Hip Replacement Following Intertrochanteric Osteosynthesis Failure: Is It Possible to Restore Normal Hip Biomechanics?
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kanis, J.A.; Oden, A.; McCloskey, E.V.; Johansson, H.; Wahl, D.A.; Cooper, C.; IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos. Int. 2012, 23, 2239–2256. [Google Scholar] [CrossRef] [PubMed]
- Mattisson, L.; Bojan, A.; Enocson, A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: Data from the Swedish fracture register. BMC Musculoskelet. Disord. 2018, 19, 369. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, M.; Civinini, R.; Carulli, C.; Matassi, F. Proximal femoral fractures: Epidemiology. Clin. Cases Miner. Bone Metab. 2009, 6, 117–119. [Google Scholar] [PubMed]
- Sambrook, P.; Cooper, C. Osteoporosis. Lancet 2006, 367, 2010–2018, Erratum in Lancet 2006, 368, 28. [Google Scholar] [CrossRef] [PubMed]
- Piazzolla, A.; Bizzoca, D.; Solarino, G.; Moretti, L.; Moretti, B. Vertebral fragility fractures: Clinical and radiological results of augmentation and fixation—A systematic review of randomized controlled clinical trials. Aging Clin. Exp. Res. 2020, 32, 1219–1232. [Google Scholar] [CrossRef] [PubMed]
- Veronese, N.; Maggi, S. Epidemiology and social costs of hip fracture. Injury 2018, 49, 1458–1460. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.M.; Magaziner, J.; Hebel, J.R.; Kenzora, J.E.; Kashner, T.M. Intertrochanteric versus femoral neck hip fractures: Differential characteristics, treatment, and sequelae. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 1999, 54, M635–M640. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Zhang, S.; Yang, J.; Dong, W.; Wang, S.; Cheng, Y.; Al-Qwbani, M.; Wang, Q.; Yu, B. Proximal femoral nail vs. dynamic hip screw in treatment of intertrochanteric fractures: A meta-analysis. Med. Sci. Monit. 2014, 20, 1628–1633. [Google Scholar] [CrossRef] [PubMed]
- Tawari, A.A.; Kempegowda, H.; Suk, M.; Horwitz, D.S. What made an intertrochanteric fracture unstable in 2015? Does the lateral wall play a role in the decision matrix? J. Orthop. Trauma 2015, 29 (Suppl. 4), S4–S9. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Uppal, H.S. Hip Fractures: Relevant Anatomy, Classification, and Biomechanics of Fracture and Fixation. Geriatr. Orthop. Surg. Rehabil. 2019, 10, 2151459319859139. [Google Scholar] [CrossRef] [PubMed]
- Marsillo, E.; Pintore, A.; Asparago, G.; Oliva, F.; Maffulli, N. Cephalomedullary nailing for reverse oblique intertrochanteric fractures 31A3 (AO/OTA). Orthop. Rev. 2022, 14, 38560. [Google Scholar] [CrossRef] [PubMed]
- Queally, J.M.; Harris, E.; Handoll, H.H.; Parker, M.J. Intramedullary nails for extracapsular hip fractures in adults. Cochrane Database Syst. Rev. 2014, 9, CD004961. [Google Scholar] [CrossRef] [PubMed]
- Bizzoca, D.; Bortone, I.; Vicenti, G.; Caringella, N.; Rifino, F.; Moretti, B. Gait analysis in the postoperative assessment of intertrochanteric femur fractures. J. Biol. Regul. Homeost. Agents 2020, 34 (Suppl. 3), 345–351. [Google Scholar] [PubMed]
- Méndez-Ojeda, M.M.; Herrera-Rodríguez, A.; Álvarez-Benito, N.; González-Pacheco, H.; García-Bello, M.A.; Álvarez-de la Cruz, J.; Pais-Brito, J.L. Treatment of Trochanteric Hip Fractures with Cephalomedullary Nails: Single Head Screw vs. Dual Integrated Compression Screw Systems. J. Clin. Med. 2023, 12, 3411. [Google Scholar] [CrossRef]
- Zeelenberg, M.L.; Nugteren, L.H.T.; Plaisier, A.C.; Loggers, S.A.I.; Joosse, P.; Den Hartog, D.; Verhofstad, M.H.J.; van Lieshout, E.M.M.; STABLE-HIP Study Group. Extramedullary versus intramedullary fixation of stable trochanteric femoral fractures: A systematic review and meta-analysis. Arch. Orthop. Trauma Surg. 2023, 143, 5065–5083. [Google Scholar] [CrossRef] [PubMed]
- Haidukewych, G.J.; Berry, D.J. Hip arthroplasty for salvage of failed treatment of intertrochanteric hip fractures. J. Bone Jt. Surg. Am. 2003, 85, 899–904. [Google Scholar] [CrossRef]
- Solarino, G.; Bizzoca, D.; Dramisino, P.; Vicenti, G.; Moretti, L.; Moretti, B.; Piazzolla, A. Total hip arthroplasty following the failure of intertrochanteric nailing: First implant or salvage surgery? World J. Orthop. 2023, 14, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Hardinge, K. The direct lateral approach to the hip. J. Bone Jt. Surg. Br. 1982, 64, 17–19. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Zhan, K.; Zhang, L.; Zeng, D.; Yu, W.; Zhang, X.; Zhao, M. Conversion to total hip arthroplasty after failed proximal femoral nail antirotations or dynamic hip screw fixations for stable intertrochanteric femur fractures: A retrospective study with a minimum follow-up of 3 years. BMC Musculoskelet. Disord. 2017, 18, 38. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Han, X.; Chen, W.; Mao, S.; Zhao, M.; Zhang, X.; Han, G.; Ye, J.; Chen, M.; Zhuang, J. Conversion from a failed proximal femoral nail anti-rotation to a cemented or uncemented total hip arthroplasty device: A retrospective review of 198 hips with previous intertrochanteric femur fractures. BMC Musculoskelet. Disord. 2020, 21, 791. [Google Scholar] [CrossRef] [PubMed]
| Patients (n = 31) | |
|---|---|
| Age | |
| Mean ± SD | 76.2 ± 6.84 |
| Gender | |
| Female, n (%) | 21 (67.74%) |
| BMI (kg/m2) | |
| Mean ± SD | 27.8 ± 4.76 |
| Side | |
| Right, n (%) | 16 (51.61%) |
| Timing from nailing to THA (mean ± SD, months) | 11.86 ± 10.3 |
| Mean operating time (mean ± SD, minutes) | 101 ± 48.73 |
| Patients undergoing ≥3 blood transfusions, n (%) | 17 (54.84%) |
| VAS (mean ± SD, at the final follow-up) | 2.3 ± 3.45 |
| Healthy Hip | Affected Hip | ∆ | p | |
|---|---|---|---|---|
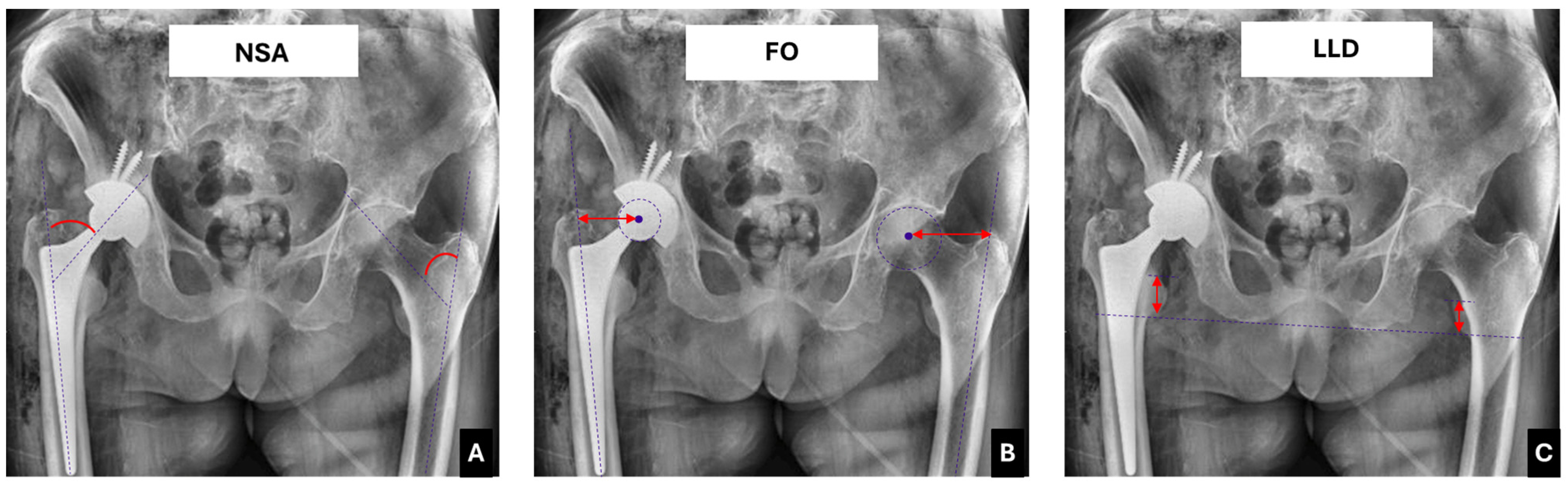
| Neck shaft angle (NSA) | 127.7 ± 5.6° | 135.1 ± 2.4° | 7.4 ± 2.6° | <0.001 * |
| Femoral offset (FO) | 42.4 ± 2.7 mm | 51.4 ± 7.42 mm | 9 ± 3.2 mm | <0.001 * |
| Limb length discrepancy (LLD) | - | - | 8.35 ± 2.25 mm | - |
| HHS | VAS | |||
|---|---|---|---|---|
| R | p | R | p | |
| ∆NSA | −0.61 | 0.01 * | 0.41 | 0.095 |
| ∆FO | −0.56 | 0.03 * | 0.24 | 0.176 |
| ∆LLD | −0.21 | 0.112 | 0.13 | 0.223 |
| Patients (n = 31) | ||
|---|---|---|
| N | Percentage | |
| Periprosthetic fractures | 3 | 9.6% |
| Implant instability | 1 | 3.23% |
| THA dislocation | 1 | 3.23% |
| Periprosthetic Joint Infections | 2 | 6.45% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bizzoca, D.; Giannini, G.; Cannito, F.D.; Colasuonno, G.; De Giosa, G.; Solarino, G. Hip Replacement Following Intertrochanteric Osteosynthesis Failure: Is It Possible to Restore Normal Hip Biomechanics? Prosthesis 2025, 7, 50. https://doi.org/10.3390/prosthesis7030050
Bizzoca D, Giannini G, Cannito FD, Colasuonno G, De Giosa G, Solarino G. Hip Replacement Following Intertrochanteric Osteosynthesis Failure: Is It Possible to Restore Normal Hip Biomechanics? Prosthesis. 2025; 7(3):50. https://doi.org/10.3390/prosthesis7030050
Chicago/Turabian StyleBizzoca, Davide, Giorgio Giannini, Francesco Domenico Cannito, Giulia Colasuonno, Giuseppe De Giosa, and Giuseppe Solarino. 2025. "Hip Replacement Following Intertrochanteric Osteosynthesis Failure: Is It Possible to Restore Normal Hip Biomechanics?" Prosthesis 7, no. 3: 50. https://doi.org/10.3390/prosthesis7030050
APA StyleBizzoca, D., Giannini, G., Cannito, F. D., Colasuonno, G., De Giosa, G., & Solarino, G. (2025). Hip Replacement Following Intertrochanteric Osteosynthesis Failure: Is It Possible to Restore Normal Hip Biomechanics? Prosthesis, 7(3), 50. https://doi.org/10.3390/prosthesis7030050








