.; Kazis, L.E. The History and Applications of the Veterans RAND 12-Item Health Survey (VR-12). J. Ambul. Care Manag. 2022, 45, 161–170. [Google Scholar] [CrossRef]
- Ding, H.; Huang, M.; Li, D.; Lin, Y.; Qian, W. Epidemiology of electrical burns: A 10-year retrospective analysis of 376 cases at a burn centre in South China. J. Int. Med. Res. 2020, 48, 300060519891325. [Google Scholar] [CrossRef]
- Radulovic, N.; Mason, S.A.; Rehou, S.; Godleski, M.; Jeschke, M.G. Acute and long-term clinical, neuropsychological and return-to-work sequelae following electrical injury: A retrospective cohort study. BMJ Open 2019, 9, e025990. [Google Scholar] [CrossRef]
- Pedrazzi, N.; Klein, H.; Gentzsch, T.; Kim, B.S.; Waldner, M.; Giovanoli, P.; Plock, J.; Schweizer, R. Predictors for limb amputation and reconstructive management in electrical injuries. Burns 2023, 49, 1103–1112. [Google Scholar] [CrossRef]
- Sun, C.F.; Lv, X.X.; Li, Y.J.; Li, W.Z.; Jiang, L.; Li, J.; Feng, J.; Chen, S.Z.; Wu, F.; Li, X.Y. Epidemiological studies of electrical injuries in Shaanxi province of China: A retrospective report of 383 cases. Burns 2012, 38, 568–572. [Google Scholar] [CrossRef]
- Dillingham, T.R.; Pezzin, L.E.; MacKenzie, E.J.; Burgess, A.R. Use and satisfaction with prosthetic devices among persons with trauma-related amputations: A long-term outcome study. Am. J. Phys. Med. Rehabil. 2001, 80, 563–571. [Google Scholar] [CrossRef]
- Pezzin, L.E.; Dillingham, T.R.; Mackenzie, E.J.; Ephraim, P.; Rossbach, P. Use and satisfaction with prosthetic limb devices and related services. Arch. Phys. Med. Rehabil. 2004, 85, 723–729. [Google Scholar] [CrossRef]
- Meulenbelt, H.E.; Geertzen, J.H.; Jonkman, M.F.; Dijkstra, P.U. Skin problems of the stump in lower limb amputees: 1. A clinical study. Acta Derm. Venereol. 2011, 91, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Grzebien, A.; Chabowski, M.; Malinowski, M.; Uchmanowicz, I.; Milan, M.; Janczak, D. Analysis of selected factors determining quality of life in patients after lower limb amputation- a review article. Pol. Przegl. Chir. 2017, 89, 57–61. [Google Scholar] [CrossRef]
- Schoppen, T.; Boonstra, A.; Groothoff, J.W.; de Vries, J.; Goeken, L.N.; Eisma, W.H. Physical, mental, and social predictors of functional outcome in unilateral lower-limb amputees. Arch. Phys. Med. Rehabil. 2003, 84, 803–811. [Google Scholar] [CrossRef] [PubMed]
- van Velzen, J.M.; van Bennekom, C.A.; Polomski, W.; Slootman, J.R.; van der Woude, L.H.; Houdijk, H. Physical capacity and walking ability after lower limb amputation: A systematic review. Clin. Rehabil. 2006, 20, 999–1016. [Google Scholar] [CrossRef] [PubMed]
- Sansam, K.; Neumann, V.; O’Connor, R.; Bhakta, B. Predicting walking ability following lower limb amputation: A systematic review of the literature. J. Rehabil. Med. 2009, 41, 593–603. [Google Scholar] [CrossRef]
- Tapking, C.; Hundeshagen, G.; Popp, D.; Lee, J.O.; Herndon, D.N.; Zapata-Sirvent, R.; Branski, L.K. The Frequency and Reason For Amputations in Electrically Burned Pediatric Patients. J. Burn. Care Res. 2019, 40, 107–111. [Google Scholar] [CrossRef]
- Brandao, C.; Meireles, R.; Brito, I.; Ramos, S.; Cabral, L. The Role Of Comorbidities On Outcome Prediction in Acute Burn Patients. Ann. Burn. Fire Disasters 2021, 34, 323–333. [Google Scholar]
- Herlianita, R.; Purwanto, E.; Wahyuningsih, I.; Pratiwi, I.D. Clinical outcome and comparison of burn injury scoring systems in burn patient in Indonesia. Afr. J. Emerg. Med. 2021, 11, 331–334. [Google Scholar] [CrossRef]
- Nguyen, N.L.; Ngo, M.D. Profile and outcome of burn injuries amongst preschool children in a developing country. Ann. Burn. Fire Disasters 2019, 32, 267–271. [Google Scholar]
- Lodha, P.; Shah, B.; Karia, S.; De Sousa, A. Post-Traumatic Stress Disorder (Ptsd) Following Burn Injuries: A Comprehensive Clinical Review. Ann. Burn. Fire Disasters 2020, 33, 276–287. [Google Scholar]
- Huang, Y.K.; Su, Y.J. Burn severity and long-term psychosocial adjustment after burn injury: The mediating role of body image dissatisfaction. Burns 2021, 47, 1373–1380. [Google Scholar] [CrossRef] [PubMed]
- Haynes, Z.A.; Collen, J.F.; Poltavskiy, E.A.; Walker, L.E.; Janak, J.; Howard, J.T.; Werner, J.K.; Wickwire, E.M.; Holley, A.B.; Zarzabal, L.A.; et al. Risk factors of persistent insomnia among survivors of traumatic injury: A retrospective cohort study. J. Clin. Sleep Med. 2021, 17, 1831–1840. [Google Scholar] [CrossRef]
- Bartley, C.N.; Atwell, K.; Cairns, B.; Charles, A. Racial and Ethnic Disparities in Discharge to Rehabilitation Following Burn Injury. J. Burn. Care Res. 2019, 40, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Meagher, A.D.; Beadles, C.A.; Doorey, J.; Charles, A.G. Racial and ethnic disparities in discharge to rehabilitation following traumatic brain injury. J. Neurosurg. 2015, 122, 595–601. [Google Scholar] [CrossRef] [PubMed]

| Variable | Non-Electrical Burn | Electrical Burn | p-Value |
|---|---|---|---|
| Ethnicity | n (%) | n (%) | <0.0001 |
| Hispanic | 1632 (27.06) | 162 (41.12) | |
| Non-Hispanic | 4399 (72.94) | 232 (58.88) | |
| Gender | n (%) | n (%) | <0.0001 |
| Male | 4401 (69.41) | 382 (93.63) | |
| Female | 1940 (30.59) | 26 (6.37) | |
| Age | 0.8141 | ||
| Mean ± Std | 30.83 ± 21.81 | 29.91 ± 16.16 | |
| Median | 29.99 | 28.44 | |
| TBSA (%) burnt | 0.0027 | ||
| Mean ± Std | 23.56 ± 20.36 (%) | 20.44 ± 19.5 (%) |
| Month 0 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| PCS | Mean ± SD | 35.90 ± 11.67 | 43.44 ± 10.71 | 34.00 ± 8.98 | 44.66 ± 9.90 | 0.0002 |
| Median | 34 | 45 | 37 | 47 | ||
| n | 30 | 516 | 11 | 29 | ||
| Month 6 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| PCS | Mean ± SD | 38.69 ± 10.56 | 45.26 ± 11.08 | 37.67 ± 9.97 | 45.31 ± 9.09 | 0.0036 |
| Median | 39 | 47 | 38 | 46 | ||
| n | 26 | 452 | 9 | 26 | ||
| Month 12 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| PCS | Mean ± SD | 39.18 ± 9.65 | 46.30 ± 10.67 | 40.11 ± 12.22 | 47.70 ± 10.20 | 0.0014 |
| Median | 40 | 48 | 39 | 50 | ||
| n | 28 | 400 | 9 | 23 | ||
| Month 0 | |||
| Group comparison | Difference between means | Simultaneous 95% confidence limits | p-value |
| Non-electrical amput vs. Non-electrical nonamput | −7.5399 | −12.8583, −2.2215 | 0.0012 |
| Elec amput vs. Elec nonamput | −10.6552 | −20.6829, −0.6274 | 0.0304 |
| Month 6 | |||
| Group comparison | Difference between means | Simultaneous 95% confidence limits | p-value |
| Non-electrical amput vs. Non-electrical nonamput | −6.5665 | −12.4164, −0.7167 | 0.0185 |
| Elec amput vs. Elec nonamput | −7.6410 | −18.8590, 3.5769 | 0.4309 |
| Month 12 | |||
| Group comparison | Difference between means | Simultaneous 95% confidence limits | p-value |
| Non-electrical amput vs. Non-electrical nonamput | −7.1189 | −12.6199, −1.6189 | 0.0040 |
| Elec amput vs. Elec nonamput | −7.5845 | −18.6486, 3.4795 | 0.4197 |
| Month 0 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| MCS | Mean ± SD | 45.27 ± 13.80 | 49.52 ± 12.07 | 46.00 ± 14.27 | 51.21 ± 10.71 | 0.2511 |
| Median | 45 | 51 | 46 | 51 | ||
| n | 30 | 516 | 11 | 29 | ||
| Month 6 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| MCS | Mean ± SD | 46.85 ± 11.15 | 50.83 ± 11.67 | 51.22 ± 10.00 | 52.46 ± 12.40 | 0.1426 |
| Median | 48 | 53 | 50 | 56 | ||
| n | 26 | 452 | 9 | 26 | ||
| Month 12 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| MCS | Mean ± SD | 48.11 ± 13.34 | 50.96 ± 12.25 | 55.67 ± 10.40 | 50.26 ± 12.82 | 0.3622 |
| Median | 48 | 55 | 60 | 54 | ||
| n | 28 | 400 | 9 | 23 | ||
| Month 0 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| Social Role Score | Mean ± SD | 48.26 ± 12.30 | 52.99 ± 10.74 | 44.00 ± 10.90 | 55.61 ± 11.29 | 0.0144 |
| Median | 43 | 53 | 42 | 62 | ||
| n | 23 | 369 | 8 | 18 | ||
| Month 6 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| Social Role Score | Mean ± SD | 50.47 ± 9.78 | 54.52 ± 10.88 | 48.78 ± 10.05 | 54.67 ± 11.31 | 0.0772 |
| Median | 51 | 59 | 49 | 59 | ||
| n | 19 | 355 | 9 | 21 | ||
| Month 12 | ||||||
| Variable | Statistics | Non-electrical amput | Non-electrical nonamput | Elec amput | Elec nonamput | p-value |
| Social Role Score | Mean ± SD | 47.53 ± 11.33 | 54.72 ± 10.16 | 55.71 ± 9.12 | 59.69 ± 9.76 | 0.0061 |
| Median | 47 | 56 | 59 | 64 | ||
| n | 17 | 296 | 7 | 16 | ||
| Month 0 | |||
| Group comparison | Difference between means | Simultaneous 95% confidence limits | p-value |
| Non-electrical amput vs. Non-electrical nonamput | −4.7337 | −10.9161, 1.4487 | 0.2581 |
| Elec amput vs. Elec nonamput | −11.6111 | −23.8346, 0.6124 | 0.0730 |
| Month 12 | |||
| Group comparison | Difference between means | Simultaneous 95% confidence limits | p-value |
| Non-electrical amput vs. Non-electrical nonamput | −7.1902 | −13.9307, −0.4496 | 0.0295 |
| Elec amput vs. Elec nonamput | −3.9732 | −16.2208, 8.2743 | 1.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, E.; Wan, B.; Solis-Beach, K.J.; Kowalske, K. Outcomes of Patients with Amputation following Electrical Burn Injuries. Eur. Burn J. 2023, 4, 318-329. https://doi.org/10.3390/ebj4030029
Kim E, Wan B, Solis-Beach KJ, Kowalske K. Outcomes of Patients with Amputation following Electrical Burn Injuries. European Burn Journal. 2023; 4(3):318-329. https://doi.org/10.3390/ebj4030029
Chicago/Turabian StyleKim, Eunyeop, Bingchun Wan, Kyra Jeanine Solis-Beach, and Karen Kowalske. 2023. "Outcomes of Patients with Amputation following Electrical Burn Injuries" European Burn Journal 4, no. 3: 318-329. https://doi.org/10.3390/ebj4030029
APA StyleKim, E., Wan, B., Solis-Beach, K. J., & Kowalske, K. (2023). Outcomes of Patients with Amputation following Electrical Burn Injuries. European Burn Journal, 4(3), 318-329. https://doi.org/10.3390/ebj4030029






