Discovery of a Three-Piece Inflatable Penile Prosthesis Implant During Donor Dissection: Anatomical Case Study
Abstract
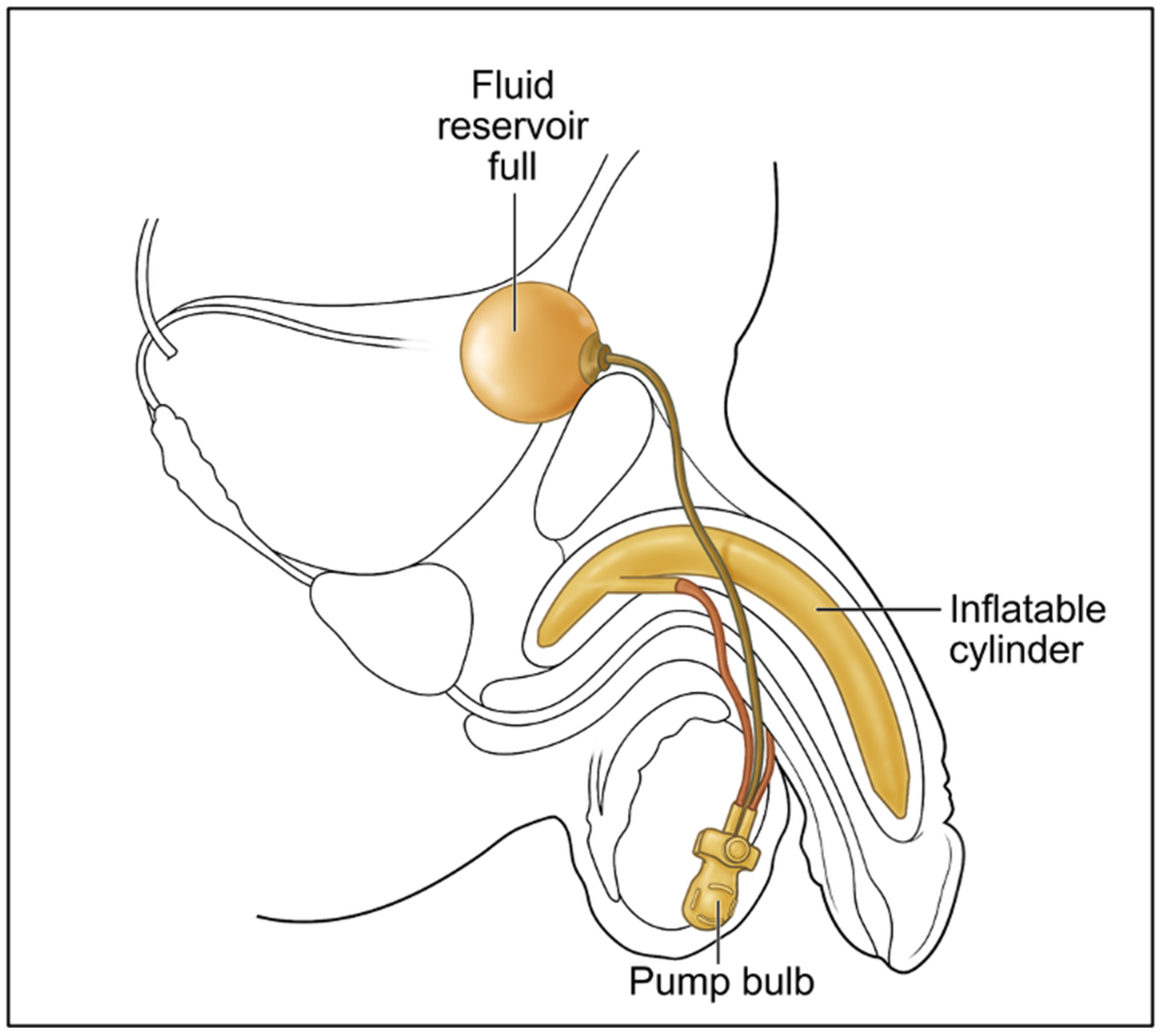
1. Introduction
2. Detailed Case Description
2.1. Donor Selection and Dissection Protocol
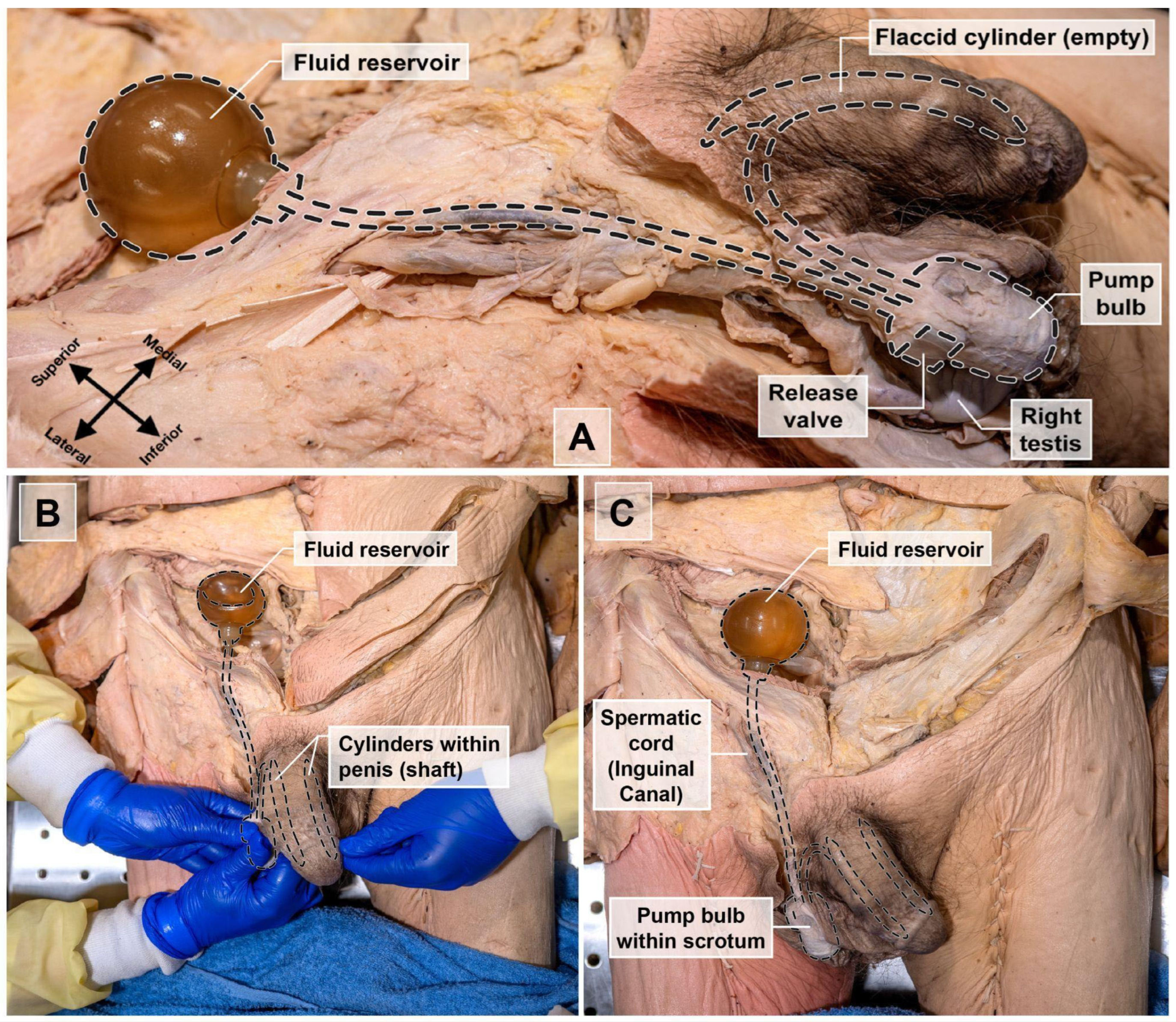
2.2. Discovery of a Penile Prosthetic Implant During Donor Dissection
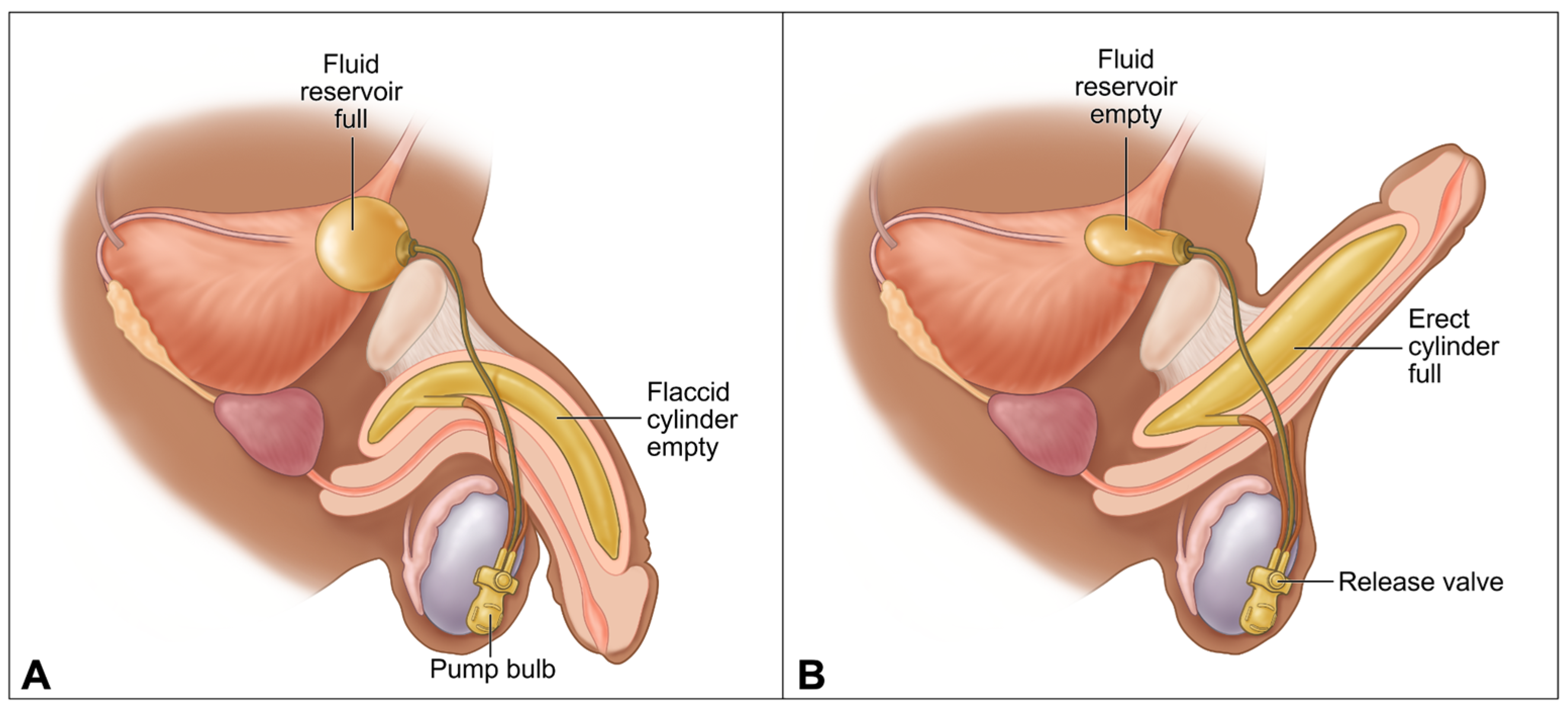
2.3. Anatomical Identification and Functional Analysis
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PPI | Penile Prosthetic Implant |
| ED | Erectile Dysfunction |
| AFCP | Anatomic Foundations of Clinical Practice |
| OUWB | Oakland University William Beaumont |
References
- Wang, C.-M.; Wu, B.-R.; Xiang, P.; Xiao, J.; Hu, X.-C. Management of male erectile dysfunction: From the past to the future. Front. Endocrinol. 2023, 14, 1148834. [Google Scholar] [CrossRef]
- Feldman, H.A.; Goldstein, I.; Hatzichristou, D.G.; Krane, R.J.; McKinlay, J.B. Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. J. Urol. 1994, 151, 54–61. [Google Scholar] [CrossRef]
- Melnik, T.; Soares, B.G.O.; Nasello, A.G. The effectiveness of psychological interventions for the treatment of erectile dysfunction: Systematic review and meta-analysis, including comparisons to sildenafil treatment, intracavernosal injection, and vacuum devices. J. Sex. Med. 2009, 5, 2562–2574. [Google Scholar] [CrossRef]
- Montorsi, P.; Montorsi, F.; Schulman, C.C. Is erectile dysfunction the "tip of the iceberg" of a systemic vascular disorder? Eur. Urol. 2003, 44, 352–354. [Google Scholar] [CrossRef]
- Krzastek, S.C.; Bopp, J.; Smith, R.P.; Kovac, J.R. Recent advances in the understanding and management of erectile dysfunction. F1000Research 2019, 8, 102. [Google Scholar] [CrossRef]
- Cakir, O.O.; Lee, W.G.; Ralph, P.; Megson, M.; Ralph, D.J. Advances in penile prosthesis surgery: A clinical update. Türk Urol. Derg./Turk. J. Urol. 2022, 48, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.; Bettocchi, C.; Egydio, P.; Love, C.; Osmonov, D.; Park, S.; Ralph, D.; Xin, Z.C.; Brock, G. The International Penile Prosthesis Implant Consensus Forum: Clinical Recommendations and surgical principles on the inflatable 3-piece penile prosthesis implant. Nat. Rev. Urol. 2022, 19, 534–546. [Google Scholar] [CrossRef] [PubMed]
- Le, B.; Burnett, A.L. Evolution of penile prosthetic devices. Korean J. Urol. 2015, 56, 179–186. [Google Scholar] [CrossRef]
- Cavayero, C.T.; Leslie, S.W.; McIntosh, G.V. Penile Prosthesis Implantation; StatPearls Publishing: St. Petersburg, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK558980/ (accessed on 7 September 2025).
- Rodriguez, K.M.; Pastuszak, A.W. A history of penile implants. Transl. Androl. Urol. 2017, 6 (Suppl. S5), S851–S857. [Google Scholar] [CrossRef]
- Baas, W.; O’Connor, B.; Welliver, C.; Stahl, P.J.; Stember, D.S.; Wilson, S.K.; Köhler, T.S. Worldwide trends in penile implantation surgery: Data from over 63,000 implants. Transl. Androl. Urol. 2020, 9, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Montague, D.K.; Angermeier, K.W. Surgical approaches for penile prosthesis implantation: Penoscrotal vs infrapubic. penile prosthesis implantation: Penoscrotal vs infrapubic. Int. J. Impot. Res. 2003, 15, S134–S136. [Google Scholar] [CrossRef] [PubMed]
- Kwan, L.; Zhao, L.C. Penoscrotal approach for inflatable penile prosthesis implantation. Asian J. Androl. 2011, 13, 711–715. [Google Scholar] [CrossRef]
- Palmisano, F.; Boeri, L.; Cristini, C.; Antonini, G.; Spinelli, M.G.; Franco, G.; Longo, F.; Gadda, F.; Colombo, F.; Montanari, E. Comparison of infrapubic vs penoscrotal approach for inflatable penile prosthesis placement: A systematic review and meta-analysis. J. Sex. Med. 2018, 15, 1712–1719. [Google Scholar] [CrossRef]
- Bertero, E.B. Infrapubic approach to penile prosthesis placement: Indications and outcomes. Urology 2015, 86, 553–557. [Google Scholar] [CrossRef]
- Park, S.H. Subcoronal inflatable penile prosthesis under local anesthesia. J. Vis. Surg. 2019, 5, 65. [Google Scholar] [CrossRef]
- Feng, C.L.; Langbo, W.A.; Anderson, L.K.; Cao, D.; Bajic, P.; Amarasekera, C.; Wang, V.; Levine, L.A. Subcoronal inflatable penile prosthesis implantation: Indications and outcomes. J. Sex. Med. 2023, 20, 888–892. [Google Scholar] [CrossRef]
- Osmonov, D.; Chomicz, A.; Tropmann-Frick, M.; Arndt, K.M.; Jünemann, K.P. High-submuscular vs. space of Retzius reservoir placement during implantation of inflatable penile implants. Int. J. Impot. Res. 2020, 32, 18–23. [Google Scholar] [CrossRef]
- Al-Enezi, A.; Al-Khadhari, S.; Al-Shaiji, T.F. Three-piece inflatable penile prosthesis: Surgical techniques and pitfalls. J. Surg. Tech. Case Rep. 2011, 3, 76–83. [Google Scholar] [CrossRef]
- Pacheco Usmayo, A.; Torregrosa Andrés, A.; Flores Méndez, J.; Luján Marco, S. Inflatable penile prosthesis (IPP): Diagnosis of complications and component imaging. Radiol./Diagn. Imaging 2021, 63, 504–510. [Google Scholar] [CrossRef]
- Otero, J.R.; Manfredi, C.; Wilson, S.K. The good, the bad, and the ugly about surgical approaches for inflatable penile prosthesis implantation. Int. J. Impot. Res. 2020, 34, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Kolb, D.A. Experiential Learning: Experience as the Source of Learning and Development; Prentice Hall: Englewood Cliffs, NJ, USA, 1984. [Google Scholar]
- Dy, G.W.; Dubin, J.M.; Morey, A.F. Penile prosthesis implantation after phalloplasty: A review of techniques and outcomes. Transl. Androl. Urol. 2019, 8, 208–215. [Google Scholar] [CrossRef]
- Krishnappa, P.; Srini, V.S.; Shah, R.; Lentz, A.C.; Garaffa, G.; Martinez-Salamanca, J.I.; Moncada, I. Cadaveric penile prosthesis workshop training improves surgical confidence levels of urologists: South Asian Society for Sexual Medicine course survey. Int. J. Urol. 2020, 27, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Khorshidi, M.A. Ex-vivo IPP implantation in cadaveric human penis with paired computational modeling. Eur. Urol. Open Sci. 2024, 67, S3. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hendricks, B.; Pakray, A.; Thomas, J.; Tomas, S.; Barremkala, M.; Gemechu, J. Discovery of a Three-Piece Inflatable Penile Prosthesis Implant During Donor Dissection: Anatomical Case Study. Prosthesis 2025, 7, 127. https://doi.org/10.3390/prosthesis7050127
Hendricks B, Pakray A, Thomas J, Tomas S, Barremkala M, Gemechu J. Discovery of a Three-Piece Inflatable Penile Prosthesis Implant During Donor Dissection: Anatomical Case Study. Prosthesis. 2025; 7(5):127. https://doi.org/10.3390/prosthesis7050127
Chicago/Turabian StyleHendricks, Bennett, Arian Pakray, Joshua Thomas, Serly Tomas, Malli Barremkala, and Jickssa Gemechu. 2025. "Discovery of a Three-Piece Inflatable Penile Prosthesis Implant During Donor Dissection: Anatomical Case Study" Prosthesis 7, no. 5: 127. https://doi.org/10.3390/prosthesis7050127
APA StyleHendricks, B., Pakray, A., Thomas, J., Tomas, S., Barremkala, M., & Gemechu, J. (2025). Discovery of a Three-Piece Inflatable Penile Prosthesis Implant During Donor Dissection: Anatomical Case Study. Prosthesis, 7(5), 127. https://doi.org/10.3390/prosthesis7050127




