Efficacy of Atmospheric Pressure Plasma Jet-Induced Surface Treatment on Wettability, Surface Topography, and Shear Bond Strength of Ceramic Surfaces for CAD-On Assembly
Abstract
1. Introduction
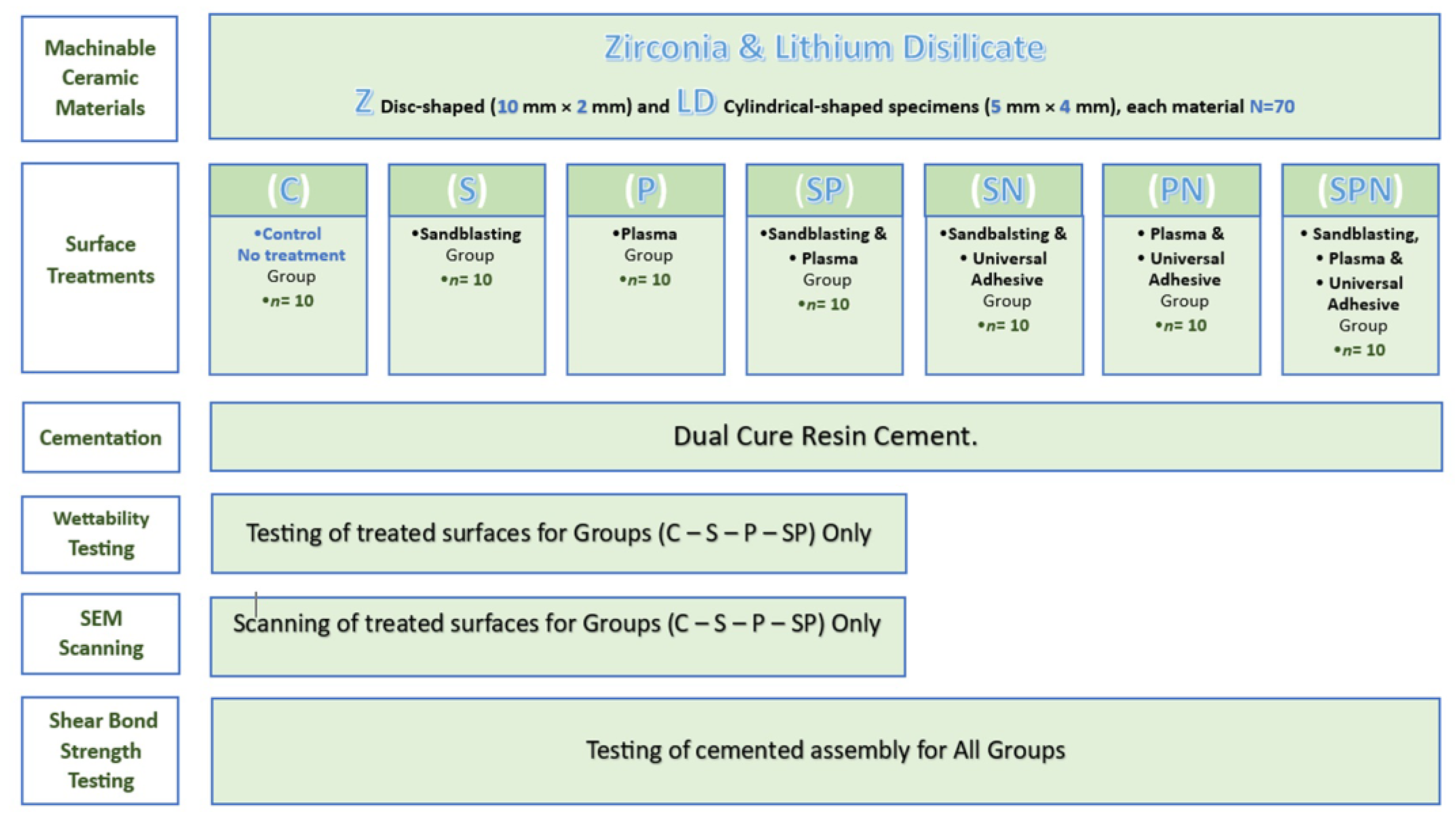
2. Materials and Methods
2.1. Specimen’s Preparation
2.2. Specimens Surface Treatments
2.3. Specimens Testing
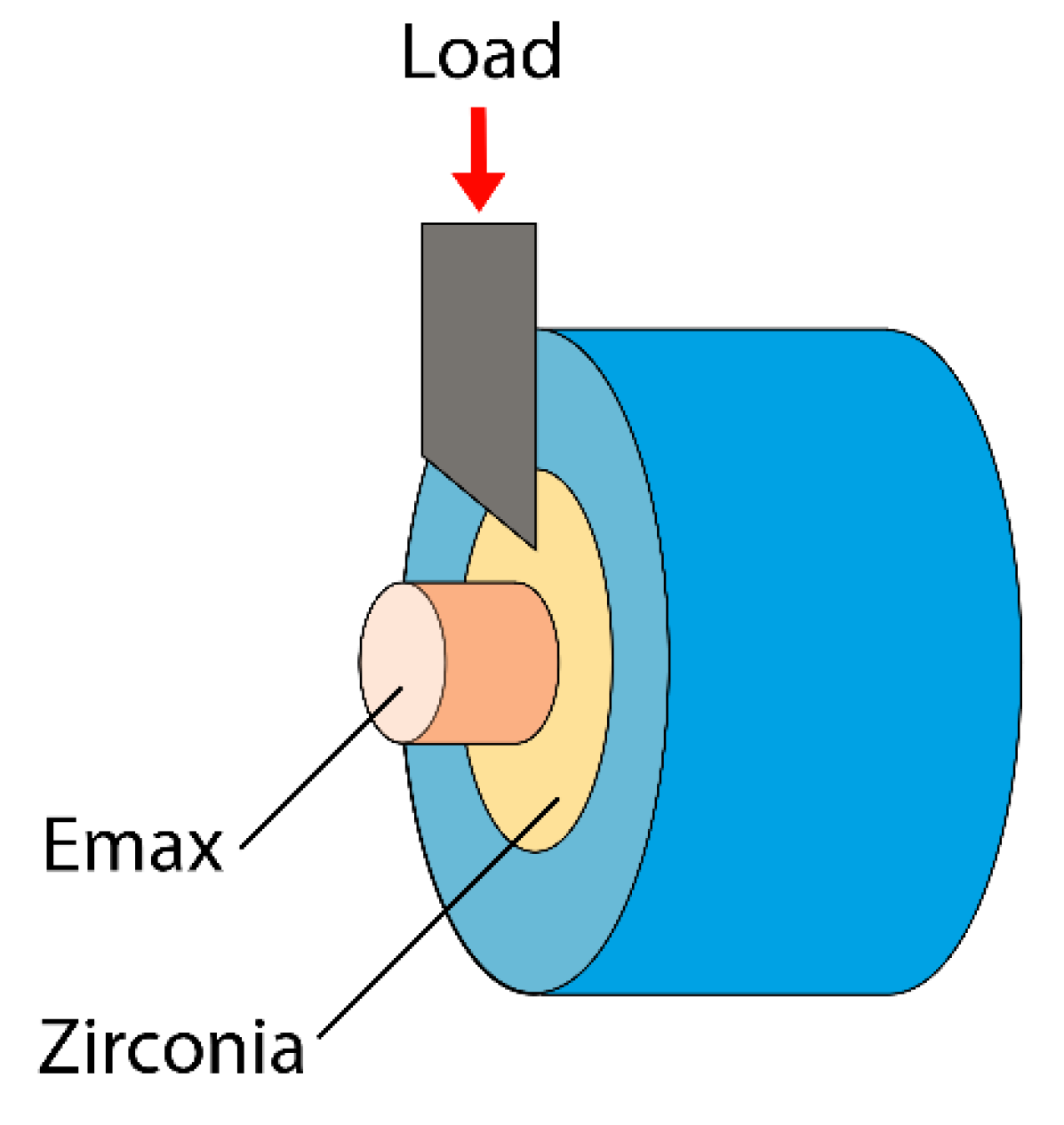
2.3.1. Shear Bond Strength
2.3.2. Contact Angle
2.3.3. Scanning Electron Microscopy (SEM)
2.4. Statistical Analysis
3. Results
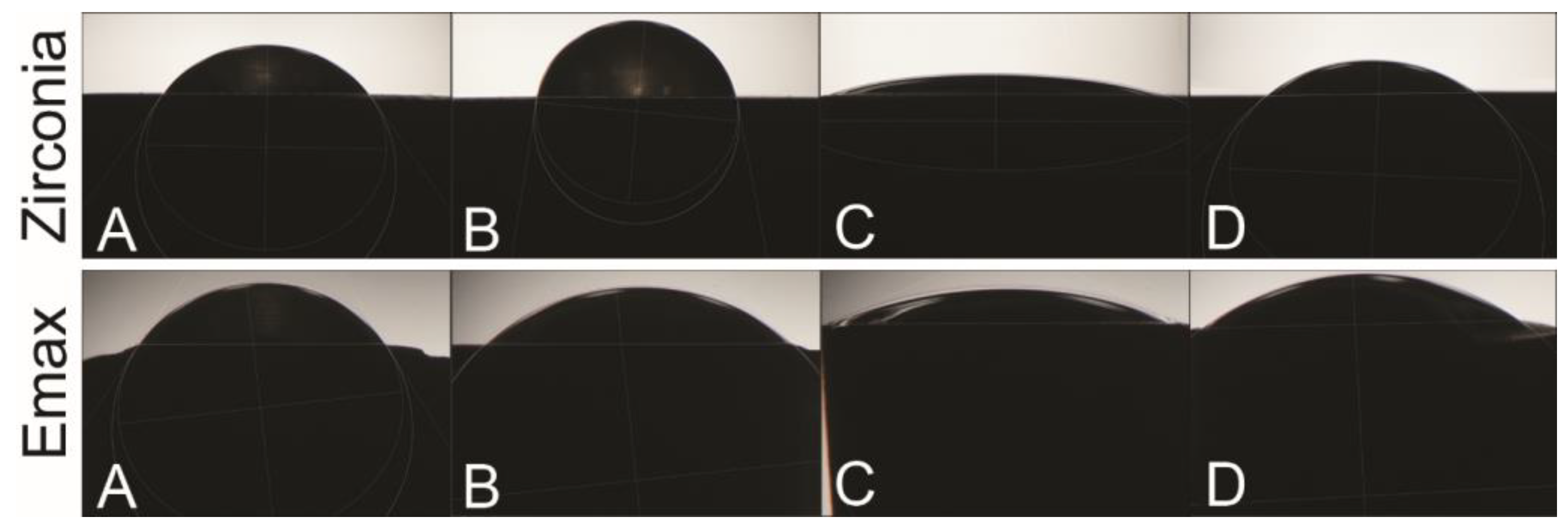
3.1. Contact Angle Test
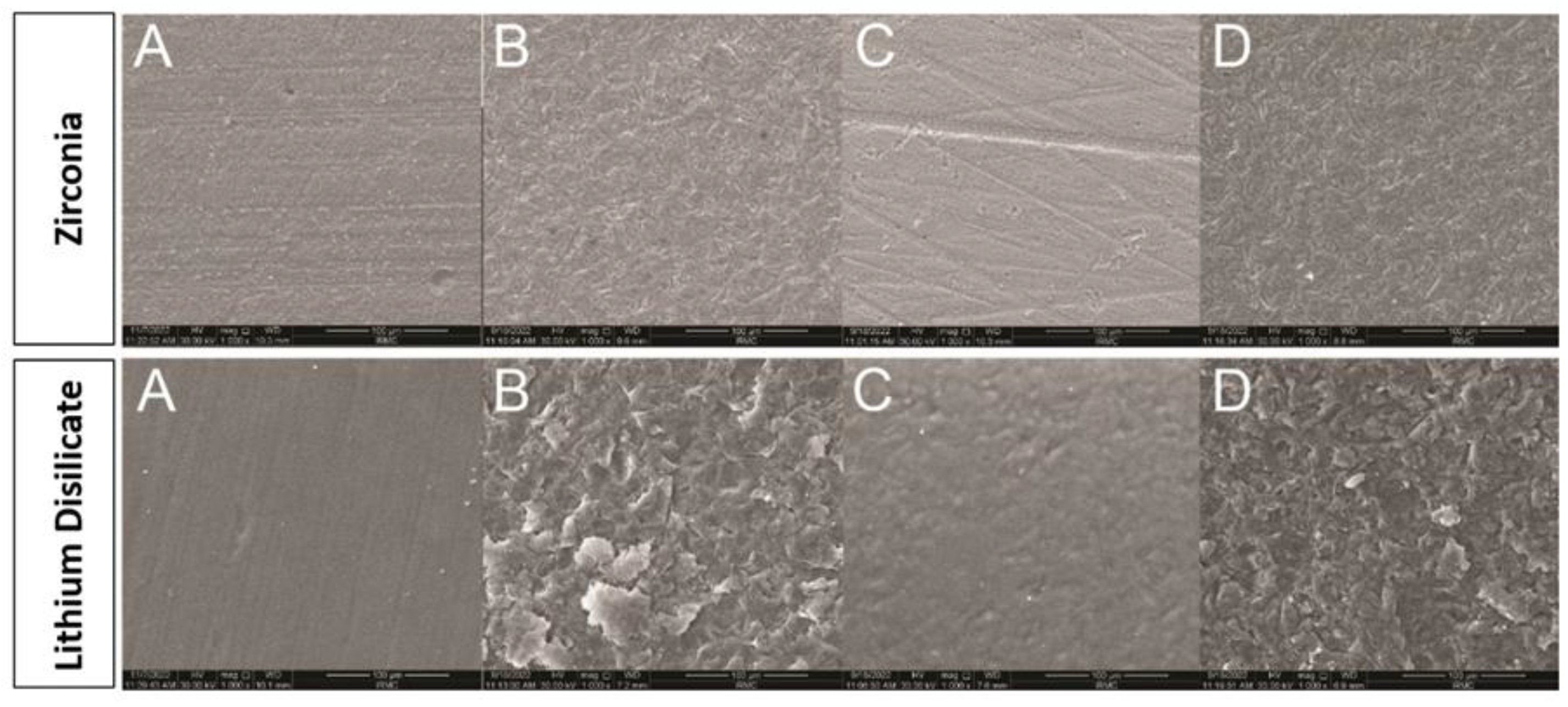
3.2. Scanning Electron Microscopy (SEM)
3.3. Shear Bond Strength Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cha, S.; Park, Y.S. Plasma in dentistry. Clin. Plasma Med. 2014, 2, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Lohbauer, U.; Zipperle, M.; Rischka, K.; Petschelt, A.; Müller, F.A. Hydroxylation of dental zirconia surfaces: Characterization and bonding potential. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 87, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, A.N.; Foxton, R.M.; Watson, T.F.; Oliveira, M.T.; Giannini, M.; Marchi, G.M. Y-TZP ceramics: Key concepts for clinical application. Oper. Dent. 2009, 34, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Soares, E.J.; de Lima Oliveira, R.F.; Silame, F.D.J.; Tonani-Torrieri, R.; Franca, R.; de CPPires-de-Souza, F. Color stability, translucency, and wettability of a lithium disilicate dental ceramics submitted to different surface treatments. Int. J. Prosthodont. Restor. Dent. 2021, 11, 4–8. [Google Scholar]
- Valverde, G.B.; Coelho, P.G.; Janal, M.N.; Lorenzoni, F.C.; Carvalho, R.M.; Thompson, V.P.; Weltemann, K.-D.; Silva, N.R. Surface characterisation and bonding of Y-TZP following non-thermal plasma treatment. J. Dent. 2013, 41, 51–59. [Google Scholar] [CrossRef]
- Tabari, K.; Hosseinpour, S.; Mohammad-Rahimi, H. The Impact of Plasma Treatment of Cercon® Zirconia Ceramics on Adhesion to Resin Composite Cements and Surface Properties. J. Lasers Med. Sci. 2017, 8 (Suppl. S1), S56–S61. [Google Scholar] [CrossRef]
- Heinlin, J.; Isbary, G.; Stolz, W.; Morfill, G.; Landthaler, M.; Shimizu, T.; Steffes, B.; Nosenko, T.; Zimmermann, J.; Karrer, S. Plasma applications in medicine with a special focus on dermatology. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 1–11. [Google Scholar] [CrossRef]
- Silva, N.R.; Coelho, P.G.; Valverde, G.B.; Becker, K.; Ihrke, R.; Quade, A.; Thompson, V.P. Surface characterization of Ti and Y-TZP following non-thermal plasma exposure. J. Biomed. Mater. Res. B Appl. Biomater. 2011, 99, 199–206. [Google Scholar] [CrossRef]
- Dou, S.; Tao, L.; Wang, R.; El Hankari, S.; Chen, R.; Wang, S. Plasma-Assisted Synthesis and Surface Modification of Electrode Materials for Renewable Energy. Adv. Mater. 2018, 30, e1705850. [Google Scholar] [CrossRef]
- Izadjoo, M.; Zack, S.; Kim, H.; Skiba, J. Medical applications of cold atmospheric plasma: State of the science. J. Wound Care 2018, 27 (Suppl. S9), S4–S10. [Google Scholar] [CrossRef]
- Domonkos, M.; Tichá, P.; Trejbal, J.; Demo, P. Applications of cold atmospheric pressure plasma technology in medicine, agriculture and food industry. Appl. Sci. 2021, 11, 4809. [Google Scholar] [CrossRef]
- Sakudo, A.; Yagyu, Y.; Onodera, T. Disinfection and Sterilization Using Plasma Technology: Fundamentals and Future Perspectives for Biological Applications. Int. J. Mol. Sci. 2019, 20, 5216. [Google Scholar] [CrossRef] [PubMed]
- Cvelbar, U.; Walsh, J.L.; Černák, M.; de Vries, H.W.; Reuter, S.; Belmonte, T.; Corbella, C.; Miron, C.; Hojnik, N.; Jurov, A.; et al. White paper on the future of plasma science and technology in plastics and textiles. Plasma Process. Polym. 2019, 16, 1700228. [Google Scholar] [CrossRef]
- Kleineidam, B.; Nokhbehsaim, M.; Deschner, J.; Wahl, G. Effect of cold plasma on periodontal wound healing-an in vitro study. Clin. Oral. Investig. 2019, 23, 1941–1950. [Google Scholar] [CrossRef]
- Liu, Y.C.; Hsieh, J.P.; Chen, Y.C.; Kang, L.L.; Hwang, C.S.; Chuang, S.F. Promoting porcelain-zirconia bonding using different atmospheric pressure gas plasmas. Dent. Mater. 2018, 34, 1188–1198. [Google Scholar] [CrossRef]
- Yılmaz Savaş, T.; Akın, C. Effect of nonthermal plasma treatment on surface roughness and bond strength between veneer ceramic and zirconia core. Int. J. Appl. Ceram. Technol. 2022, 19, 1572–1582. [Google Scholar] [CrossRef]
- Korzec, D.; Hoppenthaler, F.; Nettesheim, S. Piezoelectric Direct Discharge: Devices and Applications. Plasma 2021, 4, 1–41. [Google Scholar] [CrossRef]
- Jungbauer, G.; Favaro, L.; Müller, S.; Sculean, A.; Eick, S. The In-Vitro Activity of a Cold Atmospheric Plasma Device Utilizing Ambient Air against Bacteria and Biofilms Associated with Periodontal or Peri-Implant Diseases. Antibiotics 2022, 11, 752. [Google Scholar] [CrossRef]
- Ito, Y.; Okawa, T.; Fujii, T.; Tanaka, M. Influence of plasma treatment on surface properties of zirconia. J. Osaka Dent. Univ. 2016, 50, 79–84. [Google Scholar]
- Alessandretti, R.; Ribeiro, R.; Borba, M.; Bona, A.D. Fracture Load and Failure Mode of CAD-on Ceramic Structures. Braz. Dent. J. 2019, 30, 380–384. [Google Scholar] [CrossRef]
- Alessandretti, R.; Borba, M.; Benetti, P.; Corazza, P.H.; Ribeiro, R.; Della Bona, A. Reliability and mode of failure of bonded monolithic and multilayer ceramics. Dent. Mater. 2017, 33, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Kavut, I.; Külünk, S. Evaluation of the core thickness and resin cement on the fracture strength of zirconia-based multilayer computer-aided design/computer-aided manufacturing ceramic crowns. Dent. Med. Res. 2019, 7, 16. [Google Scholar] [CrossRef]
- Grohmann, P.; Bindl, A.; Hämmerle, C.; Mehl, A.; Sailer, I. Three-unit posterior zirconia-ceramic fixed dental prostheses (FDPs) veneered with layered and milled (CAD-on) veneering ceramics: 1-year follow-up of a randomized controlled clinical trial. Quintessence Int. 2015, 46, 871–880. [Google Scholar] [PubMed]
- Basso, G.R.; Moraes, R.R.; Borba, M.; Duan, Y.; Griggs, J.A.; Della Bona, A. Reliability and failure behavior of CAD-on fixed partial dentures. Dent. Mater. 2016, 32, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Hariton-Gross, K.; Anadioti, E.; Mante, F.; Zhang, Y.; Saleh, N. Prospective 5-year clinical evaluation of posterior zirconia fixed dental prostheses veneered with milled lithium disilicate (CADon). J. Esthet. Restor. Dent. 2022, 34, 136–144. [Google Scholar] [CrossRef]
- Nossair, S.A.; Aboushelib, M.N.; Morsi, T.S. Fracture and Fatigue Resistance of Cemented versus Fused CAD-on Veneers over Customized Zirconia Implant Abutments. J. Prosthodont. 2015, 24, 543–548. [Google Scholar] [CrossRef]
- Sasany, R.; Yilmaz, B. Marginal discrepancy and fracture load of thermomechanically fatigued crowns fabricated with different CAD-CAM techniques. J. Prosthodont. 2022, 32, 602–607. [Google Scholar] [CrossRef]
- Costa, A.K.; Borges, A.L.; Fleming, G.J.; Addison, O. The strength of sintered and adhesively bonded zirconia/veneer-ceramic bilayers. J. Dent. 2014, 42, 1269–1276. [Google Scholar] [CrossRef]
- Lee, J.J.-W.; Lloyd, I.K.; Chai, H.; Jung, Y.-G.; Lawn, B.R. Arrest, deflection, penetration and reinitiation of cracks in brittle layers across adhesive interlayers. Acta Mater. 2007, 55, 5859–5866. [Google Scholar] [CrossRef]
- Schmitter, M.; Mueller, D.; Rues, S. Chipping behaviour of all-ceramic crowns with zirconia framework and CAD/CAM manufactured veneer. J. Dent. 2012, 40, 154–162. [Google Scholar] [CrossRef]
- Schmitter, M.; Mueller, D.; Rues, S. In vitro chipping behaviour of all-ceramic crowns with a zirconia framework and feldspathic veneering: Comparison of CAD/CAM-produced veneer with manually layered veneer. J. Oral. Rehabil. 2013, 40, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Wiedenmann, F.; Klören, M.; Edelhoff, D.; Stawarczyk, B. Bond strength of CAD-CAM and conventional veneering materials to different frameworks. J. Prosthet. Dent. 2021, 125, 664–673. [Google Scholar] [CrossRef] [PubMed]
- Saeidi Pour, R.; Edelhoff, D.; Rafael, C.F.; Prandtner, O.; Frei, S.; Maziero Volpato, C.A.; Liebermann, A. Combining Esthetic Layering and Lithium Disilicate Sintering Technique on Zirconia Frameworks: A Veneering Option to Prevent Ceramic Chipping. Int. J. Periodontics Restor. Dent. 2017, 37, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Fathpour, K.; Nili Ahmadabadi, M.; Atash, R.; Fathi, A.H. Effect of Different Surface Treatment Methods on the Shear Bond Strength of Resin Composite/Zirconia for Intra-oral Repair of Zirconia Restorations. Eur. J. Dent. 2022, 17, 809–817. [Google Scholar] [CrossRef]
- Al-Hmadi, S.; Erol, F.; Guven Celik, M. Shear bond strengths of five porcelain repair systems to zirconia infrastructures. Eur. Oral. Res. 2022, 56, 55–60. [Google Scholar] [CrossRef]
- Malysa, A.; Wezgowiec, J.; Orzeszek, S.; Florjanski, W.; Zietek, M.; Wieckiewicz, M. Effect of Different Surface Treatment Methods on Bond Strength of Dental Ceramics to Dental Hard Tissues: A Systematic Review. Molecules 2021, 26, 1223. [Google Scholar] [CrossRef]
- Alagiriswamy, G.; Krishnan, C.S.; Ramakrishnan, H.; Jayakrishnakumar, S.K.; Mahadevan, V.; Azhagarasan, N.S. Surface Characteristics and Bioactivity of Zirconia (Y-TZP) with Different Surface Treatments. J. Pharm. Bioallied Sci. 2020, 12 (Suppl. S1), S114–S123. [Google Scholar]
- Li, W.; Ding, Q.; Sun, F.; Liu, B.; Yuan, F.; Zhang, L.; Bao, R.; Gu, J.; Lin, Y. Fatigue behavior of zirconia with microgrooved surfaces produced using femtosecond laser. Lasers Med. Sci. 2023, 38, 33. [Google Scholar] [CrossRef]
- Seo, S.H.; Kim, J.E.; Nam, N.E.; Moon, H.S. Effect of air abrasion, acid etching, and aging on the shear bond strength with resin cement to 3Y-TZP zirconia. J. Mech. Behav. Biomed. Mater. 2022, 134, 105348. [Google Scholar] [CrossRef]
- Su, N.; Yue, L.; Liao, Y.; Liu, W.; Zhang, H.; Li, X.; Wang, H.; Shen, J. The effect of various sandblasting conditions on surface changes of dental zirconia and shear bond strength between zirconia core and indirect composite resin. J. Adv. Prosthodont. 2015, 7, 214–223. [Google Scholar] [CrossRef]
- Borges, G.A.; Sophr, A.M.; de Goes, M.F.; Sobrinho, L.C.; Chan, D.C. Effect of etching and airborne particle abrasion on the microstructure of different dental ceramics. J. Prosthet. Dent. 2003, 89, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Borba, M.; Benetti, P.; Pecho, O.E.; Alessandretti, R.; Mosele, J.C.; Mores, R.T. Adhesion to dental ceramics. Curr. Oral. Health Rep. 2014, 1, 232–238. [Google Scholar] [CrossRef]
- Nagarkar, S.; Theis-Mahon, N.; Perdigão, J. Universal dental adhesives: Current status, laboratory testing, and clinical performance. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107, 2121–2131. [Google Scholar] [CrossRef] [PubMed]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current status on lithium disilicate and zirconia: A narrative review. BMC Oral. Health 2019, 19, 134. [Google Scholar] [CrossRef]
- Yilmaz, A.D.; Okutan, Y. Effect of air-abrasion at pre- and/or post-sintered stage and hydrothermal aging on surface roughness, phase transformation, and flexural strength of multilayered monolithic zirconia. J. Biomed. Mater. Res. B Appl. Biomater. 2021, 109, 606–616. [Google Scholar] [CrossRef]
- Yamaguchi, H.; Ino, S.; Hamano, N.; Okada, S.; Teranaka, T. Examination of bond strength and mechanical properties of Y-TZP zirconia ceramics with different surface modifications. Dent. Mater. J. 2012, 31, 472–480. [Google Scholar] [CrossRef]
- Campos, F.; Souza, R.O.; Bottino, M.A.; Özcan, M. Fracture Strength, Failure Types, and Weibull Characteristics of Three-Unit Zirconia Fixed Dental Prostheses After Cyclic Loading: Effects of Veneering and Air-Abrasion Protocols. Int. J. Periodontics Restor. Dent. 2016, 36, 901–908. [Google Scholar] [CrossRef]
- Strasser, T.; Preis, V.; Behr, M.; Rosentritt, M. Roughness, surface energy, and superficial damages of CAD/CAM materials after surface treatment. Clin. Oral. Investig. 2018, 22, 2787–2797. [Google Scholar] [CrossRef]
- International Organization for Standardization. Dentistry, Adhesion, Notched-Edge Shear Bond Strength Test; International Organization for Standardization: Geneva, Switzerland, 2013; Available online: https://www.iso.org/standard/45285.html (accessed on 3 September 2024).
- Noro, A.; Kaneko, M.; Murata, I.; Yoshinari, M. Influence of surface topography and surface physicochemistry on wettability of zirconia (tetragonal zirconia polycrystal). J. Biomed. Mater. Res. B Appl. Biomater. 2013, 101, 355–363. [Google Scholar] [CrossRef]
- Schneider, C.A.; Rasband, W.S.; Eliceiri, K.W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 2012, 9, 671–675. [Google Scholar] [CrossRef]
- Strazzi-Sahyon, H.B.; Rocha, E.P.; AssunÇÃo, W.G.; Dos Santos, P.H. Role of adhesive systems on the luting interface’s thickness of ceramic laminate veneers. Braz. Oral. Res. 2020, 34, e063. [Google Scholar] [CrossRef]
| Material/Type | Composition (Manufacturers’ Data) | Manufacturer |
|---|---|---|
| Copran® Zri | (ZR) Group | Y2O3: 4.5–5.35%, Al2O3: 0.15–0.35%, Iron hydroxide3: 0–0.01%, Other Oxides: 0–0.06% | White Peaks, Essen, Germany |
| IPS e.max CAD (LDS) Group | SiO2: 57.0–80.0, Li2O: 11.0–19.0, K2O: 0.0–13.0, P2O5: 0.0–11.0, ZrO2: 0.0–8.0, ZnO: 0.0–8.0, Other and colouring oxides: 0.0–12.0 | Ivoclar Vivadent, Schaan, Liechtenstein |
| Maxcem Elite™ Self-Etch/Self-Adhesive Dual Cure Resin Cement. | Hazardous Ingredients: Uncured Methacrylate Ester Monomers. Other ingredients: Non-hazardous inert mineral fillers, Ytterbium Fluoride, activators, stabilizers, and colorants. | Kerr, Brea, CA, USA |
| 3M™ Single Bond Universal Adhesive | MDP phosphate Monomer, Dimethacrylate resins, HEMA, Vitrebond Copolymer, Filler, Ethanol, Water, Initiators, Silane | 3M, Saint Paul, MN, USA |
| Plasma Type | Type of Delivery Device Power | Model | Gas Medium | Duration | Distance to the Target | Power of Device |
|---|---|---|---|---|---|---|
| APPJ | Piezoelectric direct discharge | (Piezobrush PZ3, Relyon plasma, Regensburg, Germany) | Ambient Air | 30 s | 5 mm | 80% |
| Surface Tx/Materials | Contact Angle (°) Mean/Std Dev | |
|---|---|---|
| Lithium Disilicate | Zirconia | |
| (C) Control Group | 53.15 ± 3.61 A | 77.34 ± 6.03 A |
| (S) Sandblasting Group | 39.92 ± 2.52 B | 52.84 ± 4.51 B |
| (P) Plasma Group | 23.99 ± 5.03 C | 23.35 ± 5.51 D |
| (SP) Sandblasting + Plasma Group | 37.70 ± 4.16 B | 35.41 ± 5.13 C |
| Surface Tx | Mean/Std Dev (MPa) |
|---|---|
| (C) Control group | 6.42 ± 2.13 C |
| (S) Sandblasting group | 10.28 ± 2.15 A |
| (P) Plasma group | 10.31 ± 1.68 A |
| (SP) Sandblasting + plasma group | 10.33 ± 2.35 A |
| (SN) Sandblasting + universal adhesive group | 8.77 ± 1.85 A,B |
| (PN) Plasma + universal adhesive group | 6.94 ± 1.87 B,C |
| (SPN) Sandblasting + plasma + universal adhesive group | 8.20 ± 2.44 B,C |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alalawi, H.; Al Mutairi, Z.; Al Abbasi, O.; Al Dossary, F.; Husain, M.; Al Ghubari, F.; Akhtar, S.; Abdalla, M.A. Efficacy of Atmospheric Pressure Plasma Jet-Induced Surface Treatment on Wettability, Surface Topography, and Shear Bond Strength of Ceramic Surfaces for CAD-On Assembly. Prosthesis 2024, 6, 1228-1239. https://doi.org/10.3390/prosthesis6050088
Alalawi H, Al Mutairi Z, Al Abbasi O, Al Dossary F, Husain M, Al Ghubari F, Akhtar S, Abdalla MA. Efficacy of Atmospheric Pressure Plasma Jet-Induced Surface Treatment on Wettability, Surface Topography, and Shear Bond Strength of Ceramic Surfaces for CAD-On Assembly. Prosthesis. 2024; 6(5):1228-1239. https://doi.org/10.3390/prosthesis6050088
Chicago/Turabian StyleAlalawi, Haidar, Ziyad Al Mutairi, Omar Al Abbasi, Fatima Al Dossary, Manayer Husain, Faleh Al Ghubari, Sultan Akhtar, and Moamen A. Abdalla. 2024. "Efficacy of Atmospheric Pressure Plasma Jet-Induced Surface Treatment on Wettability, Surface Topography, and Shear Bond Strength of Ceramic Surfaces for CAD-On Assembly" Prosthesis 6, no. 5: 1228-1239. https://doi.org/10.3390/prosthesis6050088
APA StyleAlalawi, H., Al Mutairi, Z., Al Abbasi, O., Al Dossary, F., Husain, M., Al Ghubari, F., Akhtar, S., & Abdalla, M. A. (2024). Efficacy of Atmospheric Pressure Plasma Jet-Induced Surface Treatment on Wettability, Surface Topography, and Shear Bond Strength of Ceramic Surfaces for CAD-On Assembly. Prosthesis, 6(5), 1228-1239. https://doi.org/10.3390/prosthesis6050088








