Experimental Analysis of Fractured Human Bones: Brief Review and New Approaches
Abstract
1. Introduction and the State of the Art
1.1. Theoretical Approaches
1.2. Experimental Approaches
1.3. Final Remarks
2. Materials and Methods
2.1. Local Investigation Methods
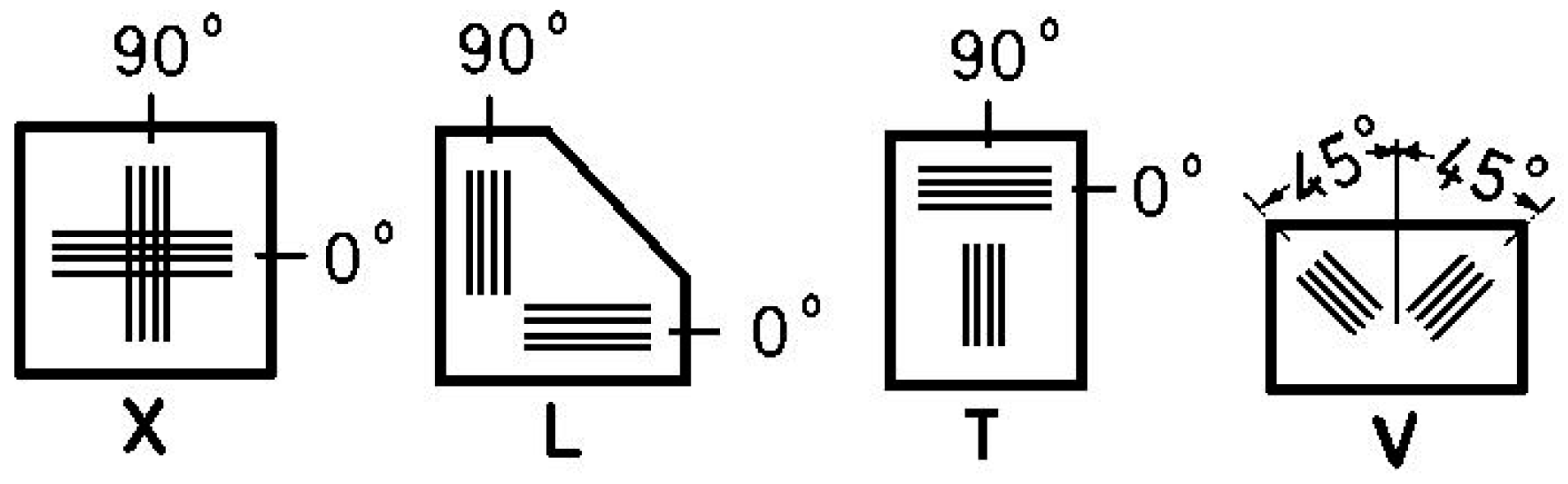
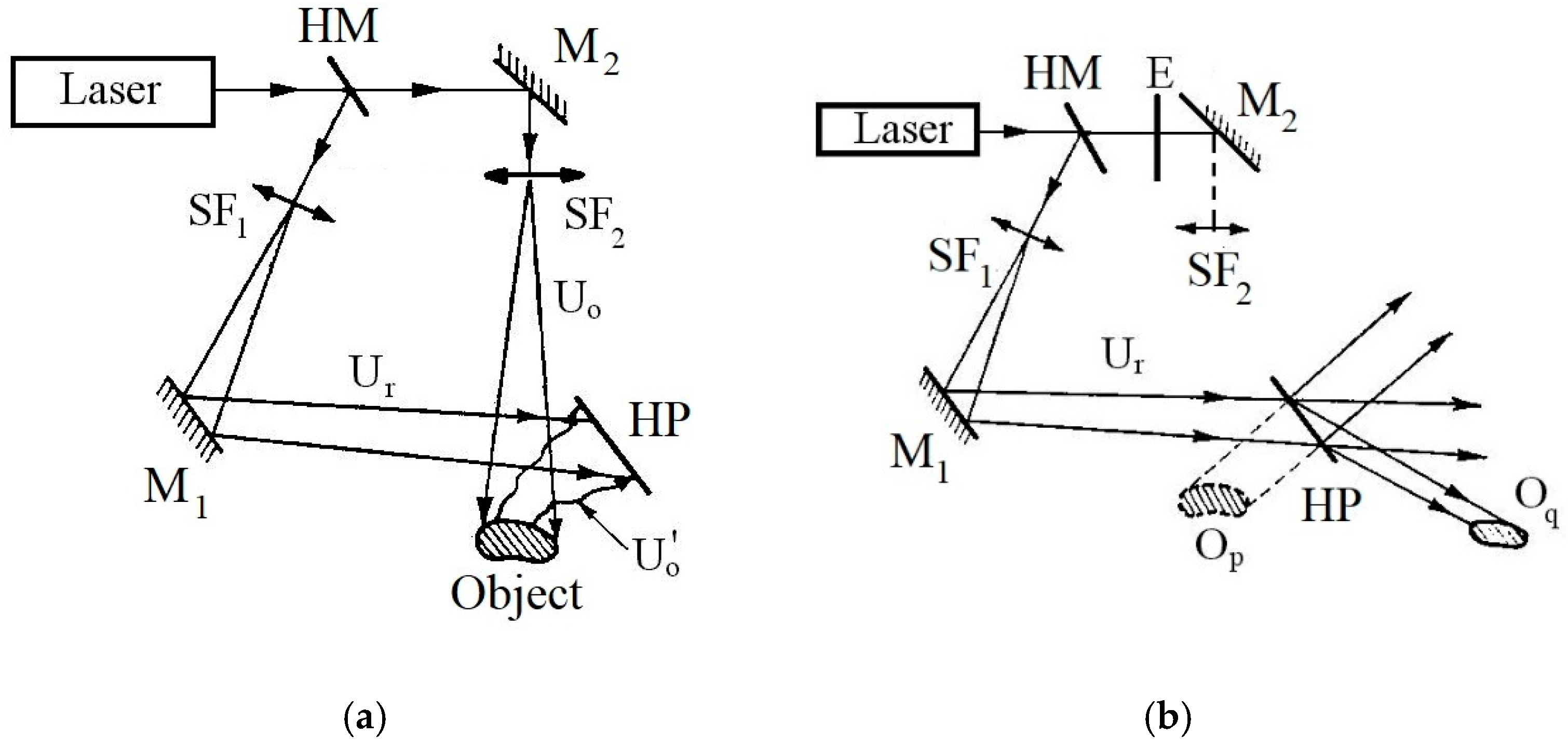
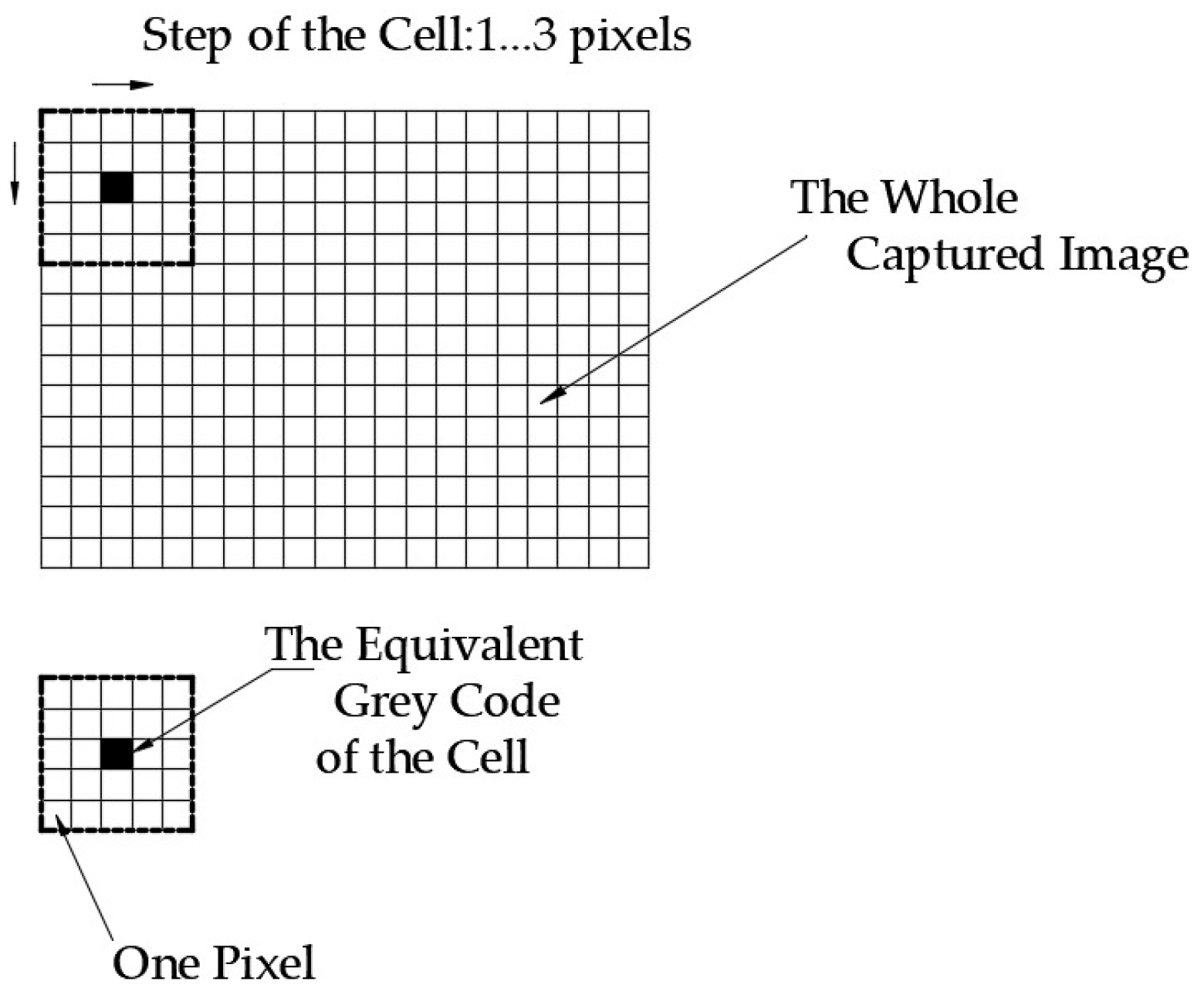
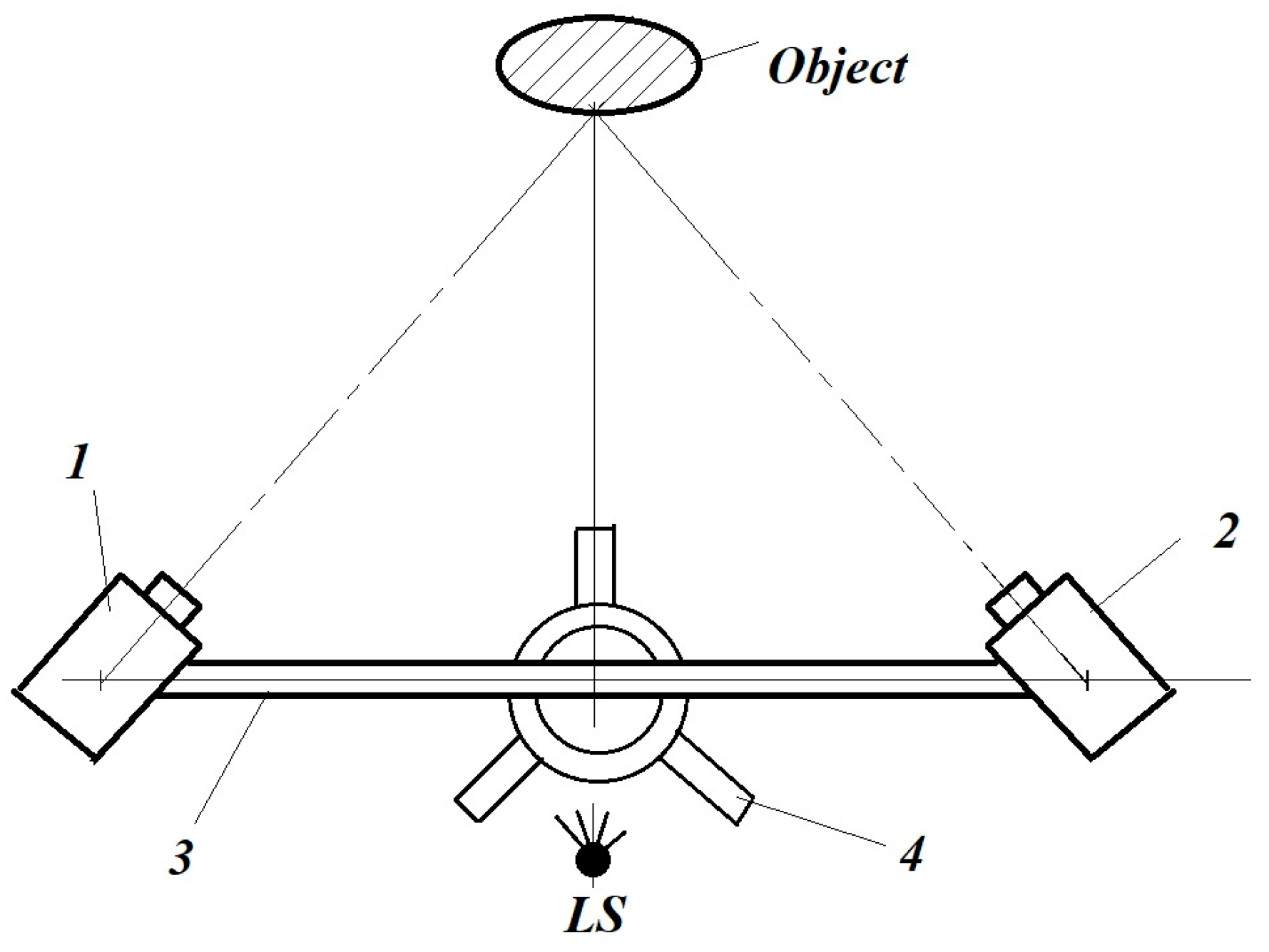
2.2. Global Investigation Methods
- It requires particularly rigorous vibration insulation of the laboratory (as it is only a laboratory method, not a field method, it cannot be applied in working/factory conditions);
- The consumables are particularly expensive, especially the HPs;
- The fringe field evaluation, with the exception of some specific optical settings, is difficult and time-consuming;
- If the common HI technique is applied, then the (3) condition offers a significant limitation.
- It is a contactless method; thus, it does not influence the analyzed phenomenon.
- It can be applied to many types of materials, including metals, wood, plastics, bones, and composites.
- It does not require expensive consumables, only some water-soluble paints (black and white), which can be easily cleaned after the experiments.
- Depending on the given optical set, it can monitor surfaces starting from some cm2 up to some m2—in the domain of 3D displacements, to several cm—with practically the same accuracy/precision.
- With the ability to apply the virtual strain gauge option, it serves as an integral substitution for ESG systems in the analysis of not only static but also quasi-dynamic and dynamic phenomena.
- As a virtual experimental method, the captured images can be reloaded and re-evaluated based on other accuracies (other subsets and step sizes, as well as other new AOIs) for smaller or larger investigation areas.
- One can define several lines and curves with the desired constitutive points, along which one can obtain the desired displacements, strains, and other useful engineering information based on several post-processing tools (given in advance or developed by the user).
- It represents a high-credibility validation tool for FEM analysis and developed models.
3. The Authors’ Own Results and Discussion
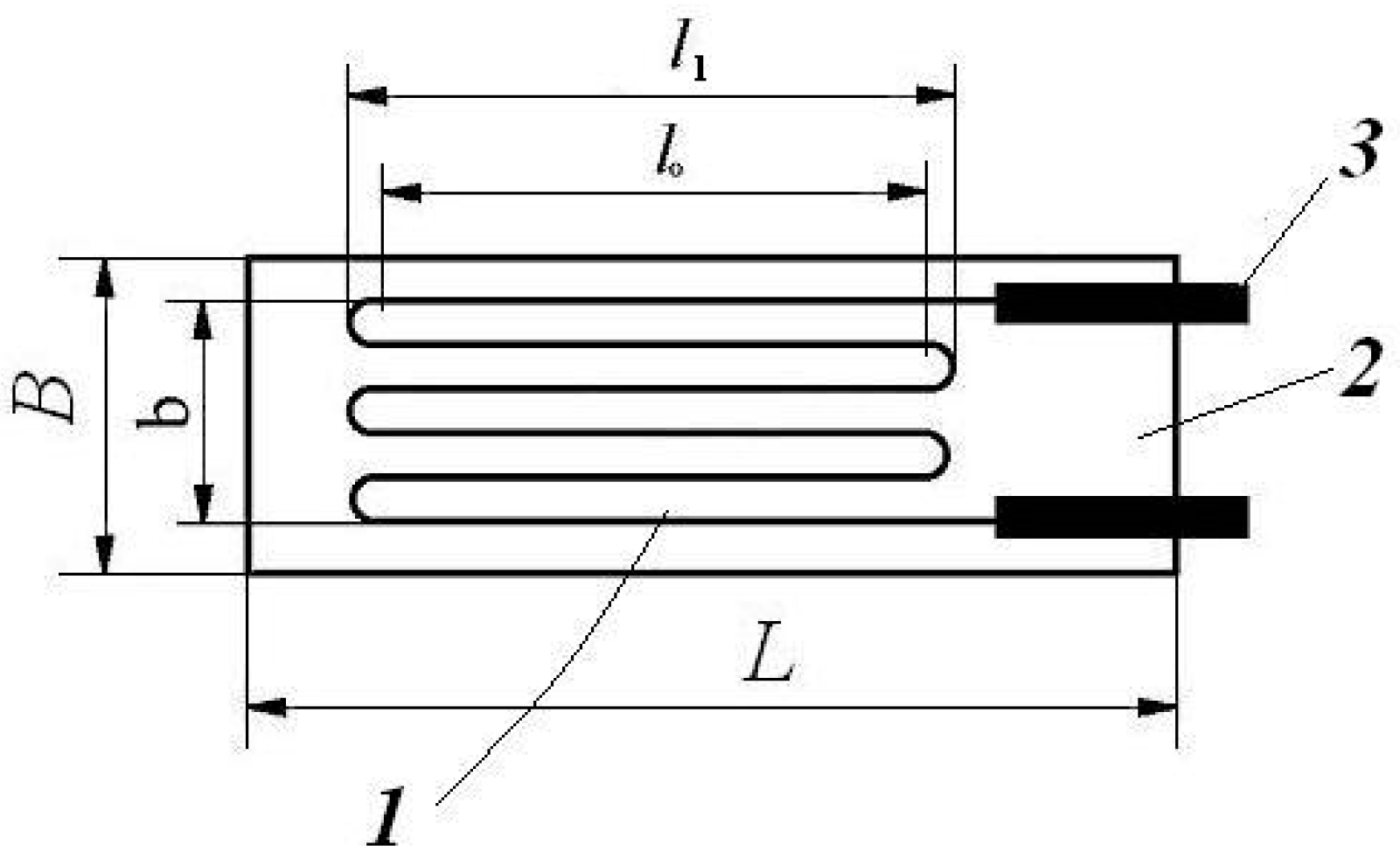
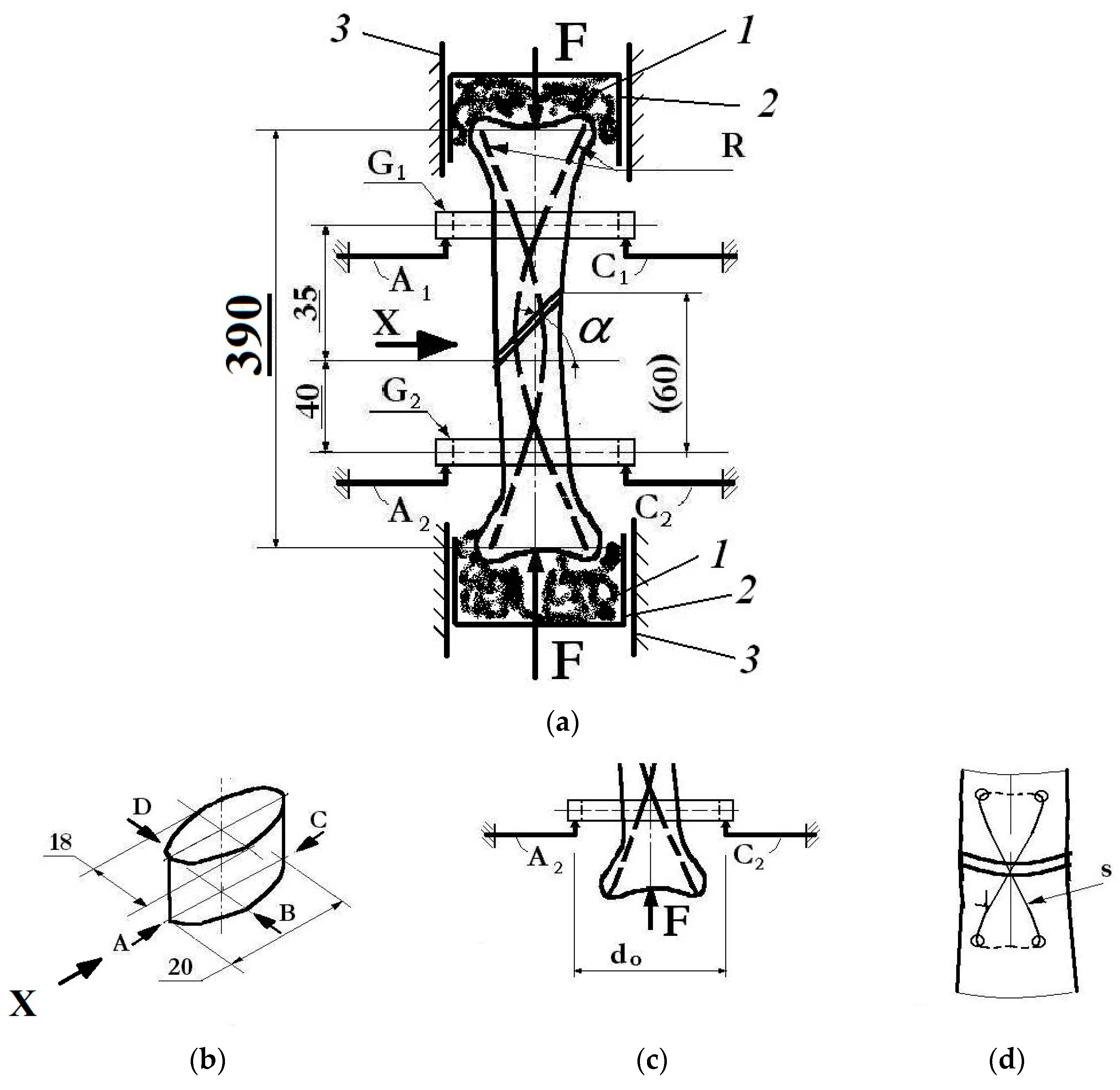
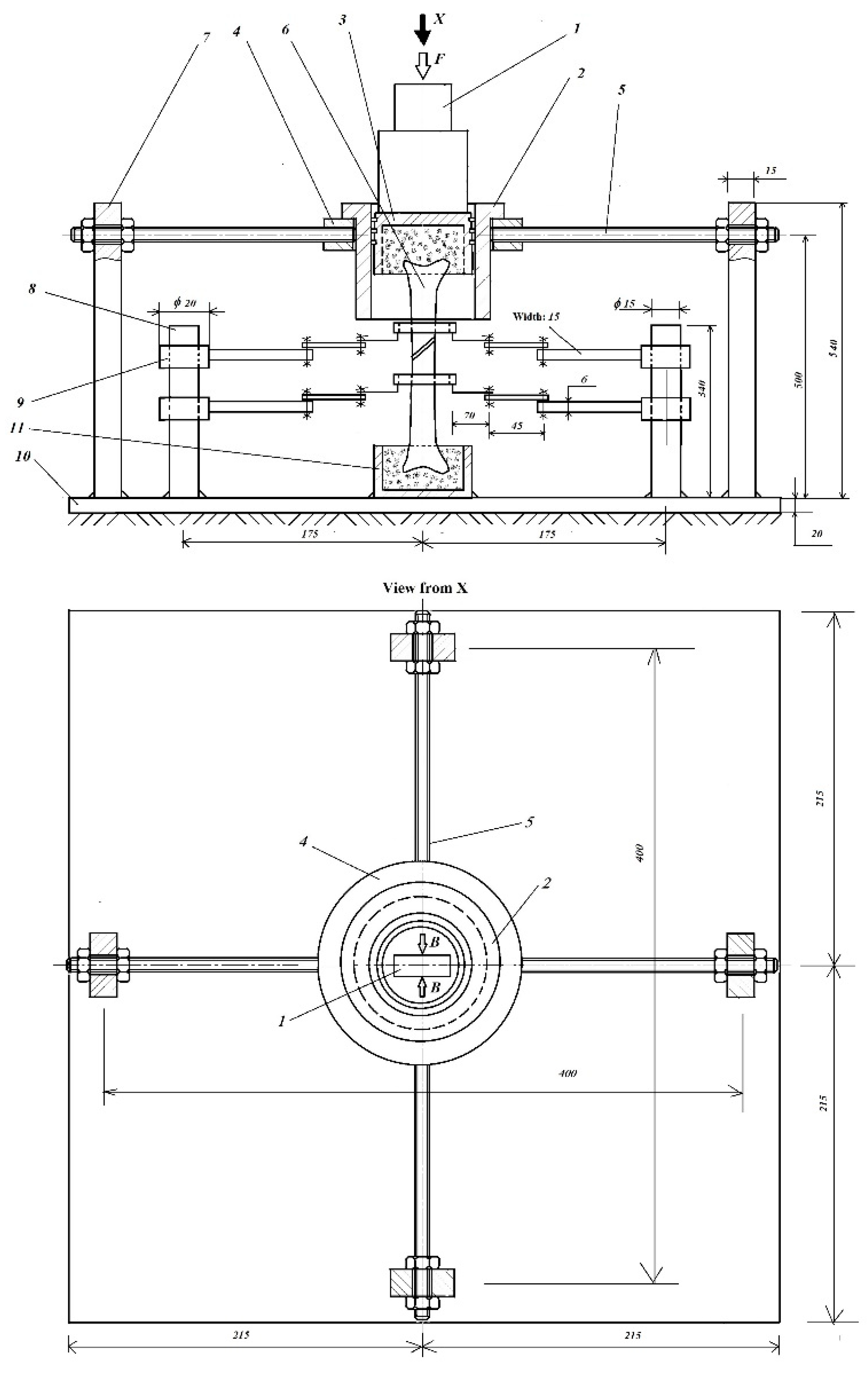
3.1. New Approaches with the ESG Technique
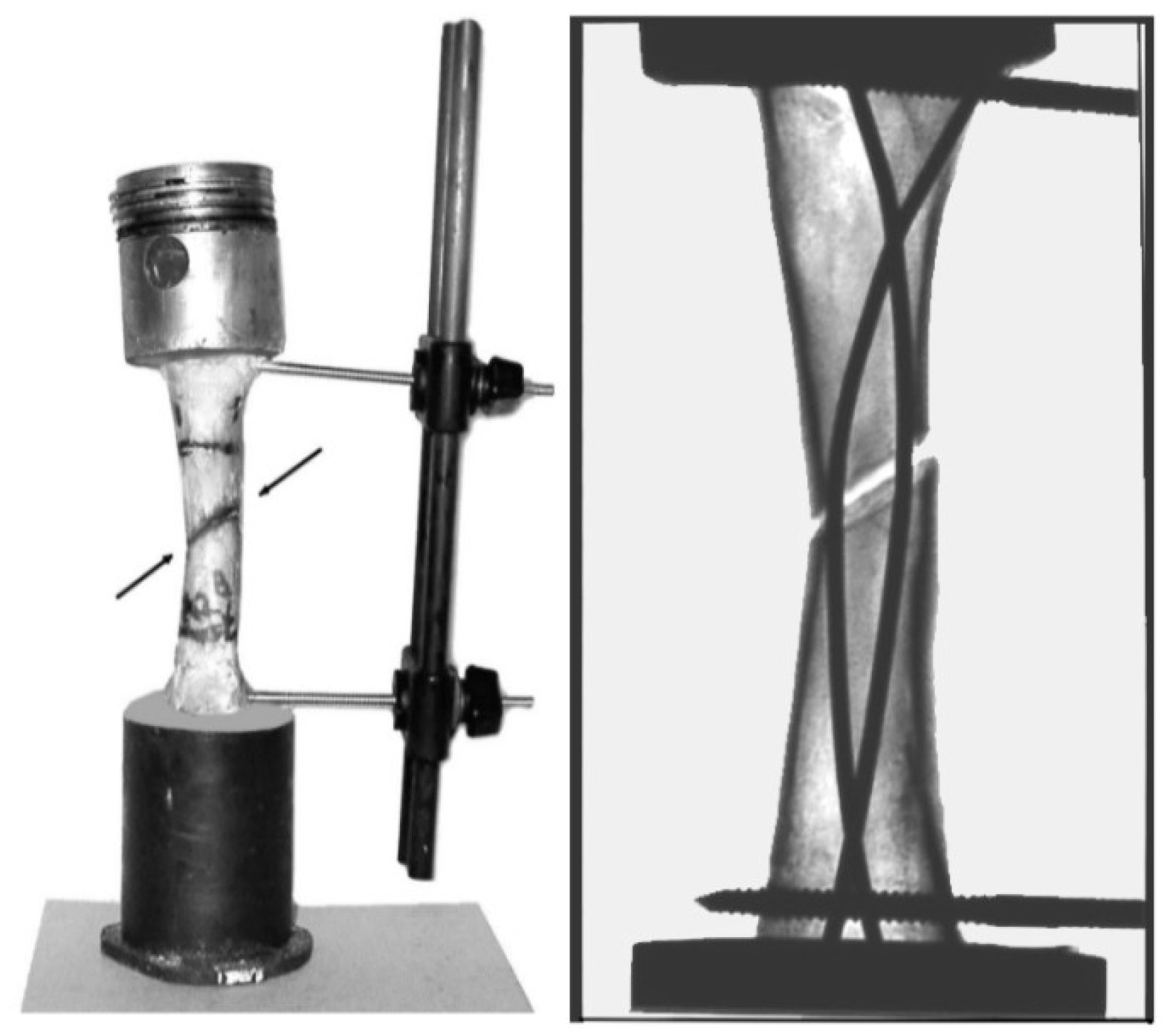
- Fixations, in the stretched area, with the help of 8-shaped thin wire loops at the level of the fracture center.
- External fixation elements.
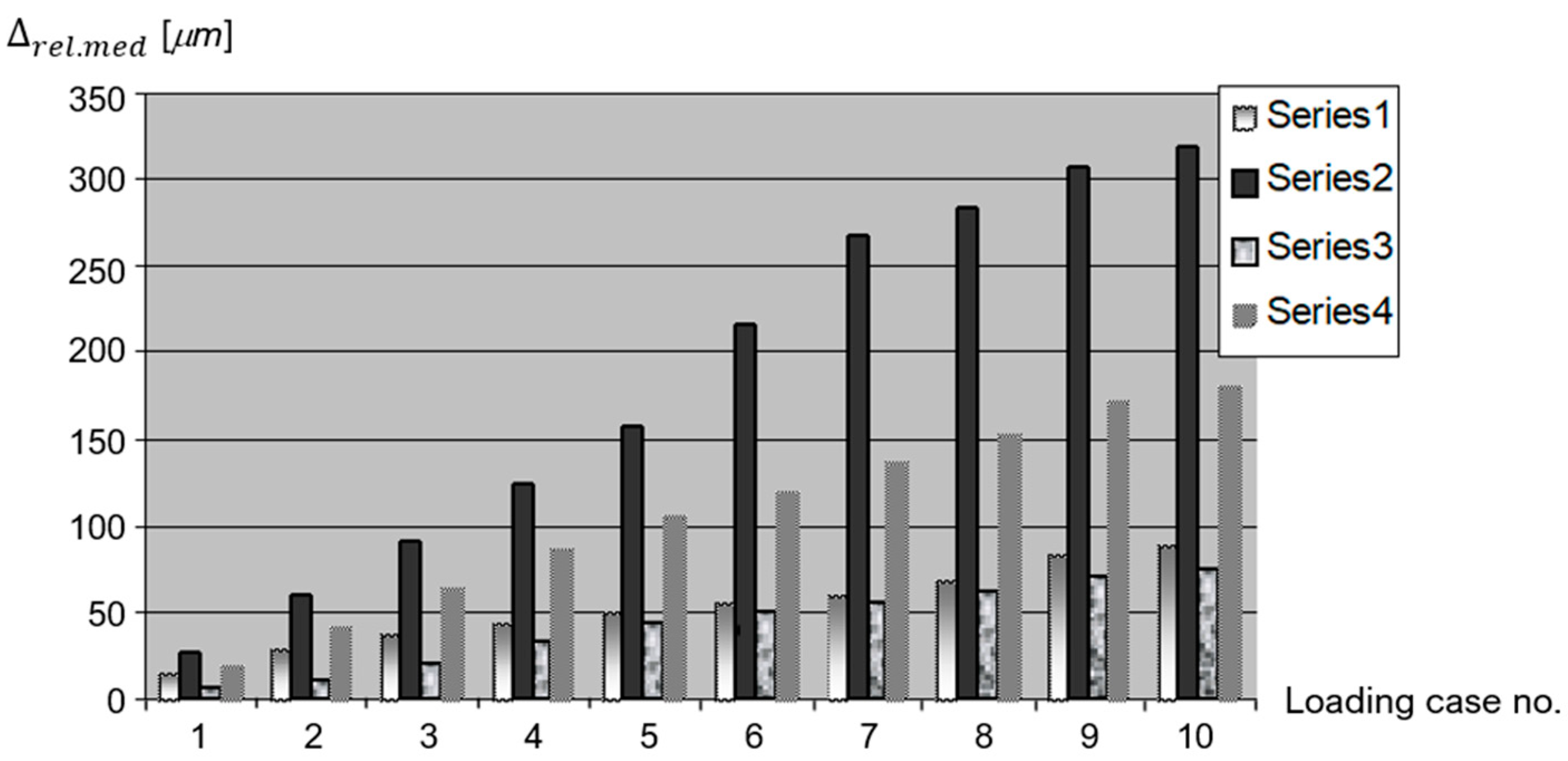
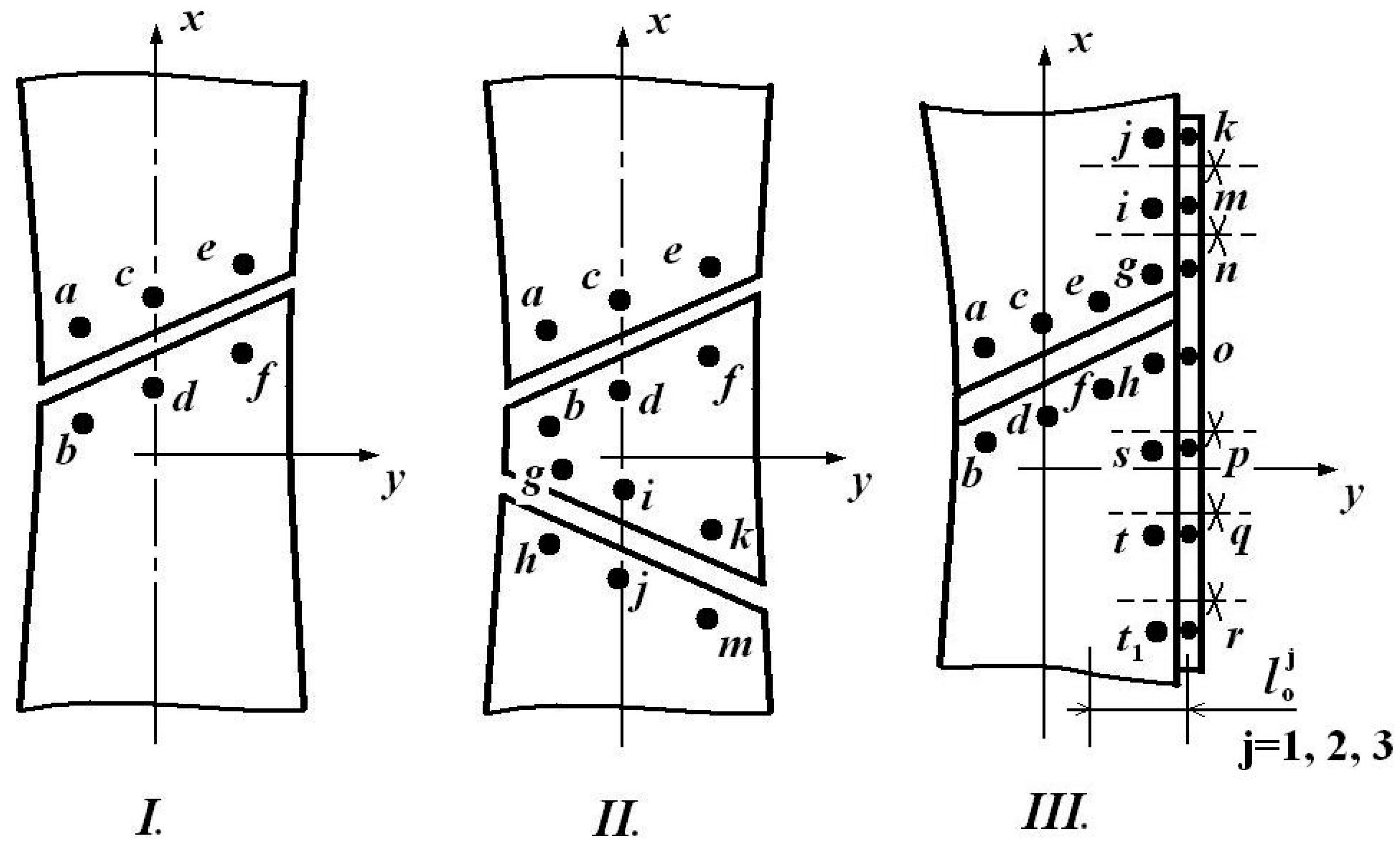
- The relative linear displacements (at the level of all pairs of lamellas) could be determined using simple relationships of the type
- The average relative displacement becomes
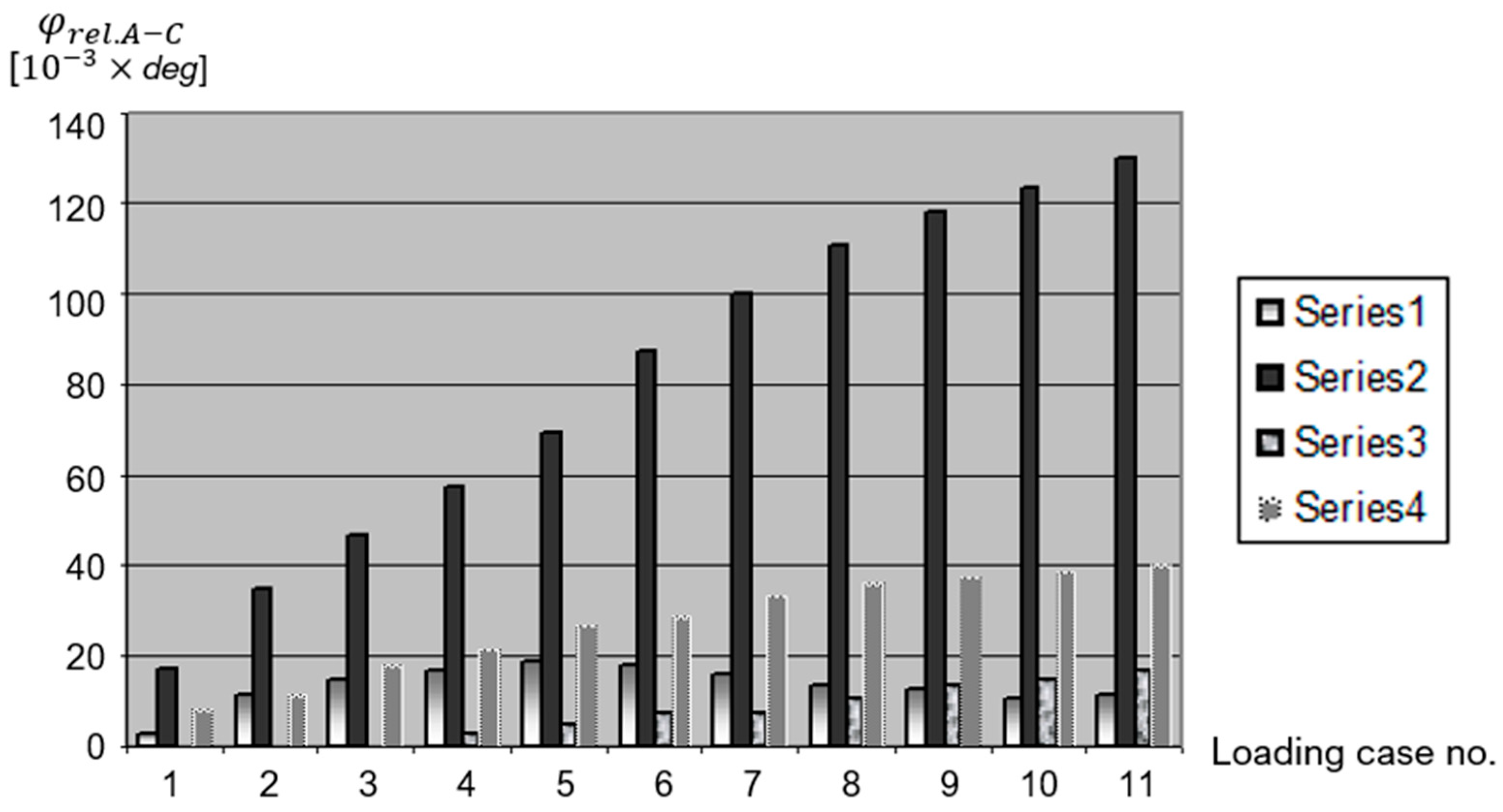
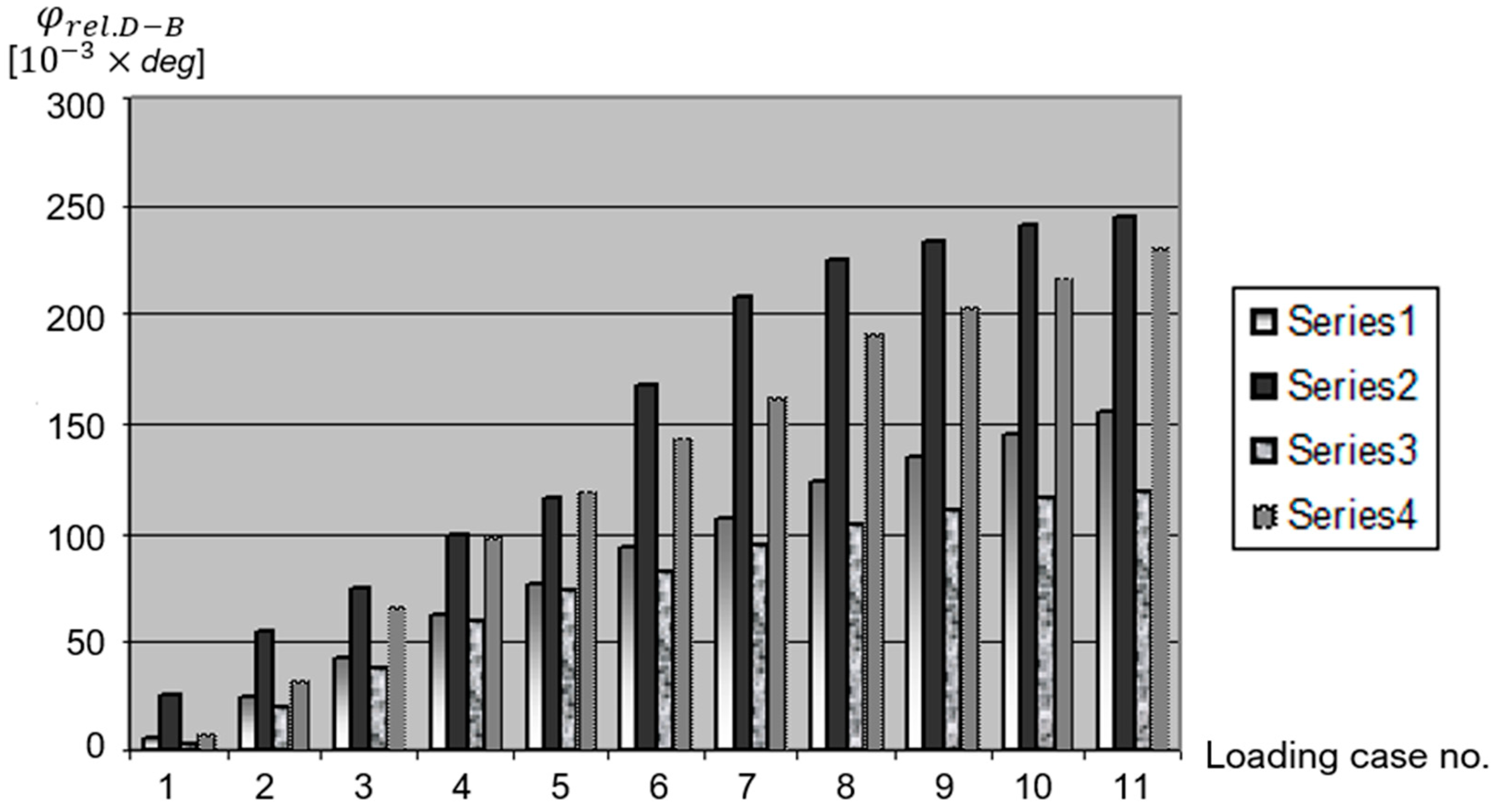
- The angular ones, that is, those with relative rotation in two orthogonal planes, correspond to the following relative linear displacements:and
- P1—intact bone, which also served as a standard in the assessment of displacements.
- P2—fracture fixation with only two elastic centro-medullary Ender nails.
- P3—fracture fixation with two elastic centro-medullary Ender nails, combined with an external one-sided external fixator.
- P4—fracture fixation with two elastic centro-medullary Ender nails, combined with an 8-shaped thin wire loop.
- This original stand and measurement strategy of the authors can serve as an efficient, highly precise, and objective tool in assessing the quality of different types of fixators for both stable and unstable fractures.
- By supplementing Ender nails with either an 8-shaped thin wire loop or an external fixator, unstable fractures will become more stable, and the healing period will be reduced due to the fact that these additional systems will also provide beneficial micro-movements for rapid healing.
- The experimental results obtained could serve as solid scientific arguments in explaining rapid healing by applying these combined elastic fixation systems.
- Using the association of a flexible fixation with “8″-shaped wiring or an external fixation causes a decrease in the movement of the fracture gap in the interval of beneficial micro-movements.
- Furthermore, the rotation in the A–C plane provides similar results for strain at the fracture site in the studied cases, while the B–D plane does not reveal significant differences.
- These experimental results, which are correlated with the clinical results, and the relative delay in forming a bone union in the patients with external fixations have an explanation in the rigidity of the fixation, which is very close to that of a normal bone.
- In addition, they conclude that adding an “8″-shaped wiring or an external fixation is a very dynamic locking. This type of fixation retains the biomechanical advantages of a flexible fixation even in unstable fractures. This way of fixation is a biological one. It has a biological advantage by protecting the bone circulation and a mechanical one by allowing movements with a beneficial amplitude.
- The average relative displacements with respect to these pairs of points, i.e.,
- The corresponding relative rotations:
- The global average displacement
- The global linear strain:
- The linear strains at the four significant points:
- The ratio between the extreme values (minimum and maximum) of the four specific linear strains:
- The ratio between the maximum and minimum values of the linear strains and the global one:
- The ratio of the two relative rotations:
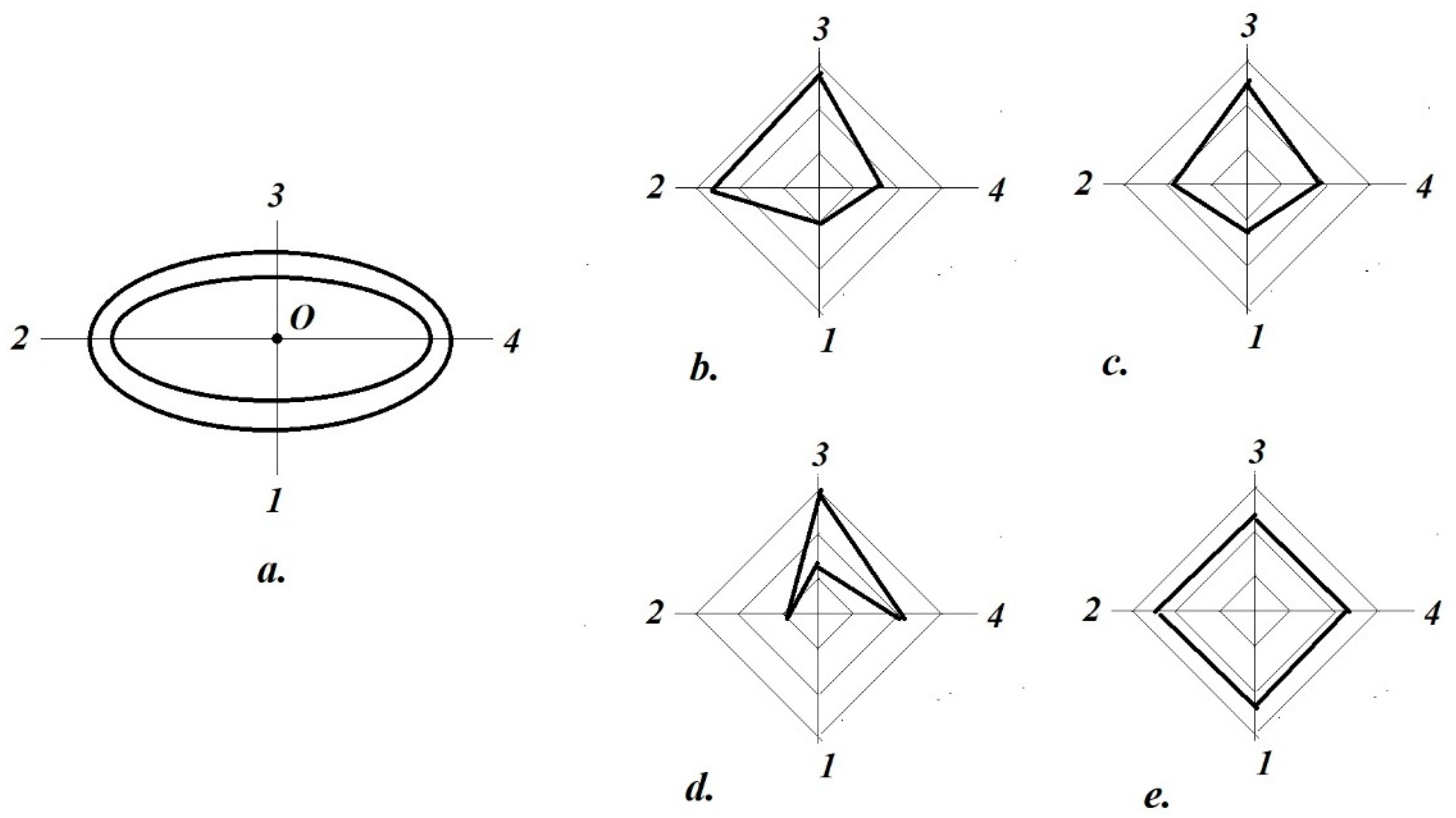
- Bending indices along
- Slip index (of tangential instability):
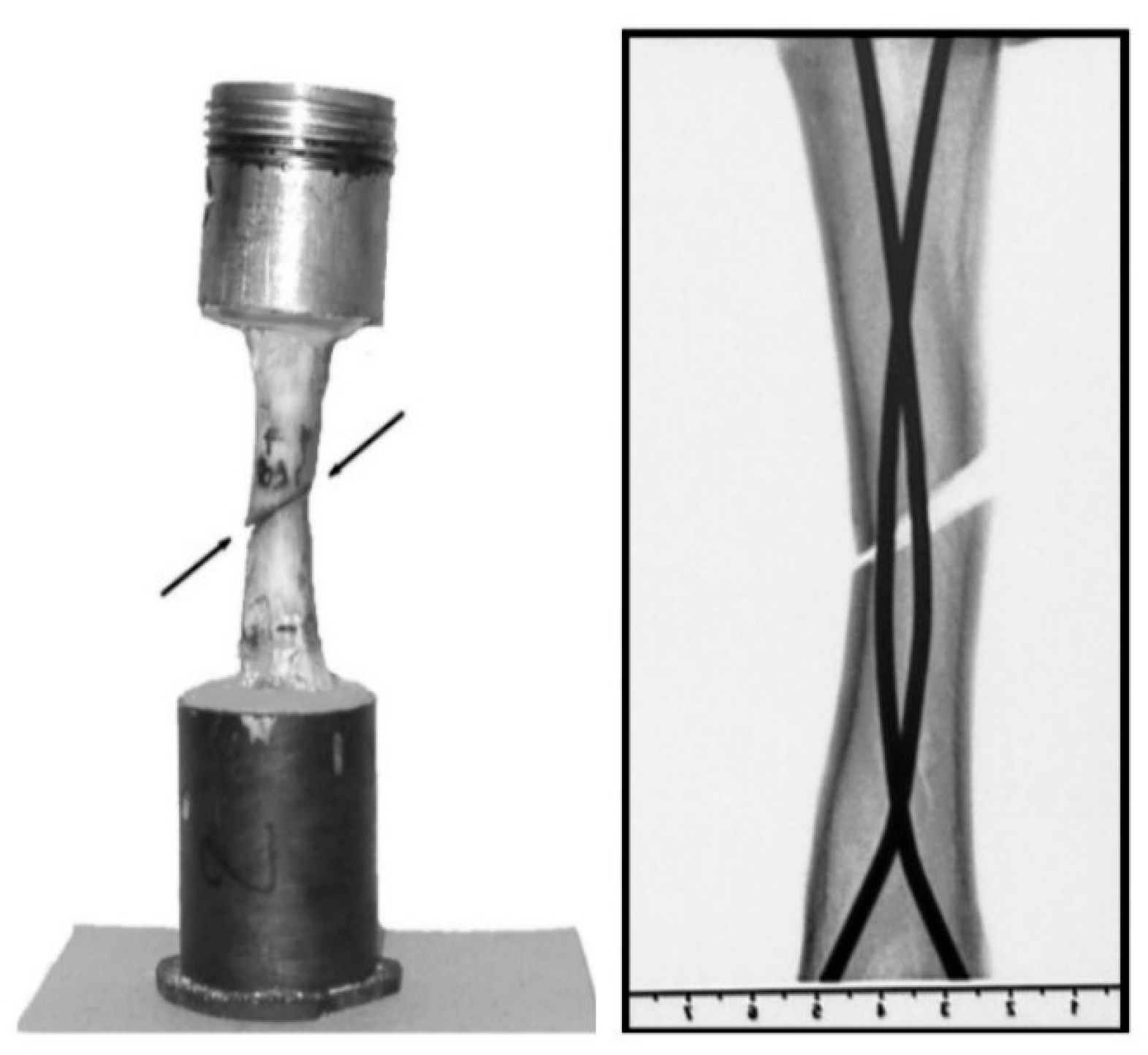
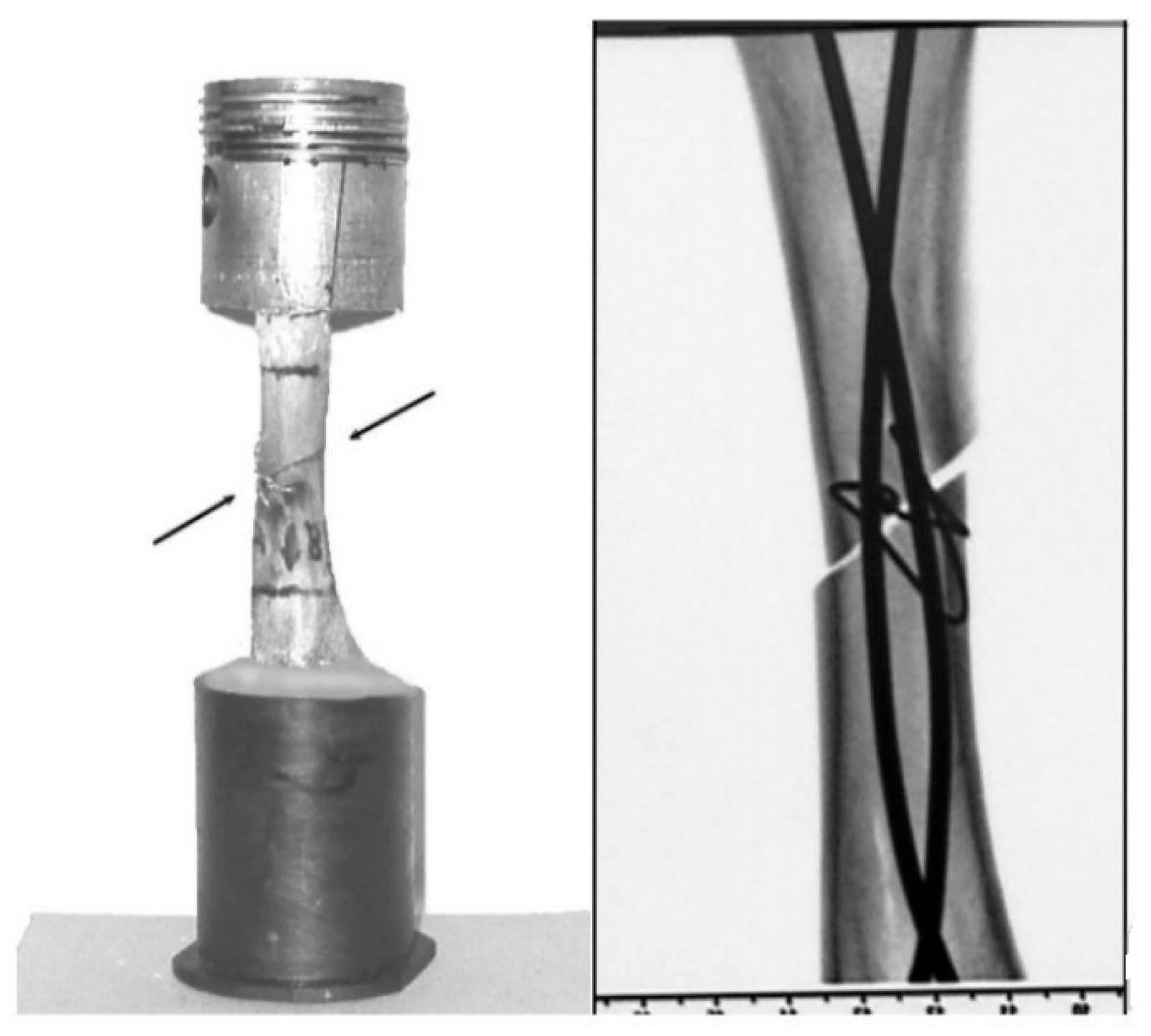
3.2. New Approaches to the DIC/VIC Technique
4. Critical Analysis of the Described ESG Test Bench
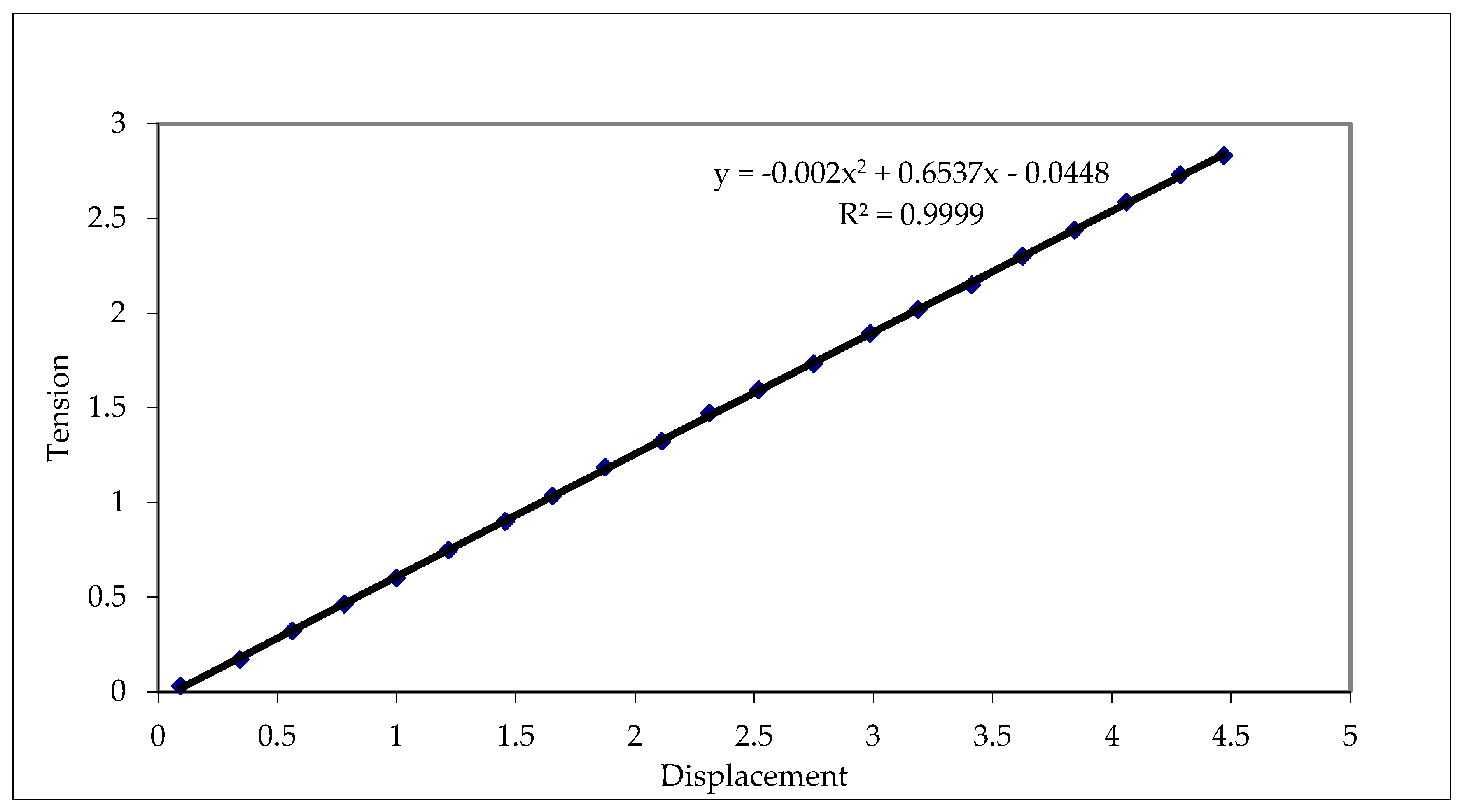
- It is strongly linear (the second-order and zero terms are negligible compared with the first-order terms).
- It has a high confidence/confidentiality coefficient of
- It has a good sensitivity, i.e., the indication of 1 mV corresponds to a displacement of 1.67
5. Conclusions and Perspective
- Their original ESG test benches, assisted by a high-precision data acquisition system (e.g., National Instruments with 32 channels), allow the development of a new strategy for objectively comparing the efficiency of different types of bone fixation (femoral or tibial fixation), especially in the case of unstable fractures.
- In the authors’ opinion, their protocol, together with the obtained measurement results, will open new opportunities for biomechanics specialists, as well as for orthopedic doctors, to find optimal and personalized solutions for the fixation of fractured parts, as well as to provide surgeons with solid biomechanical arguments for the clinical effectiveness of the chosen fixators.
- The proposed set of evaluation parameters, including the polar diagram intended for evaluating and comparing the linear displacements of the tested fixators, may represent an efficient and objective tool for evaluating the stability and effectiveness of a chosen fixator in the future.
- The implementation of the VIC-3D optical system in the evaluation of micro-displacements (both in the immediate area of external fixation plates with human bone and inter-fragmentary ones) will provide new opportunities to approach the surgical act.
- The combination of these two approaches (ESG test benches and VIC-3D) will allow the development of a modern, unified, and original methodology for the most efficient quantitative and qualitative analysis of types of fixators.
- Given the data acquisition facilities offered by this ESG and VID-3D testing system, their combination will ensure high accuracy and the desired loading speed (which can even be variable, if necessary, to simulate the effect of walking/using a particular limb); through these facilities, it will become a useful and comparatively particularly effective tool for performance evaluation.
- Among the authors’ future goals is the development and validation of a more flexible and personalized fixation solution in cooperation with surgeons.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Horta, J.; Riverab, A.L.; De La Islaa, A.; Oskamb, A.; Victor, M.; Castanob, V.M. Fracture of Femur: Simulation and Photo-elasticity Analysis. Dig. J. Nanomater. Biostruct. 2013, 8, 177–185. [Google Scholar]
- Horta-Rangel, J.; Riviera, A.L.; Castano, V.M. Modal behavior of bones during fracture, Computer Methods in Biomechanics and Biomedical Engineering. Comput. Methods Biomech. Biomed. Eng. 2010, 13, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Melchionda, R.; Scalise, L. Dynamic Characterization of a Human Tibia Including Soft Tissues: Experimental and Numerical Analysis. Master’s Thesis, Polytechnic University of Marche, Ancona, Italy, 2019. [Google Scholar]
- Perren, S.M. Evolution of the internal fixation of long bone fractures: The scientific basis of biological internal fixation: Choosing a new balance between stability and biology. J. Bone Jt. Surg. Br. 2002, 84, 1093–1110. [Google Scholar] [CrossRef]
- Müller, M.E.; Allgöwer, M.; Schneider, R.; Willenegger, H.; Perren, S.M. Manual of Internal Fixation, 3rd ed.; Springer: Berlin/Heidelberg, Germany, 1995; pp. 4–95. ISBN 978-3-540-55297-0. [Google Scholar]
- Perren, S.M. Physical and biological aspects of fracture healing with special reference to internal fixation. Clin. Orthop. Relat. Res. 1979, 138, 175–196. [Google Scholar] [PubMed]
- Perren, S.M.; Cordey, J. The Concept of Inter-Fragmentary Strain, in Current Concepts of Internal Fixation of Fractures; Springer: Berlin/Heidelberg, Germany, 1980; pp. 63–77. [Google Scholar]
- Necula, R.D.; Panait, G.h.; Száva, I.; Şamotă, I. Evaluation of Micro-movement in the biomechanical context of bone shaft fracture healing in elastic versus rigid fixations. Ann. Acad. Rom. Sci. 2011, 2, 65–78. [Google Scholar]
- Kenwright, J.; Goodship, A.E. Controlled Mechanical Stimulation in the Treatment of Tibial Fractures. Clin. Orthop. 1989, 241, 36–47. [Google Scholar] [CrossRef]
- Inacio, J.V.; Schwarzenberg, P.; Kantzos, A.; Malige, A.; Nwachuku, C.O.; Dailey, H.L. Rethinking the 10% strain rule in fracture healing: A distal femur fracture case series. J. Orthop. Res. 2023, 41, 1049–1059. [Google Scholar] [CrossRef]
- Coquim, J.; Clemenzi, J.; Salahi, M.; Sherif, A.; Avval, P.T.; Shah, S.; Schemitsch, E.H.; Bagheri, Z.S.; Bougherara, H.; Zdero, R. Biomechanical Analysis Using FEA and Experiments of Metal Plate and Bone Strut Repair of a Femur Midshaft Segmental Defect. BioMed Res. Int. J. 2018, 2018, 4650308. [Google Scholar] [CrossRef]
- Moazen, M.; Mak, J.H.; Etchels, L.W.; Jin, Z.; Wilcox, R.K.; Jones, A.C.; Tsiridis, E. Periprosthetic femoral fracture—A biomechanical comparison between Vancouver type B1 and B2 fixation methods. J. Arthroplast. 2014, 29, 3. [Google Scholar] [CrossRef]
- Moazen, M.; Jones, A.C.; Leonidou, A.; Jin, Z.; Wilcox, R.K.; Tsiridis, E. Rigid versus flexible plate fixation for periprosthetic femoral fracture-Computer modelling of a clinical case. Med. Eng. Phys. 2012, 34, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Moazen, M.; Leonidou, A.; Pagkalos, J.; Marghoub, A.; Fagan, M.J.; Tsiridis, E. Application of far cortical locking technology in periprosthetic femoral fracture fixation: A biomechanical study. J. Arthroplast. 2016, 31, 1849–1856. [Google Scholar] [CrossRef]
- Geier, A.; Kebbach, M.; Soodmand, E.; Woernle, C.; Kluess, D.; Bader, R. Neuro-musculoskeletal flexible multibody simulation yields a framework for efficient bone failure risk assessment. Sci. Rep. 2019, 9, 6928. [Google Scholar] [CrossRef]
- Son, D.S.; Mehboob, H.; Chang, S.H. Simulation of the bone healing process of fractured long bones applied with a composite bone plate with consideration of the blood vessel growth. Compos. Part B Eng. 2014, 58, 443–450. [Google Scholar] [CrossRef]
- Mishra, N.R.; Singh, K.M.; Kumar, V. Biomechanical Analysis of Human Femur using Finite Element Method: A Review Study. Mater. Today Proc. 2022, 56, 384–389. [Google Scholar] [CrossRef]
- Sawbones. Vashon, WA, USA. Available online: https://www.sawbones.com/ (accessed on 20 December 2024).
- Lindsey, R.W.; Gugala, Z.; Milne, E.; Sun, M.; Gannon, F.H.; Latta, L.L. The efficacy of cylindrical titanium mesh cage for the reconstruction of a critical-size canine segmental femoral diaphyseal defect. J. Orthop. Res. 2006, 24, 1438–1453. [Google Scholar] [CrossRef] [PubMed]
- Wieding, J.; Souffrant, R.; Mittelmeier, W.; Bader, R. Finite element analysis on the biomechanical stability of open porous titanium scaffolds for large segmental bone defects under physiological load conditions. Med. Eng. Phys. 2013, 35, 422–432. [Google Scholar] [CrossRef]
- Talbot, M.; Zdero, R.; Garneau, D.; Cole, P.A.; Schemitsch, E.H. Fixation of long bone segmental defects: A biomechanical study. Injury 2008, 39, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Juszczyk, M.M.; Cristofolini, L.; Viceconti, M. The human proximal femur behaves linearly elastic up to failure under physiological loading conditions. J. Biomech. 2011, 44, 2259–2266. [Google Scholar] [CrossRef]
- Kress, T.A.; Porta, D.J.; Snider, J.N.; Fuller, P.M.; Psihogios, J.P.; Heck, W.L.; Frick, S.J.; Wasserman, J.F. Fracture patterns of human cadaver long bones. Proc. IRCOBI 1995, 23, 155–169. [Google Scholar]
- Shiling Zhang, S.; Patel, D.; Brady, M.; Gambill, S.; Theivendran, K.; Deshmukh, S.; Leslie, L.J. Experimental testing of fracture fixation plates: A review. Proc IMechE Part H J. Eng. Med. 2022, 236, 1253–1272. [Google Scholar] [CrossRef]
- Weerasooriya, T.; Sanborn, B.; Gunnarsson, A.C.; Foster, M. Orientation Dependent Compressive Response of Human Femoral Cortical Bone as a Function of Strain Rate. J. Dyn. Behav. Mater. 2016, 2, 74–90. [Google Scholar] [CrossRef]
- Babhulkar, S.S.; Pande, K.; Babhulkar, S. Nonunion of the diaphysis of long bones. Clin. Orthop. Relat. Res. 2005, 431, 50–56. [Google Scholar] [CrossRef]
- Dao, K.D.; McGuire, M.H.; Crosby, L.A. Treatment of humeral diaphyseal nonunion using fibular allograft and compression plating. Neb. Med. J. 1994, 79, 300–302. [Google Scholar]
- Wang, J.W.; Weng, L.H. Treatment of distal femoral nonunion with internal fixation, cortical allograft struts, and autogenous bone-grafting. J. Bone Jt. Surg. 2003, 85, 436–440. [Google Scholar] [CrossRef]
- Ebrahimi, H.; Rabinovich, M.; Vuleta, V.; Zalcman, D.; Shah, S.; Dubov, A.; Roy, K.; Siddiqui, F.S.; Schemitsch, E.H.; Bougherara, H.; et al. Biomechanical properties of an intact, injured, repaired, and healed femur: An experimental and computational study. J. Mech. Behav. Biomed. Mater. 2012, 16, 121–135. [Google Scholar] [CrossRef]
- Bougherara, H.; Zdero, R.; Miric, M.; Shah, S.; Hardisty, M.; Zalzal, P.; Schemitsch, E.H. The biomechanics of the T2 femoral nailing system: A comparison of synthetic femurs with finite element analysis. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2009, 223, 3. [Google Scholar] [CrossRef] [PubMed]
- Zdero, R.; Olsen, M.; Bougherara, H.; Schemitsch, E.H. Cancellous bone screw purchase: A comparison of synthetic femurs, human femurs, and finite element analysis. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2008, 222, 8. [Google Scholar] [CrossRef] [PubMed]
- Papini, M.; Zdero, R.; Schemitsch, E.H.; Zalzal, P. The biomechanics of human femurs in axial and torsional loading: Comparison of finite element analysis, human cadaveric femurs, and synthetic femurs. J. Biomech. Eng. 2007, 129, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Zdero, R.; Aziz, M.S.R.; Nicayenzi, B.; Zdero, R. Quasi-static stiffness and strength testing of whole bones and implants. In Experimental Methods in Orthopaedic Biomechanics; Elsevier: New York, NY, USA; Academic Press: Cambridge, MA, USA, 2017; pp. 19–32. ISBN 978-0-12-803855-0. [Google Scholar]
- Zdero, R. Experimental Methods in Orthopaedic Biomechanics; Elsevier: New York, NY, USA; Academic Press: Cambridge, MA, USA, 2016; ISBN 978-0-12-803802-4. [Google Scholar]
- Drugus, D.; Necula, R.; Repanovici, A.; Azoicai, D.; Rogozea, L. Degree of Patient Satisfaction with Health Care Performance Assesed by Marketing Surveys. Med.-Surg. J.-Rev. Med.-Chir. 2015, 119, 221–225. [Google Scholar]
- Druga, C.; Necula, R.; Cotoros, D.; Miclaus, R.; Repanovici, A.; Nica, S.A. Experimental Research Regarding the Thermomechanical Behaviour of PMMA During Recovery of Patients with Joint Replacements. Plast. Mater. 2017, 54, 645–647. [Google Scholar] [CrossRef]
- Hendry, A.W. Elements of Experimental Stress Analysis; Pergamon Press: Oxford, UK, 1977. [Google Scholar]
- Hoffmann, K. An Introduction to Measurements, Using Strain Gauges; HBM GmbH Publisher: Darmstadt, Germany, 1989. [Google Scholar]
- Khan, A.; Wang, X. Strain Measurements and Stress Analysis; Prentice-Hall, Inc.: Upper Saddle River, NJ, USA, 2001. [Google Scholar]
- Kobayashi, A.S. Handbook of Experimental Mechanics; Prentice Hall: Upper Saddle River, NJ, USA, 1987. [Google Scholar]
- Rohrbach, C.h. Handbuch Für Experimentelle Spanungsanalyse; VDI-Verlag GmbH: Düsseldorf, Germany, 1989. [Google Scholar]
- Száva, I.; Šejnoha, M.; Kormaníková, E.; Vlase, S.; Piovar, S.; Kotrasova, K.; Sejnoha, M.; Vorel, J.; Marsalkova, M.; Grippon, E. Classical and modern experimental investigation methods. In Mechanics of Composite Materials III; DERC Publishing House: Tweksbury, MA, USA, 2013; Chapter 1; pp. 1–64. ISBN 978-1-939757-01-2. [Google Scholar]
- Thamm, F.; Ludvig, G.y.; Huszár, I.; Szántó, I. Dehnungsmessverfahren; Akadémia Kiadó: Budapest, Hungary, 1971. [Google Scholar]
- Durelli, A.J.; Parks, V.J. Moiré Analysis of Strain; Prentice Hall: Upper Saddle River, NJ, USA, 1970. [Google Scholar]
- Post, D.; Han, B.; Ifjú, P. High Sensitivity Moiré: Experimental Analysis for Mechanics and Materials; Springer: Berlin/Heidelberg, Germany, 2005. [Google Scholar]
- Theocaris, S.P. Moiré Fringes in Strain Analysis; Pergamon Pres: Oxford, UK, 1969. [Google Scholar]
- LF/Z-2 Reflexion Polariscope Instruction Manual; Vishay Measurements Group, Inc.: Malvern, PA, USA, 2008.
- Introduction to Stress Analysis by the Photostress Method. Technical Notes Tn-702 and Tn-702-1; Vishay Measurements Group, Inc.: Malvern, PA, USA, 1989.
- Student Manual on the Photo-Elastic Coating Technique. Bull. 315-A; Vishay Measurements Group, Inc.: Malvern, PA, USA, 1984.
- Jones, R.; Wykes, C. Holographic and Speckle Interferometry, a Discussion of the Theory, Practice and Application of the Techniques; Cambridge University Press: Cambridge, UK, 1983. [Google Scholar]
- Vest, C.M. Holographic Interferometry; John Wiley & Sons: New York, NY, USA, 1979. [Google Scholar]
- Száva, I.; Ciofoaia, V.; Botiş, M.; Dogaru, F.; Ciofoaia, V.V.; Csont, E. On the Human Bones Behaviors Analysis in the Loading and Unloading state by FEM and Holographic Interferometry, the 3rd Symposium on Orthopaedic and Prosthetic Engineering, IOP-2001, 25–27.06.2001, Bialystok, Poland. Acta Bioeng. Biomech. 2001, 3 (Suppl. S1), 231–238. [Google Scholar]
- Száva, I.; Ciofoaia, V.; Şamotă, I.; Ciofoaia, V. Analysis of the tension/strain—Stress state of the human femur during the healing process. In Proceedings of the 4th Polish Scientific Conference “Biomechanics’99”, Wroclaw, Poland, 8–11 September 1999; pp. 473–476, ISBN 83-7085-433-8. [Google Scholar]
- Száva, I.; Şamotă, I.; Ciofoaia, V.; Georgescu, L.; Chalapco, V.; Muntean, G. The Holographic Investigation of the Intact and Oblique Fractured Bones; the Effect of the Excentrical Fixation. In Proceedings of the 15th “Danubia-Adria” Symposium on Experimental Methods in Solid Mechanics, Bertinoro, Italy, 30 September–3 October 1998; pp. 159–160, ISBN 953-96243-1-2. [Google Scholar]
- User Manual and Service Instructions SE3 Shearography/Espi-System; Isi-Sys Gmbh: Kassel, Germany, 2009.
- Sutton, A.M.; Orteu, J.J.; Schreier, W.H. Image Correlation for Shape, Motion and Deformation Measurements; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- VIC-3D 2010, Testing Guide; Correlated Solutions & Isi-Sys Gmbh: Irmo, SC, USA; Kassel, Germany, 2010.
- VIC-3D 2010, Reference Manual; Correlated Solutions & Isi-Sys Gmbh: Irmo, SC, USA; Kassel, Germany, 2010.
- Száva, I.; Şamotă, I.; Necula, R.D.; Hollanda, D.; Dani, P. Electrotensometrical Investigation of The Fractured Long Bones Large Displacements. Russ. J. Biomech. 2004, 8, 83–88. [Google Scholar]
- Necula, R.D.; Şamotă, I.; Száva, I. Biomechanical and Clinical Correlations in Flexible Fixations of Unstable Shaft Fractures, International Conference “Biomechanics 2004”. In Proceedings of the Jedrzej Sniadecki Academy of Physical Education and Sport, Gdansk, Poland, 9–11 September 2004; pp. 215–219. [Google Scholar]
- Gálfi, B.; Necula, R.; Şamotă, I.; Száva, I.; Kakucs, A.; Hoţa, H. A Generalized Electric Strain Gage-Based Evaluation of The Long Human Bones Fixators’ Stiffness. Acta Tech. Napoc. Teh. Univ. Cluj-Napoca 2010, II, 359–362. [Google Scholar]
- Száva, I.; Şamotă, I.; Necula, R.; Dani, P. Some results on Electro-tensometrical Investigation of the Fractured Long Human Bones. Bull. Transilv. Univ. Braşov 2005, 12, 199–204. [Google Scholar]
- Necula, R.D. Rigid Osteosynthesis vs. Elastic Osteosynthesis. Ph.D. Thesis, Carol Davilă University, Bucharest, Romania, 2011. [Google Scholar]
- Száva, I.; Necula, R.D.; Gálfi, B.P.; Száva, D.; Şamotă, I. New Methods in Bio-mechanical Experimental Investigations. In Proceedings of the 50th Annual Conference on Experimental Stress Analysis, EAN-2012, Tábor, Czech Republic, 4–7 June 2012; The Czech Technical University of Prague: Prague, Czech Republic, 2012; pp. 449–456, ISBN 978-80-01-05060-6. [Google Scholar]











| Type of Fixator | Linear Strain at Point j | Linear Strain at Point j | ||||
|---|---|---|---|---|---|---|
| DCP plate | 0.0003 | 0.0020 | 0.0223 | 0.0600 | 0.1320 | −0.3290 |
| Bridge plate | −0.0010 | 0.0149 | 0.0237 | 0.0283 | −0.0199 | −0.0213 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Száva, I.; Șamotă, I.; Gălățanu, T.-F.; Száva, D.-T.; Száva, I.-R. Experimental Analysis of Fractured Human Bones: Brief Review and New Approaches. Prosthesis 2025, 7, 126. https://doi.org/10.3390/prosthesis7050126
Száva I, Șamotă I, Gălățanu T-F, Száva D-T, Száva I-R. Experimental Analysis of Fractured Human Bones: Brief Review and New Approaches. Prosthesis. 2025; 7(5):126. https://doi.org/10.3390/prosthesis7050126
Chicago/Turabian StyleSzáva, Ioan, Iosif Șamotă, Teofil-Florin Gălățanu, Dániel-Tamás Száva, and Ildikó-Renáta Száva. 2025. "Experimental Analysis of Fractured Human Bones: Brief Review and New Approaches" Prosthesis 7, no. 5: 126. https://doi.org/10.3390/prosthesis7050126
APA StyleSzáva, I., Șamotă, I., Gălățanu, T.-F., Száva, D.-T., & Száva, I.-R. (2025). Experimental Analysis of Fractured Human Bones: Brief Review and New Approaches. Prosthesis, 7(5), 126. https://doi.org/10.3390/prosthesis7050126