Smart Polymeric Wound Dressing for Treating Partial-Thickness Burns: A Preliminary Preclinical Study on the Porcine Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Handling of Animal, Anesthesia, and Ethical Considerations
2.2. Creation of the Partial-Thickness Burn
2.3. Dressing
2.4. Analysis
2.5. Histological Analysis
2.6. Creation of the Partial-Thickness Burn
2.7. Dressing
2.8. Microbiology
3. Results
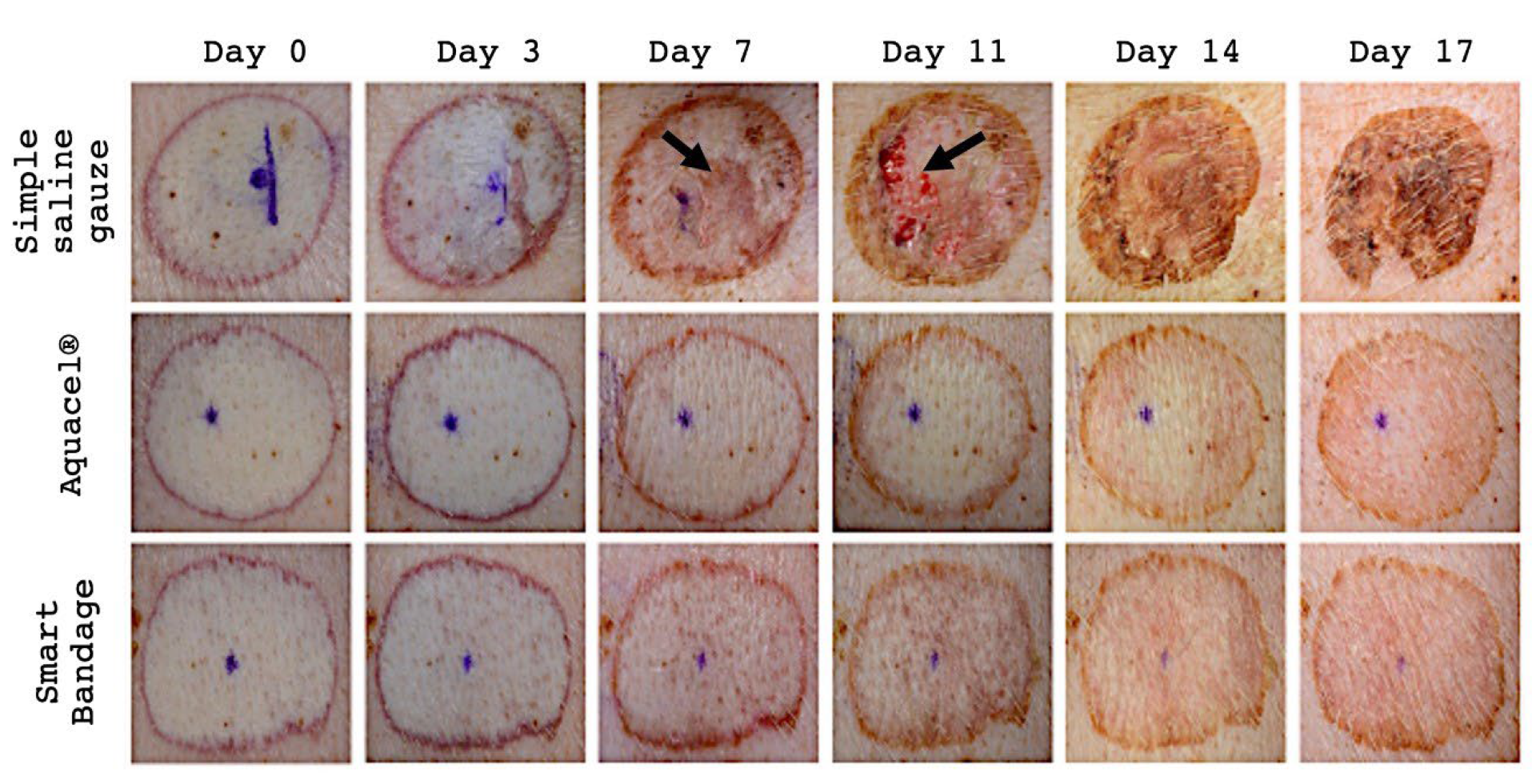
3.1. Macroscopic Assessment
3.2. Histology
3.3. Macroscopic Assessment
3.4. Histology
3.5. Microbiology
3.5.1. Pseudomonas Aeruginosa
3.5.2. Staphylococcus Aureus
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Score Finding | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| Superficial serocellular crusting or epidermal inflammation | Normal epidermis | Rare serocellular crusts | Extensive serocellular crusts | Subcorneal pustules | Extensive inflammation on the surface |
| Epidermal regeneration | Complete epidermal regeneration | Complete epidermal regeneration + mild epidermal hyperplasia | Complete epidermal regeneration + moderate to marked epidermal hyperplasia | Incomplete epidermal regeneration | persistent ulcer/no epidermal regeneration |
| Dermo-epidermal clefting | None | Rare foci of separation | Occasional areas of separation of the dermo-epidermal junction | Formation of bullae | Extensive bullae formation or complete separation of the dermo-epidermal junction |
| Granulation tissue | Normal dermis | Collagen reaches tissue with mature fibrocytes | Granulation tissue with attenuated fibrocytes | Reactive granulation tissue with prominent blood vessels | Necrosis/early fibrosis with no granulation tissue |
| Score Finding | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| Dermal inflammation: | None | Minimal | Mild | Moderate | Severe |
| Granulocyte cell presence | None | Minimal | Mild | Moderate | Severe |
| Mononuclear cell (lymphocytes +plasma cells) presence | None | Minimal | Mild | Moderate | Severe |
| Macrophages and giant cell presence | None | Minimal | Mild | Moderate | Severe |
| Necrosis in the wound area | Normal, no necrosis | Rare necrotic foci surrounded by macrophages | Minimal necrosis involving less than 25% of the wound area surrounded by macrophages Or Necrosis of epidermis adnexa and up to 10% upper dermis (depth of dermis) | Focal necrosis, involving 60% of the wound area Or Necrosis or sloughing of the epidermis. Adnexal necrosis. Necrosis of 10 to 25% depth of dermal necrosis | Complete wound area necrotic. Or Sloughing of the adnexal epidermis necrosis. More than 25% of death from dermal necrosis |
| Study | Group | Crust | Epidermal Regeneration | Cleft | Granulation Tissue | Dermis Inflammation | Mononuclear Cells | Necrosis in Wound Area | Total Average Score |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Smart Bandage | 1.5 | 2 | 0.5 | 2 | 1 | 1 | 0 | 8 |
| Aquacel® | 2 | 1.5 | 0.5 | 1 | 1.5 | 0.5 | 0 | 7 | |
| Simple saline gauze | 2 | 2 | 1.5 | 3 | 0 | 0 | 0 | 8.5 | |
| 2 | Smart Bandage+ | 0.7 | 3.1 | 2.3 | 3.5 | 1.2 | 1.1 | 1.7 | 13.7 |
| Aquacel Ag® | 0.7 | 2.8 | 2.7 | 3.7 | 1.3 | 1.0 | 2.0 | 14.2 | |
| Simple saline gauze | 1.3 | 4.0 | 2.7 | 4.0 | 3.0 | 2.0 | 3.3 | 20.3 |
References
- WHO. Burns. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/burns (accessed on 14 July 2022).
- Sadeghi-Bazargani, H.; Mohammadi, R. Epidemiology of burns in Iran during the last decade (2000–2010): Review of literature and methodological considerations. Burns 2012, 38, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Sayed, P.; Hirt-Burri, N.; de Buys Roessingh, A.; Raffoul, W.; Applegate, L.A. Evolution of biological bandages as first cover for burn patients. Adv. Wound Care 2019, 8, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Rahmanian-Schwarz, A.; Beiderwieden, A.; Willkomm, L.M.; Amr, A.; Schaller, H.E.; Lotter, O. A clinical evaluation of Biobrane(®) and Suprathel(®) in acute burns and reconstructive surgery. Burns 2011, 37, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- Schwarze, H.; Küntscher, M.; Uhlig, C.; Hierlemann, H.; Prantl, L.; Noack, N.; Hartmann, B. Suprathel, a new skin substitute, in the management of donor sites of split-thickness skin grafts: Results of a clinical study. Burns 2007, 33, 850–854. [Google Scholar] [CrossRef]
- Dhivya, S.; Padma, V.V.; Santhini, E. Wound dressings—A review. Biomedicine 2015, 5, 22. [Google Scholar] [CrossRef]
- Surowiecka, A.; Strużyna, J.; Winiarska, A.; Korzeniowski, T. Hydrogels in burn wound management—A review. Gels 2022, 8, 122. [Google Scholar] [CrossRef]
- Chhabra, S.; Chhabra, N.; Kaur, A.; Gupta, N. Wound healing concepts in clinical practice of OMFS. J. Maxillofac. Oral Surg. 2017, 16, 403–423. [Google Scholar] [CrossRef]
- Derakhshandeh, H.; Kashaf, S.S.; Aghabaglou, F.; Ghanavati, I.O.; Tamayol, A. Smart Bandages: The Future of wound care. Trends Biotechnol. 2018, 36, 1259–1274. [Google Scholar] [CrossRef]
- Sosnik, A.; Cohn, D. Reverse thermo-responsive poly(ethylene oxide) and poly(propylene oxide) multiblock copolymers. Biomaterials 2005, 26, 349–357. [Google Scholar] [CrossRef]
- Cohn, D.; Sosnik, A.; Levy, A. Improved reverse thermo-responsive polymeric systems. Biomaterials 2003, 24, 3707–3714. [Google Scholar] [CrossRef]
- Cohn, D.; Sosnik, A.; Malal, R.; Zarka, R.; Garty, S.; Levy, A. Chain extension as a strategy for the development of improved reverse thermo-responsive polymers. Polym. Adv. Technol. 2007, 18, 731–736. [Google Scholar] [CrossRef]
- Cabodi, M.; Cross, V.L.; Qu, Z.; Havenstrite, K.L.; Schwartz, S.; Stroock, A.D. An active wound dressing for controlled convective mass transfer with the wound bed. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 82, 210–222. [Google Scholar] [CrossRef]
- Shirakata, Y.; Tokumaru, S.; Yamasaki, K.; Sayama, K.; Hashimoto, K. So-called biological dressing effects of cultured epidermal sheets are mediated by the production of EGF family, TGF-beta and VEGF. J. Dermatol. Sci. 2003, 32, 209–215. [Google Scholar] [CrossRef]
- Chan, E.S.; Lam, P.K.; Liew, C.T.; Lau, H.C.; Yen, R.S.; King, W.W. A new technique to resurface wounds with composite biocompatible epidermal graft and artificial skin. J. Trauma 2001, 50, 358–362. [Google Scholar] [CrossRef]
- Griffiths, M.; Ojeh, N.; Livingstone, R.; Price, R.; Navsaria, H. Survival of Apligraf in acute human wounds. Tissue Eng. 2004, 10, 1180–1195. [Google Scholar] [CrossRef]
- Yannas, I.; Burke, J.; Warpehoski, M.; Stasikelis, P.; Skrabut, E.M.; Orgill, D.P.; Giard, D. Design principles and preliminary clinical performance of an artificial skin. In Biomaterials: Interfacial Phenomena and Applications; Cooper, S., Peppas, N., Hoffman, A., Ratner, B., Eds.; ACS Publications: Washington, DC, USA, 1982; pp. 317–350. [Google Scholar]
- Winter, G.D. Formation of the scab and the rate of epithelization of superficial wounds in the skin of the young domestic pig. Nature 1962, 193, 293–294. [Google Scholar] [CrossRef]
- Winter, G.D.; Scales, J.T. Effect of air drying and dressings on the surface of a wound. Nature 1963, 197, 91–92. [Google Scholar] [CrossRef]
- Xu, R.; Xia, H.; He, W.; Li, Z.; Zhao, J.; Liu, B.; Wang, Y.; Lei, Q.; Kong, Y.; Bai, Y.; et al. Controlled water vapor transmission rate promotes wound healing via wound re-epithelialization and contraction enhancement. Sci. Rep. 2016, 6, 24596. [Google Scholar] [CrossRef] [Green Version]
- Expert Working Group SEWG. Wound exudate and the role of dressings. A consensus document. Int. Wound J. 2008, 5 (Suppl. 1), iii-12. [Google Scholar] [CrossRef]
- Dowsett, C. Management of Wound Exudate; Independent Nurse: London, UK, 2012. [Google Scholar]
- Wlaschin, K.F.; Ninkovic, J.; Griesgraber, G.W.; Colak Atan, S.; Young, A.J.; Pereira, J.M.; Solberg, M.J.; Smith, G.; Parks, P.J.; McNulty, A.K.; et al. The impact of first-aid dressing design on healing of porcine partial thickness wounds. Wound Repair Regen. 2019, 27, 622–633. [Google Scholar] [CrossRef]
- Shu, W.; Wang, Y.; Zhang, X.; Li, C.; Le, H.; Chang, F. Functional hydrogel dressings for treatment of burn wounds. Front. Bioeng. Biotechnol. 2021, 9, 788461. [Google Scholar] [CrossRef]
- Harats, M.; Jaeger, M.; Kornhaber, R.A.; Haik, J.M. AQUACEL® Ag burn glove and silver sulfadiazine for the treatment of partial thickness hand burns: A retrospective review. Indian J. Burns 2016, 24, 18. [Google Scholar] [CrossRef] [Green Version]
- Carter, M.J.; Tingley-Kelley, K.; Warriner, R.A., 3rd. Silver treatments and silver-impregnated dressings for the healing of leg wounds and ulcers: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2010, 63, 668–679. [Google Scholar] [CrossRef] [PubMed]
- Yarboro, D.D. A comparative study of the dressings silver sulfadiazine and Aquacel Ag in the management of superficial partial-thickness burns. Adv. Skin Wound Care 2013, 26, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Sheckter, C.C.; Van Vliet, M.M.; Krishnan, N.M.; Garner, W.L. Cost-effectiveness comparison between topical silver sulfadiazine and enclosed silver dressing for partial-thickness burn treatment. J. Burn Care Res. 2014, 35, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Caruso, D.M.; Foster, K.N.; Blome-Eberwein, S.A.; Twomey, J.A.; Herndon, D.N.; Luterman, A.; Silverstein, P.; Antimarino, J.R.; Bauer, G.J. Randomized clinical study of hydrofiber dressing with silver or silver sulfadiazine in the management of partial thickness burns. J. Burn Care Res. 2006, 27, 298–309. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.F.; Chang, C.J.; Hu, W.Y.; Hayter, M.; Chang, Y.T. The effectiveness of silver-releasing dressings in the management of non-healing chronic wounds: A meta-analysis. J. Clin. Nurs. 2009, 18, 716–728. [Google Scholar] [CrossRef] [PubMed]
- Michaels, J.A.; Campbell, B.; King, B.; Palfreyman, S.J.; Shackley, P.; Stevenson, M. Randomized controlled trial and cost-effectiveness analysis of silver-donating antimicrobial dressings for venous leg ulcers (VULCAN trial). Br. J. Surg. 2009, 96, 1147–1156. [Google Scholar] [CrossRef]
- Eberlein, T.; Haemmerle, G.; Signer, M.; Gruber-Moesenbacher, U.; Traber, J.; Mittlboeck, M.; Abel, M.; Strohal, R. Comparison of PHMB-containing dressing and silver dressings in patients with critically colonised or locally infected wounds. J. Wound Care 2012, 21, 12, 14–16, 18–20. [Google Scholar] [CrossRef] [Green Version]
- Piatkowski, A.; Drummer, N.; Andriessen, A.; Ulrich, D.; Pallua, N. Randomized controlled single center study comparing a polyhexanide containing bio-cellulose dressing with silver sulfadiazine cream in partial-thickness dermal burns. Burns 2011, 37, 800–804. [Google Scholar] [CrossRef]
- de Mattos, I.B.; Holzer, J.C.J.; Tuca, A.C.; Groeber-Becker, F.; Funk, M.; Popp, D.; Mautner, S.; Birngruber, T.; Kamolz, L.P. Uptake of PHMB in a bacterial nanocellulose based wound dressing: A feasible clinical procedure. Burns 2019, 45, 898–904. [Google Scholar] [CrossRef]
- Wild, T.; Bruckner, M.; Payrich, M.; Schwarz, C.; Eberlein, T.; Andriessen, A. Eradication of Methicillin-Resistant Staphylococcus aureus in pressure ulcers comparing a polyhexanide containing cellulose dressing with polyhexanide swabs in a prospective randomized study. Adv. Ski. Wound Care 2012, 25, 17–22. [Google Scholar] [CrossRef]
- Wiegand, C.; Abel, M.; Ruth, P.; Hipler, U.C. HaCaT keratinocytes in co-culture with Staphylococcus aureus can be protected from bacterial damage by polihexanide. Wound Repair Regen. 2009, 17, 730–738. [Google Scholar] [CrossRef]
- Kirker, K.R.; Fisher, S.T.; James, G.A.; McGhee, D.; Shah, C.B. Efficacy of polyhexamethylene biguanide-containing antimicrobial foam dressing against MRSA relative to standard foam dressing. Wounds 2009, 21, 229–233. [Google Scholar]
- Gilliver, S.C. PHMB: A well-tolerated antiseptic with no reported toxic effects. J. Wound Care. 2009, 9–14. [Google Scholar]
- Moritz AR and Henriques, F.C. Studies of Thermal Injury: II. The Relative Importance of Time and Surface Temperature in the Causation of Cutaneous Burns. Am. J. Pathol. 1947, 23, 695–720. [Google Scholar]
- Cuttle, L.; Kempf, M.; Phillips, G.E.; Mill, J.; Hayes, M.T.; Fraser, J.F.; Wang, X.Q.; Kimble, R.M. A porcine deep dermal partial thickness burn model with hypertrophic scarring. Burns 2006, 32, 806–820. [Google Scholar] [CrossRef]
- Gibson, A.L.F.; Carney, B.C.; Cuttle, L.; Andrews, C.J.; Kowalczewski, C.J.; Liu, A.; Powell, H.M.; Stone, R.; Supp, D.M.; Singer, A.J.; et al. Coming to Consensus: What Defines Deep Partial Thickness Burn Injuries in Porcine Models? J. Burn Care Res. 2021, 42, 98–109. [Google Scholar] [CrossRef]





| Bacteria | Test Item | Average Recovery ± SD (Log10CFU per Sample) | Average Reduction ± SD (Log10CFU per Sample) | Statistical Significance (p-Value) |
|---|---|---|---|---|
| P. aeruginosa | Negative control | 6.30 ± 0.03 | N/A | N/A |
| Smart Bandage+ | 6.11 ± 0.44 | 0.19 ± 0.44 | N/A | |
| S. aureus | Negative control | 0.01 ± 0.11 | N/A | N/A |
| Smart Bandage+ | 0.00 ± 0.00 | 6.01 ± 0.00 | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beylin, D.; Haik, J.; Biros, E.; Kornhaber, R.; Cleary, M.; Harats, M.; Cohn, D.; Sapir, Y.; Weisberg, O. Smart Polymeric Wound Dressing for Treating Partial-Thickness Burns: A Preliminary Preclinical Study on the Porcine Model. Eur. Burn J. 2023, 4, 20-34. https://doi.org/10.3390/ebj4010004
Beylin D, Haik J, Biros E, Kornhaber R, Cleary M, Harats M, Cohn D, Sapir Y, Weisberg O. Smart Polymeric Wound Dressing for Treating Partial-Thickness Burns: A Preliminary Preclinical Study on the Porcine Model. European Burn Journal. 2023; 4(1):20-34. https://doi.org/10.3390/ebj4010004
Chicago/Turabian StyleBeylin, Dmitry, Josef Haik, Erik Biros, Rachel Kornhaber, Michelle Cleary, Moti Harats, Daniel Cohn, Yair Sapir, and Ori Weisberg. 2023. "Smart Polymeric Wound Dressing for Treating Partial-Thickness Burns: A Preliminary Preclinical Study on the Porcine Model" European Burn Journal 4, no. 1: 20-34. https://doi.org/10.3390/ebj4010004
APA StyleBeylin, D., Haik, J., Biros, E., Kornhaber, R., Cleary, M., Harats, M., Cohn, D., Sapir, Y., & Weisberg, O. (2023). Smart Polymeric Wound Dressing for Treating Partial-Thickness Burns: A Preliminary Preclinical Study on the Porcine Model. European Burn Journal, 4(1), 20-34. https://doi.org/10.3390/ebj4010004








