A 10-Year Review of Sunburn Injuries Presenting to the Manchester Adult and Paediatric Specialist Burn Services
Abstract
1. Introduction
2. Materials and Methods
3. Results
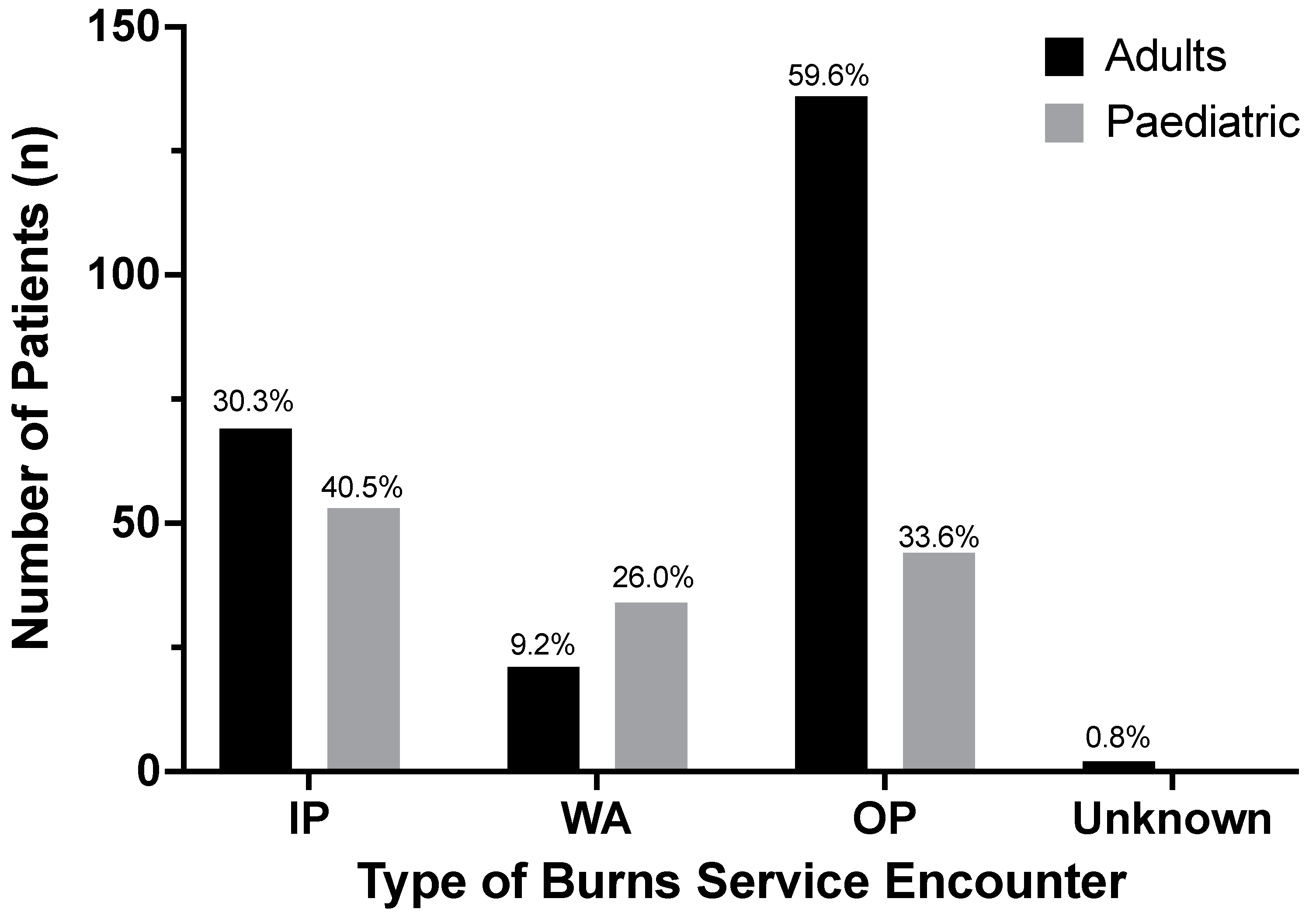
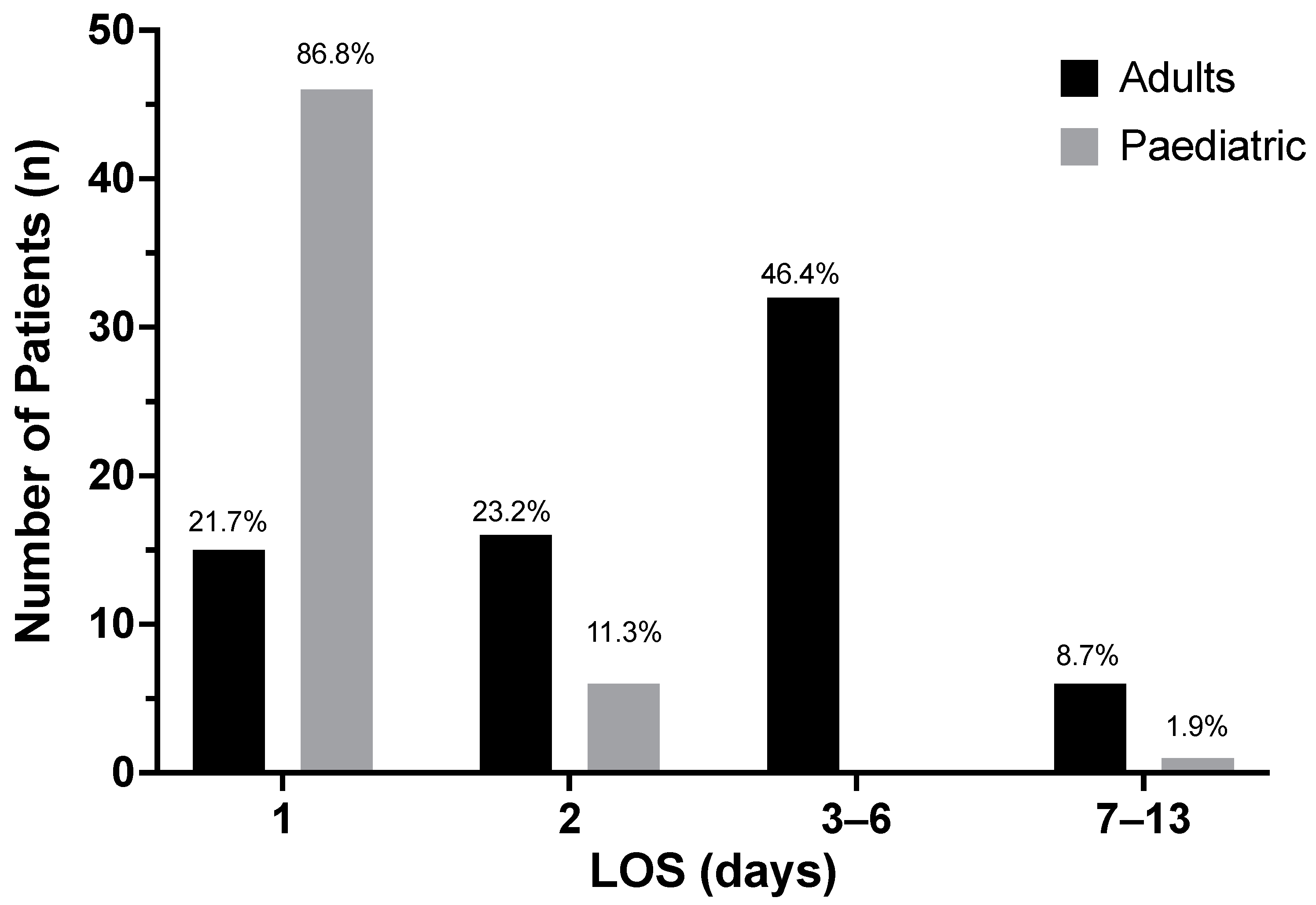
3.1. Patient Demographics and Sunburn Characteristics
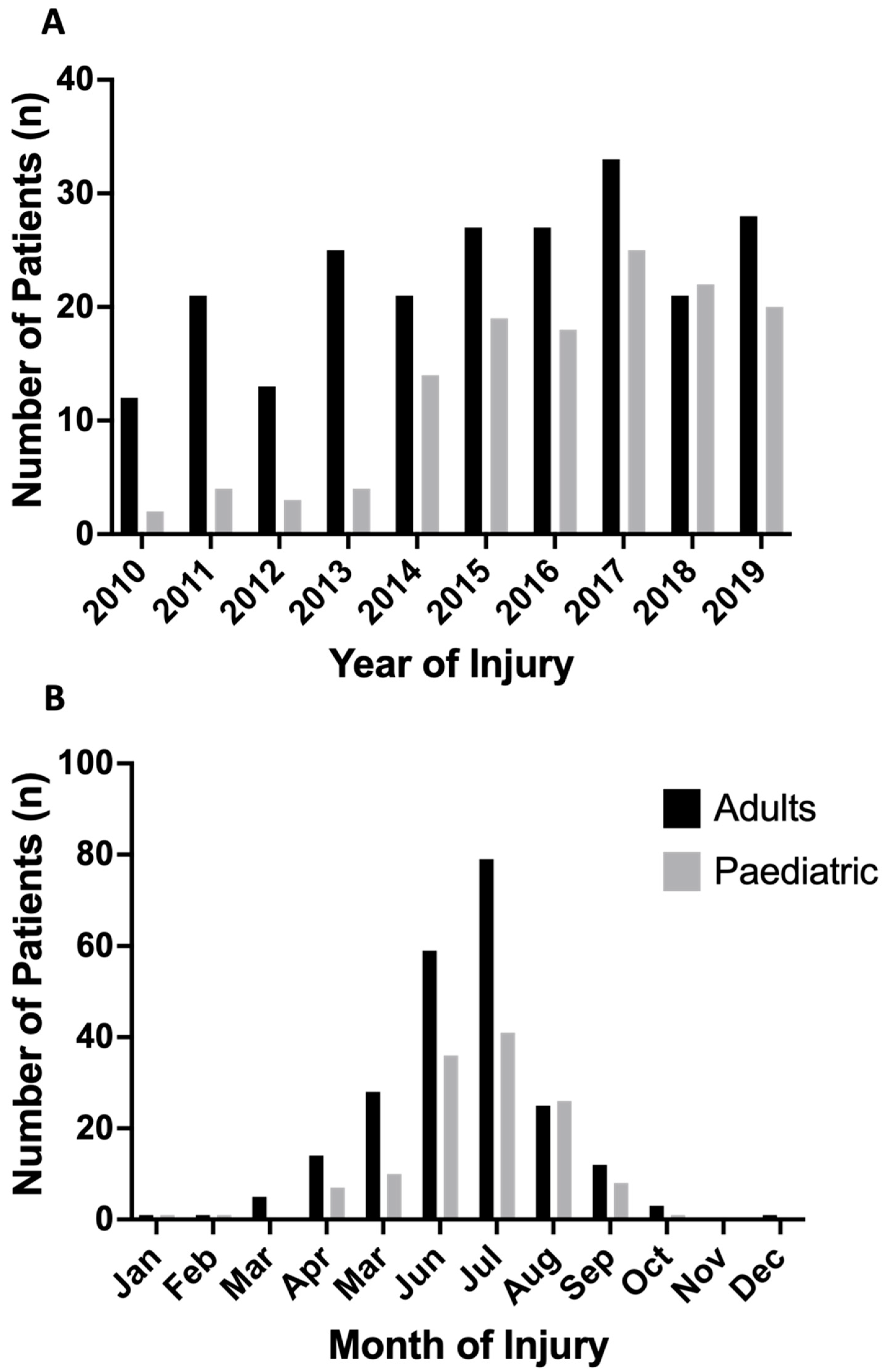
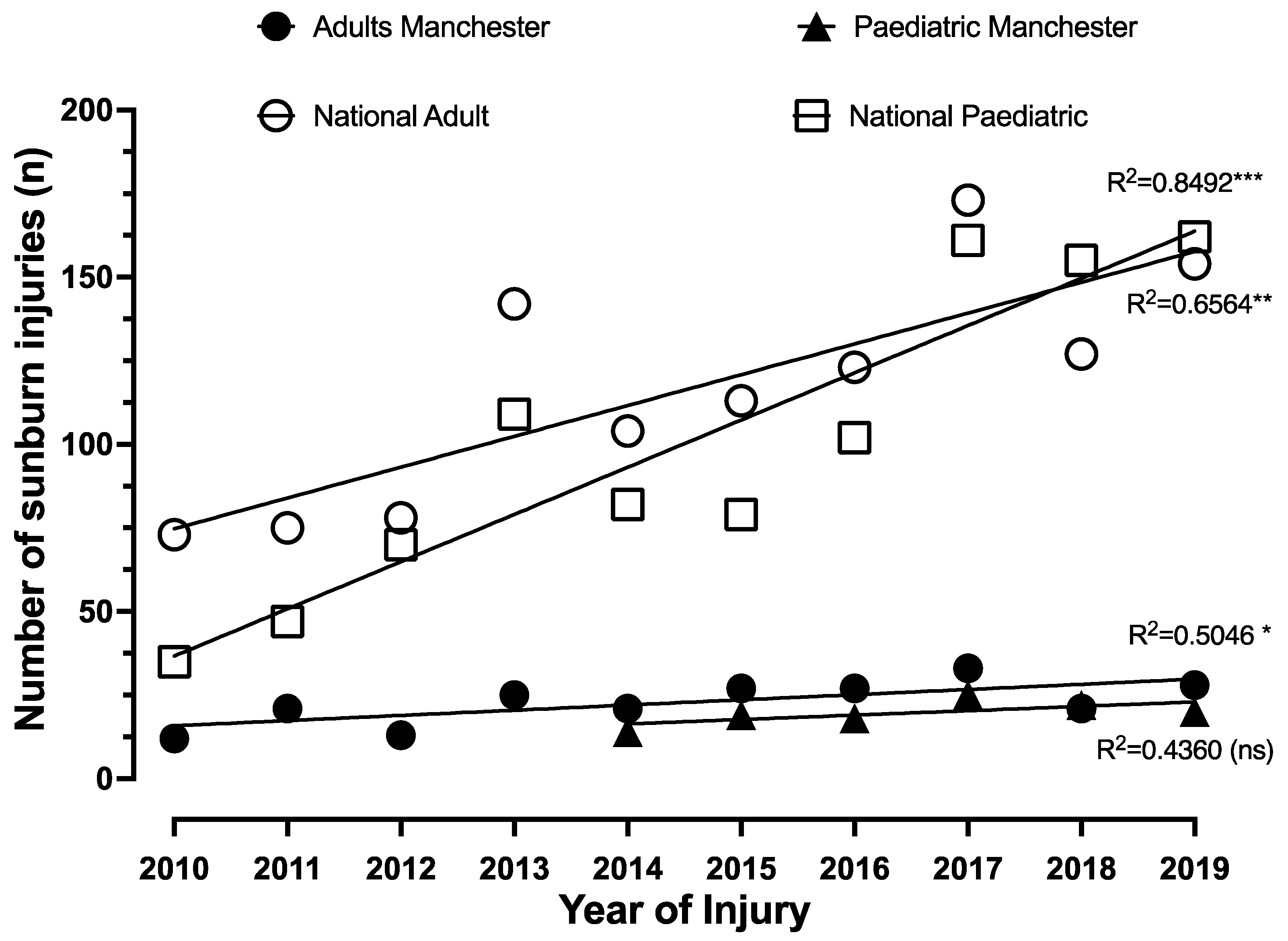
3.2. Chronological Trend in Sunburn Injuries
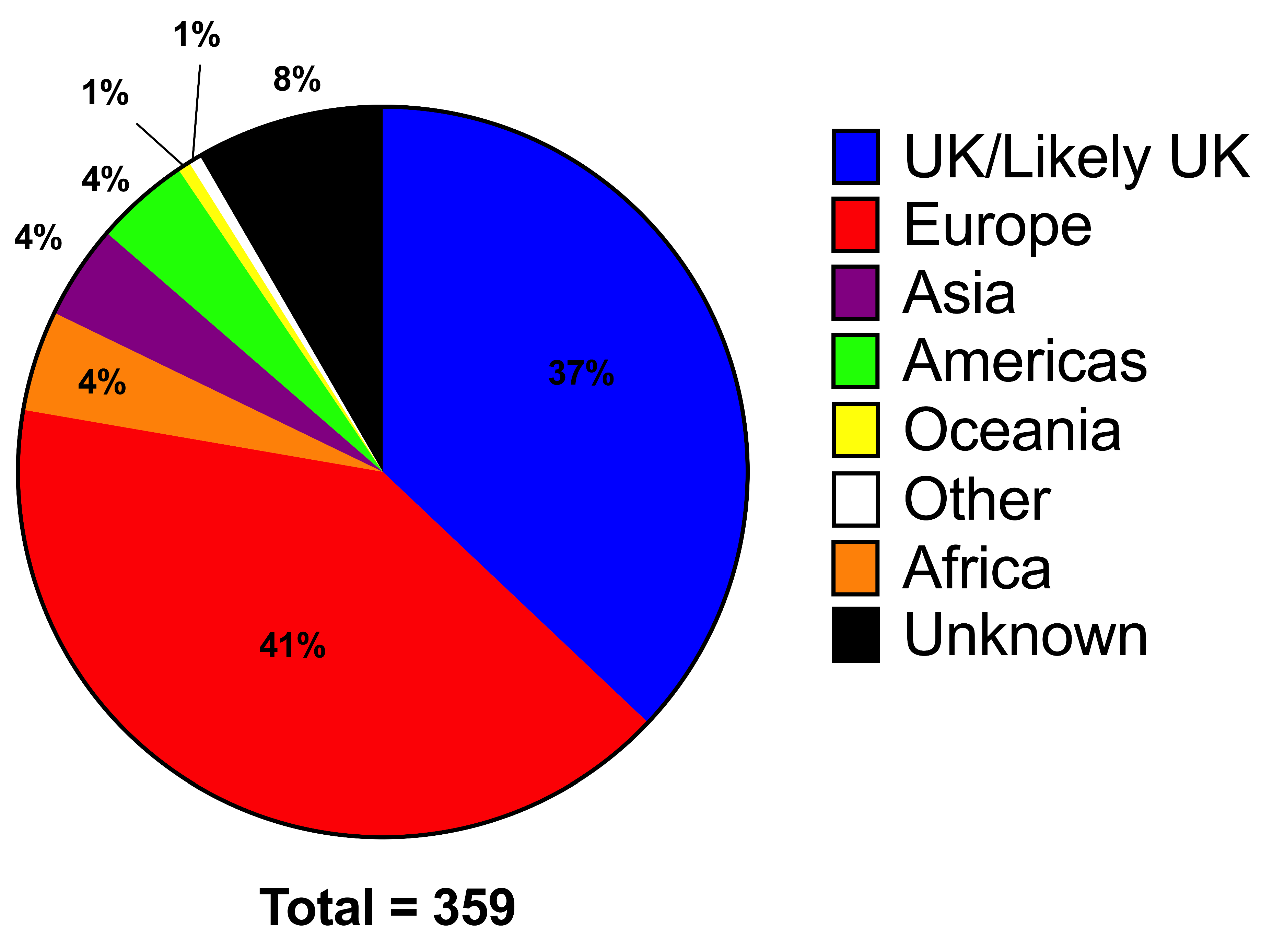
3.3. Geographical Location
3.4. National Data
3.4.1. Adults
3.4.2. Paediatric
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- ONS. Estimates of the Population for the UK, England and Wales, Scotland and Northern Ireland. 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed on 11 April 2022).
- Cancer Research UK. Half of Brits Got Sunburnt This Year and Many Would Do It Again. 2010. Available online: https://news.cancerresearchuk.org/2010/09/01/half-of-brits-got-sunburnt-this-year-and-many-would-do-it-again/ (accessed on 13 April 2022).
- Owen, J. UK Skin Cancer Statistics ‘Shocking’ as Sun-Worshippers Ingnore the Dangers of Exposure. [Newspaper Article]. 2015. Available online: https://www.independent.co.uk/life-style/health-and-families/health-news/uk-skin-cancer-statistics-shocking-as-sunworshippers-ignore-the-dangers-of-exposure-10221608.html (accessed on 11 April 2022).
- British Association of Dermatologists. Home and Away–Brits Getting Sunburnt in the UK and Abroad; British Association of Dermatologists: London, UK, 2017; Available online: https://www.skinhealthinfo.org.uk/home-and-away-brits-getting-sunburnt-in-the-uk-and-abroad/ (accessed on 13 April 2022).
- Cancer Research UK. UK Sunburn Risk: Third of Adults More Likely to Protect Their Skin Abroad than at Home. 2021. Available online: https://news.cancerresearchuk.org/2021/08/02/uk-sunburn-risk-third-of-adults-more-likely-to-protect-their-skin-abroad-than-at-home/ (accessed on 11 April 2022).
- Cancer Research UK. More than a Third of Brits Have Been Sunburnt in the UK in Past Year. 2014. Available online: https://news.cancerresearchuk.org/2014/06/26/more-than-a-third-of-brits-have-been-sunburnt-in-the-uk-in-past-year/ (accessed on 11 April 2022).
- Cancer Research UK. UK Rays Responsible for More than a Third of Most Recent Sunburn Cases. 2013. Available online: https://news.cancerresearchuk.org/2013/09/02/uk-rays-responsible-for-more-than-a-third-of-most-recent-sunburn-cases/ (accessed on 11 April 2022).
- de Troya-Martin, M.; de Gálvez-Aranda, M.V.; Rivas-Ruiz, F.; Blázquez-Sánchez, N.; Fernández-Morano, M.T.; Padilla-España, L.; Herrera-Ceballos, E. Prevalence and predictors of sunburn among beachgoers. Photodermatol. Photoimmunol. Photomed. 2018, 34, 122–129. [Google Scholar] [CrossRef]
- Cancer Research UK. Melanoma Skin Cancer Incidence Statistics. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/melanoma-skin-cancer/incidence (accessed on 12 April 2022).
- Kwiatkowska, M.; Ahmed, S.; Ardern-Jones, M.; Bhatti, L.A.; Bleiker, T.O.; Gavin, A.; Hussain, S.; Huws, D.W.; Irvine, L.; Langan, S.M.; et al. An updated report on the incidence and epidemiological trends of keratinocyte cancers in the United Kingdom 2013–2018. Skin Health Dis. 2021, 1, e61. [Google Scholar] [CrossRef] [PubMed]
- Lucas, R.M.; McMichael, A.J.; Armstrong, B.K.; Smith, W.T. Estimating the global disease burden due to ultraviolet radiation exposure. Int. J. Epidemiol. 2008, 37, 654–667. [Google Scholar] [CrossRef]
- Gandini, S.; Sera, F.; Cattaruzza, M.S.; Pasquini, P.; Picconi, O.; Boyle, P.; Melchi, C.F. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur. J. Cancer 2005, 41, 45–60. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.F.; Rumgay, H.; Dunlop, C.; Ryan, M.; Quartly, F.; Cox, A.; Deas, A.; Elliss-Brookes, L.; Gavin, A.; Hounsome, L.; et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br. J. Cancer 2018, 118, 1130–1141. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R. Almost Half of UK Parents Aren’t Worries about Sun Damage, according to New Research. 2018. Available online: https://www.independent.co.uk/life-style/health-and-families/half-uk-parents-danger-sun-damage-children-cancer-a8374396.html (accessed on 11 April 2022).
- Elsworthy, E. The UK Cities Where Children Are most at Risk of Sun Damage, according to Survey. 2019. Available online: https://www.independent.co.uk/news/sun-damage-children-cities-uv-radiation-suncream-a8898361.html (accessed on 11 April 2022).
- Met Office. Climate and Climate Change. UK and Regional Series. 2022. Available online: https://www.metoffice.gov.uk/research/climate/maps-and-data/uk-and-regional-series (accessed on 11 July 2022).
- Connolly, S.; Bertinetti, M.; Teague, W.J.; Gabbe, B.J.; Tracy, L.M. Sunburn Injuries Admitted to Burn Services in Australia and New Zealand. JAMA Dermatol. 2021, 157, 729–731. [Google Scholar] [CrossRef] [PubMed]
- Memon, A.; Bannister, P.; Rogers, I.; Sundin, J.; Al-Ayadhy, B.; James, P.W.; McNally, R.J.Q. Changing epidemiology and age-specific incidence of cutaneous malignant melanoma in England: An analysis of the national cancer registration data by age, gender and anatomical site, 1981–2018. Lancet Reg. Health Eur. 2021, 2, 100024. [Google Scholar] [CrossRef]
- Skcin.org. Skin Cancer: The problem and Facts. Available online: https://www.skcin.org/skinCancerInformation/theProblemAndFacts.htm (accessed on 11 April 2022).
- Cancer Research UK. 150% Surge in Skin Cancer Deaths since 70s. 2020. Available online: https://news.cancerresearchuk.org/2020/08/20/150-surge-in-skin-cancer-deaths-since-70s/ (accessed on 11 April 2022).
- Cancer Research UK. Melanoma Skin Cancer Mortality Statistics. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/melanoma-skin-cancer/mortality#heading-Three (accessed on 13 April 2022).
- Cancer Research UK. Non-Melanoma Skin Cancer Statistics. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/non-melanoma-skin-cancer#heading-Zero (accessed on 11 April 2022).
- Lashway, S.G.; Harris, R.B.; Farland, L.V.; O’Rourke, M.K.; Dennis, L.K. Age and Cohort Trends of Malignant Melanoma in the United States. Cancers 2021, 13, 3866. [Google Scholar] [CrossRef] [PubMed]
- Whiteman, D.C.; Whiteman, C.A.; Green, A.C. Childhood sun exposure as a risk factor for melanoma: A systematic review of epidemiologic studies. Cancer Causes Control 2001, 12, 69–82. [Google Scholar] [CrossRef]
- Oliveria, S.A.; Saraiya, M.; Geller, A.C.; Heneghan, M.K.; Jorgensen, C. Sun exposure and risk of melanoma. Arch. Dis. Child. 2006, 91, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Kimlin, M.G.; Guo, Y. Assessing the impacts of lifetime sun exposure on skin damage and skin aging using a non-invasive method. Sci. Total Environ. 2012, 425, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Andreola, G.M.; de Carvalho, V.O.; Huczok, J.; Cat, M.N.L.; Abagge, K.T. Photoprotection in adolescents: What they know and how they behave. An. Bras. Dermatol. 2018, 93, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Kolto, A.; Rodriguez, L.; McAvoy, H.; Gabhainn, S.N. Sunburn, Sun Safety and Indoor Tanning Among Schoolchildren in Ireland. Int. J. Public Health 2021, 66, 1604045. [Google Scholar] [CrossRef]
- Holman, D.M.; Ding, H.; Guy, G.P., Jr.; Watson, M.; Hartman, A.M.; Perna, F.M. Prevalence of Sun Protection Use and Sunburn and Association of Demographic and Behaviorial Characteristics With Sunburn Among US Adults. JAMA Dermatol. 2018, 154, 561–568. [Google Scholar] [CrossRef]
- Rajagopal, G.; Talluri, R.; Chuy, V.S.; Cheng, A.-L.; Dall, L. Trends in Sunscreen Use Among US Middle and High School Students, 2007–2019. Cureus 2021, 13, e16468. [Google Scholar] [CrossRef] [PubMed]
- Geller, A.C.; Colditz, G.; Oliveria, S.; Emmons, K.; Jorgensen, C.; Aweh, G.N.; Frazier, A.L. Use of Sunscreen, Sunburning Rates, and Tanning Bed Use Among More Than 10 000 US Children and Adolescents. Pediatrics 2002, 109, 1009–1014. [Google Scholar] [CrossRef]
- Thoonen, K.; Passos, V.L.; Schneider, F.; de Vries, H.; van Osch, L. Children’s sunburn exposed: Identification of sun exposure and parental sun protection patterns. Eur. J. Dermatol. 2021, 31, 538–548. [Google Scholar] [CrossRef]
- ONS. Overseas Travel and Tourism: 2020. 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/leisureandtourism/articles/overseastravelandtourism2020/2021-05-24#visits-abroad-by-uk-residents (accessed on 15 June 2022).
- VisitBritain, Great Britain Tourism Survey Decemeber 2019 Update. 2019. Available online: https://www.visitbritain.org (accessed on 26 June 2022).
- Cancer Research UK. UK Public Urged to Take Care This Summer as around 40% Spending More Time in the Sun Since COVID-19 Lockdown Cancer Research UK. 2020. Available online: https://news.cancerresearchuk.org/2020/07/22/uk-public-urged-to-take-care-this-summer-as-around-40-spending-more-time-in-the-sun-since-covid-19/ (accessed on 11 April 2022).
- Cowley, L.E.; Bennett, C.V.; Brown, I.; Emond, A.; Kemp, A.M. Mixed-methods process evaluation of SafeTea: A multimedia campaign to prevent hot drink scalds in young children and promote burn first aid. Inj. Prev. 2021, 27, 419–427. [Google Scholar] [CrossRef]
- British Association of Dermatologists. Sun Awareness Week Website. 2022. Available online: https://www.skinhealthinfo.org.uk/sun-awareness/sun-awareness-week/ (accessed on 15 June 2022).
- Henderson, S.I.; King, K.L.; Karipidis, K.K.; Tinker, R.A.; Green, A.C. Effectiveness, compliance and application of sunscreen for solar ultraviolet radiation protection in Australia. Public Health Res. Pract. 2022, 32, e3212205. [Google Scholar] [CrossRef]
- Young, A.R.; Narbutt, J.; Harrison, G.I.; Lawrence, K.P.; Bell, M.; O’Connor, C.; Olsen, P.; Grys, K.; Baczynska, K.A.; Rogowski-Tylman, M.; et al. Optimal sunscreen use, during a sun holiday with a very high ultraviolet index, allows vitamin D synthesis without sunburn. Br. J. Dermatol. 2019, 181, 1052–1062. [Google Scholar] [CrossRef]
- Walker, H.; Maitland, C.; Tabbakh, T.; Preston, P.; Wakefielda, M.; Sinclair, C. Forty years of Slip! Slop! Slap! A call to action on skin cancer prevention for Australia. Public Health Res. Pract. 2022, 32, e31452117. [Google Scholar] [CrossRef] [PubMed]
- Tabbakh, T.; Volkov, A.; Wakefield, M.; Dobbinson, S. Implementation of the SunSmart program and population sun protection behaviour in Melbourne, Australia: Results from cross-sectional summer surveys from 1987 to 2017. PLoS Med 2019, 16, e1002932. [Google Scholar] [CrossRef] [PubMed]
- Gordon, L.G.; Shihd, S.; Wattsd, C.; Goldsbury, D.; Green, A.C. The economics of skin cancer prevention with implications for Australia and New Zealand: Where are we now? Public Health Res. Pract. 2022, 32, 31502119. [Google Scholar] [CrossRef]
- Lorenc, T.; Jamal, F.; Cooper, C. Resource provision and environmental change for the prevention of skin cancer: Systematic review of qualitative evidence from high-income countries. Health Promot. Int. 2013, 28, 345–356. [Google Scholar] [CrossRef][Green Version]
- McNoe, B.M.; Morgaine, K.C.; Reeder, A.I. Effectiveness of Sun Protection Interventions Delivered to Adolescents in a Secondary School Setting: A Systematic Review. J. Skin Cancer 2021, 2021, 6625761. [Google Scholar] [CrossRef] [PubMed]
- Ventenilla, J.; França, K.; Lotti, T.; Keri, J. Psychosocial aspects associated with use of sunscreen, natural sunlight exposure, and artificial tanning. Wien. Med. Wochenschr. 2018, 168, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Rocholl, M.; Hannappel, J.; Ludewig, M.; John, S.M. UV-Induced Skin Cancer Knowledge, Sun Exposure, and Tanning Behavior among University Students: Investigation of an Opportunity Sample of German University Students. J. Skin Cancer 2021, 2021, 5558694. [Google Scholar] [CrossRef] [PubMed]
- Reinau, D.; Weiss, M.; Meier, C.R.; Diepgen, T.L.; Surber, C. Outdoor workers’ sun-related knowledge, attitudes and protective behaviours: A systematic review of cross-sectional and interventional studies. Br. J. Dermatol. 2013, 168, 928–940. [Google Scholar] [CrossRef] [PubMed]
- Khani Jeihooni, A.; Bashti, S.; Erfanian, B.; Ostovarfar, J.; Hasirini, P.A. Application of protection motivation theory (PMT) on skin cancer preventive behaviors amongst primary school students in rural areas of Fasa city-Iran. BMC Cancer 2022, 22, 21. [Google Scholar] [CrossRef]
- Diehl, K.; Lindwedel, K.S.; Mathes, S.; Görig, T.; Gefeller, O. Tanning Bed Legislation for Minors: A Comprehensive International Comparison. Children 2022, 9, 768. [Google Scholar] [CrossRef] [PubMed]
- Salvado, M.; Fraga, A.; Marques, D.L.; Pires, I.M.; Gonçalves, C.C.; Silva, N.M. Sun Exposure in Pediatric Age: Perspective of Caregivers. Children 2021, 8, 1019. [Google Scholar] [CrossRef] [PubMed]
- Seidel, N.; Fieber, V.; Breitbart, E.W.; Bornhäuser, M.; Stölzel, F. Cluster Randomized Trial: Sun Protection Intervention ‘Clever in Sun and Shade for Preschools’-Effectiveness and Dissemination. Children 2021, 8, 651. [Google Scholar] [CrossRef]
- Gordon, L.G.; Hainsworth, R.; Eden, M.; Epton, T.; Lorigan, P.; Grant, M.; Green, A.C.; Payne, K. Sunbed Use among 11- to 17-Year-Olds and Estimated Number of Commercial Sunbeds in England with Implications for a ‘Buy-Back’ Scheme. Children 2021, 8, 393. [Google Scholar] [CrossRef] [PubMed]
- Eden, M.; Hainsworth, R.; Gordon, L.G.; Epton, T.; Lorigan, P.; Rhodes, L.E.; Marais, R.; Green, A.C.; Payne, K. Cost-effectiveness of a policy-based intervention to reduce melanoma and other skin cancers associated with indoor tanning. Br. J. Dermatol. 2022, 187, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B.; Boucher, B.J. An Exploration of How Solar Radiation Affects the Seasonal Variation of Human Mortality Rates and the Seasonal Variation in Some Other Common Disorders. Nutrients 2022, 14, 2519. [Google Scholar] [CrossRef] [PubMed]
- Kent, S.T.; Kabagambe, E.K.; Wadley, V.G.; Howard, V.J.; Crosson, W.L.; Al-Hamdan, M.Z.; Judd, S.E.; Peace, F.; McClure, L.A. The relationship between long-term sunlight radiation and cognitive decline in the REGARDS cohort study. Int. J. Biometeorol. 2014, 58, 361–370. [Google Scholar] [CrossRef]
- Juzeniene, A.; Moan, J. Beneficial effects of UV radiation other than via vitamin D production. Dermato-Endocrinology 2012, 4, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Kent, S.T.; McClure, L.A.; Crosson, W.L.; Arnett, D.K.; Wadley, V.G.; Sathiakumar, N. Effect of sunlight exposure on cognitive function among depressed and non-depressed participants: A REGARDS cross-sectional study. Environ. Health 2009, 8, 34. [Google Scholar] [CrossRef]
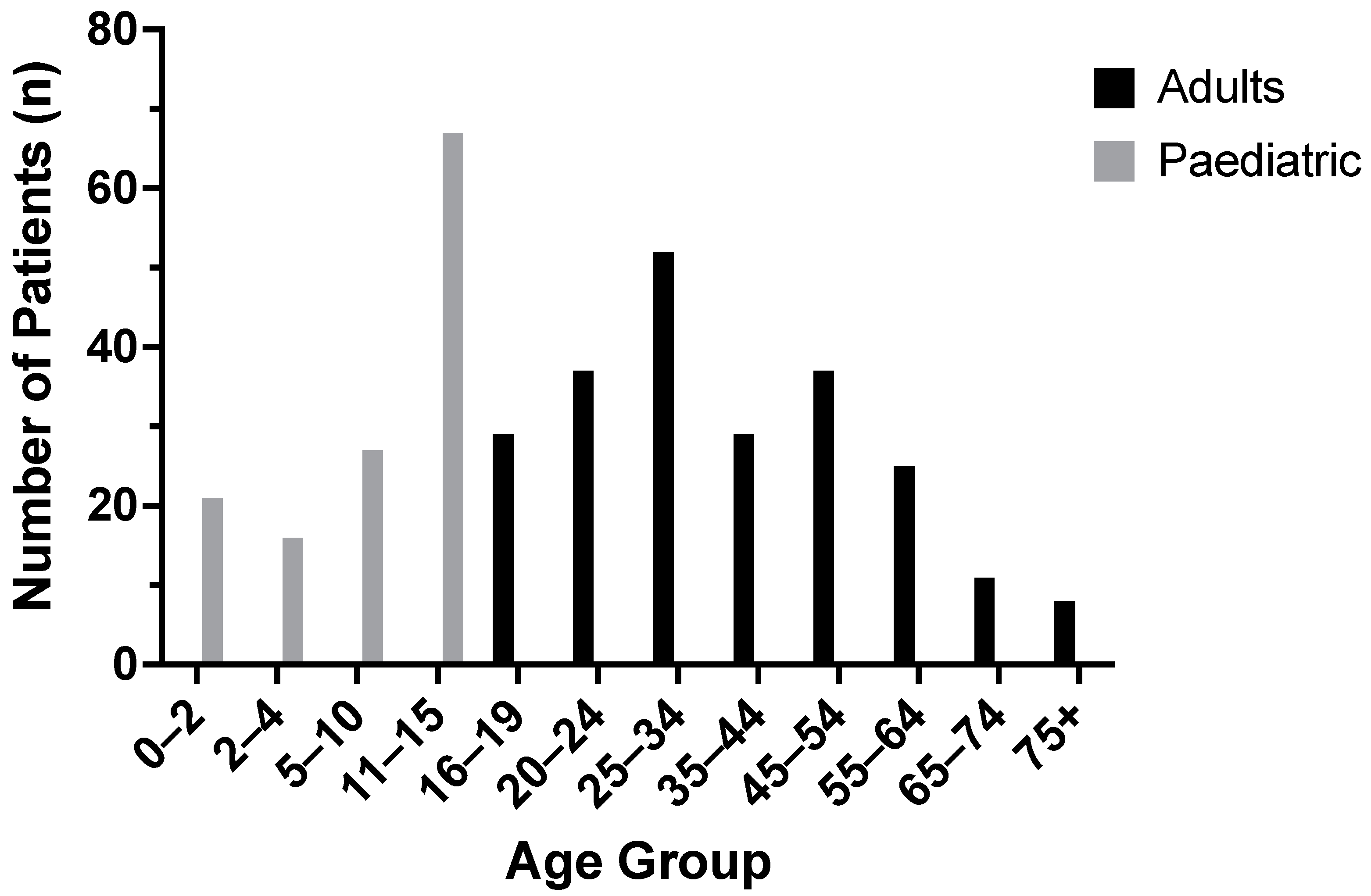
| Adult | Paediatric | |
|---|---|---|
| Total Patients, n | 228 | 131 |
| Male | 118 | 88 (67.2%) |
| Female | 110 | 43 (32.8%) |
| Age (years) | 16–19—29 (12.7%) | 0–1—21 (16.0%) |
| Patients [n, (% of total)] | 20–24—37 (16.2%) | 2–4—16 (12.2%) |
| 25–34—52 (22.8%) | 6–10—27 (20.6%) | |
| 35–44—29 (12.7%) | 11–15—75 (15.1%) | |
| 45–54—37 (16.2%) | ||
| 55–64—25 (11.0%) | ||
| 65–74—11 (4.8%) | ||
| 75+—8 (3.5%) | ||
| Mean [years, (SD, range)] | 32.0 (17.3, 16–83) | 8.9 (5.0, 0–15) |
| Total Burn TBSA [Patients, n (% total)] | ||
| 0 | 33 (14.5%) | 0 |
| 0–0.9 | 68 (29.8%) | 42 (32.1%) |
| 1–4 | 96 (31.6%) | 76 (58.05) |
| 5–9 | 23 (10.1%) | 13 (9.9%) |
| 10–14 | 6 (2.6%) | 0 |
| ND | 2 (0.9%) | 0 |
| Mean [%, (SD)] | 2.00 (2.53) | 2.12 (1.85) |
| Median (%) | 1 | 1.5 |
| Range (%) | 0–14 | 0–9 |
| Burn Depth | ||
| Superficial/SPT | ||
| Patients [n, (% of total)] | 185 ⤈ (81.1%) | 131 (100%) |
| Mean TBSA * [%, (SD)] | 2.22 (2.37) | 2.09 (1.84) |
| Median TBSA * (%) | 1.5 | 1.5 |
| Range | 0–14 | 0–9 |
| DPT/FT | ||
| Patients [n, (% of total)] | 11 ⤈ (4.8%) | 1 (0.8%) |
| Mean TBSA * [%, (SD)] | 0.44 (0.50) | N/A |
| Median TBSA * (%) | 0.1 | N/A |
| Range | 0–1.5 | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dingle, L.A.; Tan, P.; Malik, P.; McNally, S. A 10-Year Review of Sunburn Injuries Presenting to the Manchester Adult and Paediatric Specialist Burn Services. Eur. Burn J. 2022, 3, 472-485. https://doi.org/10.3390/ebj3040041
Dingle LA, Tan P, Malik P, McNally S. A 10-Year Review of Sunburn Injuries Presenting to the Manchester Adult and Paediatric Specialist Burn Services. European Burn Journal. 2022; 3(4):472-485. https://doi.org/10.3390/ebj3040041
Chicago/Turabian StyleDingle, Lewis A., Poh Tan, Parisha Malik, and Samantha McNally. 2022. "A 10-Year Review of Sunburn Injuries Presenting to the Manchester Adult and Paediatric Specialist Burn Services" European Burn Journal 3, no. 4: 472-485. https://doi.org/10.3390/ebj3040041
APA StyleDingle, L. A., Tan, P., Malik, P., & McNally, S. (2022). A 10-Year Review of Sunburn Injuries Presenting to the Manchester Adult and Paediatric Specialist Burn Services. European Burn Journal, 3(4), 472-485. https://doi.org/10.3390/ebj3040041






