Survival of Chairside Posterior Single Crowns Made from InCoris TZI Zirconia—A Retrospective Analysis up to 10 Years
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
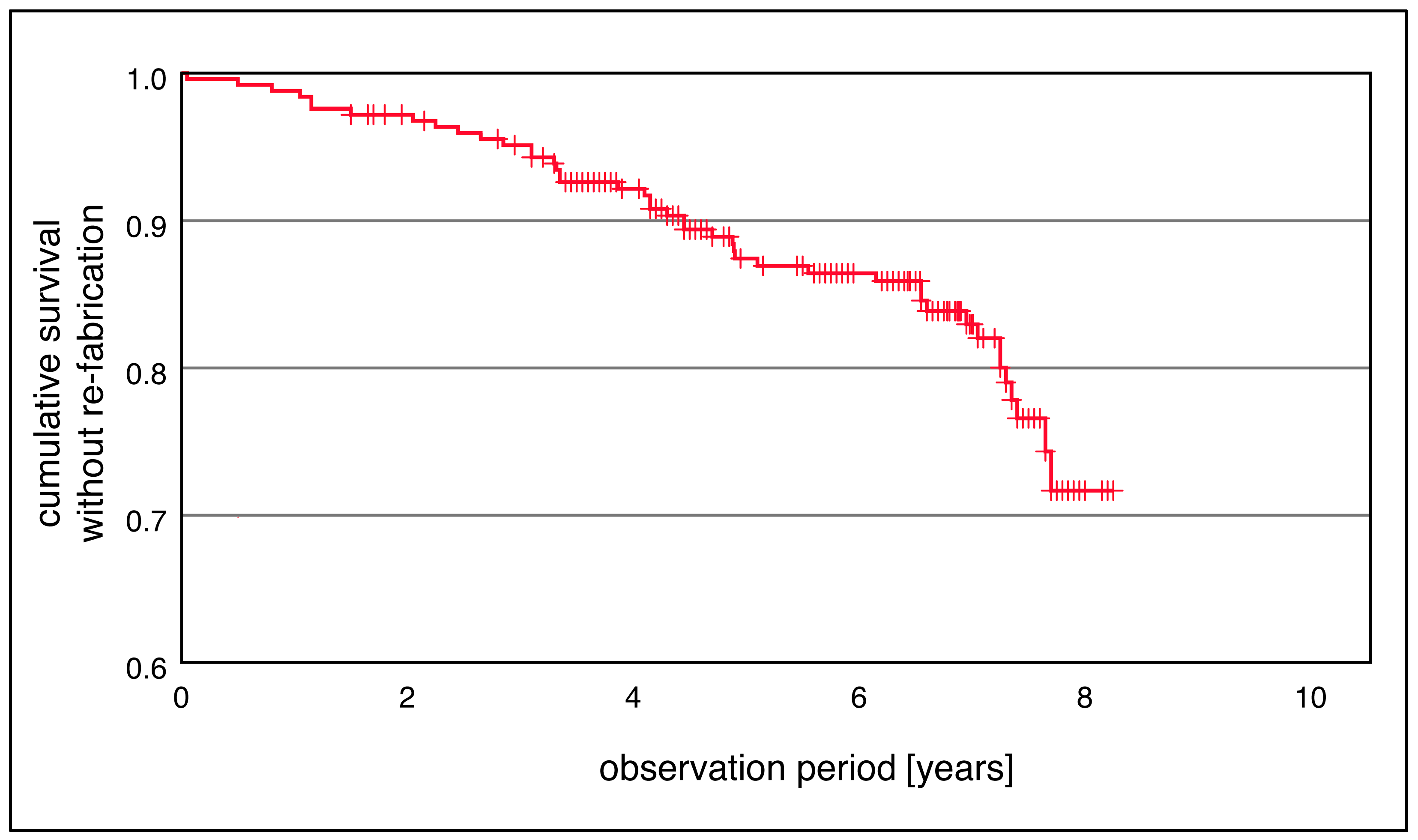
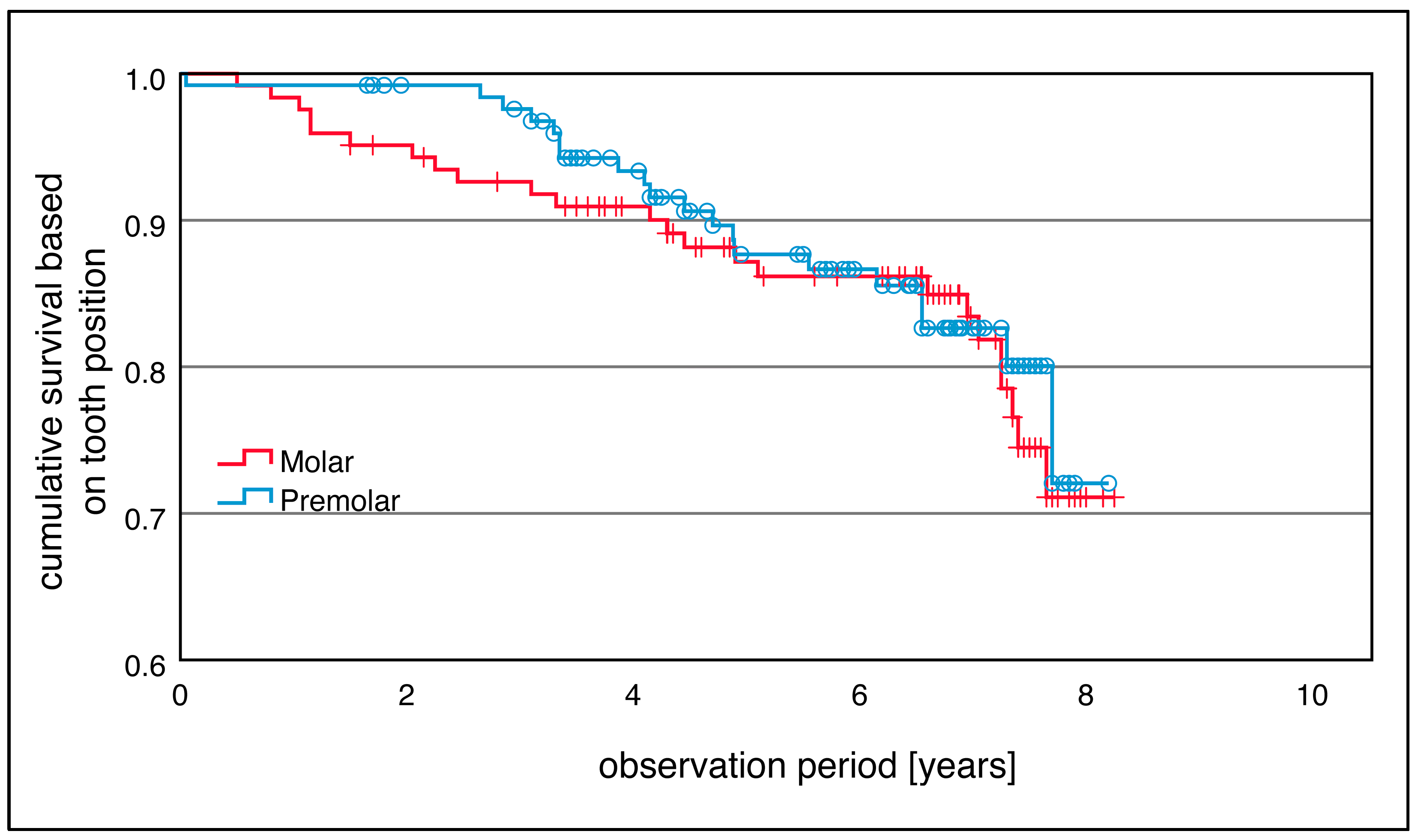
2.2. Statistical Analysis
- Duration until replacement (time in years until the end of the functional period);
- Duration until the first intervention (time in years).
2.3. Fabrication and Insertion
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Piconi, C.; Maccauro, G. Zirconia as a ceramic biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Filser, F.; Kocher, P.; Weibel, F.; Luthy, H.; Scharer, P.; Gauckler, L.J. Reliability and strength of all-ceramic dental restorations fabricated by direct ceramic machining (DCM). Int. J. Comput. Dent. 2001, 4, 89–106. [Google Scholar] [PubMed]
- Luthy, H.; Filser, F.; Loeffel, O.; Schumacher, M.; Gauckler, L.J.; Hammerle, C.H. Strength and reliability of four-unit all-ceramic posterior bridges. Dent. Mater. 2005, 21, 930–937. [Google Scholar] [CrossRef] [PubMed]
- Sannino, G.; Germano, F.; Arcuri, L.; Bigelli, E.; Arcuri, C.; Barlattani, A. CEREC CAD/CAM Chairside System. Oral Implant. 2014, 7, 57–70. [Google Scholar]
- Fasbinder, D.J. Clinical performance of chairside CAD/CAM restorations. J. Am. Dent. Assoc. 2006, 137 (Suppl. S1), 22S–31S. [Google Scholar] [CrossRef]
- Schneider, O. Long-term Cerec 3D chairside bridges milled from IPS e.max CAD LT blocks. Int. J. Comput. Dent. 2016, 19, 239–255. [Google Scholar]
- Zimmer, S.; Gohlich, O.; Ruttermann, S.; Lang, H.; Raab, W.H.; Barthel, C.R. Long-term survival of Cerec restorations: A 10-year study. Oper. Dent. 2008, 33, 484–487. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Ozcan, M.; Hallmann, L.; Ender, A.; Mehl, A.; Hammerlet, C.H. The effect of zirconia sintering temperature on flexural strength, grain size, and contrast ratio. Clin. Oral. Investig. 2013, 17, 269–274. [Google Scholar] [CrossRef]
- Mazza, L.C.; Lemos, C.A.A.; Pesqueira, A.A.; Pellizzer, E.P. Survival and complications of monolithic ceramic for tooth-supported fixed dental prostheses: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 128, 566–574. [Google Scholar] [CrossRef]
- Kaizer, M.R.; Gierthmuehlen, P.C.; Dos Santos, M.B.; Cava, S.S.; Zhang, Y. Speed sintering translucent zirconia for chairside one-visit dental restorations: Optical, mechanical, and wear characteristics. Ceram. Int. 2017, 43, 10999–11005. [Google Scholar] [CrossRef]
- Jansen, J.U.; Lumkemann, N.; Letz, I.; Pfefferle, R.; Sener, B.; Stawarczyk, B. Impact of high-speed sintering on translucency, phase content, grain sizes, and flexural strength of 3Y-TZP and 4Y-TZP zirconia materials. J. Prosthet. Dent. 2019, 122, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Wiedhahn, K.; Fritzsche, G.; Wiedhahn, C.; Schenk, O. Zirconia crowns—The new standard for single-visit dentistry? Int. J. Comput. Dent. 2016, 19, 9–26. [Google Scholar]
- Inokoshi, M.; Zhang, F.; De Munck, J.; Minakuchi, S.; Naert, I.; Vleugels, J.; Van Meerbeek, B.; Vanmeensel, K. Influence of sintering conditions on low-temperature degradation of dental zirconia. Dent. Mater. 2014, 30, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Ebeid, K.; Wille, S.; Hamdy, A.; Salah, T.; El-Etreby, A.; Kern, M. Effect of changes in sintering parameters on monolithic translucent zirconia. Dent. Mater. 2014, 30, e419–e424. [Google Scholar] [CrossRef]
- Sen, N.; Sermet, I.B.; Cinar, S. Effect of coloring and sintering on the translucency and biaxial strength of monolithic zirconia. J. Prosthet. Dent. 2018, 119, 308.E1–308.E7. [Google Scholar] [CrossRef]
- Kim, M.J.; Ahn, J.S.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Effects of the sintering conditions of dental zirconia ceramics on the grain size and translucency. J. Adv. Prosthodont. 2013, 5, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Gómez, S.Y.; da Silva, A.L.; Gouvêa, D.; Castro, R.H.R.; Hotza, D. Nanocrystalline yttria-doped zirconia sintered by fast firing. Mater. Lett. 2016, 166, 196–200. [Google Scholar] [CrossRef]
- Ersoy, N.M.; Aydogdu, H.M.; Degirmenci, B.U.; Cokuk, N.; Sevimay, M. The effects of sintering temperature and duration on the flexural strength and grain size of zirconia. Acta Biomater. Odontol. Scand. 2015, 1, 43–50. [Google Scholar] [CrossRef]
- Lawson, N.C.; Maharishi, A. Strength and translucency of zirconia after high-speed sintering. J. Esthet. Restor. Dent. 2020, 32, 219–225. [Google Scholar] [CrossRef]
- Chen, D.-J.; Mayo, M.J. Rapid Rate Sintering of Nanocrystalline ZrO2−3 mol% Y2O3. J. Am. Ceram. Soc. 1996, 79, 906–912. [Google Scholar] [CrossRef]
- Cokic, S.M.; Vleugels, J.; Van Meerbeek, B.; Camargo, B.; Willems, E.; Li, M.; Zhang, F. Mechanical properties, aging stability and translucency of speed-sintered zirconia for chairside restorations. Dent. Mater. 2020, 36, 959–972. [Google Scholar] [CrossRef] [PubMed]
- Jerman, E.; Wiedenmann, F.; Eichberger, M.; Reichert, A.; Stawarczyk, B. Effect of high-speed sintering on the flexural strength of hydrothermal and thermo-mechanically aged zirconia materials. Dent. Mater. 2020, 36, 1144–1150. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lumkemann, N. Three generations of zirconia: From veneered to monolithic. Part II. Quintessence Int. 2017, 48, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Harada, A.; Inagaki, R.; Kanno, T.; Niwano, Y.; Milleding, P.; Ortengren, U. Fracture resistance of monolithic zirconia molar crowns with reduced thickness. Acta Odontol. Scand. 2015, 73, 602–608. [Google Scholar] [CrossRef]
- Tang, Z.; Zhao, X.; Wang, H.; Liu, B. Clinical evaluation of monolithic zirconia crowns for posterior teeth restorations. Med. 2019, 98, e17385. [Google Scholar] [CrossRef]
- Sailer, I.; Makarov, N.A.; Thoma, D.S.; Zwahlen, M.; Pjetursson, B.E. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent. Mater. 2015, 31, 603–623. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Sailer, I.; Latyshev, A.; Rabel, K.; Kohal, R.J.; Karasan, D. A systematic review and meta-analysis evaluating the survival, the failure, and the complication rates of veneered and monolithic all-ceramic implant-supported single crowns. Clin. Oral. Implant. Res. 2021, 32 (Suppl. S21), 254–288. [Google Scholar] [CrossRef]
- Leitao, C.; Fernandes, G.V.O.; Azevedo, L.P.P.; Araujo, F.M.; Donato, H.; Correia, A.R.M. Clinical performance of monolithic CAD/CAM tooth-supported zirconia restorations: Systematic review and meta-analysis. J. Prosthodont. Res. 2022, 66, 374–384. [Google Scholar] [CrossRef]
- Sola-Ruiz, M.F.; Baixauli-Lopez, M.; Roig-Vanaclocha, A.; Amengual-Lorenzo, J.; Agustin-Panadero, R. Prospective study of monolithic zirconia crowns: Clinical behavior and survival rate at a 5-year follow-up. J. Prosthodont. Res. 2021, 65, 284–290. [Google Scholar] [CrossRef]
- Sulaiman, T.A. Materials in digital dentistry-A review. J. Esthet. Restor. Dent. 2020, 32, 171–181. [Google Scholar] [CrossRef]
- Kontonasaki, E.; Rigos, A.E.; Ilia, C.; Istantsos, T. Monolithic Zirconia: An Update to Current Knowledge. Optical Properties, Wear, and Clinical Performance. Dent. J. 2019, 7, 90. [Google Scholar] [CrossRef] [PubMed]
- Sax, C.; Hammerle, C.H.; Sailer, I. 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int. J. Comput. Dent. 2011, 14, 183–202. [Google Scholar] [PubMed]
- Lops, D.; Mosca, D.; Casentini, P.; Ghisolfi, M.; Romeo, E. Prognosis of zirconia ceramic fixed partial dentures: A 7-year prospective study. Int. J. Prosthodont. 2012, 25, 21–23. [Google Scholar] [PubMed]
- Kontonasaki, E.; Giasimakopoulos, P.; Rigos, A.E. Strength and aging resistance of monolithic zirconia: An update to current knowledge. Jpn. Dent. Sci. Rev. 2020, 56, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current status on lithium disilicate and zirconia: A narrative review. BMC Oral Health 2019, 19, 134. [Google Scholar] [CrossRef]
- Blatz, M.B.; Conejo, J. The Current State of Chairside Digital Dentistry and Materials. Dent. Clin. North Am. 2019, 63, 175–197. [Google Scholar] [CrossRef]
- Baroudi, K.; Ibraheem, S.N. Assessment of Chair-side Computer-Aided Design and Computer-Aided Manufacturing Restorations: A Review of the Literature. J. Int. Oral Health 2015, 7, 96–104. [Google Scholar]
- Mayinger, F.; Pfefferle, R.; Reichert, A.; Stawarczyk, B. Impact of High-Speed Sintering of Three-Unit 3Y-TZP and 4Y-TZP Fixed Dental Prostheses on Fracture Load With and Without Artificial Aging. Int. J. Prosthodont. 2021, 34, 47–53. [Google Scholar] [CrossRef]
- Rauch, A.; Reich, S.; Dalchau, L.; Schierz, O. Clinical survival of chair-side generated monolithic lithium disilicate crowns:10-year results. Clin. Oral Investig. 2018, 22, 1763–1769. [Google Scholar] [CrossRef]
- Wiedhahn, K. From blue to white: New high-strength material for Cerec--IPS e.max CAD LT. Int. J. Comput. Dent. 2007, 10, 79–91. [Google Scholar]
- Hammoudi, W.; Trulsson, M.; Svensson, P.; Smedberg, J.I. Long-term results of a randomized clinical trial of 2 types of ceramic crowns in participants with extensive tooth wear. J. Prosthet. Dent. 2022, 127, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Valenti, M.; Valenti, A.; Schmitz, J.H.; Cortellini, D.; Canale, A. Survival analysis up to 7 years of 621 zirconia monolithic single crowns with feather-edge margins fabricated with a cast-free workflow starting from intraoral scans: A multicentric retrospective study. J. Prosthet. Dent. 2023, 129, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Waldecker, M.; Behnisch, R.; Rammelsberg, P.; Bomicke, W. Five-year clinical performance of monolithic and partially veneered zirconia single crowns-a prospective observational study. J. Prosthodont. Res. 2022, 66, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Zhou, S.; Lai, R.; Liu, R.; Ma, S.; Zhou, Z.; Longquan, S. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. J. Mech. Behav. Biomed. Mater. 2014, 35, 93–101. [Google Scholar] [CrossRef]
- Johansson, C.; Kmet, G.; Rivera, J.; Larsson, C.; Vult Von Steyern, P. Fracture strength of monolithic all-ceramic crowns made of high translucent yttrium oxide-stabilized zirconium dioxide compared to porcelain-veneered crowns and lithium disilicate crowns. Acta Odontol. Scand. 2014, 72, 145–153. [Google Scholar] [CrossRef]
- Hawthan, M.; Chrcanovic, B.R.; Larsson, C. Retrospective clinical study of tooth-supported single crowns: A multifactor analysis. Eur. J. Oral. Sci. 2022, 130, e12871. [Google Scholar] [CrossRef]
- Michailova, M.; Elsayed, A.; Fabel, G.; Edelhoff, D.; Zylla, I.M.; Stawarczyk, B. Comparison between novel strength-gradient and color-gradient multilayered zirconia using conventional and high-speed sintering. J. Mech. Behav. Biomed. Mater. 2020, 111, 103977. [Google Scholar] [CrossRef]
- Lumkemann, N.; Stawarczyk, B. Impact of hydrothermal aging on the light transmittance and flexural strength of colored yttria-stabilized zirconia materials of different formulations. J. Prosthet. Dent. 2021, 125, 518–526. [Google Scholar] [CrossRef]
- Elisa Kauling, A.; Guth, J.F.; Erdelt, K.; Edelhoff, D.; Keul, C. Influence of speed sintering on the fit and fracture strength of 3-unit monolithic zirconia fixed partial dentures. J. Prosthet. Dent. 2020, 124, 380–386. [Google Scholar] [CrossRef]
- Nakamura, T.; Nakano, Y.; Usami, H.; Okamura, S.; Wakabayashi, K.; Yatani, H. In vitro investigation of fracture load and aging resistance of high-speed sintered monolithic tooth-borne zirconia crowns. J. Prosthodont. Res. 2020, 64, 182–187. [Google Scholar] [CrossRef]
- Soult, M.D.; Lien, W.; Savett, D.A.; Gallardo, F.F.; Vandewalle, K.S. Effect of high-speed sintering on the properties of a zirconia material. Gen. Dent. 2019, 67, 30–34. [Google Scholar] [PubMed]
- Quinn, J.B.; Quinn, G.D. A practical and systematic review of Weibull statistics for reporting strengths of dental materials. Dent. Mater. 2010, 26, 135–147. [Google Scholar] [CrossRef]
- Adolfsson, E.; Shen, J.Z. Advanced Ceramics for Dentistry: Chapter 17. Defect Minimization in Prosthetic Ceramics; Elsevier Inc.: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Heintze, S.D.; Cavalleri, A.; Forjanic, M.; Zellweger, G.; Rousson, V. Wear of ceramic and antagonist—A systematic evaluation of influencing factors in vitro. Dent. Mater. 2008, 24, 433–449. [Google Scholar] [CrossRef]
- Park, J.H.; Park, S.; Lee, K.; Yun, K.D.; Lim, H.P. Antagonist wear of three CAD/CAM anatomic contour zirconia ceramics. J. Prosthet. Dent. 2014, 111, 20–29. [Google Scholar] [CrossRef]
- Beuer, F.; Stimmelmayr, M.; Gueth, J.F.; Edelhoff, D.; Naumann, M. In vitro performance of full-contour zirconia single crowns. Dent. Mater. 2012, 28, 449–456. [Google Scholar] [CrossRef]
- May, L.G.; Passos, S.P.; Capelli, D.B.; Ozcan, M.; Bottino, M.A.; Valandro, L.F. Effect of silica coating combined to a MDP-based primer on the resin bond to Y-TZP ceramic. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 95, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Passos, S.P.; May, L.G.; Barca, D.C.; Ozcan, M.; Bottino, M.A.; Valandro, L.F. Adhesive quality of self-adhesive and conventional adhesive resin cement to Y-TZP ceramic before and after aging conditions. Oper. Dent. 2010, 35, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, M.; Kerkdijk, S.; Valandro, L.F. Comparison of resin cement adhesion to Y-TZP ceramic following manufacturers’ instructions of the cements only. Clin. Oral Investig. 2008, 12, 279–282. [Google Scholar] [CrossRef]
- Ozcan, M.; Cura, C.; Valandro, L.F. Early bond strength of two resin cements to Y-TZP ceramic using MPS or MPS/4-META silanes. Odontol 2011, 99, 62–67. [Google Scholar] [CrossRef]
- Thammajaruk, P.; Guazzato, M.; Naorungroj, S. Cleaning methods of contaminated zirconia: A systematic review and meta-analysis. Dent. Mater. 2023, 39, 235–245. [Google Scholar] [CrossRef]
- Quigley, N.P.; Loo, D.S.S.; Choy, C.; Ha, W.N. Clinical efficacy of methods for bonding to zirconia: A systematic review. J. Prosthet. Dent. 2021, 125, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Awad, M.M.; Alhalabi, F.; Alzahrani, K.M.; Almutiri, M.; Alqanawi, F.; Albdiri, L.; Alshehri, A.; Alrahlah, A.; Ahmed, M.H. 10-Methacryloyloxydecyl Dihydrogen Phosphate (10-MDP)-Containing Cleaner Improves Bond Strength to Contaminated Monolithic Zirconia: An In-Vitro Study. Mater. 2022, 15, 1023. [Google Scholar] [CrossRef] [PubMed]
- Amaral, R.; Ozcan, M.; Bottino, M.A.; Valandro, L.F. Microtensile bond strength of a resin cement to glass infiltrated zirconia-reinforced ceramic: The effect of surface conditioning. Dent. Mater. 2006, 22, 283–290. [Google Scholar] [CrossRef] [PubMed]
- D’Amario, M.; Campidoglio, M.; Morresi, A.L.; Luciani, L.; Marchetti, E.; Baldi, M. Effect of thermocycling on the bond strength between dual-cured resin cements and zirconium-oxide ceramics. J. Oral Sci. 2010, 52, 425–430. [Google Scholar] [CrossRef]
- Ozcan, M.; Vallittu, P.K. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent. Mater. 2003, 19, 725–731. [Google Scholar] [CrossRef]
- Tian, F.; Londono, J.; Villalobos, V.; Pan, Y.; Ho, H.X.; Eshera, R.; Sidow, S.J.; Bergeron, B.E.; Wang, X.; Tay, F.R. Effectiveness of different cleaning measures on the bonding of resin cement to saliva-contaminated or blood-contaminated zirconia. J. Dent. 2022, 120, 104084. [Google Scholar] [CrossRef]
- Del Carpio-Perochena, A.; Monteiro Bramante, C.; Hungaro Duarte, M.; Bombarda de Andrade, F.; Zardin Graeff, M.; Marciano da Silva, M.; Cavalini Cavenago, B.; Lucas Fernandes, S. Effect of Temperature, Concentration and Contact Time of Sodium Hypochlorite on the Treatment and Revitalization of Oral Biofilms. J. Dent. Res. Dent. Clin. Dent. Prospect. 2015, 9, 209–215. [Google Scholar] [CrossRef]
- Taneja, S.; Mishra, N.; Malik, S. Comparative evaluation of human pulp tissue dissolution by different concentrations of chlorine dioxide, calcium hypochlorite and sodium hypochlorite: An in vitro study. J. Conserv. Dent. 2014, 17, 541–545. [Google Scholar] [CrossRef]
- Abou-Rass, M.; Oglesby, S.W. The effects of temperature, concentration, and tissue type on the solvent ability of sodium hypochlorite. J. Endod. 1981, 7, 376–377. [Google Scholar] [CrossRef]
- Abuhaimed, T.S.; Abou Neel, E.A. Sodium Hypochlorite Irrigation and Its Effect on Bond Strength to Dentin. BioMed Res. Int. 2017, 2017, 1930360. [Google Scholar] [CrossRef]
- Santos, J.N.; Carrilho, M.R.; De Goes, M.F.; Zaia, A.A.; Gomes, B.P.; Souza-Filho, F.J.; Ferraz, C.C. Effect of chemical irrigants on the bond strength of a self-etching adhesive to pulp chamber dentin. J. Endod. 2006, 32, 1088–1090. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.D.; Lee, K.W.; Agee, K.A.; Bouillaguet, S.; Pashley, D.H. Effects of sodium hypochlorite and RC-prep on bond strengths of resin cement to endodontic surfaces. J. Endod. 2001, 27, 753–757. [Google Scholar] [CrossRef] [PubMed]
- Abou Neel, E.A.; Knowles, J.C.; Bozec, L. Effect of sodium hypochlorite on adhesive charactersitics of dentin: A systematic review of laboratory-based testing. Int. J. Adhes. Adhes. 2019, 95, 102419. [Google Scholar] [CrossRef]
- Cecchin, D.; Farina, A.P.; Bedran-Russo, A.K. Efficacy of Natural Collagen Crosslinkers on the Compromised Adhesive Bond Strength to NaOCl-treated Pulp Chamber Dentin. J. Adhes. Dent. 2018, 20, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.C.; Mak, Y.F.; Cheung, G.S.; Osorio, R.; Toledano, M.; Carvalho, R.M.; Tay, F.R.; Pashley, D.H. Reversal of compromised bonding to oxidized etched dentin. J. Dent. Res. 2001, 80, 1919–1924. [Google Scholar] [CrossRef]
- Curtis, S.R.; Richards, M.W.; Meiers, J.C. Early erosion of glass-ionomer cement at crown margins. Int. J. Prosthodont. 1993, 6, 553–557. [Google Scholar]
- Tuygunov, N.; Zakaria, M.N.; Yahya, N.A.; Abdul Aziz, A.; Cahyanto, A. Efficacy and bone-contact biocompatibility of glass ionomer cement as a biomaterial for bone regeneration: A systematic review. J. Mech. Behav. Biomed. Mater. 2023, 146, 106099. [Google Scholar] [CrossRef]


| Event | Replacement or Loss | First Intervention | ||
|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |
| Loss of retention | 3 | 1.2% | 13 | 5.2% |
| Irreparable fracture | 6 | 2.4% | 6 | 2.4% |
| Reparable fracture | 4 | 1.6% | 12 | 4.8% |
| Periodontal complications | 2 | 0.8% | 14 | 5.6% |
| Endodontic complications | 5 | 2% | 15 | 6.0% |
| Caries or secondary caries | 3 | 1.2% | 7 | 2.8% |
| Tooth fracture | 4 | 1.6% | 4 | 1.6% |
| Extraction | 9 | 3.6% | 9 | 3.6% |
| Prosthetic re-planning | 8 | 3.2% | 8 | 3.2% |
| Total | 44 | 17.6% | 88 | 35.2% |
| Type of Tooth | Mean | ||||||
| Number | Percentage | Censored | Estimator | SEM | 95% Confidence Interval | ||
| Lower Bound | Upper Bound | ||||||
| Molar | 123 | 49% | 99 | 7.341 | 0.183 | 6.981 | 7.700 |
| Premolar | 127 | 51% | 107 | 7.475 | 0.153 | 7.176 | 7.775 |
| Total | 250 | 100% | 206 | 7.425 | 0.120 | 7.191 | 7.659 |
| Cement | Mean | ||||||
| Number | Percentage | Censored | Estimator | SEM | 95% Confidence Interval | ||
| Lower Bound | Upper Bound | ||||||
| RelyX™ Unicem | 86 | 34% | 73 | 6.975 | 0.212 | 6.559 | 7.391 |
| Ketac™ Cem | 98 | 39% | 82 | 7.529 | 0.178 | 7.181 | 7.878 |
| Coltène DuoCem® | 66 | 26% | 51 | 7.393 | 0.213 | 6.975 | 7.810 |
| Total | 250 | 100% | 206 | 7.425 | 0.120 | 7.191 | 7.659 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neuhöffer, J.J.; Stoilov, L.; Enkling, N.; Stark, H.; Kraus, D.; Stoilov, M. Survival of Chairside Posterior Single Crowns Made from InCoris TZI Zirconia—A Retrospective Analysis up to 10 Years. Prosthesis 2024, 6, 1118-1132. https://doi.org/10.3390/prosthesis6050081
Neuhöffer JJ, Stoilov L, Enkling N, Stark H, Kraus D, Stoilov M. Survival of Chairside Posterior Single Crowns Made from InCoris TZI Zirconia—A Retrospective Analysis up to 10 Years. Prosthesis. 2024; 6(5):1118-1132. https://doi.org/10.3390/prosthesis6050081
Chicago/Turabian StyleNeuhöffer, Julius Jules, Lea Stoilov, Norbert Enkling, Helmut Stark, Dominik Kraus, and Milan Stoilov. 2024. "Survival of Chairside Posterior Single Crowns Made from InCoris TZI Zirconia—A Retrospective Analysis up to 10 Years" Prosthesis 6, no. 5: 1118-1132. https://doi.org/10.3390/prosthesis6050081
APA StyleNeuhöffer, J. J., Stoilov, L., Enkling, N., Stark, H., Kraus, D., & Stoilov, M. (2024). Survival of Chairside Posterior Single Crowns Made from InCoris TZI Zirconia—A Retrospective Analysis up to 10 Years. Prosthesis, 6(5), 1118-1132. https://doi.org/10.3390/prosthesis6050081








