1. Introduction
To ensure a comprehensive clinical diagnosis of the extent and depth of dental decay, compromised or fractured tooth cusp(s) or faulty restorations involving the pulp and surrounding periodontal structures, a judicious combination of methodologies is deemed necessary [
1]. The conventional visual–tactile method, patient history, radiographic interpretation including cone-beam computed tomography (CBCT), periodontal evaluation, clinical judgement and supplementary caries detection aids are pivotal components in this diagnostic process [
2]. However, it is acknowledged that the precise assessment of large carious lesions, whether associated with or without failed restorations, poses challenges when relying solely on traditional clinical methods [
2,
3].
Dentists are trained to utilize standard approaches for the early detection and diagnosis of non-cavitated carious lesions, allowing for reversal through remineralization. This enables less invasive treatments, preserves tooth structure and reduces long-term costs [
3,
4].
The surgical removal of carious lesions and infected dentin becomes imperative in more advanced scenarios, potentially impacting the integrity of the remaining dentinal tissue and dental pulp, even when the dental pulp remains intact. It is noteworthy that dentin and dental pulp share a common embryonic origin and maintain a biological connection throughout the life of the vital tooth, forming the dentin–pulp complex [
4,
5,
6]. Consequently, the surgical removal of infected dentin can compromise the integrity of the dentin and potentially lead to dental pulp breakdown. Meticulous consideration of the dentin–pulp interface is, therefore, paramount when addressing substantial carious lesions. This awareness enables dental practitioners to formulate and implement conservative restorative strategies that optimize the overall functionality and longevity of the treated tooth [
3,
4,
5,
6].
In this context, the term caries clearance management (CCM) denotes a surgical clinical exploration and restorative caries control procedure designed to establish a final restorative diagnosis in extensive and complex failed restorations. Through the evidence provided by CCM as a clinical diagnostic procedure, clinicians can effectively communicate with patients, offering comprehensive assessments on the restorability of a compromised tooth following the complete removal of defective restorations and caries and the identification of possible complications such as the need for root canal and periodontal treatment.
The objective of this report aims to describe and apply caries clearance management (CCM) to three clinical cases to determine and establish a final restorative diagnosis in teeth compromised by extensive caries, fractured cusp or complex failed restorations. Accurate restorative diagnosis is crucial for determining the restorability and overall prognosis of the affected tooth.
2. Caries Clearance Management (CCM)
Caries clearance management (CCM) is a clinical diagnostic decision-making procedure designed to assist the dental practitioner to establish a final restorative diagnosis of a tooth severely compromised by a significant carious lesion, large failed direct or indirect restoration or extensive fractured cusp without presence of caries. Through a multi-step diagnostic approach that integrates clinical examination, radiographic interpretation, 3D cone-beam computed tomography (CBCT), periodontal and endodontic assessment, clinical judgment and caries clearance management as a clinical diagnostic procedure, dentists can determine a final restorative diagnosis regarding the restorability of a highly compromised tooth and prepare a comprehensive restorative treatment plan [
2,
3,
4] (graphical abstract).
The process begins with a thorough intraoral and extraoral clinical examination (
Figure 1) to assess the patient’s overall oral condition, including symptoms, soft tissue health and visible signs of structural compromise [
4]. Following this, radiographic interpretation (
Figure 2) and CBCT analysis [
2] (
Figure 3) are performed to evaluate the extent of caries, the thickness of the remaining dentin, the proximity of carious lesion or crack line to the pulp, the condition of existing restorations and any associated periodontal or endodontic concerns [
7]. With these initial findings, clinical judgment plays a key role in guiding the caries removal process [
8]. Minimally invasive restorative procedures are employed to preserve as much sound dentin and enamel as possible while preparing the tooth for potential restorative or endodontic therapy [
9,
10]. Magnification [
11,
12] and various diagnostic tools (caries detector dye, fluorescence-based devices and transillumination) [
2,
3,
4,
5] play a crucial role in the clinical cleanup or caries control phase of the CCM procedure for preserving questionable teeth and establishing a conservative restorative treatment plan (
Figure 4).
A critical component of the CCM diagnostic approach is assessing the health of the dental pulp and periodontal structures, particularly the supra crestal tissue attachment (SCTA). This biological evaluation informs the need for adjunctive treatments such as endodontic therapy or periodontal surgery. The ability to integrate endodontic assessment and periodontal examination at this stage helps avoid overtreatment and ensures appropriate case selection [
13,
14].
In cases where endodontic intervention is likely, the placement of a pre-endodontic restoration (e.g., a provisional crown) is strongly advised for structurally compromised teeth [
15]. This temporary barrier protects the tooth structure during endodontic treatment, reduces bacterial contamination and minimizes the risk of vertical root fracture (VRF) under normal masticatory force [
15,
16]. VRF is a frequent cause of tooth extraction during and following endodontic treatment, with an incidence rate of 13.4% [
17,
18]. A provisional crown, while not a permanent restoration, does play a crucial role in preventing vertical root fractures during and after root canal therapy, which significantly impacts the tooth’s long-term prognosis. Vertical root fractures are a serious complication that can lead to tooth loss [
15,
18,
19,
20]. As VRF is the third most common reason for tooth extraction, following caries and periodontal disease, its prevention is critical for long-term success [
15,
20,
21,
22] (
Figure 5).
Ultimately, this CCM approach emphasizes the value of clear communication with the patient regarding findings, treatment options and potential risks such as the need for endodontic therapy, crown lengthening or, in some cases, tooth extraction, along with financial considerations [
13,
14]. Providing patients with realistic expectations and a clearly outlined plan supports informed consent and fosters trust. By incorporating radiographic analysis, clinical expertise, endodontic and periodontal evaluation and structured caries clearance, the clinicians are better equipped to preserve tooth vitality, improve prognosis and deliver more predictable restorative outcomes [
13,
20,
23].
3. Determinant Factors for Final Restorative Diagnosis
The successful restorative treatment of a severely compromised tooth after a caries clearance management (CCM) procedure requires a thorough, meticulous and systematic evaluation of several crucial factors to achieve successful restoration and ensure long-lasting outcomes [
20].
3.1. Structural Integrity Evaluation
Dentists should be cognizant that the traditional clinical examination, relying on visual and tactile inspection, does not fully detect the depth of caries or the full extent of other dental problems such as the depth of defective restoration, subgingival cracks and tooth fracture. A comprehensive final restorative diagnosis of the remaining sound tooth structure should be conducted only after the selective surgical excavation of caries, the removal of decalcified tooth surface and defective restorations during the CCM procedure. This careful clinical approach minimizes any damage to the dentin–pulp complex. The key factors that affect the prognosis of the tooth are the amount of remaining sound coronal tooth structure, pulp status, occlusal trauma and specific occlusal scheme [
9,
20].
Managing recurrent caries at the margins of crowns or extensive, defective restorations including the proximal surfaces pose a unique and significant challenge in restorative dentistry. Until the failed direct or indirect restorations are removed, the dental practitioner cannot know exactly how much tooth structure remains and how deep the caries extends axially and gingivally. The clinical clean-up diagnostic procedure known as CCM is important in assessing the true extent of tooth damage to make the final diagnosis and to craft the proper restorative treatment plan [
20].
During the assessment of the remaining tooth structure after the clean-up procedure, it is crucial to have in consideration a circumferential 360° collar of 1.5–2 mm in height of healthy tooth structure above gingival margin for a successful ferrule design in crown preparation, especially for endodontically treated teeth requiring posts and cores [
20,
23,
24,
25] (
Figure 6). Therefore, the ferrule effect provided by a circumferential band of the final crown that encompasses the compromised tooth structure is important for the long-term prognosis of the restoration because it provides structural support and reduces the risk of fracture [
24,
25]. Smaller dimensions of ferrule can compromise the prognosis and increase the risk of failure of the restoration (
Figure 7). In addition, it is very important to emphasize that the dentin walls thinner than 1 mm are considered inadequate, making the tooth more susceptible to tooth fracture (
Figure 8) [
20]. Current evidence suggests that presence of a partial ferrule (1–3 walls) may be sufficient [
24,
25]. Other biomechanical parameters, such as the height and thickness of the remaining cusp, are essential to define the types of final direct or indirect restorations that will be planned [
20].
3.2. Endodontic Evaluation
The treatment of deep carious lesions approaching dental pulp presents a significant challenge to the practitioner. It is critical to assess the status of dental pulp before commencing CCM. If the pulp is healthy, it is essential to selectively remove the infected dentin while preserving affected dentin near the pulp. It is recommended to apply a bioactive material on the exposed tooth structure such as a glass ionomer to seal the lesion, protect the pulp, release fluoride and protect the dentin from bacteria. If there is a small pulpal exposure, mineral trioxide aggregate (MTA) can be applied to stimulate dentin regeneration while inhibiting bacterial invasion [
20,
21].
When the practitioner is dealing with a defective crown associated with deep caries, the defective restoration and caries should be removed and the compromised tooth structure sealed with glass ionomer to ensure the integrity of the pulp. A provisional crown is then placed to protect the tooth, thereby maintaining the integrity of the periodontium and restoring the function of a compromised tooth.
It should be noted that the two most important considerations when dealing with a fractured tooth are to determine to what extent the fracture will influence the restorability of the tooth, and whether the fracture extends axially and involves the pulp. This is especially of concern with structural deficiencies involving previous caries and pre-existing restorations [
15,
16].
3.3. Periodontal Evaluation
During CCM, it is important to note that the carious lesion or the margins of an old defective direct or indirect restoration may be situated below the gingival margin within the SCTA. Violation of the SCTA is believed to lead to adverse periodontal reactions such as gingival inflammation, bone loss, bleeding, and pain [
26,
27,
28].
The average apical-coronal dimension of the SCTA is 2.15–2.30 mm, but this can vary depending on the tooth type, site, periodontal health, and healing time after previous surgery. Therefore, it is important to measure the SCTA dimension in each specific situation rather than relying solely on average values. When surgically increasing the crown length or performing a flapless gingivectomy to expose sound tooth tissue in structurally compromised teeth, it is critical to evaluate the placement of the finish line after removing active caries [
27,
28].
After conducting the restorability assessment, it is imperative to develop a definitive restorative treatment plan and stabilize the tooth to prevent further complications.
4. Materials and Methods
This section includes the description and application of caries clearance management (CCM) to three clinical cases to establish the final restorative diagnosis of severely compromised teeth.
The primary goal is to remove all carious lesion and faulty restoration using the clinical guidelines of minimally invasive restorative procedures (
Figure 9). The remaining tooth structure is assessed after the clinical clean-up approach to diagnose the restorability of the compromised teeth. If the teeth are restorable, the dentist will develop a comprehensive restorative treatment plan [
29,
30].
The secondary goal is to assess the health status of the dental pulp, considering that the dentist is dealing with very complex restorative cases. The cold test and electric pulp test (EPT) were performed in each clinical case. These pulp test diagnostic procedures are widely used for this purpose; however, it is important to understand their limitations and how to interpret the results accurately, especially when dealing with complex cases like those involving full coverage restorations or teeth with compromised pulp vitality [
1,
20].
Restoration survival rates, in these clinical cases, were not applied because this manuscript only described three clinical cases to determine the final restorative diagnosis. Only in one clinical case was the tooth diagnosed as not restorable.
All clinical cases were performed and managed by the same operator at UCLA School of Dentistry under the observation and supervision of our clinical restorative team.
4.1. Clinical Case Report 1
4.1.1. Patient History and Examination
A 45-year-old white male, without medical history that limits or prevent dental treatment, presented with a chief complaint of tooth sensitivity on the upper right side. He was classified as ASA1 according to the American Society of Anesthesiologists Classification [
32]. Clinical examination revealed a large distal-occlusal carious lesion on the maxillary right first molar, involving a deteriorated occlusal lingual composite restoration. Radiographic evaluation confirmed the depth and extent of the lesion (
Figure 10a–c).
The tooth was diagnosed with symptomatic irreversible pulpitis, based on lingering sensitivity (approximately five seconds) during a cold pulp test (Endo-Ice, Coltene-Whaledent, Cuyahoga Falls, OH, USA), and loss of vitality under electric pulp tester (Vitality Scanner 2006 Dental Pulp Tester, Sybron/Kerr, Orange, CA, USA) reported sensitivity to warm water and chewing. Periodontal probing depths and TMJ function were within normal limits (WNL).
Based on the extent of dental pulp damage, endodontic treatment was recommended. However, the tooth’s restorability was unclear, necessitating the use of caries clearance management (CCM) to establish the final restorative diagnosis (
Figure 11).
4.1.2. CCM Protocol Application (Figure 11)
1. Isolation and Initial Caries Removal:
- ○
The tooth was isolated with a rubber dam, and minimally invasive restorative procedure was initiated using a #6 carbide round bur (Brasseler Dental, Savannah, GA, USA) under water cooling (
Figure 10d).
- ○
Peripheral carious dentin (buccal, lingual and distal) was removed until hard dentin was reached. The main concern was to determine the depth and severity of a carious lesion on the gingival margin. The carious lesion on gingival margin was very deep close to the alveolar bone.
2. Pulpal Wall Management:
- ○
Caries near the pulp was carefully excavated with a spoon excavator, leaving soft infected dentin on the axial wall to preserve the structural integrity of the pulp chamber considering that the tooth needs endodontic treatment. The Caries Detector Dye (CDD) was not used because it cannot differentiate the infected and affected dentin; and stain dentin matrix and not bacteria [
33,
34,
35,
36].
- ○
During the removal of a carious lesion on the distal surface, it was extended approximately 4 mm below the gingival margin. It was stopped until the hard dentin was reached (
Figure 10e).
3. Radiographic and Clinical Assessment:
- ○
Post-excavation, new periapical and bitewing radiographs were obtained to evaluate the root length, furcation involvement and position of the gingival margin relative to the alveolar bone (
Figure 10f,g).
4.1.3. Final Restorative Diagnosis
The maxillary right first molar was not restorable.
Reason: The tooth required extensive crown lengthening (approximately 4 mm) on the distal, buccal, and lingual surfaces. Furcation involvement was noted, and insufficient remaining tooth structure indicated a poor ability to achieve the ferrule effect.
Prognosis
The maxillary right first molar has a poor prognosis due to the following factors:
Poor crown-to-root ratio;
Furcation involvement.
Inadequate ferrule effects for structural reinforcement;
Insufficient post length to support core build-up.
As a result, the tooth was temporarily restored with glass ionomer GC Fuji IX GP (GC America Inc, Alsip, IL, USA) (
Figure 10h).
4.1.4. Treatment Plan
Surgical extraction with bone augmentation.
4.2. Clinical Case Report 2
4.2.1. Patient History and Examination
A 53-year-old white male, without medical history that limits or prevent dental treatment, presented with the chief complaint, a fractured mandibular right first molar. He was classified as ASA1 according to the American Society of Anesthesiologists Classification [
32]. Clinical examination revealed an extensive distal-lingual carious lesion involving a MODL amalgam restoration on the mandibular right first molar (
Figure 12a,b). Radiographs confirmed the lesion’s depth and extension toward the gingiva and axial wall (
Figure 12c,d).
The tooth was non-responsive to percussion and thermal stimuli and cold testing with Endo-Ice Coltene-Whaledent (Cuyahoga Falls, OH, USA), and showed loss of vitality under electric pulp tester Vitality Scanner 2006 Dental Pulp Tester (Sybron/Kerr, Orange, CA, USA). The pulpal diagnosis was pulp necrosis. Periodontal probing depths and occlusal/TMJ evaluations were within normal limits.
Based on the extent of the dental pulp damage, endodontic treatment was recommended. However, the tooth’s restorability was unclear, necessitating the use of caries clearance management (CCM) to establish the final restorative diagnosis.
4.2.2. CCM Protocol Application (Figure 11)
1. Isolation and Initial Caries Removal:
- ○
The tooth was isolated with a rubber dam, and minimally invasive restorative procedure was initiated using a #6 carbide round bur (Brasseler Dental, Savannah, GA, USA) under water cooling.
- ○
Defective amalgam restoration and caries were on occlusal, mesial and distal surfaces. Peripheral carious dentin (mesial, lingual and distal) was removed until hard dentin was reached.
2. Pulpal Wall Management:
- ○
Caries near the pulp was carefully excavated with a spoon excavator, leaving soft infected dentin on the distal axial wall to preserve structural integrity of the pulp chamber considering that the tooth needs endodontic treatment (
Figure 12e)
3. Lingual Wall Management
The carious lesion on the lingual margin was removed until hard dentin was reached. Considering that the compromised tooth needed root canal treatment, 70% of tooth structure was damaged by dental caries and failed direct restoration; the operator with the clinical restorative team decided not to remove the amalgam on the lingual axial wall during the conservative complete tooth preparation performed with diamond bur 856 (Brasseler Dental, Savannah, GA, USA) (
Figure 12f). The provisional crown was made with a bis-acrylic provisional crown (Visalys Temp, Kettenbach Dental, Huntington Beach, CA, USA) to protect the coronal tooth structure before the endodontic treatment was started (
Figure 12g,h). If the remaining amalgam on the lingual axial wall is removed, the provisional crown cannot stay because of a lack of coronal tooth structure to hold the provisional crown in place. In this case, the compromised remaining tooth structure will not be protected. It is important to protect the debilitated tooth with a provisional crown to minimize microleakage and to prevent vertical root fracture after root canal treatment [
17,
18].
After the endodontic treatment was performed, the defective remaining amalgam restoration was removed (
Figure 12i–k). A retentive shoulder core build-up design [
35,
36] was used to provide a strong and stable core foundation for a crown. It achieves this by utilizing a combination of mechanical and adhesive principles. The buccal axial wall was prepared carefully, creating a shoulder design about 2 mm above the gingival level and a trestle design on axial wall. This retentive shoulder design will hold the core build-up in place by friction, a trestle curved design and increased surface area for the adhesion. Resin modified glass ionomer GC Fuji lining (GC America Inc., Alsip, IL, USA) was placed on the top of the gutta-percha to seal the floor of pulp chamber and the entire tooth was built-up with Core Flo DC (Bisco Dental Products, Schaumburg, IL, USA) [
37,
38,
39].
Crown Tooth Preparation: Final tooth preparation for full gold crown was performed after the core build-up, positioning the distal and lingual gingival margin on sound dentin approximately 0.5 mm below the free gingiva. On the lingual axial wall was a ferrule design about 1.5 mm above the lingual margin and 2 mm on the buccal axial wall. A new provisional crown was made and cemented with Temp Bond NE (Kerr Dental, Pomona, CA, USA) (
Figure 12l).
4.2.3. Restorative Diagnosis
The mandibular right first molar was restorable.
Reason: The tooth did not require crown lengthening. There were enough clinical tooth structures for ferrule design and to be restored with indirect gold restoration after endodontic therapy.
4.2.4. Prognosis
The mandibular right first molar had a good prognosis.
4.2.6. Provisional Restorative Phase
The first bis-acrylic provisional crown (Visalys Temp, Kettenbach Dental, Huntington Beach, CA, USA) was fabricated and cemented with Temp Bond NE (Kerr Dental, Pomona, CA, USA) to protect and to prevent vertical tooth fracture during endodontic treatment (
Figure 12g,h). After completing endodontic therapy, core build-up was performed and a new provisional crown was cemented (
Figure 12l).
4.3. Clinical Case Report 3
4.3.1. Patient History and Examination
A 69-year-old white woman, without medical history that limits or prevent dental treatment, presented with the chief complaint, a fractured maxillary left first molar. She was classified as ASA1 according to the American Society of Anesthesiologists Classification [
32]. Clinical examination revealed an extensive carious lesion on the mesio-occlusal-lingual surface associated with the fracture of the disto-palatal cusp on the maxillary left first molar. A distal-lingual fractured cusp was observed clinically but was not apparent radiographically (
Figure 13a–c). The tooth was not sensitive to percussion, warm water, or cold pulp testing with Endo-Ice (Coltene-Whaledent, Cuyahoga Falls, OH, USA), and there was no loss of vitality under electric pulp tester Vitality Scanner 2006 Dental Pulp Tester (Sybron/Kerr, Orange, CA, USA) Coltene-Whaledent). Periodontal probing depths, occlusion, and TMJ evaluation were all within normal limits (WNL).
The clinical and radiographic findings were insufficient to fully assess the depth of the carious lesion from the mesial surface to the pulpal axial wall. Additionally, the presence of a fracture or crack line in the undermined mesio-buccal cusp could not be confirmed. As a result, caries clearance management (CCM) was planned to further explore the lesion and assess the remaining tooth structure to establish the final restorative diagnosis.
4.3.2. CCM Protocol Application
The tooth was isolated with a rubber dam, and selective caries removal was initiated using a #6 round bur (Brasseler Dental, Savannah, GA, USA) under water cooling via the occlusal/buccal approach (
Figure 13d). All soft caries and the existing restoration on the occlusal, mesial, and lingual surfaces were removed, stopping at hard dentin and enamel on the periphery (
Figure 13e).
- 2.
Pulpal Wall and Crack Management
Caries on the pulpal wall was carefully excavated until firm dentin was reached. A crack line extending from the occlusal toward the lingual surface was identified but did not propagate beyond the middle third of the lingual wall (
Figure 13f). The endodontist suggested there is no need to do CBCT analysis because the crack line was very smooth and there is not any catch with the explorer.
4.3.3. Final Restorative Diagnosis
The maxillary left first molar was restorable.
Reason: The tooth did not require crown lengthening. The crack line on the pulpal/lingual wall was localized. This tooth has a compromised tooth structure because the carious lesion and failed composite resin affected the mesial, occlusal, and lingual surfaces. There was undermined tooth structure on the mesio-buccal cusp and fractured disto-lingual cusp. The tooth was planned to be restored with a composite resin core build-up and full gold crown.
4.3.4. Prognosis
The maxillary left first molar had a good prognosis.
4.3.6. Treatment Execution
Composite Resin Core Build-Up and Crown Preparation:
A composite resin core build-up with Core Flo DC (Bisco Dental Products, Schaumburg, IL, USA) was completed, and the tooth was prepared for a full gold crown with diamond brasseler bur 850 and 856 (Brasseler USA, Savannah, GA, USA) (
Figure 13g).
Immediate Dentin Sealing (IDS): IDS was applied using Self-etching Universal Bond (Bisco Dental Products, Schaumburg, IL, USA) to seal the crack line on the lingual-occlusal surface and the entire preparation. This approach optimized bond strength, minimized postoperative sensitivity, and supported stress-free bonding. Glycerin was applied to displace the oxygen-inhibited layer (OIL), followed by light curing for 20 s to polymerize the OIL.
A provisional crown was made with bis-acrylic provisional crown (Visalys Temp, Kettenbach Dental, Huntington Beach, CA, USA) and cemented with Temp-Bond NE (Kerr Dental, Pomona, CA, USA) to protect the tooth for further restorative and endodontic assessment (
Figure 13h).
4.3.7. Follow-Up
At the follow-up appointment, the provisional crown performed well, and the patient reported no symptoms. The tooth showed a favorable response, with no sensitivity to cold pulp testing using Endo-Ice (Coltene-Whaledent).
4.3.8. Prognosis
The tooth was expected to have a favorable outcome following final crown placement, ensuring long-term function and stability.
5. Discussion
To ensure a comprehensive clinical diagnosis of severely compromised teeth in modern restorative dentistry is a challenge. The traditional visual-tactile method, patient history, radiographic interpretation including cone-beam computed tomography (CBCT), periodontal evaluation, clinical judgement and supplementary caries detection aids are pivotal components in this diagnostic process [
2]. However, it is acknowledged that the precise assessment of extensive carious lesions, whether associated with or without failed direct/indirect restorations, poses challenges when relying solely on traditional clinical methods [
1,
6].
In recent years, with an improved understanding of dental caries pathogenesis and the need to minimize pulp exposure risk, more conservative caries removal procedures have been developed with the concept of minimal intervention dentistry [
4,
5]. The primary goal in treating caries with minimally invasive restorative procedures is to preserve the dental pulp and tooth structure, contributing to tooth longevity while restoring the tooth to normal form and function [
30,
31]. Evidence suggests that less invasive treatment should be used whenever possible, and the International Caries Consensus Collaboration (ICCC) has published recommendations on the terminology of caries lesions and tissue removal [
40,
41]. Caries Detector Dye (CDD) is questionable. During its clinical application, can not differentiate the infected and affected dentin. CDD stain dentin matrix and not bacteria [
33,
34,
35,
36].
However, various concepts in carious tissue removal procedures [
30,
31,
42] do not emphasize in detail the importance of tooth restorability for highly compromised teeth with fractured cusp associated with extensive failed restoration without caries or failed and symptomatic indirect restoration (crown) with no presence of dental caries clinically.
Studies show conflicting success rates for nonsurgical endodontic treatment on molars over 2–10 years following root canal treatments, ranging between 74–94% [
43,
44,
45]. Lately, endodontists request a restorability assessment of questionable teeth before proceeding with root canal therapy, especially in teeth with extensively failed direct or indirect (crowns) restorations whether associated with dental caries or not [
46]. Currently, there is not a very well-defined diagnostic procedure to establish the final restorative diagnosis in highly compromised teeth that might require complex restorative treatment, associated or not with crown lengthening or endodontic therapy.
Caries clearance management (CCM) is a novel comprehensive clinical diagnostic restorative procedure designed to assist dentists in establishing the final restorative diagnosis regarding the restorability of a tooth compromised by extensive caries, a tooth with fractured cusp(s) or a failed large direct/indirect restoration without caries or a combination of all of them (
Figure 11).
To accurately determine the compromised tooth’s restorability, a comprehensive multi-step diagnostic approach including the CCM should emphasize three key elements in the assessment report: the structural integrity of the tooth, an endodontic report and the periodontal status of periodontium.
Caries clearance management (CCM) as a clinical decision-making procedure was utilized in three clinical cases with different levels of restorative difficulty in patients aged 45 to 69 years old in whom CCM was applied to determine the final restorative diagnosis to know the restorability status of the questionable tooth.
Case 1: The tooth was deemed non-restorable because crown lengthening would require the removal of 3 mm of alveolar bone, compromising the adjacent tooth and involving the furcation. No CBCT was taken, as the tooth was determined to be non-restorable.
Case 2: The tooth had a necrotic pulp and required root canal therapy. Preparation was performed while maintaining the lingual wall to support a provisional crown. The priority was to seal the margin with the provisional crown to limit microleakage and prevent tooth fracture during the endodontic therapy. Following root canal treatment, the temporary filling was removed, the tooth was built up, and a new provisional crown was fabricated. After 6 weeks with no symptoms, the tooth was deemed restorable, and the final restoration was placed.
Case 3: Dental caries had damaged the mesio-occlusal-lingual surface associated with the fracture of the disto-lingual cusp. Although the buccal appeared intact, the undermined structure weakened the mesio-buccal cusp. The mesio-occlusal-lingual involvement by dental caries, undermined mesio-buccal cusp and fractured disto-lingual cusp made this a complex case. The old composite and carious lesion were removed under rubber dam isolation. A crack line was identified on the occlusal-lingual surface. Additional caries was removed until firm dentin was reached, after which the tooth was built up and provisional restoration was cemented and assessed at 4–6-weeks. Endodontic consultation concluded that the tooth has a healthy pulp. The restorative treatment was proceeded with the final crown, and no CBCT was required, as root canal therapy was unnecessary.
6. Conclusions
Caries clearance management (CCM) is a clinical diagnostic procedure. Its main goal is to establish the final restorative diagnosis in severely compromised teeth, which will determine their restorability. Clinical examinations, periapical films, CBCT analysis and several other diagnostic assistance aids do not provide sufficient information to enable dental practitioners to accurately evaluate teeth that have been previously restored and have pulp and/or periapical pathosis. The presence of the most common causes of pulp and periapical disease (marginal breakdown, caries, cracks and fractures) cannot be fully diagnosed without removing the existing restoration.
It is essential to carefully assess the remaining tooth structure after removing the caries and defective direct or indirect restoration to determine and establish the restorability of debilitated teeth. In some cases, it will need consultation with a periodontist and endodontist before the final restorative diagnosis is achieved to establish a comprehensive restorative treatment plan.
There are several limitations in applying CCM in severely compromised teeth. (a) Clear and detailed communication with patients about the steps of CCM is required before this diagnostic procedure starts, explaining in detail the advantages and disadvantages. One of the major disadvantages is when the dentist, after the diagnostic cleanup, decides the tooth is not restorable. It means the tooth should be extracted. (b) The procedure is time-consuming because of the complexity of the debilitated tooth; it will need proper isolation with a rubber dam and the dentist must be very cautious during caries and defective restoration removal. (c) There is a high cost in cases where consultations with specialists such as a periodontist and an endodontist are needed before making the final restorative diagnosis. (d) The procedure must be slowed down to assess the pulp condition during the provisional stage before establishing the final restorative treatment plan.
The main advantages of CCM, by carefully removing the caries and old failing restoration or removing the failing restoration associated with cusp fracture with no presence of caries or removing defective crown with no caries, when the tooth is very sensitive to warm water and lingering pain to Endo Ice Test, are the following (
Figure 11): (a) Allow to achieve accurate restorative diagnosis, (b) establishing a proper restorative comprehensive treatment plan, (c) reduced misunderstanding with patients, (d) preventing further damage and preserving tooth structure and (e) achieving excellent restorative outcomes.
Using CCM as a clinical diagnostic procedure in addition to other examinations allows the clinician to make a proper clinical judgement and decision in determining the final restorative diagnosis of a tooth with a significant and extensive carious lesion; and possibly involving a failed restoration.
In summary, The clinical application of CCM as diagnostic procedure allow to establish the final restorative diagnosis and helps prevent miscommunication between the dentist and patient regarding potential complications, such as the need for a root canal or crown lengthening treatment after the complete excavation of the tooth. It is crucial to inform the patient about potential treatments and costs before initiating the dental diagnostic procedure.
Author Contributions
Conceptualization, E.D.B.; methodology, R.A.-R., D.F. and C.M.; validation, M.H.; investigation, E.D.B. and E.T.; resources, E.D.B. and E.T.; writing—original draft preparation, E.D.B. and E.T.; writing—review and editing, E.D.B., R.A.-R., M.H., D.F. and C.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available upon request to the corresponding author(s).
Acknowledgments
Nathan Kang, Salma Durra, David Yamin, Nadia Ballard, Thomas Boyce, and Terrence Donovan.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bjørndal, L.; Simon, S.; Tomson, P.L.; Duncan, H.F. Management of deep caries and the exposed pulp. Int. Endod. J. 2019, 52, 949–973. [Google Scholar] [CrossRef]
- Du, M.; Wu, X.; Ye, Y.; Fang, S.; Zhang, H.; Chen, M. A combined approach for accurate and accelerated teeth detection on cone beam CT images. Diagnostics 2022, 12, 1679. [Google Scholar] [CrossRef] [PubMed]
- Pretty, I.A. Caries detection and diagnosis: Novel technologies. J. Dent. 2006, 34, 727–739. [Google Scholar] [CrossRef]
- Featherstone, J.; Crystal, Y.O.; Ramos Gomez, F.R. CAMBRA® Caries Management by Risk Assessment: A Comprehensive Caries Management Guide for Dental Professionals. J. Calif. Dent. Assoc. 2019, 47, 25–34. [Google Scholar]
- Gugnani, N.; Pandit, I.; Srivastava, N.; Gupta, M.; Sharma, M. International Caries Detection and Assessment System (ICDAS): A new concept. Int. J. Clin. Pediatr. Dent. 2010, 4, 93–100. [Google Scholar] [CrossRef]
- Dawood, A.; Patel, S. The dental practicality index -assessing the restorability of teeth. Br. Dent. J. 2017, 222, 755–758. [Google Scholar] [CrossRef]
- Ekstrand, K.; Qvist, V.; Thylstrup, A. Light microscope study of the effect of probing in occlusal surfaces. Caries Res. 1987, 21, 368–374. [Google Scholar] [CrossRef]
- Ntovas, P.; Loubrinis, N.; Maniatakos, P.; Rahiotis, C. Evaluation of dental explorer and visual inspection for the detection of residual caries among Greek dentists. J. Conserv. Dent. 2018, 21, 311–318. [Google Scholar] [CrossRef]
- Lim, Z.E.; Duncan, H.F.; Moorthy, A.; McReynolds, D. Minimally invasive selective caries removal: A clinical guide. Br. Dent. J. 2023, 234, 233–240. [Google Scholar] [CrossRef]
- Bonilla, E.D.; Stevenson, R.G.; Caputo, A.A.; White, S.N. Microleakage resistance of minimally invasive Class I flowable composite restorations. Oper. Dent. 2012, 37, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, E.D.; Hayashi, M.; Johnson, W.R.; Pameijer, C. Dental magnification technology evolves to become an industry icon. Quintessence Intl. 2021, 52, 749–750. [Google Scholar] [CrossRef]
- Bonilla, E.D.; Mishail, D.; Zhang, E.; Hayashi, M.; Pameijer, C.H. Hallmark of Dentistry: The evolution and benefits of the dental magnifying loupe. J. Calif. Dent. Assoc. 2023, 51, 2176579. [Google Scholar] [CrossRef]
- Lang, N.P.; Bartold, P.M. Periodontal Health. J. Clin. Periodontol. 2018, 45, S9–S16. [Google Scholar] [CrossRef] [PubMed]
- Marzadori, M.; Stefanini, M.; Sangiorgi, M.; Mounssif, I.; Monaco, C.; Zucchelli, G. Crown lengthening and restorative procedures in the esthetic zone. Periodontol. 2000 2018, 77, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Gavriil, D.; Kakka, A.; Myers, P.; O’Connor, C.J. Pre-endodontic restoration of structurally compromised teeth: Current concepts. Br. Dent. J. 2021, 231, 243–349. [Google Scholar] [CrossRef]
- ElAyouti, A.; Serry, M.I.; Geis-Gerstorfer, J.; Löst, C. Influence of cusp coverage on the fracture resistance of premolars with endodontic access cavities. Int. Endod. J. 2011, 44, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Touré, B.; Faye, B.; Kane, A.W.; Lo, C.M.; Niang, B.; Boucher, Y. Analysis of reasons for extraction of endodontically treated teeth: A prospective study. J. Endod. 2011, 37, 1512–1515. [Google Scholar] [CrossRef]
- Chang, W.T.; Huang, H.Y.; Lee, T.M.; Sung, T.Y.; Yang, C.H.; Kuo, Y.M. Predicting root fracture after root canal treatment and crown installation using deep learning. J. Dent. Sci. 2024, 19, 587–593. [Google Scholar] [CrossRef]
- Bonilla, E.D.; Del Aguila, C.L.; Wetzel, D. Eating disorders: Diagnosis and prosthodontic management. BAOJ Dent. 2017, 3, 037. [Google Scholar]
- Shillingburg, H.T.; Sather, D.; Wilson, E.; Cain, J.R.; Mitchell, D.L. Fundamentals of Fixed Prosthodontics, 4th ed.; Quintessence Publishing: Chicago, IL, USA, 2012. [Google Scholar]
- Liao, W.C.; Tsai, Y.L.; Wang, C.Y.; Chang, M.C.; Huang, W.L.; Lin, H.J.; Liu, H.C. Clinical and Radiographic characteristics of vertical root fracture in endodontically and non-endodontically treated teeth. J. Endod. 2017, 43, 687–693. [Google Scholar] [CrossRef]
- Patel, S.; Bhuva, B.; Bose, R. Present status and future directions: Vertical root fractures in root filled teeth. Int. Endod. J. 2022, 5, 804–826. [Google Scholar] [CrossRef]
- Grossmann, Y.; Sadan, A. The prosthodontic concept of crown-to-root ratio: A review of the literature. J. Prosthet. Dent. 2005, 93, 559–562. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.A.; Engelman, M.J. Ferrule design and fracture resistance of endodontically treated teeth. J. Prosthet. Dent. 1990, 63, 529–536. [Google Scholar] [CrossRef]
- Naumann, M.; Schmitter, M.; Frankenberger, R.; Krastl, G. “Ferrule Comes First. Post Is Second!” Fake News and Alternative Facts? A Systematic Review. J. Endod. 2018, 44, 212–219. [Google Scholar] [CrossRef]
- Jain, A.; Bahuguna, R. Role of matrix metalloproteinases in dental caries, pulp and periapical inflammation: An overview. J. Oral Biol. Craniofacial Res. 2015, 5, 212–218. [Google Scholar] [CrossRef]
- Newman, M.G.; Takei, H.H.; Carranza, F.A. Carranza’s Clinical Periodontology, 10th ed.; Saunders Elsevier: St. Louis, MO, USA, 2006. [Google Scholar]
- Schmidt, J.C.; Sahrmann, P.; Weiger, R.; Schmidlin, P.R.; Walter, C. Biologic width dimensions—A systematic review. J. Clin. Periodontol. 2013, 40, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, S.; Caton, J.G.; Albandar, J.M.; Bissada, N.F.; Bouchard, P.; Cortellini, P.; Demirel, K. Periodontal manifestations of systemic diseases and developmental and acquired conditions: Consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S237–S248. [Google Scholar] [CrossRef]
- Jurasic, M.M.; Gillespie, S.; Sorbara, P.; Clarkson, J.; Ramsay, C.; Nyongesa, D.; McEdward, D. Deep caries removal strategies: Findings from the National Dental Practice—Based Research Network. JADA 2022, 153, 1078–1088. [Google Scholar] [CrossRef]
- Innes, N.P.; Frencken, J.E.; Bjørndal, L.; Maltz, M.; Manton, D.J.; Ricketts, D.; Van Landuyt, K.; Barnerjee, A.; Campus, G.; Fontana, M.; et al. Managing carious lesions: Consensus recommendations on terminology. Adv. Dent. Res. 2016, 28, 49–57. [Google Scholar] [CrossRef]
- Doyle, D.J.; Hendrix, J.M.; Garmon, E.H. American Society of Anesthesiologists Classification; StatPearls Publishing: Tampa, FL, USA, 2023. [Google Scholar]
- Zacharia, M.A.; Munshi, A.K. Microbiological assessment of dentin stained with a caries detector dye. J. Clin. Pediatr. Dent. 1995, 19, 111–115. [Google Scholar] [PubMed]
- Kidd, E.A.; Joyston-Bechal, S.; Beighton, D. The use of a caries detector dye during cavity preparation: A microbiological assessment. Br. Dent. J. 1993, 174, 245–258. [Google Scholar] [CrossRef]
- McComb, D. Caries-detector dyes-How accurate and useful are they? J. Can. Dent. Assoc. 2000, 66, 195–198. [Google Scholar] [PubMed]
- Yip, H.K.; Stevenson, A.G.; Beeley, J.A. The specificity of caries detector dyes in cavity preparation. Br. Dent. J. 1994, 176, 417–421. [Google Scholar] [CrossRef]
- Bonilla, E.D.; Mardirossian, G.; Caputo, A.A. Fracture toughness of various core build-up materials. J. Prosthodont. 2000, 9, 14–18. [Google Scholar] [CrossRef]
- Bonilla, E.D.; Pameijer, C.H.; Do Nascimento, C.; Garcia-Godoy, F.; Hayashi, M.; Khabbaz, C.; Bonilla, B.C.; Pedrazzi, V. Influence of a Retentive Shoulder Design to Prevent Early Failure of Three Core Build-Ups. Braz. Dent. J. 2019, 30, 569–576. [Google Scholar] [CrossRef]
- Bonilla, E.D.; Zhao, Z.; Maslucan, R.A.; Frimpong, C.; Al Khalifah, S. Influence of Core Build-Up Designs on Preventing Early Failure of Composite Resin Core in Molars Under Traction Forces: A Finite Element Analysis Study. J. Calif. Dent. Assoc. 2024, 52, 2426250. [Google Scholar] [CrossRef]
- Widbiller, M.; Weiler, R.; Knüttel, H.; Galler, K.M.; Buchalla, W.; Scholz, K.J. Biology of selective caries removal: A systematic scoping review protocol. BMJ 2022, 12, e061119. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Frencken, J.E.; Schwendicke, F.; Innes, N.P.T. Contemporary operative caries management: Consensus recommendations on minimally invasive caries removal. Br. Dent. J. 2017, 223, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F. Contemporary concepts in carious tissue removal: A review. J. Esthet. Restor. Dent. 2017, 29, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Lumley, P.J.; Lucarotti, P.S.; Burke, F.L. Ten-year outcome of root canal fillings in General Dental Services in England and Wales. Int. Endod. J. 2008, 41, 577–585. [Google Scholar] [CrossRef]
- Ng, Y.; Mann, V.; Gulabivala, K. Tooth survival following non-surgical root canal treatment: A systemic review of the literature. Int. Endod. J. 2010, 40, 171–189. [Google Scholar] [CrossRef] [PubMed]
- Raedel, M.; Hartmann, A.; Bohm, S.; Walter, M.H. Three-year outcomes of root canal treatment: Mining an insurance database. J. Dent. 2015, 43, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Mehta, D.; Coleman, A.; Lessani, M. Success and failure of endodontic treatment: Predictability, complications, challenges and maintenance. Br. Dent. J. 2025, 238, 527–535. [Google Scholar] [CrossRef] [PubMed]
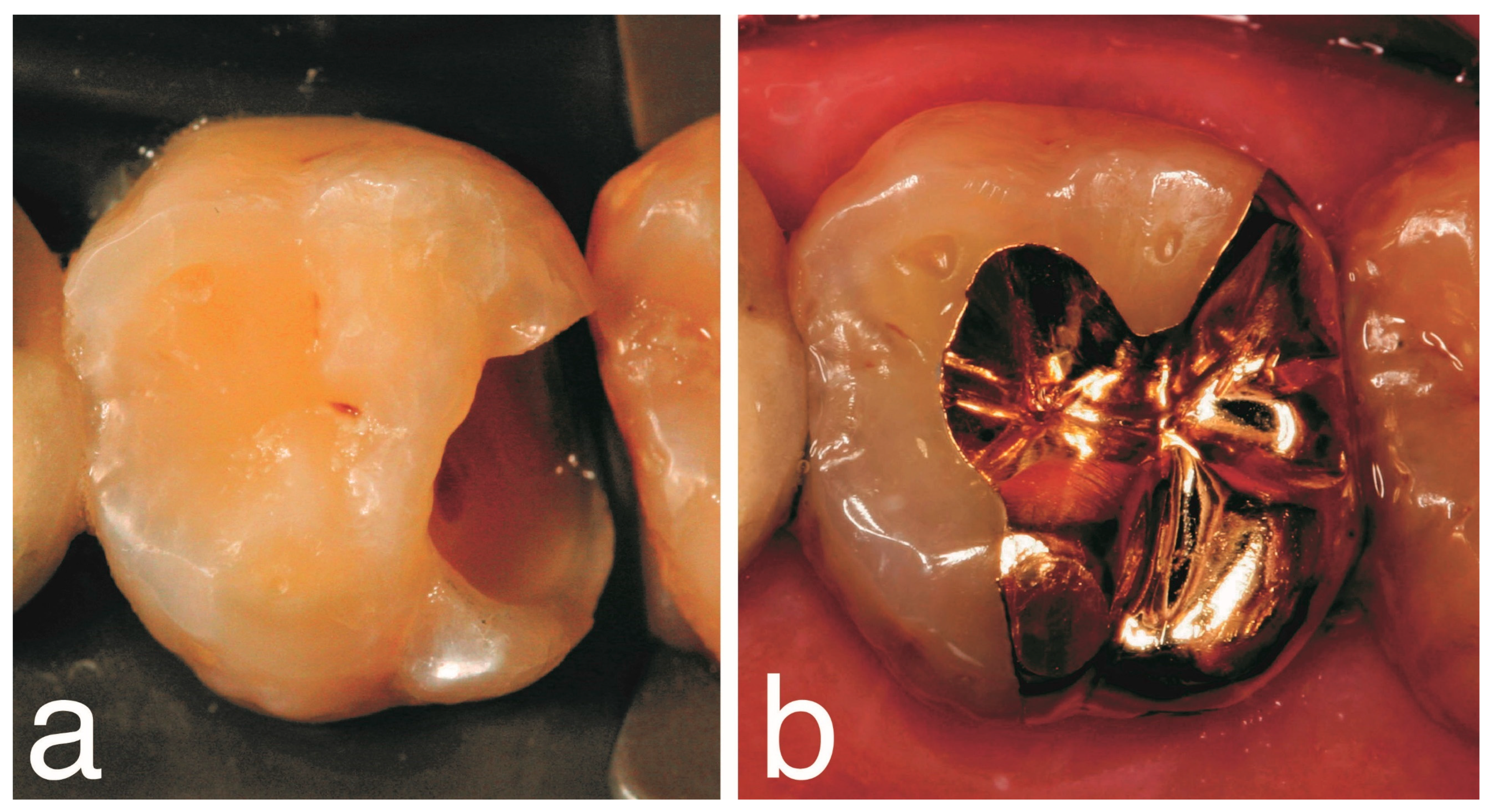
Figure 1.
Preoperative image. (a,b) Occlusal-lingual view of severely compromised mandibular first molars with failed amalgam restorations and dental caries.
Figure 1.
Preoperative image. (a,b) Occlusal-lingual view of severely compromised mandibular first molars with failed amalgam restorations and dental caries.
Figure 2.
Preoperative radiographic images. (a,b) View of severely compromised endodontically treated maxillary first molar with failed crown and radiolucency image consistent with the presence of dental caries. (c,d) View of a compromised endodontically treated maxillary first molar with a failed amalgam restoration and radiolucency image consistent with the presence of dental caries.
Figure 2.
Preoperative radiographic images. (a,b) View of severely compromised endodontically treated maxillary first molar with failed crown and radiolucency image consistent with the presence of dental caries. (c,d) View of a compromised endodontically treated maxillary first molar with a failed amalgam restoration and radiolucency image consistent with the presence of dental caries.
Figure 3.
Preoperative clinical and radiographic images. (a) Lingual view of severely compromised maxillary canine with failed amalgam associated with crack line propagating to mesial surface. (b) Radiographic image of the canine showing a radiolucency image consistent with dental caries. (c,d) CBCT image does not show the crack line involving the pulp chamber of the canine.
Figure 3.
Preoperative clinical and radiographic images. (a) Lingual view of severely compromised maxillary canine with failed amalgam associated with crack line propagating to mesial surface. (b) Radiographic image of the canine showing a radiolucency image consistent with dental caries. (c,d) CBCT image does not show the crack line involving the pulp chamber of the canine.
Figure 4.
Occlusal view. (a) Image of maxillary left first molar after CCM determined final restorative diagnosis regarding restorability. (b) Post-operative image of cemented gold onlay restoration.
Figure 4.
Occlusal view. (a) Image of maxillary left first molar after CCM determined final restorative diagnosis regarding restorability. (b) Post-operative image of cemented gold onlay restoration.
Figure 5.
Maxillary right first molar had an extensive carious lesion compromising the structural integrity of the tooth. This molar was temporized with intermediate restorative material (IRM) (Dentsply Sirona, Charlotte, NC, USA) and was not protected by a temporary crown. The tooth developed a vertical root fracture (VRF) 72 h after root canal therapy.
Figure 5.
Maxillary right first molar had an extensive carious lesion compromising the structural integrity of the tooth. This molar was temporized with intermediate restorative material (IRM) (Dentsply Sirona, Charlotte, NC, USA) and was not protected by a temporary crown. The tooth developed a vertical root fracture (VRF) 72 h after root canal therapy.
Figure 6.
View of schematic drawing and explanation of adequate ferrule. The white arrow show the height of ferrule. The red arrow represent the ability of the core build-up to tolerate severe mechanical loads maintaining the structural integrity of ferrule thickness ranging from 1 to 1.5 mm.
Figure 6.
View of schematic drawing and explanation of adequate ferrule. The white arrow show the height of ferrule. The red arrow represent the ability of the core build-up to tolerate severe mechanical loads maintaining the structural integrity of ferrule thickness ranging from 1 to 1.5 mm.
Figure 7.
View of schematic drawing of ferrule design. The red arrow goes from adequate ferrule design to no presence of or inadequate ferrule.
Figure 7.
View of schematic drawing of ferrule design. The red arrow goes from adequate ferrule design to no presence of or inadequate ferrule.
Figure 8.
View of the importance of ferrule after the build-up of endodontic treated tooth. (a) Adequate ferrule, 2 mm from gingival margin design for a crown; (b) tooth fractured because there was no ferrule.
Figure 8.
View of the importance of ferrule after the build-up of endodontic treated tooth. (a) Adequate ferrule, 2 mm from gingival margin design for a crown; (b) tooth fractured because there was no ferrule.
Figure 9.
Flowchart of the summary of caries removal procedures [
30,
31,
32,
33,
34,
35,
36].
Figure 9.
Flowchart of the summary of caries removal procedures [
30,
31,
32,
33,
34,
35,
36].
Figure 10.
Clinical and radiographic images of maxillary right first molar. (a) Preoperative clinical image showed an occlusal-lingual composite restoration. (b,c) The periapical and bitewing radiographs showed a distal large radiolucency compatible with deep caries. (d) Isolation with rubber dam. (e) Clinical image showed the selective removal distal caries during CCM procedure, which was very deep gingivally and violated the SCTA. (f,g) The periapical and bitewing radiographs confirmed the depth axially and gingivally of cavity preparation. (h) Postoperative image of the molar filled with glass ionomer.
Figure 10.
Clinical and radiographic images of maxillary right first molar. (a) Preoperative clinical image showed an occlusal-lingual composite restoration. (b,c) The periapical and bitewing radiographs showed a distal large radiolucency compatible with deep caries. (d) Isolation with rubber dam. (e) Clinical image showed the selective removal distal caries during CCM procedure, which was very deep gingivally and violated the SCTA. (f,g) The periapical and bitewing radiographs confirmed the depth axially and gingivally of cavity preparation. (h) Postoperative image of the molar filled with glass ionomer.
Figure 11.
Flowchart of protocol for caries clearance management to establish the final restorative diagnosis [
19].
Figure 11.
Flowchart of protocol for caries clearance management to establish the final restorative diagnosis [
19].
Figure 12.
Clinical and radiographic images of mandibular right first molar. (a,b) The preoperative clinical image showed occlusal-distal caries and fracture amalgam restoration. (c,d) The periapical and bitewing radiographs showed a large distal radiolucency compatible with deep caries. (e) Occlusal view of tooth preparation and selective caries removal on mesial and distal-lingual surfaces leaving soft dentin on axial wall during CCM to check tooth restorability. (f) Occlusal-lingual view showed remaining occlusal-lingual amalgam left intact for convenience to hold provisional crown in place. There is no evidence of caries on the lingual margin. (g,h) Occlusal and buccal view of provisional crown. (i,j) Periapical radiographs pre- and post-root canal treatment. (k) Clinical image showed complete removal of temporary cement from the pulp chamber and occlusal-lingual amalgam. (l) Occlusal view of provisional crown which is supported by the composite resin core build-up.
Figure 12.
Clinical and radiographic images of mandibular right first molar. (a,b) The preoperative clinical image showed occlusal-distal caries and fracture amalgam restoration. (c,d) The periapical and bitewing radiographs showed a large distal radiolucency compatible with deep caries. (e) Occlusal view of tooth preparation and selective caries removal on mesial and distal-lingual surfaces leaving soft dentin on axial wall during CCM to check tooth restorability. (f) Occlusal-lingual view showed remaining occlusal-lingual amalgam left intact for convenience to hold provisional crown in place. There is no evidence of caries on the lingual margin. (g,h) Occlusal and buccal view of provisional crown. (i,j) Periapical radiographs pre- and post-root canal treatment. (k) Clinical image showed complete removal of temporary cement from the pulp chamber and occlusal-lingual amalgam. (l) Occlusal view of provisional crown which is supported by the composite resin core build-up.
Figure 13.
Clinical and radiographic images of maxillary left first molar. (a) The preoperative clinical image showed occlusal-mesial caries and extensive distal-palatal cusp fractured. (b) Cervical caries present on buccal surface. (c) Bitewing radiograph did not show caries lesion on the mesial surface. (d) Isolation with rubber dam. (e) Clinical image of occlusal, mesial and lingual outline during CCM procedure. (f) Occlusal view showed a crack line extending from occlusal to lingual surface after selective caries removal. (g) Composite resin core build-up and tooth preparation for full gold crown performed. (h) Occlusal view of provisional crown.
Figure 13.
Clinical and radiographic images of maxillary left first molar. (a) The preoperative clinical image showed occlusal-mesial caries and extensive distal-palatal cusp fractured. (b) Cervical caries present on buccal surface. (c) Bitewing radiograph did not show caries lesion on the mesial surface. (d) Isolation with rubber dam. (e) Clinical image of occlusal, mesial and lingual outline during CCM procedure. (f) Occlusal view showed a crack line extending from occlusal to lingual surface after selective caries removal. (g) Composite resin core build-up and tooth preparation for full gold crown performed. (h) Occlusal view of provisional crown.
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).