Retrospective Clinical Study of Resin Composite and Ceramic Indirect Posterior Restorations up to 11 Years
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of Patients
- Presence of systemic health conditions affecting salivary flow or quality.
- Teeth in the terminal stage of periodontal disease.
2.2. Evaluation of Restorations
2.3. Statistical Analysis
3. Results
3.1. Failure Criteria and Overview
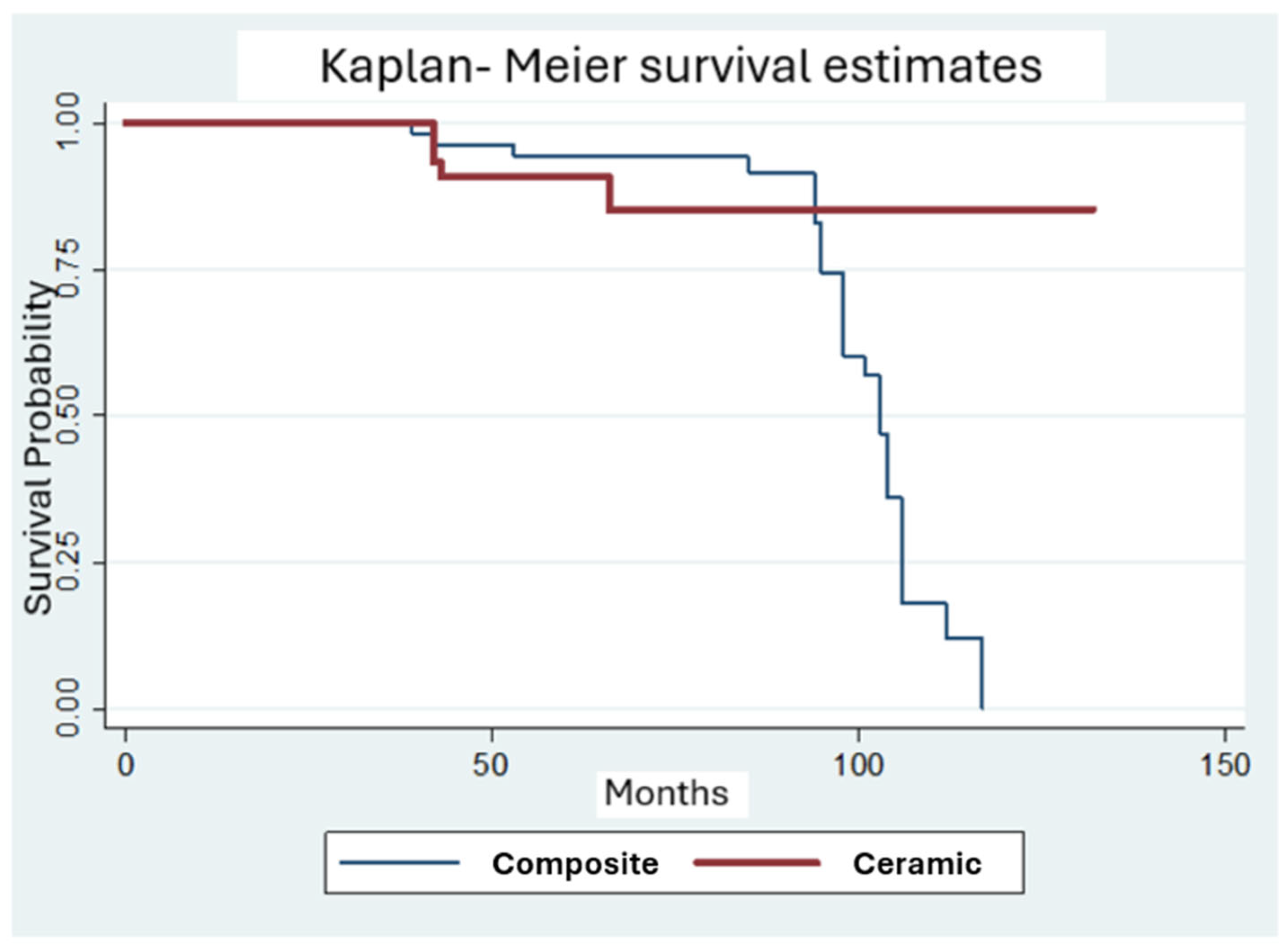
3.2. Material Performance
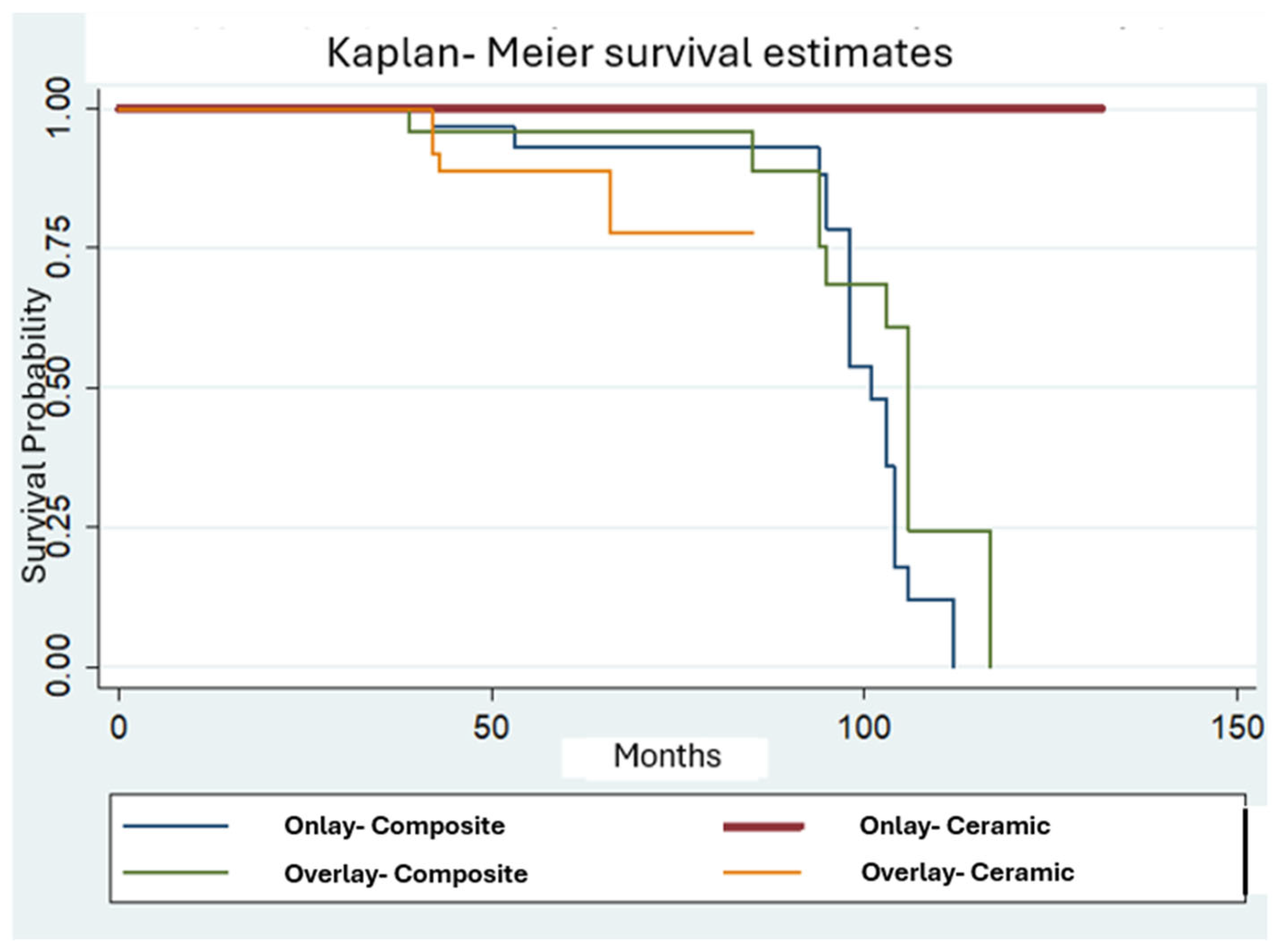
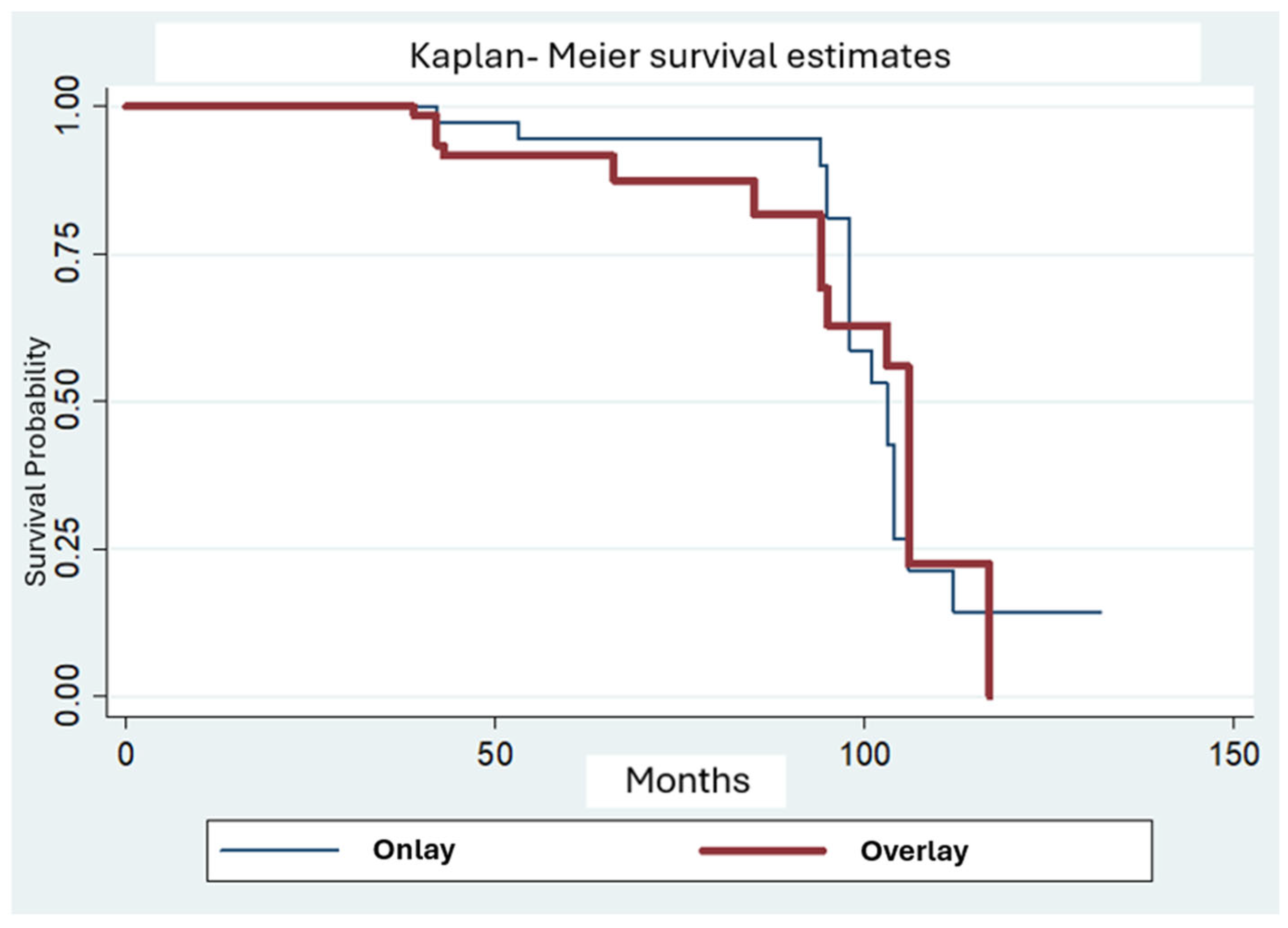
3.3. Restoration Type
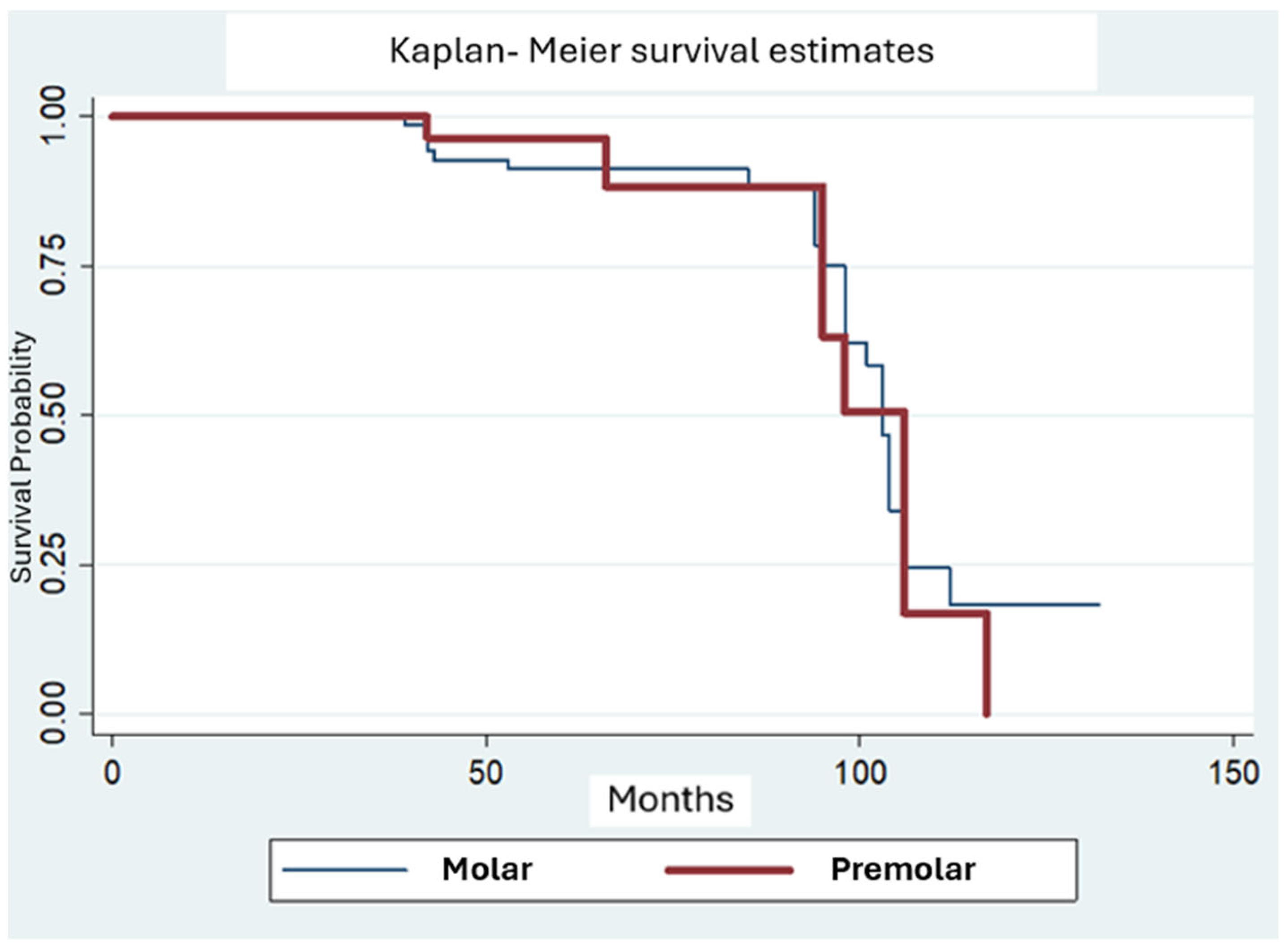
3.4. Tooth Type
3.5. Pulp Vitality
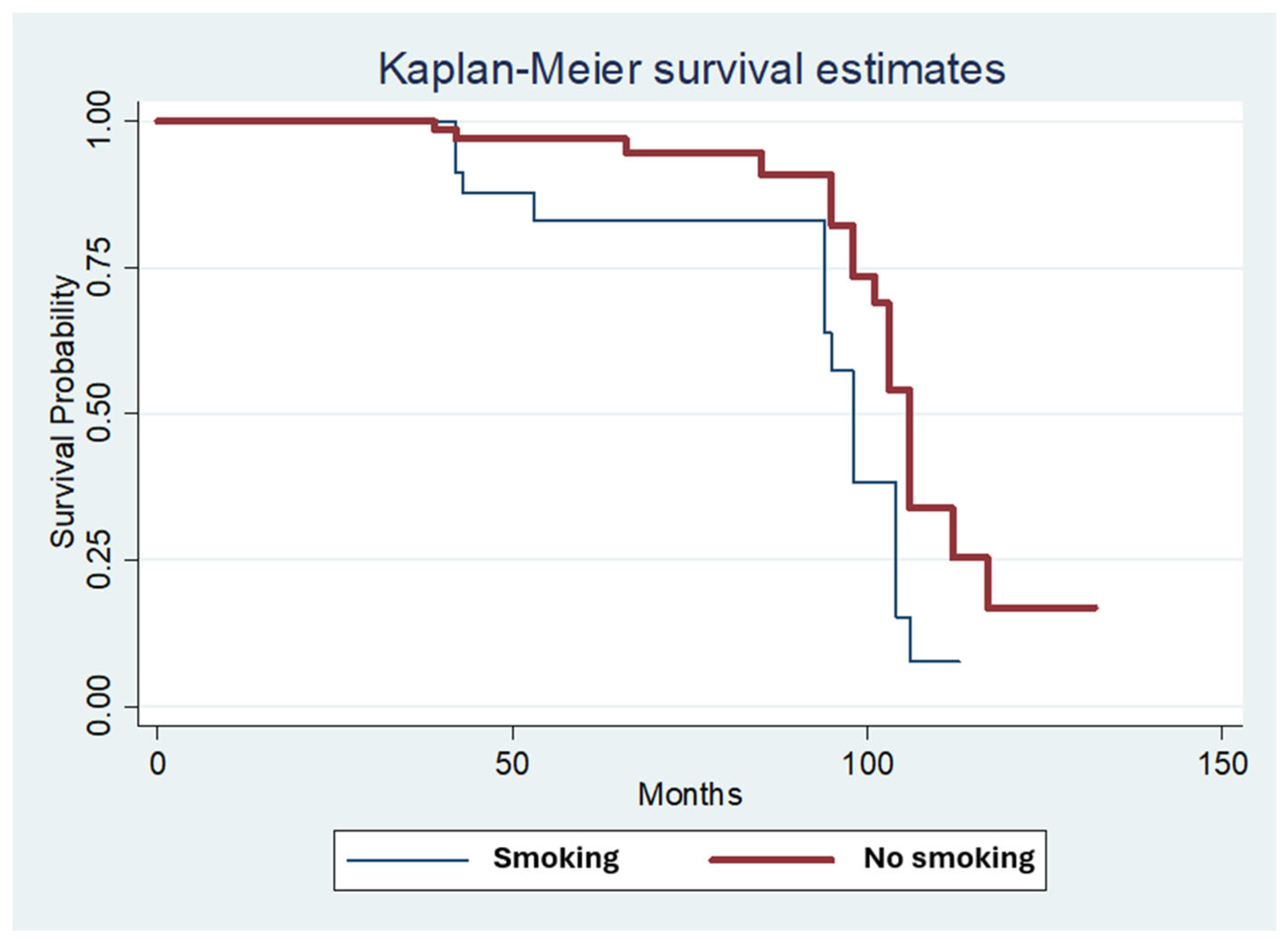
3.6. Smoking Status
3.7. Multivariate Analysis
4. Discussion
Clinical Relevance
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Morimoto, S.; Rebello de Sampaio, F.B.W.; Braga, M.M.; Sesma, N.; Özcan, M. Survival rate of resin and ceramic inlays, onlays, and overlays: A systematic review and meta-analysis. J. Dent. Res. 2016, 95, 985–994. [Google Scholar] [CrossRef]
- Barabanti, N.; Preti, A.; Vano, M.; Derchi, G.; Mangani, F.; Cerutti, A. Indirect composite restorations luted with two different procedures: A ten years follow up clinical trial. J. Clin. Exp. Dent. 2015, 7, e54. [Google Scholar] [CrossRef]
- Özcan, M. Clinical Performance of Posterior Indirect Resin Composite Restorations with the Proximal Box Elevation Technique: A Prospective Clinical Trial up to 3 Years. J. Adhes. Dent. 2024, 26, 19–30. [Google Scholar]
- D’Arcangelo, C.; Zarow, M.; De Angelis, F.; Vadini, M.; Paolantonio, M.; Giannoni, M.; D’Amario, M. Five-year retrospective clinical study of indirect composite restorations luted with a light-cured composite in posterior teeth. Clin. Oral Investig. 2014, 18, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Hofsteenge, J.W.; Fennis, W.M.M.; Kuijs, R.H.; Özcan, M.; Cune, M.S.; Gresnigt, M.M.; Kreulen, C.M. Clinical survival and performance of premolars restored with direct or indirect cusp-replacing resin composite restorations with a mean follow-up of 14 years. Dent. Mater. 2023, 39, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Ravasini, F.; Bellussi, D.; Pedrazzoni, M.; Ravasini, T.; Orlandini, P.; Meleti, M.; Bonanini, M. Treatment Outcome of Posterior Composite Indirect Restorations: A Retrospective 20-Year Analysis of 525 Cases with a Mean Follow-Up of 87 Months. Int. J. Periodontics Restor. Dent. 2018, 38, 655–663. [Google Scholar] [CrossRef]
- Van den Breemer, C.R.; Buijs, G.J.; Cune, M.S.; Özcan, M.; Kerdijk, W.; Van der Made, S.; Gresnigt, M.M. Prospective clinical evaluation of 765 partial glass-ceramic posterior restorations luted using photo-polymerized resin composite in conjunction with immediate dentin sealing. Clin. Oral Investig. 2021, 25, 1463–1473. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, R.; Taschner, M.; Garcia-Godoy, F.; Petschelt, A.; Krämer, N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J. Adhes. Dent. 2008, 10, 393–398. [Google Scholar]
- van Dijken, J.W.; Hasselrot, L. A prospective 15-year evaluation of extensive dentin–enamel-bonded pressed ceramic coverages. Dent. Mater. 2010, 26, 929–939. [Google Scholar] [CrossRef] [PubMed]
- Naeselius, K.; Arnelund, C.F.; Molin, M.K. Clinical evaluation of all-ceramic onlays: A 4-year retrospective study. Int. J. Prosthodont. 2008, 21, 40–44. [Google Scholar]
- Strasding, M.; Sebestyén-Hüvös, E.; Studer, S.; Lehner, C.; Jung, R.E.; Sailer, I. Long-term outcomes of all-ceramic inlays and onlays after a mean observation time of 11 years. Quintessence Int. 2020, 51, 566–576. [Google Scholar] [PubMed]
- Archibald, J.J.; Santos Jr, G.C.; Santos, M.J.M.C. Retrospective clinical evaluation of ceramic onlays placed by dental students. J. Prosthet. Dent. 2018, 119, 743–748. [Google Scholar] [CrossRef]
- Krug, R.; Droste, L.; Schreiber, C.; Reichardt, E.; Krastl, G.; Hahn, B.; Soliman, S. Long-term performance of ceramic in/-onlays vs. cast gold partial crowns–a retrospective clinical study. Clin. Oral Investig. 2024, 28, 298. [Google Scholar] [CrossRef]
- Saavedra, G.D.S.F.A.; Tribst, J.P.M.; Ramos, N.D.C.; Melo, R.M.D.; Rodrigues, V.A.; Ramos, G.F.; Bottino, M.A. Feldspathic and lithium disilicate onlays with a 2-year follow-up: Split-mouth randomized clinical trial. Braz. Dent. J. 2021, 32, 53–63. [Google Scholar] [CrossRef]
- Bresser, R.A.; Gerdolle, D.; Van den Heijkant, I.A.; Sluiter-Pouwels, L.M.A.; Cune, M.S.; Gresnigt, M.M.M. Up to 12 years clinical evaluation of 197 partial indirect restorations with deep margin elevation in the posterior region. J. Dent. 2019, 91, 103227. [Google Scholar] [CrossRef]
- Lempel, E.; Gyulai, S.; Lovász, B.V.; Jeges, S.; Szalma, J. Clinical evaluation of lithium disilicate versus indirect resin composite partial posterior restorations–A 7.8-year retrospective study. Dent. Mater. 2023, 39, 1095–1104. [Google Scholar] [CrossRef]
- Chabouis, H.F.; Faugeron, V.S.; Attal, J.P. Clinical efficacy of composite versus ceramic inlays and onlays: A systematic review. Dent. Mater. 2013, 29, 1209–1218. [Google Scholar] [CrossRef]
- Bresser, R.A.; Hofsteenge, J.W.; Wieringa, T.H.; Braun, P.G.; Cune, M.S.; Özcan, M.; Gresnigt, M.M.M. Clinical longevity of intracoronal restorations made of gold, lithium disilicate, leucite, and indirect resin composite: A systematic review and meta-analysis. Clin. Oral Investig. 2023, 27, 4877–4896. [Google Scholar] [CrossRef]
- Hickel, R.; Peschke, A.; Tyas, M.; Mjör, I.; Bayne, S.; Peters, M.; Hiller, K.A.; Randall, R.; Vanherle, G.; Heintze, S.D. FDI World Dental Federation: Clinical criteria for the evaluation of direct and indirect restorations—update and clinical examples. Clin. Oral Investig. 2010, 14, 349–366. [Google Scholar] [CrossRef] [PubMed]
- Murgueitio, R.; Bernal, G. Three-year clinical follow-up of posterior teeth restored with leucite-reinforced IPS Empress onlays and partial veneer crowns. J. Prosthodont. Implant. Esthet. Reconstr. Dent. 2012, 21, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Xu, Y.; Si, L.; Li, X.; Fu, B.; Hannig, M. Long-term clinical performance of composite resin or ceramic inlays, onlays, and overlays: A systematic review and meta-analysis. Oper. Dent. 2021, 46, 25–44. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, G.; Campus, G.; Strohmenger, L.; Lingstrom, P. Tobacco and dental caries: A systematic review. Acta Odontol. Scand. 2013, 71, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Vohra, F.; Andejani, A.F.; Alamri, O.; Alshehri, A.; Al-Hamdan, R.S.; Almohareb, T.; Abduljabbar, T. Influence of electronic nicotine delivery systems (ENDS) in comparison to conventional cigarette on color stability of dental restorative materials. Pak. J. Med. Sci. 2020, 36, 993. [Google Scholar] [CrossRef] [PubMed]

| Fracture of Restorative Material and Restoration Retention | Tooth Cracks and Fractures | Recurrence of Initial Pathology |
|---|---|---|
| 1. No fractures/cracks | 1. Complete integrity or small marginal fracture or hairline crack on enamel (<150 μm) | 1. No secondary or primary caries |
| 2. Small hairline crack | 2. Small marginal fracture or hairline crack on enamel (<150 μm) | 2. Small/localized area of demineralization or erosion or abfraction |
| 3. Larger hairline cracks and/or limited material chipping not affecting marginal quality or proximal contacts | 3.1 Marginal enamel defect or crack (<250 μm) 3.2 Enamel chipping 3.3 Multiple cracks | 3. Larger areas or demineralization or erosion or abfraction (on dentine not exposed) Only preventive measures |
| 4.1. Material chip fractures affecting marginal quality and/or proximal contacts 4.2. Bulk fractures affecting less than half of the restoration | 4.1. Enamel marginal gap >250 μm or dentin or base exposure 4.2. Large cracks >250 μm probe penetrates 4.3 Large enamel chipping or wall fracture | 4. Cavitation caries and suspected undermining caries. Erosion and/or abfraction in dentine that can be repaired |
| 5. Partial or complete loss of restoration or multiple fractures | 5. Cusp or tooth fracture | 5. Deep caries or exposed dentine, not accessible for repair |
| Male | Female | Molar | Premolar | Onlay | Overlay | Composite | Ceramic | Endo | Vital | Smoking | No Smoking | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | 17 | 95 | 79 | 33 | 40 | 72 | 62 | 50 | 16 | 96 | 36 | 76 |
| Total | 112 | 112 | 112 | 112 | 112 | 112 | ||||||
| FDI CFDI Criteria/Score | 1 | 2 | 3 | 4 | 5 | TOTAL |
|---|---|---|---|---|---|---|
| Fracture of restorative material and restoration retention | 83 | 3 | 4 | 5 | 17 | 112 |
| Recurrence of initial pathology | 97 | - | 1 | 3 | 11 | 112 |
| Tooth cracks and fractures | 110 | - | 1 | - | 1 | 112 |
| Time Interval | n | % Failures | Caries | Fracture | Composite | LiSi | Onlay | Overlay | Molar | Premolar | Vital | Endo |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–4 y | 6 | 18.2 | 1 | 5 | 4 | 2 | 1 | 5 | 5 | 1 | 6 | 0 |
| 4–6 y | 2 | 6.1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 6–8 y | 7 | 21.2 | 1 | 5 | 7 | 0 | 3 | 4 | 5 | 2 | 5 | 2 |
| 8–10 y | 18 | 54.5 | 8 | 10 | 18 | 0 | 13 | 5 | 14 | 4 | 15 | 3 |
| >10 y | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Covariates | Significance Values for Survival |
|---|---|
| Restoration material | 0.625 |
| Restoration type | 0.993 |
| Tooth | 0.456 |
| Endodontic treatment | 0.967 |
| Smoking | 0.019 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spyropoulou, N.; Diamantopoulou, S.; Patrinos, S.; Papazoglou, E. Retrospective Clinical Study of Resin Composite and Ceramic Indirect Posterior Restorations up to 11 Years. Prosthesis 2025, 7, 108. https://doi.org/10.3390/prosthesis7050108
Spyropoulou N, Diamantopoulou S, Patrinos S, Papazoglou E. Retrospective Clinical Study of Resin Composite and Ceramic Indirect Posterior Restorations up to 11 Years. Prosthesis. 2025; 7(5):108. https://doi.org/10.3390/prosthesis7050108
Chicago/Turabian StyleSpyropoulou, Nikolina, Sofia Diamantopoulou, Stavros Patrinos, and Efstratios Papazoglou. 2025. "Retrospective Clinical Study of Resin Composite and Ceramic Indirect Posterior Restorations up to 11 Years" Prosthesis 7, no. 5: 108. https://doi.org/10.3390/prosthesis7050108
APA StyleSpyropoulou, N., Diamantopoulou, S., Patrinos, S., & Papazoglou, E. (2025). Retrospective Clinical Study of Resin Composite and Ceramic Indirect Posterior Restorations up to 11 Years. Prosthesis, 7(5), 108. https://doi.org/10.3390/prosthesis7050108






