Subischial vs. Ischial Containment Sockets: A Multicenter Randomized Crossover Trial to Assess Comfort and Mobility in Daily Life Situations
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
- -
- Were ≥18 years;
- -
- Had a unilateral or bilateral AKA;
- -
- Were equipped with a definitive IC socket;
- -
- Used a liner regardless of the suspension system;
- -
- Had a residual limb length ≥ 16 cm from the perineum to the limb extremity when wearing the liner;
- -
- Were able to don their prosthesis in a standing position;
- -
- Were able to walk (from d4600 to d4608, according to the International Classification of Functioning, Disability and Health—ICF, equivalent to K1–K4).
- -
- Were a protected person;
- -
- Were a pregnant or breast-feeding woman;
- -
- Had a silicone allergy;
- -
- Had a residual limb that was not stable in volume or infected;
- -
- Had any pathology affecting the sensations or the capacity to don the prosthesis.
2.2. Experimental Design
2.3. Intervention
2.4. Procedure
2.5. Outcome Measures
2.6. Sample Size Determination
2.7. Data Analysis
3. Results
3.1. Comfort
- -
- Sitting on a rigid chair: +3.2(2.3) (p < 0.001; d = 1.38);
- -
- Sitting in a car: +3.1(2.7) (p = 0.001; d = 1.13);
- -
- Standing: +1.5(2.7) (p = 0.027; d = 0.57);
- -
- Walking: +1.2(3.1) (p = 0.212; d = 0.38).
3.2. Mobility
3.3. Adverse Events
3.4. Preference
4. Discussion
4.1. Study Limitations
4.2. Longer-Term Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 2MWT | Two Minute Walk Test |
| IC | Ischial containment |
| I-SUB | Subischial |
| MDC | Minimum detectable change at 90% confidence level |
| NU-FlexSIS | Northwestern University Flexible Subischial Suction socket |
| NU-FlexSIV | Northwestern University Flexible Subischial Vacuum Socket |
| PLUS-M | Prosthetic Limb Users Survey of Mobility |
| PMR | Physical medicine and rehabilitation |
| RL | Residual limb |
| SCS | Socket Score Comfort |
| VAS | Vacuum-assisted suspension |
References
- ATIH Data for 2022. Available online: https://www.atih.sante.fr/ (accessed on 8 August 2024).
- Sanders, J.E.; Daly, C.H. Normal and shear stresses on a residual limb in a prosthetic socket during ambulation: Comparison of finite element results with experimental measurements. J. Rehabil. Res. Dev. 1993, 30, 191–204. [Google Scholar]
- Bauman, A.; Ainsworth, B.; Sallis, J.; Hagströmer, M.; Craig, C.; Bull, F.; Pratt, M.; Venugopal, K.; Chau, J.; Sjöström, M.; et al. The Descriptive Epidemiology of Sitting: A 20-Country Comparison Using the International Physical Activity Questionnaire (IPAQ). Am. J. Prev. Med. 2011, 41, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Jans, M.; Proper, K.; Hildebrandt, V. Sedentary Behavior in Dutch Workers: Differences Between Occupations and Business Sectors. Am. J. Prev. Med. 2007, 33, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, K.; Zügner, R.; Thomsen, P.; Tranberg, R. Daily Activity of Individuals with an Amputation Above the Knee as Recorded from the Nonamputated Limb and the Prosthetic Limb. J. Meas. Phys. Behav. 2023, 6, 223–232. [Google Scholar] [CrossRef]
- Sabolich, J. Contoured adduction trochanteric-controlled alignment method (CAT-CAM). Clin. Prosthet. Orthot. 1985, 9, 15–26. [Google Scholar]
- Hoyt, C.; Littig, D.; Lundt, J.; Staats, T. The UCLA CAT-CAM Above-Knee Socket, 3rd ed.; UCLA Prosthetics Education and Research Program: Los Angeles, CA, USA, 1987. [Google Scholar]
- Pritham, C.H. Biomechanics and shape of the above-knee socket considered in light of the ischial containment concept. Prosthet. Orthot. Int. 1990, 14, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Klotz, R.; Colobert, B.; Botino, M.; Permentiers, I. Influence of different types of sockets on the range of motion of the hip joint by the transfemoral amputee. Ann. Phys. Rehabil. Med. 2011, 54, 399–410. [Google Scholar] [CrossRef]
- Mohd Hawari, N.; Jawaid, M.; Md Tahir, P.; Azmeer, R.A. Case study: Survey of patient satisfaction with prosthesis quality and design among below-knee prosthetic leg socket users. Disabil. Rehabil. Assist. Technol. 2017, 12, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Fidler, V.; Eisma, W.H. Walking speed of normal subjects and amputees: Aspects of validity of gait analysis. Prosthet. Orthot. Int. 1993, 17, 78–82. [Google Scholar] [CrossRef]
- Dillingham, T.; Pezzin, L.; MacKenzie, E. Limb amputations and limb deficiencies: Epidemiology and recent trends in the United States. South. Med. J. 2001, 95, 875–883. [Google Scholar] [CrossRef]
- Fairley, M. M.A.S. Socket: A Transfemoral Revolution. O P Edge. 2004. Available online: https://opedge.com/m-a-s-socket-a-transfemoral-revolution/ (accessed on 8 August 2024).
- Fatone, S.; Caldwell, R. Northwestern University Flexible Subischial Vacuum Socket for persons with transfemoral amputation: Part 1 description of technique. Prosthet. Orthot. Int. 2017, 41, 237–245. [Google Scholar] [CrossRef]
- Fatone, S.; Johnson, W.; Tran, L.; Tucker, K.; Mowrer, C.; Caldwell, R. Quantification of rectifications for Northwestern University Flexible Sub-Ischial Vacuum (NU-FlexSIV) Socket. Prosthet. Orthot. Int. 2017, 41, 251–257. [Google Scholar] [CrossRef]
- Fatone, S.; Caldwell, R.; Angelico, J.; Stine, R.; Kim, K.Y.; Gard, S.; Oros, M. Comparison of Ischial Containment and Subischial Sockets on Comfort, Function, Quality of Life, and Satisfaction with Device in Persons with Unilateral Transfemoral Amputation: A Randomized Crossover Trial. Arch. Phys. Med. Rehabil. 2021, 102, 2063–2073.e2. [Google Scholar] [CrossRef]
- Brown, S.; Russell Esposito, E.; Ikeda, A.; Wilken, J.; Fatone, S. Evaluation of NU-FlexSIV Socket performance for military service members with transfemoral amputation. US Army Med. Dep. J. 2018, 2–18, 38–47. [Google Scholar]
- Caldwell, R.; Fatone, S. Technique modifications for a suction suspension version of the Northwestern University Flexible Sub-Ischial Vacuum socket: The Northwestern University Flexible Sub-Ischial Suction socket. Prosthet. Orthot. Int. 2019, 43, 233–239. [Google Scholar] [CrossRef]
- Hanspal, R.; Fisher, K.; Nieveen, R. Prosthetic socket fit comfort score. Disabil. Rehabil. 2003, 25, 1278–1280. [Google Scholar] [CrossRef]
- Hafner, J.B.; Morgan, J.S.; Askew, R.; Salem, R. Psychometric evaluation of self- report outcome measures for prosthetic applications. J. Rehab. Res. Dev. 2016, 53, 797–812. [Google Scholar] [CrossRef] [PubMed]
- Reeve, B.; Hays, R.; Bjorner, J.; Cook, K.; Crane, P.; Teresi, J.; Thissen, D.; Revicki, D.; Weiss, D.; Hambleton, R.; et al. Psychometric Evaluation and Calibration of Health-Related Quality of Life Item Banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med. Care 2007, 45, S22–S31. [Google Scholar] [CrossRef] [PubMed]
- Morgan, S.J.; Amtmann, D.; Abrahamson, D.C.; Kajlich, A.J.; Hafner, B.J. Use of cognitive interviews in the development of the PLUS-M item bank. Qual. Life Res. 2014, 23, 1767–1775. [Google Scholar] [CrossRef] [PubMed]
- Karatzios, C.; Loiret, I.; Luthi, F.; Leger, B.; Le Carre, J.; Saubade, M.; Muff, G.; Benaim, C. Transcultural adaptation and validation of a French version of the Prosthetic Limb Users Survey of Mobility 12-item Short-Form (PLUS-M/FC-12) in active amputees. Ann. Phys. Rehabil. Med. 2019, 62, 142–148. [Google Scholar] [CrossRef]
- Prosthetic Limb Users Survey of Mobility (PLUS-M™) Version 1.2 Short Forms Users Guide. 16 September 2022. Available online: http://www.plus-m.org (accessed on 8 August 2024).
- Miller, M.; Cook, P.; Kline, P.; Anderson, C.; Stevens-Lapsley, J.; Christiansen, C. Physical Function and Pre-Amputation Characteristics Explain Daily Step Count after Dysvascular Amputation. PMR 2019, 11, 1050–1058. [Google Scholar] [CrossRef]
- Gaunaurd, I.; Kristal, A.; Horn, A.; Krueger, C.; Muro, O.; Rosenberg, A.; Gruben, K.; Kirk-Sanchez, N.; Pasquina, P.; Gailey, R. The Utility of the 2-Minute Walk Test as a Measure of Mobility in People with Lower Limb Amputation. Arch. Phys. Med. Rehabil. 2020, 101, 1183–1189. [Google Scholar] [CrossRef]
- Resnik, L.; Borgia, M. Reliability of outcome measures for people with lower-limb amputations: Distinguishing true change from statistical error. Phys. Ther. 2011, 91, 555–565. [Google Scholar] [CrossRef] [PubMed]
- Maikos, J.T.; Chomack, J.M.; Loan, J.P.; Bradley, K.M.; D’Andrea, S.E. Effects of Prosthetic Socket Design on Residual Femur Motion Using Dynamic Stereo X-Ray-A Preliminary Analysis. Front. Bioeng. Biotechnol. 2021, 10, 697651. [Google Scholar] [CrossRef]
- Kahle, J.T.; Miro, R.M.; Ho, L.T.; Porter, M.R.; Lura, D.J.; Carey, S.L.; Lunseth, P.; Swanson, A.E.; Highsmith, M.J. Effect of transfemoral prosthetic socket interface design on gait, balance, mobility, and preference: A randomized clinical trial. Prosthet. Orthot. Int. 2021, 45, 304–312. [Google Scholar] [CrossRef]
- Kahle, J.; Miro, R.M.; Ho, L.T.; Porter, M.; Lura, D.J.; Carey, S.L.; Lunseth, P.; Highsmith, J.; Highsmith, M.J. The effect of the transfemoral prosthetic socket interface designs on skeletal motion and socket comfort: A randomized clinical trial. Prosthet. Orthot. Int. 2020, 44, 145–154. [Google Scholar] [CrossRef]
- Dillingham, T.R.; Kenia, J.L.; Shofer, F.S.; Marschalek, J.S. A Prospective Assessment of an Adjustable, Immediate Fit, Subischial Transfemoral Prosthesis. Arch. Rehabil. Res. Clin. Transl. Dev. 2022, 4, 100200. [Google Scholar] [CrossRef] [PubMed]
- Kahle, J.T.; Highsmith, M.J. Transfemoral sockets with vacuum-assisted suspension comparison of hip kinematics, socket position, contact pressure, and preference: Ischial containment versus brimless. J. Rehabil. Res. 2013, 50, 1241–1252. [Google Scholar] [CrossRef]
- Miro, R.; Hanson, A.; Randolph, B.; Highsmith, J. Prosthetic, functional, and clinical outcomes among female amputees with limb loss: A systematic review of the literature. Technol. Innov. 2025, 24, 67–81. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Fatone, S.; Dillon, M.; Stine, R.; Tillges, R. Coronal plane socket stability during gait in persons with unilateral transfemoral amputation: Pilot study. J. Rehabil. Res. Dev. 2014, 51, 1217–1228. [Google Scholar] [CrossRef] [PubMed]
- Fatone, S.; Yohay, J.; Caldwell, R. Change in residual limb size over time in the NU-FlexSIV Socket: A case study. Prosthet. Orthot. Int. 2018, 42, 620–625. [Google Scholar] [CrossRef] [PubMed]

 Randomization
Randomization  Assessment.
Assessment.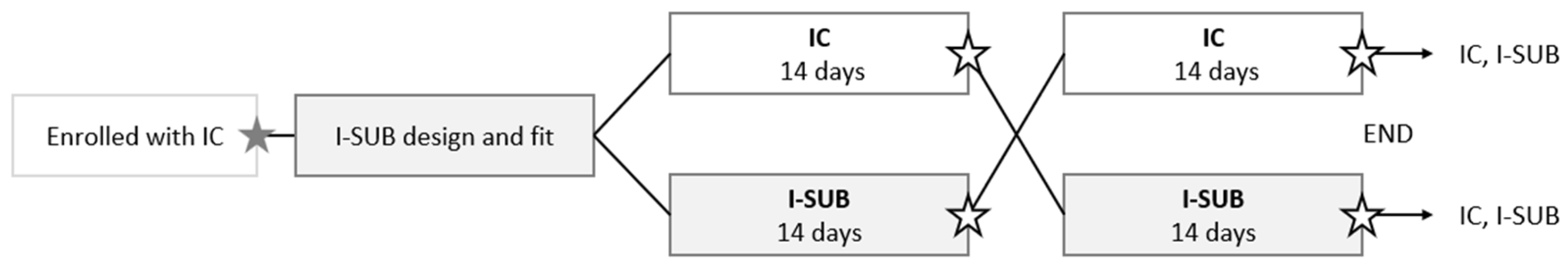


| Subject Number | Gender | Height (m) | Mass (kg) | Age (Years) | Time Since Amputation (Years) | Etiology | RL Side (Left/Right) | Activity Level (ICF) |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 1.85 | 75 | 64 | 6 | Trauma | L | d4602 |
| 2 | M | 1.70 | 81 | 62 | 3 | Vascular | R | d4602 |
| 3 | M | 1.76 | 75 | 41 | 24 | Trauma | L | d4608 |
| 4 | M | 1.73 | 80 | 72 | 1.5 | Vascular | L | d4602 |
| 5 | M | 1.82 | 105 | 47 | 4 | Trauma | L AK/R BK | d4608 |
| 6 | M | 1.79 | 78 | 78 | 14 | Trauma | L | d4608 |
| 7 | F | 1.65 | 50 | 63 | 2 | Trauma | L | d4608 |
| 8 | M | 1.80 | 63 | 60 | 31 | Trauma | R | d4601 |
| 9 | M | 1.85 | 107 | 49 | 25 | Trauma | R | d4602 |
| 10 | M | 1.82 | 82 | 47 | 29 | Trauma | L | d4608 |
| 11 | M | 1.76 | 79 | 75 | 10 | Infection | L | d4602 |
| 12 | M | 1.85 | 80 | 32 | 6 | Trauma | R | d4602 |
| 13 | M | 1.63 | 62 | 36 | 4 | Cancer | d4602 | |
| 14 | M | 1.80 | 65 | 69 | 4 | Vascular | R | d4602 |
| 15 | M | 1.76 | 70 | 71 | 49 | Trauma | L | d4608 |
| 16 | M | 1.73 | 89 | 71 | 6.5 | Vascular | R | d4601 |
| 17 | M | 1.75 | 85 | 71 | 4 | Vascular | L | d4600 |
| 18 | M | 1.77 | 98 | 63 | 2 | Infection | L | d4608 |
| 19 | M | 1.80 | 105 | 73 | 14 | Vascular | R | d4602 |
| 20 | M | 1.69 | 78 | 78 | 57 | Trauma | R | d4608 |
| 21 | F | 1.50 | 48 | 68 | 13 | Trauma | L | d4608 |
| 22 | F | 1.75 | 67 | 34 | 2 | Cancer | R | d4608 |
| 23 | M | 1.76 | 95 | 58 | 41 | Trauma | R | d4602 |
| Socket Comfort Score | Main Effect | Estimate | SE | F-Value | p-Value |
|---|---|---|---|---|---|
| General | Socket | −1.75 | 0.63 | 7.72 | 0.008 |
| Order | 0.71 | 0.64 | 1.22 | 0.275 | |
| Socket × Order | −0.07 | 0.91 | 0.01 | 0.941 | |
| Sitting on a rigid chair | Socket | −3.25 | 0.59 | 30.8 | <0.001 |
| Order | 0.65 | 0.60 | 1.2 | 0.283 | |
| Socket × Order | 0.07 | 0.85 | 0.01 | 0.936 | |
| Standing | Socket | −1.67 | 0.73 | 5.26 | 0.027 |
| Order | 0.39 | 0.74 | 0.28 | 0.599 | |
| Socket × Order | 0.21 | 1.05 | 0.04 | 0.841 | |
| Walking | Socket | −1.00 | 0.79 | 1.61 | 0.212 |
| Order | 0.60 | 0.81 | 0.55 | 0.462 | |
| Socket × Order | −0.45 | 1.14 | 0.16 | 0.692 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Loiret, I.; Duraffourg, C.; Permentiers, I.; Barbazanges, P.; Bokobza, G.; Da Costa, M.; Elie, E.; Fons, N.; Popineau, C.; Rey, S.; et al. Subischial vs. Ischial Containment Sockets: A Multicenter Randomized Crossover Trial to Assess Comfort and Mobility in Daily Life Situations. Prosthesis 2026, 8, 5. https://doi.org/10.3390/prosthesis8010005
Loiret I, Duraffourg C, Permentiers I, Barbazanges P, Bokobza G, Da Costa M, Elie E, Fons N, Popineau C, Rey S, et al. Subischial vs. Ischial Containment Sockets: A Multicenter Randomized Crossover Trial to Assess Comfort and Mobility in Daily Life Situations. Prosthesis. 2026; 8(1):5. https://doi.org/10.3390/prosthesis8010005
Chicago/Turabian StyleLoiret, Isabelle, Clément Duraffourg, Iris Permentiers, Pascal Barbazanges, Guillaume Bokobza, Marta Da Costa, Estelle Elie, Nicolas Fons, Christophe Popineau, Sandrine Rey, and et al. 2026. "Subischial vs. Ischial Containment Sockets: A Multicenter Randomized Crossover Trial to Assess Comfort and Mobility in Daily Life Situations" Prosthesis 8, no. 1: 5. https://doi.org/10.3390/prosthesis8010005
APA StyleLoiret, I., Duraffourg, C., Permentiers, I., Barbazanges, P., Bokobza, G., Da Costa, M., Elie, E., Fons, N., Popineau, C., Rey, S., Roche, G., Ronzi, Y., Thomas-Pohl, M., Klotz, R., & Calistri, L. (2026). Subischial vs. Ischial Containment Sockets: A Multicenter Randomized Crossover Trial to Assess Comfort and Mobility in Daily Life Situations. Prosthesis, 8(1), 5. https://doi.org/10.3390/prosthesis8010005






