The Use of the Flexible Thermoplastic Nylon-Based Dental Prostheses: A Literature Review
Abstract
1. Introduction
- Superior esthetics: its translucent nature allows seamless integration with oral tissues, enhancing the overall appearance of the prosthesis [16].
- Enhanced comfort: the material conforms naturally to oral tissue movements during mastication, reducing discomfort and irritation.
- Absence of allergenic metals and monomers [20].
- Minimally invasive: Valplast® (Valplast, USA) does not require extensive tooth preparation, preserving natural dental structures.
- Reduced stability and retention compared to conventional cast metal frameworks [24].
- Hygiene challenges, for patients with poor oral care, as the material’s flexibility may promote plaque accumulation in hard-to-clean areas.
- Increased bacterial and fungal plaque accumulation compared to acrylic materials, attributed to its higher surface roughness [27].
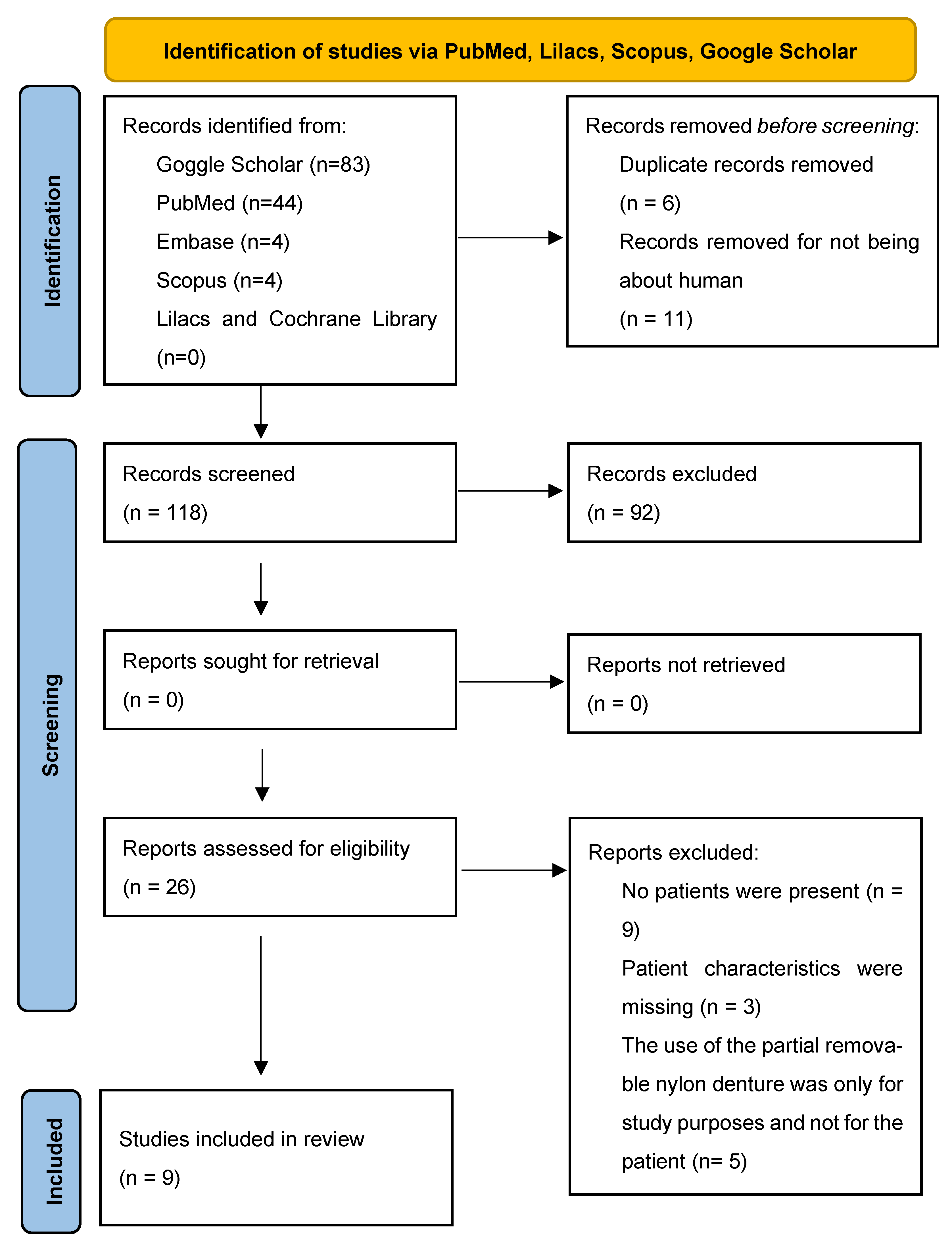
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
- Human subjects.
- Patients rehabilitated with a removable partial denture made of nylon.
- Patients who underwent oral surgical extraction procedures prior to prosthetic rehabilitation.
- Published papers in English language.
- Non-human subjects.
- Patients who did not undergo surgical intervention.
- Patients who were not rehabilitated with any form of prosthesis.
- Patients rehabilitated with materials other than nylon-based removable partial dentures.
2.3. Search Terms
- -
- “Valplast”, “nylon denture”, “polyamide denture”, “nylon prosthesis”, “polyamide prosthesis” to identify studies focused on nylon-based removable partial dentures.
- -
- “post-surgical” “surgery” to identify prosthetic rehabilitations following surgical procedures.
- -
- “male”, “female” to filter studies involving specific patient demographics.
2.4. Screening and Data Extraction Process
2.5. Quality Assessment
3. Results
3.1. Characteristics of the Identified Subject
3.2. Characteristics of Patients’ Edentulism
3.3. Rehabilitation of the Patients’ Edentulism
3.4. The Reasons for the Choice
3.5. The Follow-Up
4. Discussion
4.1. Clinical Indications and Patient Considerations
4.2. Functional and Esthetic Outcomes
4.3. Evaluation of the Reason for Prosthetic Choice
4.4. Follow-Up and Outcome Stability
4.5. Evaluation of the BIAS
4.6. Limitations of the Review
4.7. Implications for Clinical Practice and Research
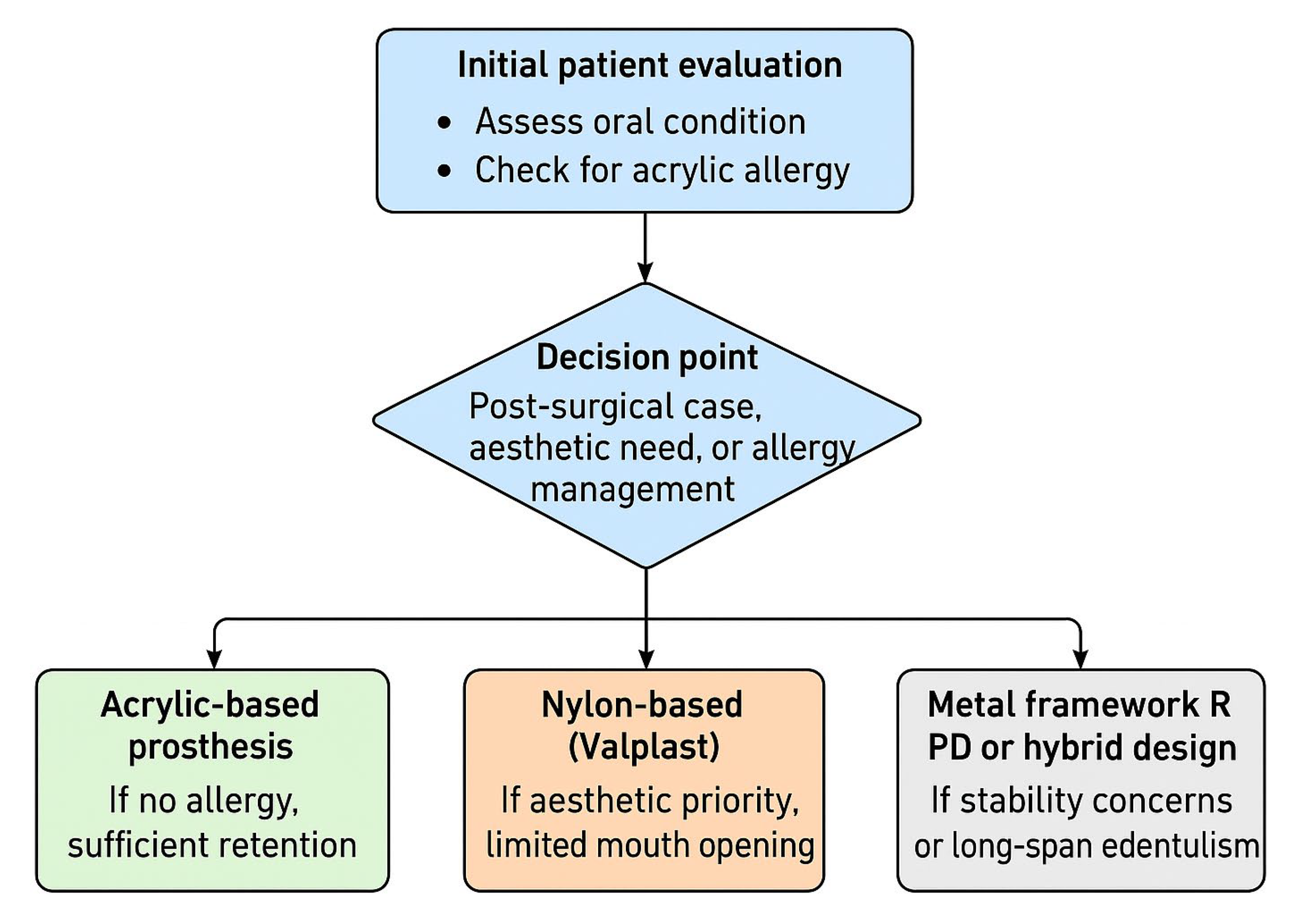
4.8. Clinical Decision-Making Algorithm for the Indication of Nylon-Based Removable Partial Dentures
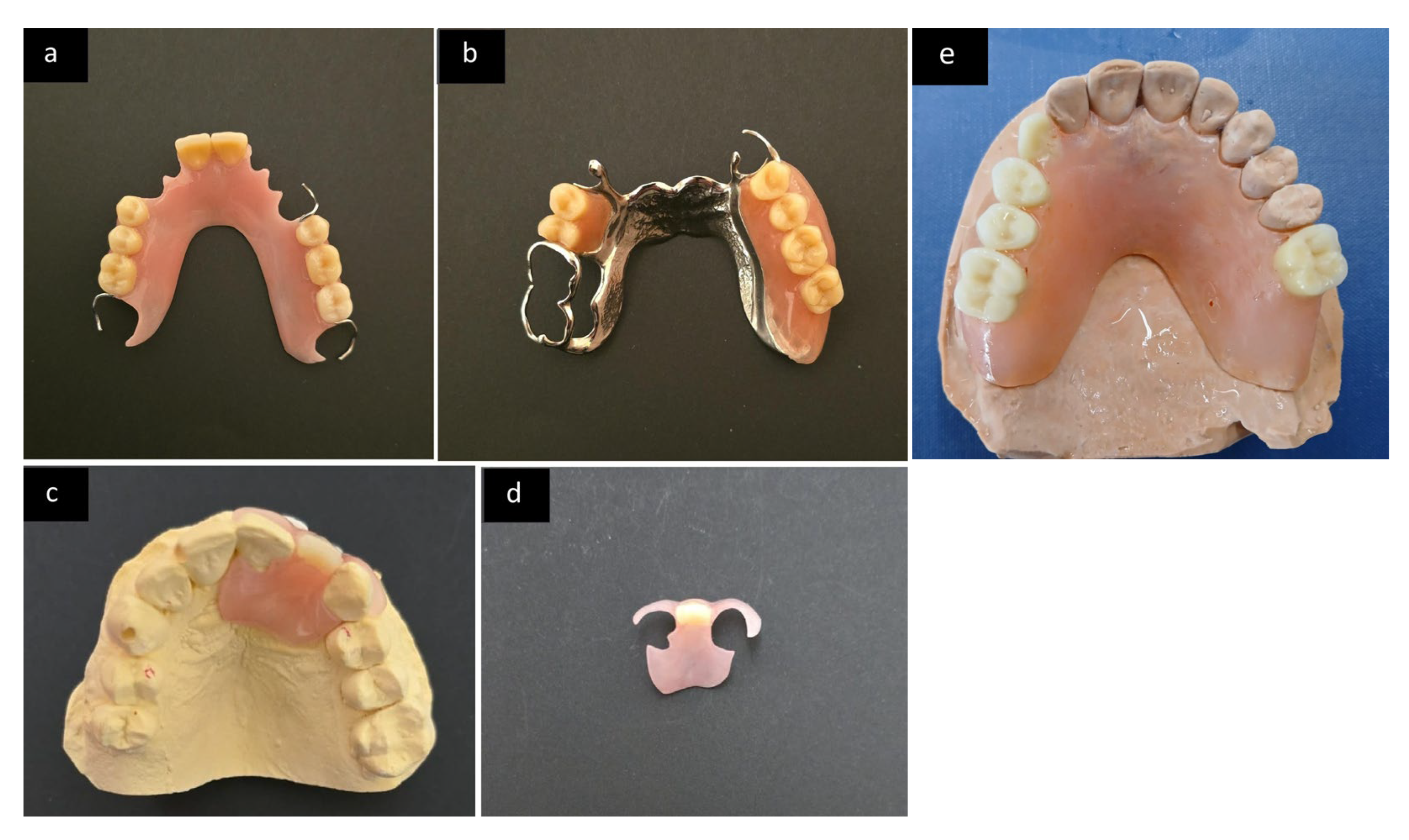
- Acrylic-based prostheses (Figure 3a) remain the gold standard when no allergy is present, and sufficient retention can be achieved.
- Metal framework or hybrid RPDs (Figure 3b) are indicated in long-span edentulism or cases where mechanical stability and repairability are priorities.
- Nylon-based (Valplast, Figure 3c,d) solutions are most suitable for patients with limited mouth opening, high esthetic expectations, or a history suggestive of acrylic hypersensitivity. However, evidence supporting their superiority is limited by the methodological weaknesses highlighted in this review.
4.9. Limitations of the Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zarb, G.A.; Hobkirk, J.; Eckert, S.; Jacob, R. Prosthodontic Treatment for Edentulous Patients: Complete Dentures and Implant-Supported Prostheses, 13th ed.; Elsevier Mosby: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Fueki, K.; Ohkubo, C.; Yatabe, M.; Arakawa, I.; Arita, M.; Ino, S.; Kanamori, T.; Kawai, Y.; Kawara, M.; Komiyama, O.; et al. Clinical application of removable partial dentures using thermoplastic resin-part I: Definition and indication of non-metal clasp dentures. J. Prosthodont. Res. 2014, 58, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Chuchulska, B.; Yankov, S.; Hristov, I.; Aleksandrov, S. Thermoplastic Materials in the Dental Practice: A Review. Int. J. Sci. Res. 2017, 6, 1074–1076. [Google Scholar] [CrossRef]
- Forkel, S.; Schubert, S.; Corvin, L.; Heine, G.; Lang, C.C.V.; Oppel, E.; Pföhler, C.; Treudler, R.; Bauer, A.; Sulk, M.; et al. Contact allergies to dental materials in patients. Br. J. Dermatol. 2024, 190, 895–903. [Google Scholar] [CrossRef]
- Abdelhamid, A.; Ashour, M.; Abdelrahman, A. Evaluation of a Newly Formulated Thermoplastic Monomer Free Complete Denture Base Material (Microbiological Study). Int. J. Sci. Res. 2016, 5, 656–662. [Google Scholar]
- Bishop, S.; Roberts, H. Methacrylate perspective in current dental practice. J. Esthet. Restor. Dent. Off. Publ. Am. Acad. Esthet. Dent. 2020, 32, 673–680. [Google Scholar] [CrossRef]
- Tanoue, N.; Nagano, K.; Matsumura, H. Use of a light-polymerized composite removable partial denture base for a patient hypersensitive to poly(methyl methacrylate), polysulfone, and polycarbonate: A clinical report. J. Prosthet. Dent. 2005, 93, 17–20. [Google Scholar] [CrossRef]
- Fletcher, R.; Harrison, W.; Crighton, A. Dental material allergies and oral soft tissue reactions. Br. Dent. J. 2022, 232, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Vojdani, M.; Giti, R. Polyamide as a Denture Base Material: A Literature Review. J. Dent. 2015, 16, 1–9. [Google Scholar]
- Kumar, B.S.P.; Pacharne, A.P.; Sadafule, N.; Singh, K. Flexible denture base material: A viable alternative for conventional denture base material. Int. J. Health Sci. 2022, 6, 11096–11105. [Google Scholar] [CrossRef]
- Scheman, A.; Jacob, S.; Zirwas, M.; Warshaw, E.; Nedorost, S.; Katta, R.; Cook, J.; Castanedo-Tardan, M.P. Contact Allergy: Alternatives for the 2007 North American contact dermatitis group (NACDG) Standard Screening Tray. Dis. Mon. 2008, 54, 7–156. [Google Scholar] [CrossRef]
- Gligorijević, N.R.; Igić, M.A.; Kostić, M.M.; Pejčić, A.S. Properties and applications of dental polyamides. Acta Stomatol. Naissi 2020, 36, 2098–2105. [Google Scholar] [CrossRef]
- Singh, R.; Chawla, P.S.; Shaw, E.; Av, R.; Mehrotra, A.; Pandey, V. Comparison of Flexural Strength and Surface Roughness of two Different Flexible and Heat Cure Denture Base Material: An in Vitro Study. J. Contemp. Dent. Pract. 2018, 19, 1214–1220. [Google Scholar] [CrossRef]
- Manzon, L.; Fratto, G.; Poli, O.; Infusino, E. Patient and Clinical Evaluation of Traditional Metal and Polyamide Removable Partial Dentures in an Elderly Cohort. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2019, 28, 868–875. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Shashidhara, H.S. A review: Flexible removable partial dentures. J. Dent. Med. Scien. 2014, 13, 58–62. [Google Scholar] [CrossRef]
- Singh, J.P.; Dhiman, R.K.; Bedi, R.P.; Girish, S.H. Flexible denture base material: A viable alternative to conventional acrylic denture base material. Contemp. Clin. Dent. 2011, 2, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Soygun, K.; Bolayir, G.; Boztug, A. Mechanical and thermal properties of polyamide versus reinforced PMMA denture base materials. J. Adv. Prosthodont. 2013, 5, 153–160. [Google Scholar] [CrossRef]
- Namritha, N. Comparative Evaluation of the Mechanical Properties of Three Commercially Available Flexible Denture Base Materials—An In Vitro Study. Master’s Thesis, Rajiv Gandhi University of Health Sciences, Bangalore, India, 2018. Order No. 30584224 dissertation. Available online: https://www.proquest.com/dissertations-theses/comparative-evaluation-mechanical-properties/docview/2866351931/se-2 (accessed on 15 November 2025).
- Abhay, P.N.; Karishma, S. Comparative evaluation of impact and flexural strength of four commercially available flexible denture base materials: An in vitro study. J. Indian Prosthodont. Soc. 2013, 13, 499–508. [Google Scholar] [CrossRef]
- Nguyen, L.G.; Kopperud, H.M.; Øilo, M. Water sorption and solubility of polyamide denture base materials. Acta Biomater. Odontol. Scand. 2017, 3, 47–52. [Google Scholar] [CrossRef]
- Ucar, Y.; Akova, T.; Aysan, I. Mechanical properties of polyamide versus different PMMA denture base materials. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2012, 21, 173–176. [Google Scholar] [CrossRef]
- Sun, Y.; Song, S.Y.; Lee, K.S.; Park, J.H.; Ryu, J.J.; Lee, J.Y. Effects of relining materials on the flexural strength of relined thermoplastic denture base resins. J. Adv. Prosthodont. 2018, 10, 361–366. [Google Scholar] [CrossRef]
- Hamanaka, I.; Shimizu, H.; Takahashi, Y. Bond strength of a chairside autopolymerizing reline resin to injection-molded thermoplastic denture base resins. J. Prosthodont. Res. 2017, 61, 67–72. [Google Scholar] [CrossRef]
- Vozza, I.; Manzon, L.; Passarelli, P.C.; Pranno, N.; Poli, O.; Grippaudo, C. The Effects of Wearing a Removable-Partial-Denture on the Bite Forces: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 11401. [Google Scholar] [CrossRef]
- Shah, V.R.; Shah, D.N.; Chauhan, C.J.; Doshi, P.J.; Kumar, A. Evaluation of flexural strength and color stability of different denture base materials including flexible material after using different denture cleansers. J. Indian Prosthodont. Soc. 2015, 15, 367–373. [Google Scholar] [CrossRef]
- Wieckiewicz, M.; Opitz, V.; Richter, G.; Boening, K.W. Physical properties of polyamide-12 versus PMMA denture base material. BioMed Res. Int. 2014, 2014, 150298. [Google Scholar] [CrossRef] [PubMed]
- Sultana, N.; Ahmed, S.; Nandini, V.V.; Lathief, J.; Boruah, S. An In Vitro Comparison of Microbial Adhesion on Three Different Denture Base Materials and Its Relation to Surface Roughness. Cureus 2023, 15, e37085. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Systematic reviews of etiology and risk (2020). In JBI Manual for Evidence Synthesis; Aromataris, E., Lockwood, C., Porritt, K., Pilla, B., Jordan, Z., Eds.; JBI: Adelaide, Australia, 2024; Available online: https://synthesismanual.jbi.global (accessed on 15 November 2025).
- Papi, D.; Rosella, R.; Giardino, S.; Di Carlo, S.; Piccoli, L.; Cascone, P.; Pompa, G. Prosthetic rehabilitation with partial removable and aesthetic dentures (Valplast®) in a patient with recurrent right TMJ ankylosis: A case report. In Proceedings of the XXIII Congresso Nazionale Collegio dei Docenti Universitari di Discipline Odontostomatologiche, Roma, Italy, 14–16 April 2016; Volume 65, pp. 245–246. [Google Scholar]
- Yaala, M.; Mabrouk-Aguir, Y.; Bounaouara, R.; Rzigui, S. La prothèse flexible dans tous ses aspects the flexible prosthesis in all aspects. Afr. J. Dent. Implantol. 2024. Available online: https://www.researchgate.net/publication/384434571_LA_PROTHESE_FLEXIBLE_DANS_TOUS_SES_ASPECTS_THE_FLEXIBLE_PROSTHESIS_IN_ALL_ASPECTS (accessed on 15 November 2025).
- Spintzyk, S.; Schmunk, R.; Kraemer Fernandez, P.; Huettig, F.; Unkovskiy, A. 3D Printing of Polyamide to Fabricate a Non-Metal Clasp Removable Partial Denture via Fused Filament Fabrication: A Case Report. Int. J. Environ. Res. Public Health 2021, 18, 8241. [Google Scholar] [CrossRef]
- Mounika, K.L.; Rao, H.K.; Kumar, M.M.; Kishore, K.K.; Babu, M.S.; Deepika, M. Pliable Dentures—An Alternate Denture Base Material- Case Reports. J. Adv. Med. Dent. Sci. Res. 2021, 9, 43–46. [Google Scholar] [CrossRef]
- Ahuja, S.; Jain, V.; Wicks, R.; Hollis, W. Restoration of a partially edentulous patient with combination partial dentures. Br. Dent. J. 2019, 226, 407–410. [Google Scholar] [CrossRef]
- Kavaja, L.; Nushi, V. Temporary prosthetics rehabilitation in adolescents patient. Int. J. Oral Sci. Dent. Med. 2018, 169. [Google Scholar]
- Belal, A.; Monther, B.; Alzarif, W. Possibility of Using Flexible Dentures over Iliac Bone Graft in Adolescent Patients with Ameloblastoma: A 9-Month Follow-up Clinical Report. Case Rep. Dent. 2021, 2021, 2415707. [Google Scholar] [CrossRef]
- Gandhimathi, J.; Krishnameera, N.; Sriramaprabu, G.; Vinayagavel, K.; Sabarigirinathan, C.; Rupkumar, P.; Sivasakthikumar, S.; Srividya, S.; Sangeethameena, N. A Systematic Approach for Functional Rehabilitation of Hemimandibulectomy Patient. Int. J. Oral. Health Med. Res. 2015, 2, 60–62. [Google Scholar]
- Kwon, I.J.; Eo, M.Y.; Park, S.J.; Kim, S.M.; Lee, J.H. Newly designed retentive posts of mandibular reconstruction plate in oral cancer patients based on preliminary FEM study. World J. Surg. Oncol. 2016, 14, 292. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Aeran, H.; Kumar, N.; Gupta, N. Flexible thermoplastic denture base materials for aesthetical removable partial denture framework. J. Clin. Diagn. Res. 2013, 7, 2372–2373. [Google Scholar] [CrossRef]
- Samet, N.; Tau, S.; Findler, M.; Susarla, S.M.; Findler, M. Flexible, removable partial denture for a patient with systemic sclerosis (scleroderma) and microstomia: A clinical report and a three-year follow-up. Gen. Dent. 2007, 55, 548–551. [Google Scholar]
- Hundal, M.; Madan, R. Comparative clinical evaluation of removable partial dentures made of two different materials in Kennedy Applegate class II partially edentulous situation. Med. J. Armed Forces India 2015, 71, S306–S312. [Google Scholar] [CrossRef] [PubMed]
- Jain, N.; Naitam, D.; Wadkar, A.; Nemane, A.; Katoch, S.; Dewangan, A. Prosthodontic rehabilitation of hereditary ectodermal dysplasia in an 11-year-old patient with flexible denture: A case report. Case Rep. Dent. 2012, 2012, 489769. [Google Scholar] [CrossRef]
- Taguchi, Y.; Shimamura, I.; Sakurai, K. Effect of buccal part designs of polyamide resin partial removable dental prosthesis on retentive force. J. Prosthodont. Res. 2011, 55, 44–47. [Google Scholar] [CrossRef]
- Ito, M.; Wee, A.G.; Miyamoto, T.; Kawai, Y. The combination of a nylon and traditional partial removable dental prosthesis for improved esthetics: A clinical report. J. Prosthet. Dent. 2013, 109, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Le Bars, P.; Kouadio, A.A.; Amouriq, Y.; Bodic, F.; Blery, P.; Bandiaky, O.N. Different Polymers for the Base of Removable Dentures? Part II: A Narrative Review of the Dynamics of Microbial Plaque Formation on Dentures. Polymers 2023, 16, 40. [Google Scholar] [CrossRef]
- Meirowitz, A.; Rahmanov, A.; Shlomo, E.; Zelikman, H.; Dolev, E.; Sterer, N. Effect of Denture Base Fabrication Technique on Candida albicans Adhesion In Vitro. Materials 2021, 14, 221. [Google Scholar] [CrossRef] [PubMed]
- Hamanaka, I.; Iwamoto, M.; Lassila, L.V.J.; Vallittu, P.K.; Takahashi, Y. Wear resistance of injection-molded thermoplastic denture base resins. Acta Biomater. Odontol. Scand. 2016, 2, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Hamanaka, I.; Shimizu, H.; Takahashi, Y. Shear bond strength of an autopolymerizing repair resin to injection-molded thermoplastic denture base resins. Acta Odontol. Scand. 2013, 71, 1250–1254. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Title | Type of Study | No of Patients | Age | Sex | Kennedy Classification for Max | Kennedy Classification for Man | Type of Polyamide Denture | Allergy | Reason for the Choice | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|---|
| P. Papi et al. (2016) | Prosthetic rehabilitation with partial removable and esthetic dentures (Valplast) in a patient with recurrent right TMJ ankylosis: A case report [30] | case report | 1 | 45 | f | / | / | Partial removable | Not reported | esthetic and functional | Positive |
| M. B. Yaala et al. (2024) | LA PROTHÈSE FLEXIBLE DANS TOUS SES ASPECTS THE FLEXIBLE PROSTHESIS IN ALL ASPECTS [31] | case series | 2 | 45 | m | I | III | Partial removable | Not reported | esthetic | Not reported |
| 42 | f | 21 | - | Partial removable | Not reported | esthetic | Not reported | ||||
| S. Spintzyk et al. (2021) | Three-dimensional printing of polyamide to fabricate a non-metal clasp removable partial denture via fused filament fabrication: a case report [32] | case report | 1 | Not reported | f | 26 | - | Partial removable | Not reported | indicated | Not reported |
| K. L. Mounika et al. (2021) | Pliable Dentures-An Alternate Denture Base Material-Case Reports [33] | case series | 1 | 58 | m | I (skeletal type prosthesis) | III | Partial removable | Not reported | Not reported | Not reported |
| S. Ahuja et al. (2019) | Restoration of a partially edentulous patient with combination partial dentures [34] | case report | 1 | 77 | m | I | I | Partial removable | Not reported | esthetic | Negative |
| L. Kavaja et al. (2018) | TEMPORARY PROSTHETICS REHABILITATION IN ADOLESCENTS PATIENT [35] | case report | 1 | 16 | f | III | II | Partial removable | Not reported | esthetic and functional | Not reported |
| A. Belal et al. (2021) | Possibility of Using Flexible Dentures over Iliac Bone Graft in Adolescent Patients with Ameloblastoma: A 9-Month Follow-Up Clinical Report [36] | case report | 1 | 12 | m | no | II | Partial removable | Not reported | esthetic and functional | Not reported |
| J. Gandhimathi et al. (2015) | A systematic approach for functional rehabilitation of hemimandibulectomy patient [37] | case report | 1 | 25 | f | I | I | Partial removable with acetal resins clasps | Not reported | esthetic and functional | Positive |
| I. J. Kwon et al. (2016) | Newly designed retentive posts of mandibular reconstruction plate in oral cancer patients based on preliminary FEM study [38] | case series | 2 | 58 | f | no | II | Partial removable on retentive posts applied in the reconstruction plates | Not reported | functional | Positive |
| 52 | m | totlal edentulism | totlal edentulism | Partial removable on retentive posts applied in the reconstruction plates | Not reported | functional | positive |
| Author (Year) | Type of Study | JBI Tool Used | Total “Yes” Score (%) | Risk of Bias | Main Bias Source |
|---|---|---|---|---|---|
| P. Papi et al. (2016) [30] | Case report | JBI Case Report Checklist | 45% | High | Lack of follow-up; unclear outcome measurement |
| M.B. Yaala et al. (2024) [31] | Case series | JBI Case Series Checklist | 40% | High | Incomplete patient data; absence of standardized outcome assessment |
| S. Spintzyk et al. (2021) [32] | Case report | JBI Case Report Checklist | 60% | Moderate | Limited description of prosthetic adaptation process |
| K.L. Mounika et al. (2021) [33] | Case series | JBI Case Series Checklist | 45% | High | Missing follow-up; unclear inclusion criteria |
| S. Ahuja et al. (2019) [34] | Case report | JBI Case Report Checklist | 35% | High | Absence of long-term evaluation; limited reproducibility |
| L. Kavaja et al. (2018) [35] | Case report | JBI Case Report Checklist | 80% | Low | Minor reporting limitations |
| A. Belal et al. (2021) [36] | Case report | JBI Case Report Checklist | 70% | Low | Small sample size; adequate clinical description |
| J. Gandhimathi et al. (2015) [37] | Case report | JBI Case Report Checklist | 85% | Low | Good follow-up and clear intervention reporting |
| I.J. Kwon et al. (2016) [38] | Case series | JBI Case Series Checklist | 40% | High | Limited case details; no patient-reported outcomes |
| Category | Description | Impact on Results | Potential Mitigation |
|---|---|---|---|
| Limited sample size | Only 11 patients across 9 studies | Reduces statistical power and external validity | Future multicenter studies with larger samples |
| Research design | All included papers were case reports or small case series | High risk of bias; absence of control groups | Conduct prospective comparative or randomized trials |
| Inconsistent follow-up | Follow-up duration reported in less than half of the studies | Prevents evaluation of long-term outcomes | Standardized follow-up protocols (≥12 months) |
| Lack of standardized outcome measures | Esthetic, comfort, and function were qualitatively described only | Limits comparability and meta-analysis | Use validated questionnaires (e.g., OHIP-EDENT) |
| Absence of confirmed allergy cases | No study included patients with diagnostic confirmation of acrylic hypersensitivity | Limits conclusions regarding the allergy-safe claim | Inclusion of patch-tested patients in future research |
| Incomplete reporting | Missing details on prosthesis fabrication, hygiene, and maintenance | Reduces reproducibility | Implement CONSORT-like reporting checklists |
| Potential publication bias | Positive outcomes overrepresented | Inflates apparent success rate | Systematic registration of case studies |
| Language and regional bias | Most reports from single centers or specific countries | Limits generalizability | Encourage international multicenter collaboration |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceraulo, S.; Barbarisi, A.; Hu, Z.H.; Caccianiga, G.; Lauritano, D.; Carinci, F. The Use of the Flexible Thermoplastic Nylon-Based Dental Prostheses: A Literature Review. Prosthesis 2025, 7, 169. https://doi.org/10.3390/prosthesis7060169
Ceraulo S, Barbarisi A, Hu ZH, Caccianiga G, Lauritano D, Carinci F. The Use of the Flexible Thermoplastic Nylon-Based Dental Prostheses: A Literature Review. Prosthesis. 2025; 7(6):169. https://doi.org/10.3390/prosthesis7060169
Chicago/Turabian StyleCeraulo, Saverio, Antonio Barbarisi, Zhong Hao Hu, Gianluigi Caccianiga, Dorina Lauritano, and Francesco Carinci. 2025. "The Use of the Flexible Thermoplastic Nylon-Based Dental Prostheses: A Literature Review" Prosthesis 7, no. 6: 169. https://doi.org/10.3390/prosthesis7060169
APA StyleCeraulo, S., Barbarisi, A., Hu, Z. H., Caccianiga, G., Lauritano, D., & Carinci, F. (2025). The Use of the Flexible Thermoplastic Nylon-Based Dental Prostheses: A Literature Review. Prosthesis, 7(6), 169. https://doi.org/10.3390/prosthesis7060169










