Comparison of Vertical Measurements Between Panoramic Radiograph Images and Corresponding Cone-Beam Computed Tomography Scans
Abstract
1. Introduction
2. Materials and Methods
- -
- Images taken between February 2010 and January 2017;
- -
- Images with correct patient positioning;
- -
- Clear reference points were visible and well reproducible in both images.Participants were excluded if, in the measurement area on one or both image modalities, the following conditions were met:
- -
- Apical lesions, extractions, augmentations or implantations were detected;
- -
- No matching dental status in PAN/CBCT was available;
- -
- Deviation of alveolar bone morphology or the maxillary sinus floor was detected;
- -
- Periodontal defects were visible;
- -
- Artefacts (e.g., metal restorations of the crestal alveolar process) were present.
3. Results
Vertical Measurements with Defects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBCT | cone-beam computed tomography |
| cm | centimetre |
| DH | defect height |
| FOV | field of view |
| kV | kilovolt |
| M1 | first molar mesial |
| M2 | first molar distal |
| mA | milliampere |
| mm | millimetre |
| PAN | panoramic radiography |
| SD | standard deviation |
| sec | second |
| SL | sinus lifting |
| VD | vertical distance |
References
- Buser, D.; Chappuis, V.; Belser, U.C.; Chen, S. Implant placement post extraction in esthetic single tooth sites: When immediate, when early, when late? Periodontol. 2000 2017, 73, 84–102. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Hämmerle, C.H. European Workshop on Periodontology Group C. Advances in bone augmentation to enable dental implant placement: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35 (Suppl. S8), 168–172. [Google Scholar] [CrossRef] [PubMed]
- Aghaloo, T.L.; Moy, P.K. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int. J. Oral Maxillofac. Implant. 2007, 22, 49–70, Erratum in Int. J. Oral Maxillofac. Implant. 2008, 23, 56. [Google Scholar] [PubMed]
- Khoury, F.; Schmidt, C.; Jackowski, J. The influence of suturing and or gluing of perforated Schneiderian membrane during sinuslift procedure on the outcome: A retrospective study. Int. J. Implant. Dent. 2024, 10, 48. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pjetursson, B.E.; Tan, W.C.; Zwahlen, M.; Lang, N.P. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J. Clin. Periodontol. 2008, 35 (Suppl. S8), 216–240. [Google Scholar] [CrossRef] [PubMed]
- Zijderveld, S.A.; van den Bergh, J.P.; Schulten, E.A.; ten Bruggenkate, C.M. Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures. J. Oral Maxillofac. Surg. 2008, 66, 1426–1438. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Eguia, A.; Alkhraisat, M.H. Extra-short implants (≤6.5 mm in length) in atrophic and non-atrophic sites to support screw-retained full-arch restoration: A retrospective clinical study. Int. J. Implant. Dent. 2023, 9, 29. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thoma, D.S.; Haas, R.; Sporniak-Tutak, K.; Garcia, A.; Taylor, T.D.; Tutak, M.; Pohl, V.; Hämmerle, C.H.F. Randomized controlled multi-centre study comparing shorter dental implants (6 mm) to longer dental implants (11–15 mm) in combination with sinus floor elevation procedures: 10-year data. J. Clin. Periodontol. 2024, 51, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Pistilli, R.; Felice, P.; Cannizzaro, G.; Piatelli, M.; Corvino, V.; Barausse, C.; Buti, J.; Soardi, E.; Esposito, M. Posterior atrophic jaws rehabilitated with prostheses supported by 6 mm long 4 mm wide implants or by longer implants in augmented bone. One-year post-loading results from a pilot randomised controlled trial. Eur. J. Oral Implantol. 2013, 6, 359–372. [Google Scholar] [PubMed]
- Esquivel, J.; Meda, R.G.; Blatz, M.B. The Impact of 3D Implant Position on Emergence Profile Design. Int. J. Periodontics Restor. Dent. 2021, 41, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Pelekos, G.; Chin, B.; Wu, X.; Fok, M.R.; Shi, J.; Tonetti, M.S. Association of crown emergence angle and profile with dental plaque and inflammation at dental implants. Clin. Oral Implants Res. 2023, 34, 1047–1057. [Google Scholar] [CrossRef] [PubMed]
- Jose, E.P.; Paul, P.; Reche, A. Soft Tissue Management Around the Dental Implant: A Comprehensive Review. Cureus 2023, 15, e48042. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Puisys, A.; Janda, M.; Auzbikaviciute, V.; Gallucci, G.O.; Mattheos, N. Contour angle and peri-implant tissue height: Two interrelated features of the implant supracrestal complex. Clin. Exp. Dent. Res. 2023, 9, 418–424. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fayek, M.M.; Amer, M.E.; Bakry, A.M. Evaluation of the posterior superior alveolar artery canal by cone-beam computed tomography in a sample of the Egyptian population. Imaging Sci. Dent. 2021, 51, 35–40. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hung, K.; Montalvao, C.; Yeung, A.W.K.; Li, G.; Bornstein, M.M. Frequency, location, and morphology of accessory maxillary sinus ostia: A retrospective study using cone beam computed tomography (CBCT). Surg. Radiol. Anat. 2020, 42, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Kämmerer, P.W.; Thiem, D.; Eisenbeiß, C.; Dau, M.; Schulze, R.K.; Al-Nawas, B.; Draenert, F.G. Surgical evaluation of panoramic radiography and cone beam computed tomography for therapy planning of bisphosphonate-related osteonecrosis of the jaws. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Friedland, B.; Metson, R. A guide to recognizing maxillary sinus pathology and for deciding on further preoperative assessment prior to maxillary sinus augmentation. Int. J. Periodontics Restor. Dent. 2014, 34, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Lurie, A.G. Panoramic Imaging. In Oral Radiology: Principles and Interpretation, 5th ed.; White, S.C., Pharoah, M.J., Eds.; Mosby: Shanghai, China, 2004; pp. 191–209. [Google Scholar]
- Crockett, B.; Broome, A.; Tawil, P.; Tyndall, D. Comparison of incidental findings on cone beam computed tomographic and 2-dimensional images. Gen. Dent. 2023, 71, 64–71. [Google Scholar] [PubMed]
- Fukuda, M.; Matsunaga, S.; Odaka, K.; Oomine, Y.; Kasahara, M.; Yamamoto, M.; Abe, S. Three-dimensional analysis of incisive canals in human dentulous and edentulous maxillary bones. Int. J. Implant. Dent. 2015, 1, 12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ketabi, A.R.; Hassfeld, S.; Lauer, H.C.; Piwowarczyk, A. The comparison of visibility of the maxillary sinus septa between cone-beam computed tomography scans and panoramic radiograph images as dependent on the cortical bone thickness: A retrospective comparative study. Int. J. Implant. Dent. 2024, 10, 23. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Chen, Z.; Li, J.; Sinjab, K.; Mendonca, G.; Yu, H.; Wang, H.L. Accuracy of flapless immediate implant placement in anterior maxilla using computer-assisted versus freehand surgery: A cadaver study. Clin. Oral Implants Res. 2018, 29, 1186–1194. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.F.; De Kok, I.J.; Thalji, G.; Bryington, M.S. Prosthodontic Management of Implant Therapy: Esthetic Complications. Dent. Clin. N. Am. 2019, 63, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Shiki, K.; Tanaka, T.; Kito, S.; Wakasugi-Sato, N.; Matsumoto-Takeda, S.; Oda, M.; Nishimura, S.; Morimoto, Y. The significance of cone beam computed tomography for the visualization of anatomical variations and lesions in the maxillary sinus for patients hoping to have dental implant-supported maxillary restorations in a private dental office in Japan. Head. Face Med. 2014, 10, 20. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Malina-Altzinger, J.; Damerau, G.; Grätz, K.W.; Stadlinger, P.D. Evaluation of the maxillary sinus in panoramic radiography-a comparative study. Int. J. Implant. Dent. 2015, 1, 17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lana, J.P.; Carneiro, P.M.; Machado Vde, C.; de Souza, P.E.; Manzi, F.R.; Horta, M.C. Anatomic variations and lesions of the maxillary sinus detected in cone beam computed tomography for dental implants. Clin. Oral Implants Res. 2012, 23, 1398–1403. [Google Scholar] [CrossRef] [PubMed]
- Wolff, C.; Mücke, T.; Wagenpfeil, S.; Kanatas, A.; Bissinger, O.; Deppe, H. Do CBCT scans alter surgical treatment plans? Comparison of preoperative surgical diagnosis using panoramic versus cone-beam CT images. J. Craniomaxillofac. Surg. 2016, 44, 1700–1705. [Google Scholar] [CrossRef] [PubMed]
- Maridati, P.; Stoffella, E.; Speroni, S.; Cicciu, M.; Maiorana, C. Alveolar antral artery isolation during sinus lift procedure with the double window technique. Open Dent. J. 2014, 8, 95–103. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wen, S.C.; Chan, H.L.; Wang, H.L. Classification and management of antral septa for maxillary sinus augmentation. Int. J. Periodontics Restor. Dent. 2013, 33, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Özalp, Ö.; Tezerişener, H.A.; Kocabalkan, B.; Büyükkaplan, U.Ş.; Özarslan, M.M.; Şimşek Kaya, G.; Altay, M.A.; Sindel, A. Comparing the precision of panoramic radiography and cone-beam computed tomography in avoiding anatomical structures critical to dental implant surgery: A retrospective study. Imaging Sci. Dent. 2018, 48, 269–275. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Storelli, S.; Abbà, A.; Scanferla, M.; Botticelli, D.; Romeo, E. 6 mm vs 10 mm-long implants in the rehabilitation of posterior jaws: A 10-year follow-up of a randomised controlled trial. Eur. J. Oral Implantol. 2018, 11, 283–292. [Google Scholar] [PubMed]
- Mecall, R.A.; Rosenfeld, A.L. Influence of residual ridge resorption patterns on implant fixture placement and tooth position. 1. Int. J. Periodontics Restor. Dent. 1991, 11, 8–23. [Google Scholar] [PubMed]
- Thoma, D.S.; Mühlemann, S.; Jung, R.E. Critical soft-tissue dimensions with dental implants and treatment concepts. Periodontol. 2000 2014, 66, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Couso-Queiruga, E.; Stuhr, S.; Tattan, M.; Chambrone, L.; Avila-Ortiz, G. Post-extraction dimensional changes: A systematic review and meta-analysis. J. Clin. Periodontol. 2021, 48, 126–144. [Google Scholar] [CrossRef] [PubMed]
- Suomalainen, A.; Pakbaznejad Esmaeili, E.; Robinson, S. Dentomaxillofacial imaging with panoramic views and cone beam CT. Insights Imaging 2015, 6, 1–16. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schulze, R.; Heil, U.; Gross, D.; Bruellmann, D.D.; Dranischnikow, E.; Schwanecke, U.; Schoemer, E. Artefacts in CBCT: A review. Dentomaxillofac. Radiol. 2011, 40, 265–273. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tronje, G.; Eliasson, S.; Julin, P.; Welander, U. Image distortion in rotational panoramic radiography. II. Vertical distances. Acta Radiol. Diagn. 1981, 22, 449–455. [Google Scholar] [CrossRef] [PubMed]
- ICRP Publication 105. Radiation protection in medicine. Ann. ICRP 2007, 37, 1–63. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, T.; Arai, Y.; Chikui, T.; Hayashi-Sakai, S.; Honda, K.; Indo, H.; Kawai, T.; Kobayashi, K.; Murakami, S.; Nagasawa, M.; et al. Clinical guidelines for dental cone-beam computed tomography. Oral Radiol. 2018, 34, 89–104. [Google Scholar] [CrossRef] [PubMed]
| N | Mean | SD | Minimum | Maximum | Percentiles | ||||
|---|---|---|---|---|---|---|---|---|---|
| 25th | 50th | 75th | |||||||
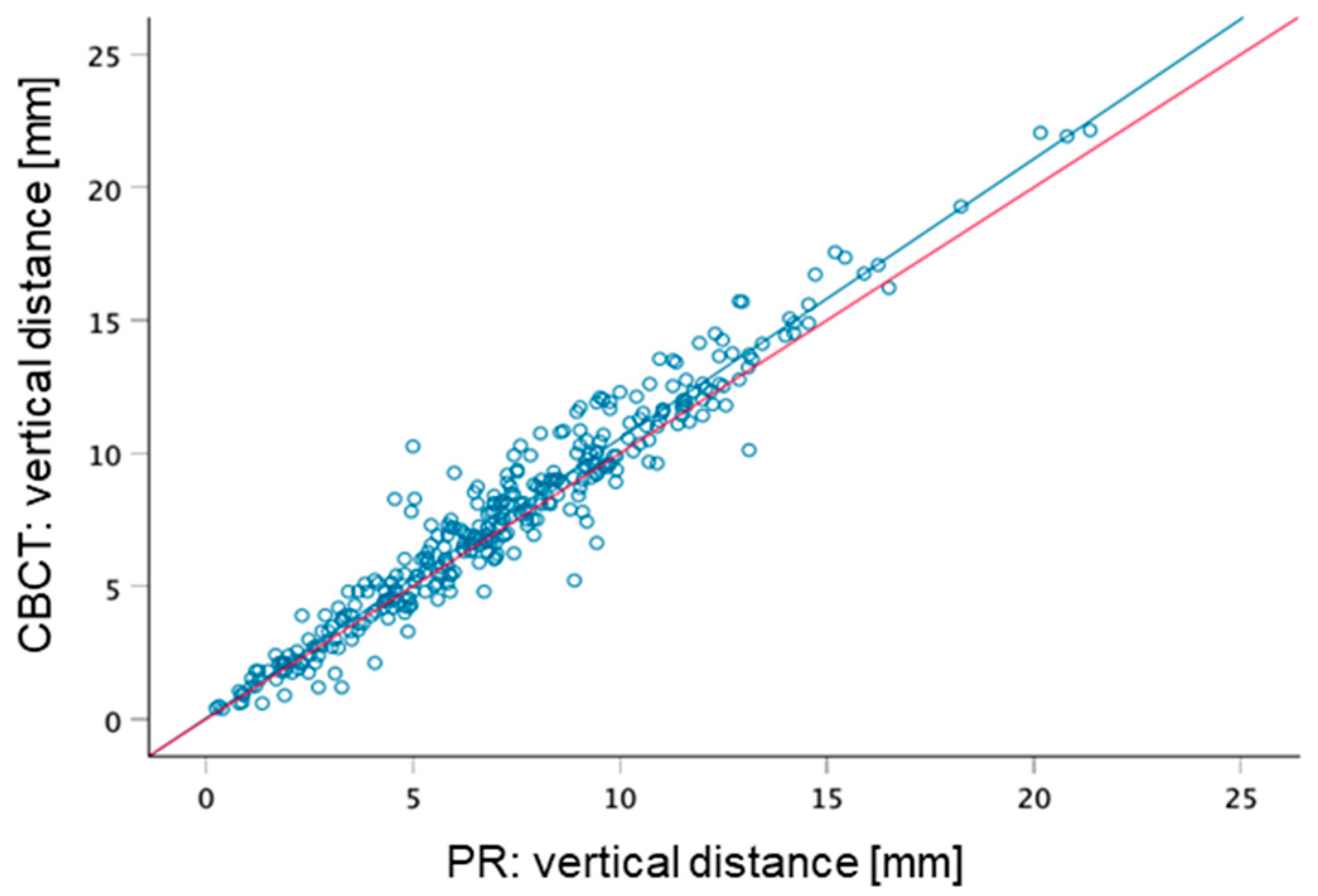
| Maxilla right | PAN | 175 | 7.45 | 3.77 | 0.32 | 20.16 | 4.80 | 7.12 | 9.52 |
| CBCT | 175 | 7.93 | 4.16 | 0.50 | 22.05 | 4.81 | 7.51 | 10.31 | |
| Maxilla left | PAN | 166 | 6.95 | 3.71 | 0.24 | 21.36 | 4.38 | 6.84 | 9.44 |
| CBCT | 166 | 7.30 | 3.94 | 0.39 | 22.15 | 4.28 | 7.28 | 9.91 | |
| Total | PAN | 341 | 7.21 | 3.74 | 0.24 | 21.36 | 4.56 | 6.96 | 9.44 |
| CBCT | 341 | 7.62 | 4.06 | 0.39 | 22.15 | 4.80 | 7.35 | 10.07 | |
| Region | Paired Differences | t | df | Significance | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | SEM | 95% Difference CI | One-Sided p | Two-Sided p | ||||||
| Lower | Upper | ||||||||||
| Maxilla right | Pair 1 | PAN–CBCT | −0.48 | 1.07 | 0.081 | −0.64 | −0.32 | −5.89 | 174 | 0.0001 | 0.0001 |
| Maxilla left | Pair 1 | PAN–CBCT | −0.35 | 0.98 | 0.076 | −0.50 | −0.20 | −4.57 | 165 | 0.0001 | 0.0001 |
| Total | Pair 1 | PAN–CBCT | −0.41 | 1.03 | 0.056 | −0.52 | −0.30 | −7.43 | 340 | 0.0001 | 0.0001 |
| Standardiser | Point Estimate | 95% Confidence Interval | |||||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Maxilla right | Pair 1 | PAN–CBCT | Cohen’s d | 1.072 | −0.445 | −0.600 | −0.289 |
| Hedges’ correction | 1.076 | −0.443 | −0.597 | −0.288 | |||
| Maxilla left | Pair 1 | PAN–CBCT | Cohen’s d | 0.979 | −0.355 | −0.511 | −0.197 |
| Hedges’ correction | 0.983 | −0.353 | −0.509 | −0.196 | |||
| Total | Pair 1 | PAN–CBCT | Cohen’s d | 1.028 | −0.402 | −0.512 | −0.292 |
| Hedges’ correction | 1.031 | −0.402 | −0.511 | −0.291 | |||
| Region | N | Mean | SD | Minimum | Maximum | Percentile | |||
|---|---|---|---|---|---|---|---|---|---|
| 25th | 50th | 75th | |||||||
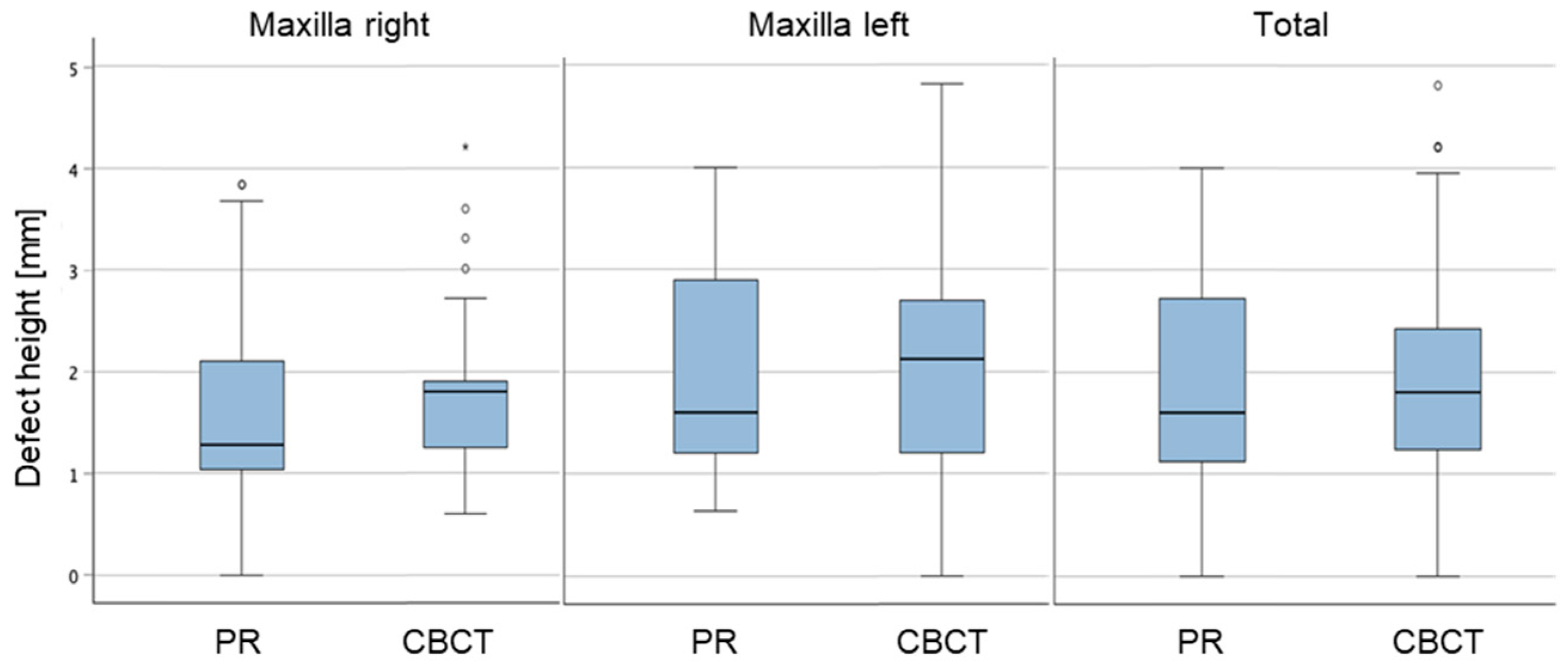
| Maxilla right | PAN defects | 33 | 1.74 | 1.03 | 0.00 | 3.84 | 1.04 | 1.28 | 2.41 |
| CBCT defects | 33 | 1.85 | 0.82 | 0.60 | 4.21 | 1.25 | 1.80 | 2.00 | |
| Maxilla left | PAN defects | 25 | 1.99 | 1.09 | 0.64 | 4.00 | 1.16 | 1.60 | 2.93 |
| CBCT defects | 25 | 2.20 | 1.19 | 0.00 | 4.81 | 1.20 | 2.12 | 2.85 | |
| Total | PAN defects | 58 | 1.85 | 1.05 | 0.00 | 4.00 | 1.12 | 1.60 | 2.64 |
| CBCT defects | 58 | 1.99 | 1.00 | 0.00 | 4.81 | 1.24 | 1.80 | 2.42 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ketabi, A.-R.; Hassfeld, S.; Schuster, L.; Ketabi, S.; Stueben, J.; Piwowarczyk, A. Comparison of Vertical Measurements Between Panoramic Radiograph Images and Corresponding Cone-Beam Computed Tomography Scans. Prosthesis 2025, 7, 131. https://doi.org/10.3390/prosthesis7060131
Ketabi A-R, Hassfeld S, Schuster L, Ketabi S, Stueben J, Piwowarczyk A. Comparison of Vertical Measurements Between Panoramic Radiograph Images and Corresponding Cone-Beam Computed Tomography Scans. Prosthesis. 2025; 7(6):131. https://doi.org/10.3390/prosthesis7060131
Chicago/Turabian StyleKetabi, Ali-Reza, Stefan Hassfeld, Laurentia Schuster, Sandra Ketabi, Julius Stueben, and Andree Piwowarczyk. 2025. "Comparison of Vertical Measurements Between Panoramic Radiograph Images and Corresponding Cone-Beam Computed Tomography Scans" Prosthesis 7, no. 6: 131. https://doi.org/10.3390/prosthesis7060131
APA StyleKetabi, A.-R., Hassfeld, S., Schuster, L., Ketabi, S., Stueben, J., & Piwowarczyk, A. (2025). Comparison of Vertical Measurements Between Panoramic Radiograph Images and Corresponding Cone-Beam Computed Tomography Scans. Prosthesis, 7(6), 131. https://doi.org/10.3390/prosthesis7060131






