Abstract
A proxy-assessment of health-related quality of life (HRQL) may be an alternative for burn patients who are medically unable to self-report shortly after being admitted to the hospital. This study examined the patient–partner agreement on the recalled pre-injury HRQL of burn patients. In a multi-centre study of 117 patient–partner pairs, the recalled pre-burn HRQL was assessed with the EQ-5D-3L + Cognition during the acute phase following the burns. Agreement was evaluated with Kappa and ICC statistics. Burn severity and PTSD symptoms were assessed as potential predictors of disagreement. The results showed that pre-burn EQ-Index scores were similar to population norms, whereas the EQ Visual Analog Scale (EQ-VAS) scores of patients were significantly higher. Agreement varied across EQ-5D domains and, after adjusting for prevalence, was substantial to almost perfect. Average agreement on the EQ-Index and EQ-VAS was, respectively, substantial and moderate, but differences between partners were larger at lower levels of HRQL, and specifically in the pain/discomfort domain. Patient–partner differences could not be explained by the patient’s age or gender, number of surgeries, partner’s presence at the burn event, or post-traumatic stress disorder (PTSD) symptoms of either the patient or partner. In conclusion, patient–partner agreement is substantial and partner–proxy reports of pre-burn EQ-5D domains and EQ-Index scores may be used to complement or serve as a substitute for the patient’s assessment. Given the moderate agreement on the EQ-VAS, it may be less suited for proxy assessment.
1. Introduction
A severe burn injury can vastly impact the patient’s physical, psychological, and social well-being. Consequently, reduced levels of health-related quality of life (HRQL) [1] are common within the first year post-burn [2]. A growing number of studies have assessed pre-burn HRQL [3,4], which may serve as a reliable benchmark for patient recovery of HRQL and may aid prognosis and treatment choices [5]. Since sustaining burns is an unexpected event, pre-burn functioning is preferably assessed retrospectively and within the first weeks after the injury [6,7]. Compared to a prospective assessment, a retrospective assessment carries the risk of recall bias, but prevents bias related to scale recalibration or response shift [8]. To estimate pre-burn health status more accurately, partner–proxy assessment may complement the patient’s self-reporting, since partners are well aware of the patient’s pre-burn functioning. Alternatively, the partner’s proxy assessment may serve as a substitute for the patient’s assessment if medical status prevents timely self-report by the patient. In that case, data collection by proxy may avoid systematic non-participation and reduce missing data [7,9].
In general, proxies of critically ill patients tend to report lower levels of HRQL than patients, both prospectively [10,11] and retrospectively [12,13]. Furthermore, patients usually report pre-injury HRQL levels that are higher than population norms [14]. Proxy agreement of (pre-injury) HRQL has not been studied in the adult burn population, but studies in intensive care unit (ICU) patients have shown varying levels of pre-injury agreement, ranging from slight-to-moderate [13,15,16] to moderate-to-high agreement (e.g., [17,18]).
For clinical decision making, reliance on proxy judgements in the absence of self-report may have significant implications for the evaluation of the success of care and treatment. To better understand the origin of proxy–patient disagreement and to estimate whether the partner is a reliable proxy, it is important to study factors that may predict disagreement [9,19]. First, the level of HRQL impairment may impact agreement, in either a linear or u-shaped relation [9]. Some empirical research shows lower levels of agreement in relation to more impaired functioning [9,19,20], while another study showed larger discrepancies for patients with moderately impaired health rather than for those with either good or poor health [21]. Second, it is important to study the relation between burn severity and patient–partner disagreement to establish the accuracy of proxy reports for more severely burned patients. Indeed, proxy–patient agreement may be most relevant for patients who are medically unable to self-report their HRQL [9]. Third, agreement may partly depend on the concreteness of the domains under consideration. That is, proxies may have most difficulty in assessing the more subjective domains (e.g., anxiety and depression) compared to more objective physical aspects (e.g., mobility and self-care [17,20]). Fourth, increased levels of post-traumatic stress disorder (PTSD) symptoms may be related to patient–partner differences. Increased levels of PTSD symptoms have been reported in both patients with burns [22] and their partners [23,24], and memory disturbances, which are part of the PTSD diagnostic criteria [25], have been related to its symptoms [26]. Empirical evidence shows that increased PTSD symptom levels were related to changes in recalled pre-injury HRQL over a period of 12 months [27], exemplifying the possible effect of PTSD symptoms on the recollection of pre-injury HRQL.
The aim of the current study was twofold. First, to compare recalled pre-burn HRQL from patients and their proxies (partners) to population norms and second, to evaluate patient–partner agreement on the recall of a patient’s pre-burn HRQL and study factors related to discrepancies. In line with relevant factors reported in the literature, the effect of HRQL impairment, burn severity, and PTSD symptoms on patient–partner differences was studied.
2. Materials and Methods
2.1. Inclusion and Procedure
The data in this study were collected as part of a larger project concerning the social impact of burns. All consecutively admitted patients and their partners were invited to participate by a local researcher during the patient’s stay in one of the three Dutch or three Belgian burn centres. Recruitment took place between October 2013 and October 2015. The patients’ pre-burn HRQL data were also part of previous work that described patients’ recovery to pre-burn HRQL [28]. In the current study, a subsample of patients with a participating partner was studied. The larger project was approved by the ethics boards in The Netherlands and Belgium (NL44682.094.13 and B670201420373). Inclusion criteria for patients were a hospital stay of >24 h following the burn event, age ≥18 years and proficiency in Dutch. The latter two criteria also applied to the partners. Exclusion criteria were psychiatric problems that interfere with the comprehension of questionnaires (e.g., psychosis, cognitive problems), and inhalation injury without external burns. After receiving oral and written study information, the participants provided informed written consent.
2.2. Measures
2.2.1. Recalled Pre-Burn Health-Related Quality of Life
The EQ-5D-3L + cognition [29] is a self-report scale used to assess generic HRQL and was administered in the acute phase following the burn injury (Mpatients = 22 days post-burn, SD = 23; Mpartners = 24 days post-burn, SD = 24). The HRQL was assessed along five single-item health domains: mobility, self-care, usual activities, pain and anxiety/depression as well as the added cognition domain, which measured the extent to which the patient experienced problems with memory and concentration. For each domain, patients and partners independently recalled the patient’s health before the burn event from their own perspective. Answers were rated on a 3-point scale: “no problems”, “moderate problems”, or “severe problems”. The first five domains were combined into the EQ-5D Index (EQ-Index) using calculations based on the European Visual Analog Scale (VAS) value set [30]. The resulting EQ-Index ranges from 0 “death” to 1 “full health”. In addition, the EQ-5D includes an EQ-VAS that is scaled vertically and runs from 0 (worst imaginable health state) to 100 (best imaginable health state). The EQ-5D, which is short and easy to complete, is often used after burns [31] and has good feasibility and reasonable criterion validity in the burn population [32]. The addition of a cognition domain slightly improved the psychometric performance of the EQ-5D in traumatic brain injury patients [33].
2.2.2. Posttraumatic Stress Disorder Symptoms
The Impact of Event Scale-Revised (IES-R; [34]) was used to assess patient and partner PTSD symptoms in the acute phase following the burn event. The IES-R is a 22-item self-reporting questionnaire that measures three PTSD symptom clusters––intrusion, avoidance and hyper-arousal––over the previous week. Answers were given on a 5-point Likert scale and summed to obtain a total score, and sumscores ≥ 33 indicated a possible diagnosis of PTSD [35]. If at least 19 of the 22 items were completed, the sum scores were calculated based on the mean of the completed items. The IES-R was validated in Dutch trauma populations and showed good psychometric properties [36]. Reliability of the IES-R in the current study was excellent, with a Cronbach’s alpha of 0.95 for patients and 0.93 for partners.
2.2.3. Burn Characteristics
The total body surface area (TBSA) burned, number of surgeries and need for mechanical ventilation were recorded from the medical file. The TBSA is the estimated percentage of the body covered with partial and full thickness burns. The number of surgeries indicates the number of skin graft procedures that was required to cover the wounds, and it is used as an indicator of burn severity. Presence at the burn event was self-reported by the partner.
2.3. Statistical Analysis
First, the pre-burn EQ-Index and EQ-VAS scores of patients and their partners were compared to gender-and-age adjusted population norms from a national representative sample of the non-institutionalized adult population of their country: Belgium or The Netherlands [37]. One-sample Student’s t-tests were used to test the differences for significance.
Second, agreement between patients and partners on the six domains of the EQ-5D was assessed using Cohen’s Kappa with 95% confidence intervals. Linear weights were applied to account for the ordinal structure in the data [38], and a prevalence-adjusted weighted kappa [39] was reported. A prevalence effect may be present if the majority of the sample reported the same response option, (e.g., “no problems”) on a given EQ-5D domain, causing large absolute differences among the counts in the cells of agreement (i.e., the cells on the diagonal of a cross-table). These differences increase the proportion of agreement expected by chance, thereby reducing the kappa, even with a large proportion of absolute agreement. To obtain a prevalence-adjusted kappa (PAK) the cells of agreement were replaced by their combined average before calculating the weighted kappa [39]. For the EQ-Index and EQ-VAS, agreement was assessed by the intraclass correlation coefficient (ICC) using a two-way random effects model for absolute agreement [40]. Differences in the EQ-Index and EQ-VAS were also compared to the minimally important difference (MID), which indicates the minimum change that reflects a clinically relevant change in the HRQL. For the EQ-Index, a MID of 0.074 was used, based on a study in patients with a wide range of medical conditions [41]. For the EQ-VAS, an MID of 8 was chosen, based on several studies in specific (non-burn) patient populations [42,43,44]. The MIDs were established using both anchor- and distribution-based methods. For the kappa and ICC coefficients, 0.00 to 0.20 was considered slight, 0.21 to 0.40 fair, 0.41 to 0.60 moderate, 0.61 to 0.80 substantial, and 0.81 to 1.00 almost perfect agreement [45].
Third, differences between patients and partners regarding EQ-Index and EQ-VAS scores were further tested using paired Student’s t-tests. Bland–Altman plots were generated to visually inspect the difference between patients and partners in relation to the combined mean of the patient and partner responses [46]. The mean difference and limits of agreement (95% confidence interval) were also calculated. Furthermore, the effects of gender, age, burn severity, partner’s presence at the burn event, and PTSD symptoms on patient–partner differences on the EQ-Index and the EQ-VAS were examined in multiple regression analyses. A p-value < 0.05 was considered significant. Analyses were performed using IBM SPSS 24 (IBM Corp., Armonk, NY, USA).
3. Results
3.1. Descriptive Analyses
The final sample consisted of 117 pairs of patients with burns and their partners. Of the 266 originally participating patients, 71 reported no partner and 8 did not say. Of the remaining 187 patients with a partner, 117 (62.6%) couples completed the pre-burn HRQL measure and were included in the study. Comparing the 117 included couples to the 70 couples with incomplete data and to the 79 patients without a partner, no statistically significant differences (p > 0.05) were observed with respect to patient’s gender, patient’s reported pre-burn and post-burn HRQL, TBSA burned, and number of surgeries. However, the 79 patients without a partner were significantly younger (M = 39.2, SD = 16.9) than the included patients (M = 45.8, SD = 15.1, p = 0.012) and the patients with incomplete couple data (M = 45.7, SD = 14.5, p = 0.035).
The patients had a mean age of 45.8 years (SD = 15.1); for partners this was 44.4 years (SD = 14.4). Most pairs consisted of a male patient and a female partner (n = 90, 76.9%); the remainder were female patients with a male partner (n = 27, 23.1%). The patient’s mean total body surface area (TBSA) burned was 10.4% (SD = 11.1, range 1.0–75.0). The median number of surgeries was 1 (range 0–14). For further analyses, this variable was categorised as: “no surgeries” (n = 53; 45.3%), “one surgery” (n = 39; 33.3%) or “more than one surgery” (n = 25; 21.4%). Forty-four partners (40%) were present at the burn event. The number of patients with clinically relevant levels of PTSD symptoms was 21 (18.1%); for partners, this was 34 (29.1%). One patient did not complete the IES-R.
3.2. Recalled Pre-Burn HRQL Compared to Population Norms
Table 1 describes the average pre-burn EQ-Index and EQ-VAS, reported by both patients and their partners. Compared to age, gender and country specific population norms [37], the EQ-Index from both patients and partners did not deviate significantly from the adjusted norm. Patients’ EQ-VAS was on average 4 points higher than the adjusted population norms, which was a significant difference but within the bounds of the MID. Partners’ EQ-VAS did not differ significantly from the population norms.

Table 1.
Descriptive and one-sample t-test results for the comparison of pre-burn EQ-Index and EQ-VAS of patients and partners (proxy) with population norms.
3.3. Agreement
Table 2 shows that most patients and partners reported no problems in a specific EQ-5D domain. Exact agreement was around 90% for most domains except for pain (71.8%). Agreement based on the weighted kappa, ranged from slight to substantial for the six EQ-5D domains. After adjustment for prevalence, the weighted kappa (PAKw) was considerably higher and indicated substantial-to-almost-perfect agreement for the six domains. Agreement according to the PAKw was the lowest for pain/discomfort and highest for mobility. Exact agreement for the EQ-Index was acceptable, but exact agreement for the EQ-VAS was low even if defined within the borders of the MID. The single-rater ICC for the EQ-Index and EQ-VAS was, respectively, moderate and fair, and the average inter-rater ICC was substantial and moderate.

Table 2.
Agreement between patients and partners on pre-burn EQ domains, EQ-Index and EQ-VAS.
3.4. Predictors of Differences on the EQ-Index and the EQ-VAS
Patients reported significantly higher pre-burn EQ-Index scores than their partners, (t(116) = 2.93, p = 0.009), but the mean paired difference of 0.05 (see Table 1) lies within the MID. The mean paired difference on the EQ-VAS was 3.0 and was not significant (t(106) = 1.89, p = 0.062). To examine the relation between patient–partner differences and possible explaining factors, differences on the EQ-Index and EQ-VAS were regressed on the couple’s mean score, patient’s age and gender, number of surgeries, partner’s presence at the burn event, and PTSD symptoms of both patients and partners. The regression models were not significant for either the EQ-Index, (F (8, 100) = 0.83, p = 0.58, R2 = 0.25) or the EQ-VAS, (F (8, 90) = 1.50, p = 0.17, R2 = 0.34), indicating that the predictors did not significantly add to the prediction of systematic differences. Absolute differences between patients and partners were significantly correlated to couple’s mean scores for both the EQ-Index (r = −0.61, p < 0.001) and EQ-VAS (r = −0.53, p < 0.001), indicating that differences between patients and partners tended to be larger at lower EQ-Index and EQ-VAS scores. The Bland–Altman plots of actual differences between patients and partners in Figure 1 illustrate this relationship. The plots also show that on both the EQ-Index and the EQ-VAS, extreme differences were reported that fell outside the confidence intervals.
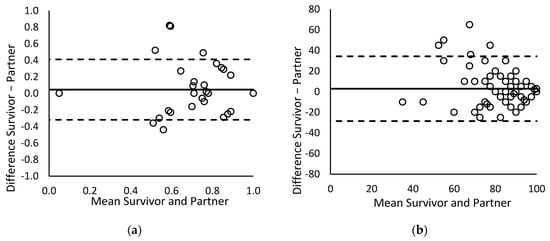
Figure 1.
Bland–Altman plots of differences between patient and partner ratings against the mean of both ratings for (a) the EQ-Index and (b) the EQ-VAS. The horizontal lines represent the mean difference and limits of agreement (95% Confidence Interval around the mean difference).
4. Discussion
This study examined patient–partner agreement on the retrospectively recalled pre-burn HRQL. EQ-Index scores from both patients and partners were comparable to population norms, whereas the patients’ EQ-VAS scores were higher. Agreement varied across the six EQ-5D domains, but after adjustment for prevalence, it was substantial to almost perfect. The average inter-rater agreement on the EQ-Index and EQ-VAS was, respectively, substantial and moderate. On average, patients reported a higher pre-burn EQ-Index compared to partners. Differences were larger at lower HRQL levels, but could not be explained by demographic or burn-related factors or by the PTSD symptoms of patients and partners.
Compared to age- and gender- adjusted population norms, the EQ-Index scores from both perspectives were comparable to the norm scores, but patients’ EQ-VAS scores exceeded the norms, whereas the partners’ did not. However, post hoc analyses excluding three extremely low-scoring partners (with high-scoring patients), showed that, on average partners may also exceed population norms. This was in line with studies that reported a pre-injury HRQL above population norms [14,47,48]. Deviation from the norms on the EQ-VAS, but not the EQ-Index, may be related to a more subjective interpretation of the EQ-VAS compared to the more objectively rated EQ domains [8], which makes the EQ-VAS more prone to recall bias and response shift. Recall bias may cause inflated pre-burn EQ-VAS scores, because of the idealization of the pre-burn situation [14]. Alternatively, and especially in patients themselves, the experience of the burn event may cause a response shift—an change in the internal standards of what constitutes “good” health [49,50]—resulting in a more highly recalled EQ-VAS than in the (mostly uninjured) norm population, and possibly making comparisons to the norm populations less valid.
The EQ-Index outperformed the EQ-VAS on both the single-rater and the average inter-rater agreement. Single-rater agreement on the EQ-Index and EQ-VAS was, respectively, moderate and fair, and the average inter-rater agreement was substantial and moderate. However, the ICC estimates may have been compromised by three extremely low scoring partners. Indeed, post hoc analyses, excluding these cases, showed that all ICC estimates increased by about 0.10. Agreement according to the unadjusted weighted kappa was only fair in most individual domains. These results fit within the wide range of agreement levels reported in the ICU literature (e.g., [13,15,16,17,18]), and are the first assessment of proxy agreement in the adult burn population. However, the current study showed that the kappa for pre-burn HRQL is highly affected by prevalence [39] since the vast majority of patients and partners reported no problems in any EQ-5D domain. Adjustment for prevalence revealed almost perfect agreement between patients and partners on mobility, self-care, usual activities, and anxiety/depression, and substantial agreement for pain/discomfort and cognition. Agreement was the lowest on the pain/discomfort domain, which is not surprising, given that pain is a subjective experience that cannot directly be observed by others [51]. Besides, the experience of severe burn-related pain may have especially recalibrated the patient’s interpretation of pain [8,49], while the partner’s interpretation may not have changed that much, resulting in disagreement on pre-burn levels of pain. The results partly support previous findings, showing that proxies have more difficulty in assessing subjective domains compared to more the objective physical aspects of HRQL [17,20] although (prevalence adjusted) agreement on anxiety/depression was high in the current study.
The analyses of patient–partner differences showed that patients reported higher levels of pre-burn HRQL than partners, in line with the ICU literature [12,13]. However, post hoc inspection of the data revealed that these differences were partly driven by a few partners who reported an extremely low pre-burn HRQL. These partners may have erroneously reported on the post-burn HRQL of the patient. Nevertheless, the Bland–Altman plots showed that differences between the two informants were larger at lower levels of HRQL. Although this supports the idea of a linear relationship between agreement and functioning, we cannot exclude the existence of a u-shaped relationship due to the lack of data in the lower HRQL spectrum [9]. Furthermore, it should be noted that the relationship between absolute differences and a couple’s mean HRQL scores may also be the consequence of a ceiling effect because the majority of couples reported a perfect pre-burn health state (i.e., the maximum of 1 on the EQ-Index), preventing variability at the higher end of the spectrum. Differences on the EQ-Index and EQ-VAS were not related to burn severity, indicating that proxy reports were similarly accurate for severely and less severely burned patients. Furthermore, differences were also not explained by the PTSD symptoms of patients or partners, indicating that the symptoms did not disturb agreement in any direction. Further research should investigate patient–partner agreement and differences with respect to the post-burn HRQL because it may well be that these factors do relate to post-burn differences.
Some limitations of this study should be noted. First, the sample was mostly restricted to patients with good pre-burn health, limiting generalizability to those who have low levels, especially since the results showed that differences between patients and partners increased at lower levels of a pre-burn HRQL. Second, the results cannot be generalized over other close relatives because the sample was limited to partners. Future research could compare multiple proxy perspectives (e.g., adult children, parents and siblings) to evaluate the eligibility of each of these proxies. Third, the partners were only asked to estimate a patient’s pre-burn health status, which precludes conclusions about agreement on post-burn HRQL. An assessment of both the pre-burn and post-burn HRQL by the partners could also have reduced the possibility of their erroneously evaluating the current HRQL instead of the pre-burn HRQL, which could explain some of the extreme differences between patients and partners in the current study. Fourth, about half of the patients and partners completed the pre-burn assessment after the recommended two weeks post-injury [7], which may have increased the possibility of recall bias. Although we cannot rule out recall bias on the EQ-5D Index, the average recalled pre-burn scores of both patients and partners did not differ from prospectively assessed population norms, which is a preliminary indication that no substantial recall bias (or response shift) occurred for the EQ-Index. Recall bias and response shift more likely have occurred on the EQ-VAS because of the subjective nature of this scale. Future research could investigate the effects of recall bias and response shift on the retrospective assessment of pre-burn functioning.
In conclusion, this study demonstrated that patient–partner agreement on the pre-burn HRQL is substantial. These results are a first indication that partner reports of pre-burn EQ domains may be reliably used to complement or, if needed, substitute for the patient’s assessment for research purposes. For monitoring the patient’s recovery in clinical practice, partner assessment may also substitute for the patient’s assessment if the patient is medically not able to self-report. However, the pain/discomfort domain may be more difficult to assess for partners, so it should be interpreted with caution. Furthermore, the EQ-VAS may be less suited for proxy reporting because of its subjective interpretation and lower level of agreement. Further research on proxy agreement is needed to evaluate the use of a proxy in the post-burn context and to evaluate the eligibility of other close relatives as proxies.
Author Contributions
Conceptualization, E.B.-v.D. and N.E.E.V.L.; methodology, E.B.-v.D. and N.E.E.V.L.; formal analysis, E.B.-v.D.; data collection, H.W.C.H., data curation, E.B.-v.D. and N.E.E.V.L.; writing—original draft preparation, E.B.-v.D.; writing—review and editing, H.W.C.H., A.E.E.d.J. and N.E.E.V.L.; funding acquisition, N.E.E.V.L.; All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Dutch Burn Foundation, grant numbers 12.105 and 17.102.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of METC NoordHolland (protocol code NL44682.094.13, date: 11 October 2013) in The Netherlands and Commissie voor Medische Ethiek Universiteit Gent in Belgium (protocol code B670201420373, date: 27 May 2014).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to them containing information that could compromise participant privacy.
Acknowledgments
This study represents the collaborative efforts of the Dutch–Belgian psychosocial research group, consisting of J. Meijer, A. Boekelaar, A.S. Goemanne, E. Vandermeulen, I. Bastiansen, and L. Braem, representing the burn centers in Groningen, Beverwijk, Rotterdam, Ghent, Brussels, and Antwerp.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Testa, M.A.; Simonson, D.C. Assessment of Quality-of-Life Outcomes. N. Engl. J. Med. 1996, 334, 835–840. [Google Scholar] [CrossRef]
- Spronk, I.; Legemate, C.; Oen, I.; van Loey, N.; Polinder, S.; van Baar, M. Health related quality of life in adults after burn injuries: A systematic review. PLoS ONE 2018, 13, e0197507. [Google Scholar] [CrossRef] [Green Version]
- Abouzeid, C.A.; Wolfe, A.E.; Ni, P.; Carrougher, G.J.; Gibran, N.S.; Hammond, F.M.; Holavanahalli, R.; McMullen, K.A.; Roaten, K.; Suman, O.; et al. Are Burns a Chronic Condition? Examining Patient Reported Outcomes up to 20 Years after Burn Injury—A Burn Model System National Database Investigation. J. Trauma Acute Care Surg. 2022. [Google Scholar] [CrossRef]
- Sibbett, S.H.; Carrougher, G.J.; Pham, T.N.; Mandell, S.P.; Arbabi, S.; Stewart, B.T.; Gibran, N.S. Burn survivors’ perception of recovery after injury: A Northwest Regional Burn Model System investigation. Burns 2020, 46, 1768–1774. [Google Scholar] [CrossRef]
- Hofhuis, J.G.; Spronk, P.E.; van Stel, H.F.; Schrijvers, G.J.; Rommes, J.H.; Bakker, J. The impact of critical illness on perceived health-related quality of life during ICU treatment, hospital stay, and after hospital discharge: A long-term follow-up study. Chest 2008, 133, 377–385. [Google Scholar] [CrossRef]
- Polinder, S.; Haagsma, J.A.; Belt, E.; Lyons, R.A.; Erasmus, V.; Lund, J.; van Beeck, E.F. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health 2010, 10, 783. [Google Scholar] [CrossRef] [Green Version]
- Van Beeck, E.F.; Larsen, C.F.; Lyons, R.A.; Meerding, W.J.; Mulder, S.; Essink-Bot, M.L. Guidelines for the conduction of follow-up studies measuring injury-related disability. J. Trauma 2007, 62, 534–550. [Google Scholar] [CrossRef]
- Blome, C.; Augustin, M. Measuring change in quality of life: Bias in prospective and retrospective evaluation. Value Health 2015, 18, 110–115. [Google Scholar] [CrossRef] [Green Version]
- von Essen, L. Proxy ratings of patient quality of life--factors related to patient-proxy agreement. Acta Oncol. 2004, 43, 229–234. [Google Scholar] [CrossRef] [Green Version]
- Tol, M.C.J.M.; Kuipers, J.P.; Willigenburg, N.W.; Willems, H.C.; Poolman, R.W. How are you doing in the eyes of your spouse? Level of agreement between the self-completed EQ-5D-5L and two proxy perspectives in an orthopaedic population: A randomized agreement study. Health Qual. Life Outcomes 2021, 19, 35. [Google Scholar] [CrossRef]
- McPhail, S.; Beller, E.; Haines, T. Two perspectives of proxy reporting of health-related quality of life using the Euroqol-5D, an investigation of agreement. Med. Care 2008, 46, 1140–1148. [Google Scholar] [CrossRef]
- Geense, W.W.; van den Boogaard, M.; Peters, M.A.A.; Simons, K.S.; Ewalds, E.; Vermeulen, H.; van der Hoeven, J.G.; Zegers, M. Physical, Mental, and Cognitive Health Status of ICU Survivors Before ICU Admission: A Cohort Study. Crit. Care Med. 2020, 48, 1271–1279. [Google Scholar] [CrossRef]
- Scales, D.C.; Tansey, C.M.; Matte, A.; Herridge, M.S. Difference in reported pre-morbid health-related quality of life between ARDS survivors and their substitute decision makers. Intensive Care Med. 2006, 32, 1826–1831. [Google Scholar] [CrossRef]
- Scholten, A.C.; Haagsma, J.A.; Steyerberg, E.W.; van Beeck, E.F.; Polinder, S. Assessment of pre-injury health-related quality of life: A systematic review. Popul. Health Metr. 2017, 15, 10. [Google Scholar] [CrossRef] [Green Version]
- Dinglas, V.D.; Gifford, J.M.; Husain, N.; Colantuoni, E.; Needham, D.M. Quality of life before intensive care using EQ-5D: Patient versus proxy responses. Crit. Care Med. 2013, 41, 9–14. [Google Scholar] [CrossRef] [Green Version]
- Gifford, J.M.; Husain, N.; Dinglas, V.D.; Colantuoni, E.; Needham, D.M. Baseline quality of life before intensive care: A comparison of patient versus proxy responses. Crit. Care Med. 2010, 38, 855–860. [Google Scholar] [CrossRef] [Green Version]
- Hofhuis, J.; Hautvast, J.L.A.; Schrijvers, A.J.P.; Bakker, J. Quality of life on admission to the intensive care: Can we query the relatives? Intensive Care Med. 2003, 29, 974–979. [Google Scholar] [CrossRef]
- Capuzzo, M.; Grasselli, C.; Carrer, S.; Gritti, G.; Alvisi, R. Quality of life before intensive care admission: Agreement between patient and relative assessment. Intensive Care Med. 2000, 26, 1288–1295. [Google Scholar] [CrossRef]
- Weinfurt, K.P.; Trucco, S.M.; Willke, R.J.; Schulman, K.A. Measuring agreement between patient and proxy responses to multidimensional health-related quality-of-life measures in clinical trials. An application of psychometric profile analysis. J. Clin. Epidemiol. 2002, 55, 608–618. [Google Scholar] [CrossRef]
- Hwang, H.F.; Chen, C.Y.; Lin, M.R. Patient-Proxy Agreement on the Health-Related Quality of Life One Year after Traumatic Brain Injury. Arch. Phys. Med. Rehabil. 2017, 98, 2540–2547. [Google Scholar] [CrossRef]
- Sneeuw, K.C.; Aaronson, N.K.; Sprangers, M.A.; Detmar, S.B.; Wever, L.D.; Schornagel, J.H. Evaluating the quality of life of cancer patients: Assessments by patients, significant others, physicians and nurses. Br. J. Cancer 1999, 81, 87–94. [Google Scholar] [CrossRef] [Green Version]
- Giannoni-Pastor, A.; Eiroa-Orosa, F.J.; Fidel Kinori, S.G.; Arguello, J.M.; Casas, M. Prevalence and Predictors of Posttraumatic Stress Symptomatology among Burn Survivors: A Systematic Review and Meta-Analysis. J. Burn Care Res. 2016, 37, e79–e89. [Google Scholar] [CrossRef]
- Bond, S.; Gourlay, C.; Desjardins, A.; Bodson-Clermont, P.; Boucher, M.E. Anxiety, depression and PTSD-related symptoms in spouses and close relatives of burn survivors: When the supporter needs to be supported. Burns 2017, 43, 592–601. [Google Scholar] [CrossRef]
- Boersma-van Dam, E.; van de Schoot, R.; Geenen, R.; Engelhard, I.M.; Van Loey, N.E. Prevalence and course of posttraumatic stress disorder symptoms in partners of burn survivors. Eur. J. Psychotraumatol. 2021, 12, 1909282. [Google Scholar] [CrossRef]
- American Psychiatric Association. Trauma- and Stressor-Related Disorders. In Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- Samuelson, K.W. Post-traumatic stress disorder and declarative memory functioning: A review. Dialogues Clin. Neurosci. 2011, 13, 346–351. [Google Scholar]
- Haagsma, J.; Bonsel, G.; de Jongh, M.; Polinder, S. Agreement between retrospectively assessed health-related quality of life collected 1 week and 12 months post-injury: An observational follow-up study. Health Qual. Life Outcomes 2019, 17, 70. [Google Scholar] [CrossRef] [Green Version]
- Boersma-van Dam, E.; van de Schoot, R.; Hofland, H.W.C.; Engelhard, I.M.; Van Loey, N.E.E. Individual recovery of health-related quality of life during 18 months post-burn using a retrospective pre-burn measurement: An exploratory study. Qual. Life Res. 2021, 30, 737–749. [Google Scholar] [CrossRef]
- Brooks, R. EuroQol: The current state of play. Health Policy 1996, 37, 53–72. [Google Scholar] [CrossRef]
- Greiner, W.; Weijnen, T.; Nieuwenhuizen, M.; Oppe, S.; Badia, X.; Busschbach, J.; Buxton, M.; Dolan, P.; Kind, P.; Krabbe, P.; et al. A single European currency for EQ-5D health states. Results from a six-country study. Eur. J. Health Econ. 2003, 4, 222–231. [Google Scholar] [CrossRef]
- Synodinou, D.; Savoie-White, F.H.; Sangone, A.; Chang, S.-L.; Beaudoin Cloutier, C.; Bergeron, F.; Guertin, J.R. Health utilities in burn injury survivors: A systematic review. Burns 2022, 48, 13–22. [Google Scholar] [CrossRef]
- Öster, C.; Willebrand, M.; Dyster-Aas, J.; Kildal, M.; Ekselius, L. Validation of the EQ-5D questionnaire in burn injured adults. Burns 2009, 35, 723–732. [Google Scholar] [CrossRef]
- Geraerds, A.; Bonsel, G.J.; Janssen, M.F.; de Jongh, M.A.; Spronk, I.; Polinder, S.; Haagsma, J.A. The added value of the EQ-5D with a cognition dimension in injury patients with and without traumatic brain injury. Qual. Life Res. 2019, 28, 1931–1939. [Google Scholar] [CrossRef] [Green Version]
- Weiss, D.S.; Marmar, C.R. The Impact of Event Scale—Revised. In Assessing Psychological Trauma and PTSD; Wilson, J.P., Keane, T.M., Eds.; Guilford Press: New York, NY, USA, 1997; pp. 399–411. [Google Scholar]
- Creamer, M.; Bell, R.; Failla, S. Psychometric properties of the Impact of Event Scale—Revised. Behav. Res. Ther. 2003, 41, 1489–1496. [Google Scholar] [CrossRef]
- Olde, E.; Kleber, R.; Hart, O.; Pop, V. Childbirth and Posttraumatic Stress Responses: A Validation Study of The Dutch Impact of Event Scale—Revised. Eur. J. Psychol. Assess. 2006, 22, 259–267. [Google Scholar] [CrossRef]
- Janssen, B.; Szende, A. Population Norms for the EQ-5D. In Self-Reported Population Health: An International Perspective based on EQ-5D; Szende, A., Janssen, B., Cabases, J., Eds.; Springer: Dordrecht, The Netherlands, 2014; pp. 19–30. [Google Scholar] [CrossRef] [Green Version]
- Cicchetti, D.V.; Allison, T. A New Procedure for Assessing Reliability of Scoring EEG Sleep Recordings. Am. J. EEG Technol. 1971, 11, 101–110. [Google Scholar] [CrossRef]
- Sim, J.; Wright, C.C. The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef] [Green Version]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Walters, S.J.; Brazier, J.E. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual. Life Res. 2005, 14, 1523–1532. [Google Scholar] [CrossRef]
- Hoehle, L.P.; Phillips, K.M.; Speth, M.M.; Caradonna, D.S.; Gray, S.T.; Sedaghat, A.R. Responsiveness and minimal clinically important difference for the EQ-5D in chronic rhinosinusitis. Rhinology 2019, 57, 110–116. [Google Scholar] [CrossRef]
- Pickard, A.S.; Neary, M.P.; Cella, D. Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual. Life Outcomes 2007, 5, 70. [Google Scholar] [CrossRef] [Green Version]
- Zanini, A.; Aiello, M.; Adamo, D.; Casale, S.; Cherubino, F.; Della Patrona, S.; Raimondi, E.; Zampogna, E.; Chetta, A.; Spanevello, A. Estimation of minimal clinically important difference in EQ-5D visual analog scale score after pulmonary rehabilitation in subjects with COPD. Respir. Care 2015, 60, 88–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Fauerbach, J.A.; Lezotte, D.; Hills, R.A.; Cromes, G.F.; Kowalske, K.; de Lateur, B.J.; Goodwin, C.W.; Blakeney, P.; Herndon, D.N.; Wiechman, S.A.; et al. Burden of burn: A norm-based inquiry into the influence of burn size and distress on recovery of physical and psychosocial function. J. Burn Care Rehabil. 2005, 26, 21–32. [Google Scholar] [CrossRef] [PubMed]
- de Graaf, M.W.; Reininga, I.H.F.; Wendt, K.W.; Heineman, E.; El Moumni, M. Pre-injury health status of injured patients: A prospective comparison with the Dutch population. Qual. Life Res. 2019, 28, 649–662. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, C.E.; Sprangers, M.A.G. Methodological approaches for assessing response shift in longitudinal health-related quality-of-life research. Soc. Sci. Med. 1999, 48, 1531–1548. [Google Scholar] [CrossRef]
- Haagsma, J.A.; Spronk, I.; de Jongh, M.A.C.; Bonsel, G.J.; Polinder, S. Conventional and retrospective change in health-related quality of life of trauma patients: An explorative observational follow-up study. Health Qual. Life Outcomes 2020, 18, 157. [Google Scholar] [CrossRef]
- Wideman, T.H.; Edwards, R.R.; Walton, D.M.; Martel, M.O.; Hudon, A.; Seminowicz, D.A. The Multimodal Assessment Model of Pain: A Novel Framework for Further Integrating the Subjective Pain Experience Within Research and Practice. Clin. J. Pain 2019, 35, 212–221. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).