1. Introduction
Aging is a universal, ongoing, and irreversible process that involves loss of function, but it varies among individuals. Although the Chilean population has a life expectancy of over 80 years, total life expectancy encompasses both healthy and unhealthy years [
1]. In practical terms, this means that a substantial fraction of the added years of life are lived with morbidity and with varying degrees of functional limitation. The demographic shift towards an older age structure has placed increasing pressure on health and social care systems, amplifying the importance of preventive strategies that sustain functionality for as long as possible.
Along with the country’s rapid economic growth over the past few decades, public policies addressing socioeconomic inequalities have been inadequate [
2]. The persistence of structural inequalities has translated into marked gradients in health status, health behaviors, and access to timely and effective care. These gradients are particularly evident in older adults, a group in which cumulative exposures across the life course compound the effects of current barriers to care. Additionally, the structure of the health system, characterized by the coexistence of public health insurance programs and market-based private health insurance, has exacerbated unequal access to healthcare [
3]. While in the public health system, employee contributions are based on income; in the private insurance system, contributions depend on individual health risks and the number of dependents. Private health insurance companies are permitted to create barriers to enrollment for poorer and older individuals by raising premiums, deductibles, and copayments, as well as considering pre-existing conditions and health status [
4]. Consequently, older people enrolled in the private health insurance system tend to be a select group with incomes high enough to afford these costs [
4,
5].
Chile has a population of 19.6 million people. The portion aged 60 and over accounts for 18% (3.5 million) [
6]. Of these, 86% are self-sufficient [
7]. Most older adults receive care through the public health system, with 87.6% of those aged 60 to 64 and 91.9% of those aged 65 and older receiving care through this system. These figures are relevant to oral health because patterns of service use, benefit design, and coverage of rehabilitative interventions differ substantially between public and private schemes. In an aging society, the ability to access routine dental care, prosthetic rehabilitation, and follow-up directly influences nutritional status, communication, and quality of life.
In addition to changes in vision, hearing, smell, taste, and swallowing, there is also a decrease in salivary flow and a higher risk of tooth loss, along with a gradual decline in muscle mass and strength. Geriatric syndromes [
8] emerge as multifactorial health conditions that develop when deficiencies in multiple systems combine, making older individuals vulnerable to various challenges [
9]. These common conditions, if not managed through interdisciplinary care [
10,
11,
12,
13], threaten independence. This includes sarcopenia and frailty. Handgrip strength (HGS) is a strong predictor of sarcopenia, a condition that contributes to frailty [
14]. Beyond its role as a surrogate of global muscle function, HGS is an attractive marker for clinical services because it is simple, inexpensive, and reproducible across settings. It correlates with mobility, disability, and adverse outcomes, and it has been proposed as a core vital sign in geriatric assessment.
A primary focus of geriatrics is maintaining autonomy and preventing frailty. Research has shown that the masseter muscle thickness in healthy older adults correlates with grip strength. They suggest that decreased grip strength could indicate reduced masseter muscle mass, especially in men. It is possible to increase masseter muscle thickness by restoring occlusion in healthy older adults, regardless of age [
15]. This observation supports a plausible biological link between oral function and systemic muscle performance: rehabilitation of occlusal support improves masticatory efficiency, which can favor nutritional intake and stimulate orofacial musculature, with downstream effects on overall muscle conditioning [
15,
16]. Other researchers have examined the fit and presence of sarcopenia in removable denture users. Individuals with poorly fitting dentures face a significantly higher risk of sarcopenia than those with well-fitting dentures. Their findings indicate that deteriorating dentition is strongly associated with sarcopenia among community-dwelling Japanese adults aged ≥75 years [
16]. Together, these findings situate oral rehabilitation as a potential lever for improving functional health in older populations.
In Chile, the public system, which serves patients with health insurance through the National Health Fund (FONASA), offers preventive medical exams for older adults (EMPAM) [
17], including a Comprehensive Geriatric Assessment for individuals aged 65 and older. This exam is conducted at Family Health Centers (CESFAM) and involves anthropometric measurements, as well as assessments of functional, mental, and social aspects. It is free, performed annually, and supported by ministerial public policies. Its goal is to identify factors that could lead to loss of functionality and to develop a care and follow-up plan for implementation by the health team, as is common in other regions [
18,
19,
20]. In Chile, significant progress has been made in emphasizing the importance of regular check-ups for older adults. Similarly to Mexico [
21], today, 65% of older adults enrolled in primary healthcare (PHC) have current health records. Notably, the structured nature of EMPAM—anchored in routine invitations and standardized instruments—facilitates longitudinal monitoring and timely referrals.
The Chilean private health system (ISAPRES) also includes EMPAM, which designates the providers that beneficiaries must visit. If individuals choose to have the exam from providers other than those specified by their insurance, they forfeit the free benefit. They receive a comprehensive evaluation there, but must pay for any tests they request [
22]. This organizational detail has practical implications: adherence to routine checks may be lower, and out-of-pocket expenses can inhibit follow-through with recommended investigations or rehabilitative treatments, including dental prostheses. Regarding oral health, according to the National Health Survey (ENS) 2016–2017 in Chile, partial edentulism has a prevalence of 79.8% among people aged 65 to 74, and total edentulism has a prevalence of 17.6%. For those aged 75 and older, these prevalences shift to 57.8% for partial and 41.2% for total edentulism. The use of upper and lower dentures at age 75 has a prevalence of 40.7% [
23]. These figures underscore the substantial demand for prosthetic rehabilitation and the importance of ensuring adequate fit, comfort, and function, as suboptimal prostheses may impair chewing, nutrition, and social participation.
At the national level, there is a ministerial program called Explicit Health Guarantees (GES), specifically GES 60. It is the only dental program for older adults, providing comprehensive dental care for individuals up to 60 years, 11 months, and 29 days old. It does not include monitoring or follow-up of the oral health conditions of the beneficiaries after the interventions [
24]. This cut-off and the absence of post-treatment surveillance leave a gap precisely at the stage of life when edentulism and functional vulnerability intensify.
Maintaining natural dentition or using removable dental prostheses (RDPs) is essential for preserving masticatory function, ensuring proper nutrition, and preventing geriatric syndromes in the elderly population (EP) [
25]. In this context, RDPs are not merely aesthetic devices: they restore occlusal contacts, support soft tissues, and can improve phonation and social confidence. Building on these considerations, this study aimed to compare changes in HGS adjusted for masticatory function, risk of malnutrition, and body mass index (BMI) after denture use in two groups of elderly patients aged 70 and older from the public and private sectors in Chile. We hypothesized that immediate oral functionalization with RDPs would be associated with immediate improvements in HGS, and that differences between health systems might reflect varying baseline characteristics and patterns of care.
2. Methods
2.1. Participants
A prospective, pre–post study was conducted. Between March 2020 and 2023, patients aged 70 years and older who had no molars or premolars and provided informed consent were included. Exclusion criteria included refusal to participate, cognitive or sensory impairments, and functional dependence that prevented reliable evaluation. They were categorized based on masticatory function according to the Eichner index [
26] and assessed for malnutrition risk or absence using calf circumference (CC) and BMI.
Participants were recruited from lists of patients undergoing routine prosthodontic care. Eligibility screening was performed by calibrated clinicians who verified the absence of posterior occlusal contacts and confirmed the planned delivery of RDPs. The target population comprised community-dwelling older adults who were independently mobile and able to attend clinic visits. Because the pandemic overlapped with the enrolment period, visits were organized to minimize exposure risk, and local infection-prevention guidance was followed. The design was pragmatic and mirrored real-world care pathways in both systems.
2.2. Data Collection
The primary outcome was HGS of the dominant hand. Measurements were taken with a manual hydraulic dynamometer (Jamar™ Sammons Preston, Rolyon, Bolingbrrook, IL, USA) following a standardized seated protocol. The shoulder was abducted and neutrally rotated, the elbow flexed at 90°, the forearm in a neutral position, and the wrist between 0° and 30° dorsiflexion. Two attempts were recorded at each time point while participants clenched their teeth; the higher value (kg) was used for analysis. According to the European Working Group on Sarcopenia in the Elderly, grip strength levels of ≤30 kg in men and ≤20 kg in older women indicate a risk of sarcopenia.
Masticatory function was evaluated using the Eichner index, which classifies occlusal support based on the presence of contacts in four posterior support zones (left and right premolar–molar regions) formed by natural teeth, fixed prostheses, or implant-supported prostheses. Occlusal contacts were identified in maximum intercuspation using articulating paper under light bite closure, and the class was assigned by calibrated examiners. Category A indicates contacts in all four support zones (full posterior support). Category B indicates contacts in one to three support zones (reduced posterior support). Category C indicates no occlusal contacts in any of the support zones (no posterior support). For this analysis, categories B and C encompassed the spectrum of impaired posterior support. The Eichner Index categories, which include patients with premolar and molar loss, correspond to categories B and C. For calf circumference, a cutoff point of ≤31 cm was used for both sexes to identify malnourished older adults with low muscle mass and nutritional risk [
27]. Regarding BMI, thinness was defined as a BMI < 23.0; normal as 23.0–27.9; overweight as >28.0–31.9; and obesity as ≥32.0 [
28].
We also recorded age, sex, and the health system (public or private). Where available, clinical notes were reviewed to identify comorbid conditions and medication use. These variables were inspected descriptively to understand the case mix but were not used as model covariates to preserve degrees of freedom and avoid overfitting in subgroup analyses.
2.3. Quality Assurance
HGS measurements were taken at two time points: baseline and 15 days after the prosthesis was used. The 15-day interval was selected to capture early functional gains once patients had adapted to the device while minimizing attrition. Clinicians provided standard instructions regarding insertion, removal, and hygiene, and made minor adjustments if discomfort or pressure areas were noted.
Three calibrated operators carried out all clinical and measurement procedures. Inter-operator agreement was substantial (Kappa = 0.79), confirming the reliability of classification and outcome measurement. Training included joint sessions on dynamometer positioning, Eichner index scoring using photographs and clinical cases, and the use of a checklist to ensure standardization at each visit. The private system cohort is derived from secondary data obtained from medical records accessible to the authors, provided by private treating clinicians. Data extraction followed a predefined template, and ambiguous entries were clarified with the treating teams.
2.4. Statistical Analysis
Differences in HGS were evaluated using a linear mixed-effects regression model with SAS 9.4 software (p < 0.05). The public system cohort comprises patients over 70 years of age who received prosthetic treatment at a public hospital in Santiago and participated in a project funded by the National Agency for Research and Development (ANID, Santiago, Chile), with approval from the Ethics Committee of the Eastern Metropolitan Health Service and signed informed consent.
Analytically, we modeled HGS as a continuous outcome with repeated measures at two time points (baseline and 15 days). Fixed effects included health system (public vs. private), time, sex, age, BMI, and malnutrition risk; a random intercept accounted for within-participant correlation. The main contrast of interest was the between-system difference at each time point and the change from baseline within system. Given the large sample size and the robustness of mixed models, estimates are reliable even with mild deviations. Missing outcome values were minimal; when present, mixed models provide valid inference under the assumption of missing at random by using all available data.
We summarized demographics and baseline clinical characteristics using means (standard deviations) or counts (percentages) as appropriate. p-values were two-sided with α = 0.05. To support interpretability, we report adjusted means with 95% confidence intervals and the absolute difference (Δ) between systems at each time point. No multiplicity adjustment was applied because outcomes and comparisons were prespecified and limited in number.
3. Results
The purposive sample consisted of 248 older adults, divided into two groups: 124 in the public system group and 124 in the private system group. Each group had 73 women (p > 0.05), with a mean age of 81.2 years in the public system and 75.2 years in the private system (p < 0.0001). These figures indicate that the public cohort was, on average, six years older than the private cohort, a difference that is clinically relevant given the age-related decline in muscle strength. The sex distribution was balanced across groups, simplifying interpretation of aggregate HGS results.
The mean BMI was 27.0 in those in the public system and 24.7 in those in the private system (
p < 0.0001). From a clinical standpoint, this implies that a larger proportion of the public cohort fell within the normal to overweight range, whereas the private cohort tended toward lower BMI values. The risk of malnutrition due to deficiency, as indicated by calf circumference, was found in 5 beneficiaries of the public system and 31 beneficiaries of the private system (
p < 0.0001) (
Table 1). This stark difference suggests that the private cohort contained a sizeable subgroup with low muscle mass, a factor known to depress HGS values and potentially attenuate the immediate gains following rehabilitation.
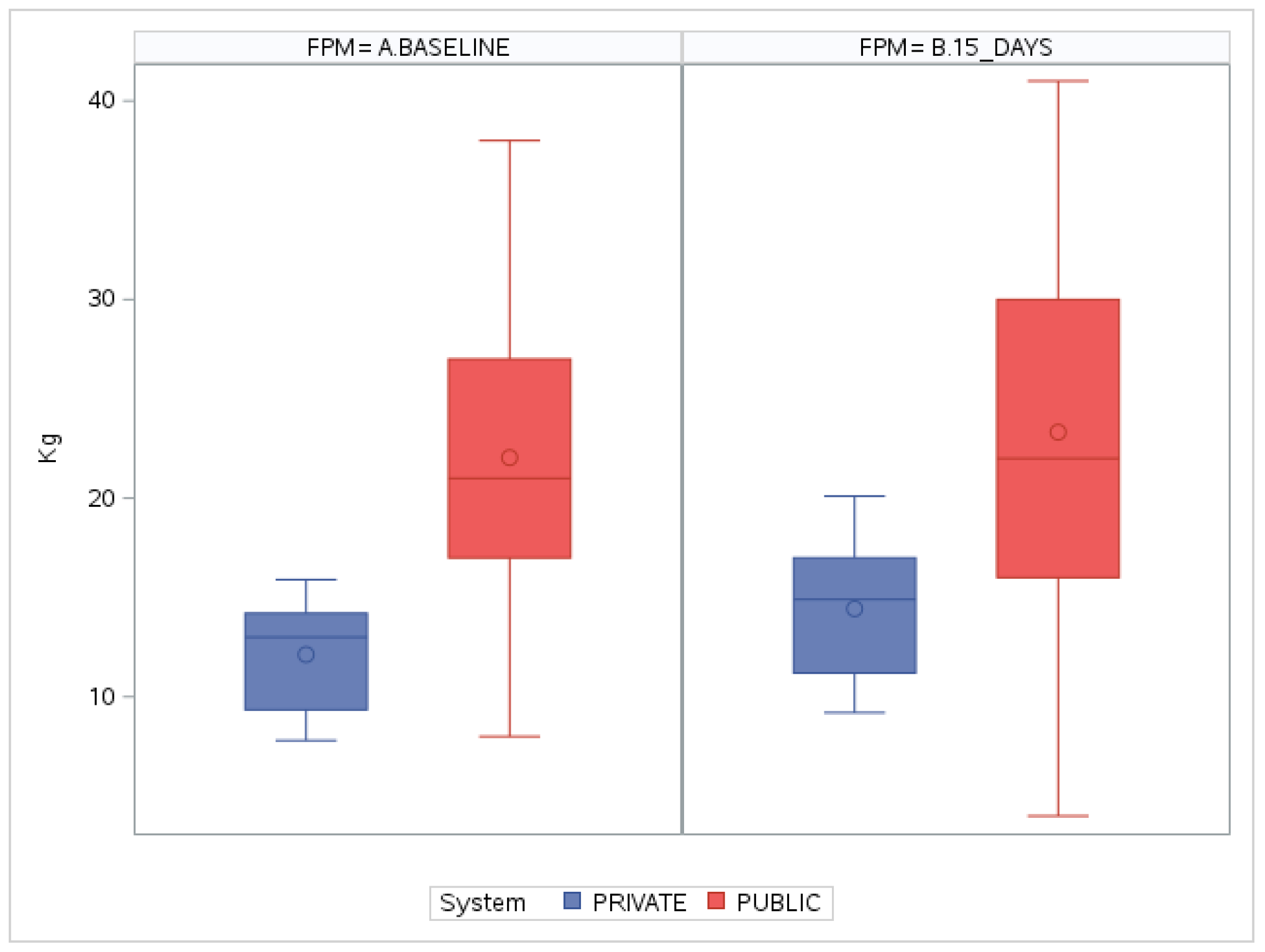
In a multivariate model adjusted for sex, age, BMI, and risk of malnutrition, baseline grip strength before prosthesis use was 22.8 kg in those in the public system and 11.7 kg in those in the private system. The post-prosthesis measurement was 23.0 kg in the public system and 14.2 kg in the private system (
Table 2). The variation in measurements compared to baseline values in the public system was an increase of 1.8 kg, while in the private system, the increase was 2.5 kg. These within-group changes, though modest in absolute terms, occurred over a short time frame and were directionally consistent with the hypothesized early functional benefits of RDP use.
Comparing the baseline measurements, a positive difference of up to 11.1 kg was observed in the public cohort compared to the private cohort (Δ11.1 kg;
p < 0.0001). After treatment, the positive difference decreased slightly to 8.8 kg more handgrip strength in the public system cohort (Δ = 8.8 kg;
p < 0.0001) (
Figure 1). The attenuation of the gap indicates that the private cohort experienced a relatively larger short-term improvement, albeit starting from a much lower baseline. Boxplots in
Figure 1 also reveal broader variability in the public group, consistent with its older age distribution yet higher mean strength; meanwhile, the private group shows a narrower spread with lower central tendency.
From a clinical perspective, the adjusted post-treatment HGS in the public cohort (23.0 kg) situates many women above the sarcopenia risk threshold and men nearer to the cut-point, whereas the private cohort mean (14.2 kg) remains well below typical thresholds for both sexes.
4. Discussion
This study provides pragmatic, real-world evidence that immediate functionalization with RDPs is associated with short-term improvements in HGS in older adults receiving care in Chile’s public and private systems. The pattern of results is coherent with the conceptual framework that links the restoration of occlusal support to improved mastication, enhanced food intake, and stimulation of the stomatognathic musculature, which may, in turn, contribute to systemic muscle performance. Although gains at 15 days were modest, they occurred against different baseline contexts—older age and higher BMI in the public group versus a substantially higher malnutrition risk in the private group—yet pointed in the same beneficial direction.
There are waiting lists for non-GES medical and dental care in the Chilean public system, with extended waiting times. Dental specialties account for 19.4%, involving approximately 447,143 people in 2023. The most in-demand specialty is Prosthodontics, which accounts for 26.6% [
29]. Data from the ‘GLOSA 06’ report, issued by the Chilean sub-secretariat of Healthcare Networks, shows that the number of patients awaiting oral rehabilitation increased from 126,083 in 2018 to 132,110 in 2019. However, the subsequent years saw a gradual decrease, with 121,236 cases in 2020, 113,137 in 2021, and 110,894 in 2022 [
30]. The reduction in cases on the waiting list since 2020 aligns with the COVID-19 pandemic years, during which mortality from this disease significantly affected the older population. These figures also suggest that access pressures are dynamic and sensitive to broader demographic and epidemiologic shocks.
There is no up-to-date information on the number of patients on waiting lists who have defective prosthetic devices, whether they were never able to use them, or how many are requiring them for the first time, except in the private system. A 1997 study of low-income elderly people with prostheses found that 47.4% of the devices were defective [
31]. The lack of dental care in partially or completely edentulous populations, as well as its association with comorbidities [
32,
33,
34,
35], has been shown to influence the relationship between nutritional status and oral health-related quality of life (OHrQoL). This relationship is also influenced by the need for and desire for prostheses [
36]. In other words, the simple presence of a prosthesis is not enough: fitness, comfort, and masticatory efficiency are critical determinants of whether oral rehabilitation translates into better diet, social engagement, and functional outcomes. Our results—short-term HGS gains following immediate use—may reinforce the notion that timely provision and adjustment matter and can have measurable systemic correlates.
The results show a normal nutritional status among older adults in both public and private health systems. This differs from data from the 2016–2017 National Health Survey, which indicated that only 21.5% of people aged 65 and older had a normal nutritional status. Several factors could explain the discrepancy. The present cohorts were recruited from clinical settings where individuals actively sought rehabilitative care; this group may be more engaged with health services, may receive more frequent counseling, and may have better social support than the general population. Additionally, BMI is an imperfect proxy for nutritional quality and muscle mass in older adults; sarcopenic obesity, for instance, can coexist with normal or elevated BMI.
The risk of malnutrition due to deficiency, assessed by calf circumference, was lower than in the Ñuble region of Chile, where 39.6% had deficits, and this was linked to a risk of sarcopenia [
37]. A Spanish study found a higher risk of malnutrition associated with smaller calf circumference measurements, at 74.2%, particularly among individuals over 85 years old [
38]. In our sample, the private group exhibited a substantially higher proportion at risk by calf circumference than the public group. This aligns with the markedly lower baseline HGS in the private cohort and underscores the importance of integrating nutritional and functional screening in routine dental care for older adults, especially in contexts where follow-up testing may incur out-of-pocket costs. It is plausible that individuals in the private system defer or fragment care because of copayments, leading to under-recognition of malnutrition and delayed rehabilitative interventions.
Regarding handgrip strength values, improvements were seen in both groups, with more notable results at baseline and within the private system. These were analyzed as a continuous numerical variable. In the model used, sex was not a significant explanatory variable because the groups were balanced, so no differences by sex were observed. The lack of sex differences should be interpreted with caution, as the use of absolute rather than sex-standardized HGS values may dilute the detection of interaction effects. Nonetheless, the direction of change was consistent across strata, suggesting that the immediate benefits of RDP use are generalizable across sexes.
The differences between users of the two health systems may stem from the fact that individuals in the public system are regularly monitored at primary care centers, where through the EMPAM, which includes the Comprehensive Geriatric Assessment, they are referred to the appropriate specialist when abnormalities are found. In contrast, monitoring in the private system relies on patients’ spontaneous requests, often leading to additional out-of-pocket costs. This situation could indicate that many older adults in the private system might be experiencing malnutrition or clinically unrecognized muscle loss, which directly affects their handgrip strength and may partly explain the observed findings. In practice, this means that strengthening routine geriatric assessment in private care—and ensuring that prosthodontic rehabilitation is embedded within multidisciplinary management—could narrow the functional gap we observed.
Handgrip strength has been suggested as a new vital sign in older adults, functioning as a key health biomarker that assesses muscle function and overall physical capacity [
14]. Weak handgrip strength is also seen as a predictor of cardiometabolic disease, disability, morbidity, and early death [
39]. A weakened musculoskeletal system is considered a major indicator of frailty. Handgrip strength is an important measure of physical performance that has been consistently used to diagnose musculoskeletal frailty. The improvements seen in both groups align with studies indicating that wearing dentures is associated with a lower risk of musculoskeletal frailty in older Americans, with nutritional intake accounting for about one-third of this link [
40]. In healthy individuals, age and gender are the main factors affecting hand grip strength [
41]. However, in cases of acute or chronic illness, other factors, such as disease severity, comorbidity load, medical treatments, and immobilization, also influence muscle weakness and, in turn, the overall well-being of patients. Still, hand grip strength remains a simple bedside measure that offers valuable insights beyond assessing nutritional and/or functional status. To identify patients at risk, dependable cutoff values still need to be established and validated [
42]. Recent studies have explored the connection between hand grip strength and oral health, including the number of teeth [
43,
44].
The improvements in handgrip strength observed in our study, compared to baseline values in both public and private systems, offer an optimistic view of how oral rehabilitation benefits older adults with dentition loss, particularly considering the positive impact that increased handgrip strength has on their daily lives. For example, a study on the connection between handgrip strength and falls in older adults found that in 808 individuals (409 men/399 women) in Germany, aged 65 and older, the risk of falls in the past 12 months decreased by about 3% for each 1 kg increase in maximum grip strength, after adjusting for age and gender. When analyzing women and men separately, both groups showed that those with low maximum grip strength experienced more falls compared to those with higher maximum grip strength [
45]. This magnitude suggests that even the 1.8–2.5 kg early gains observed here could translate into meaningful changes in fall risk if maintained or further improved over time. Moreover, improved chewing efficiency following RDP insertion may increase dietary protein and micronutrient intake, which are known to support muscle anabolism; such mechanisms provide a plausible pathway linking oral rehabilitation to functional resilience.
Strengths and Limitations
This study has several strengths. It employs a pragmatic design that mirrors real-world practice in both public and private systems, achieving a simple yet reliable functional outcome with strong clinical significance. Additionally, it includes a standardized classification of occlusal support via the Eichner index, demonstrating substantial inter-operator agreement. The sample size is relatively large for a dental rehabilitation study in older adults, allowing for adjusted estimation of between-system differences.
Limitations should also be noted. The follow-up period was short; more extended observation is needed to determine whether early HGS gains persist, grow with improved adaptation to RDPs, or attenuate over time. Although models were adjusted for age, sex, BMI, and malnutrition risk, residual confounding by unmeasured variables (e.g., comorbidity burden, physical activity, or socioeconomic status) is possible. The private cohort data were derived from medical records, which can introduce information variability despite standardized extraction. HGS was measured only on the dominant hand, and we did not collect patient-reported outcomes (e.g., satisfaction, OHrQoL) that could triangulate functional benefits. Finally, the study did not directly assess dietary intake changes; future work linking masticatory performance, nutritional biomarkers, and physical performance would be valuable.
Clinically, the results support the inclusion of HGS as part of routine pre- and post-prosthesis assessment. Measuring HGS requires minimal training and equipment and can serve as an anchor for interprofessional collaboration: when low values persist after prosthesis delivery, rapid referral to nutrition or exercise programs may be warranted. For policymakers, the findings argue for aligning dental benefits with geriatric care pathways. Particularly in the private system—where we observed lower baseline HGS and higher malnutrition risk—structured programs that subsidized early adjustments, nutritional screening, and brief functional assessments could yield appreciable benefits.