Cervical Margin Relocation: Effect of Crown, Endocrown and Onlay Margin Location and Material Type on the Fracture Resistance of Endodontically Treated Molars
Abstract
1. Introduction
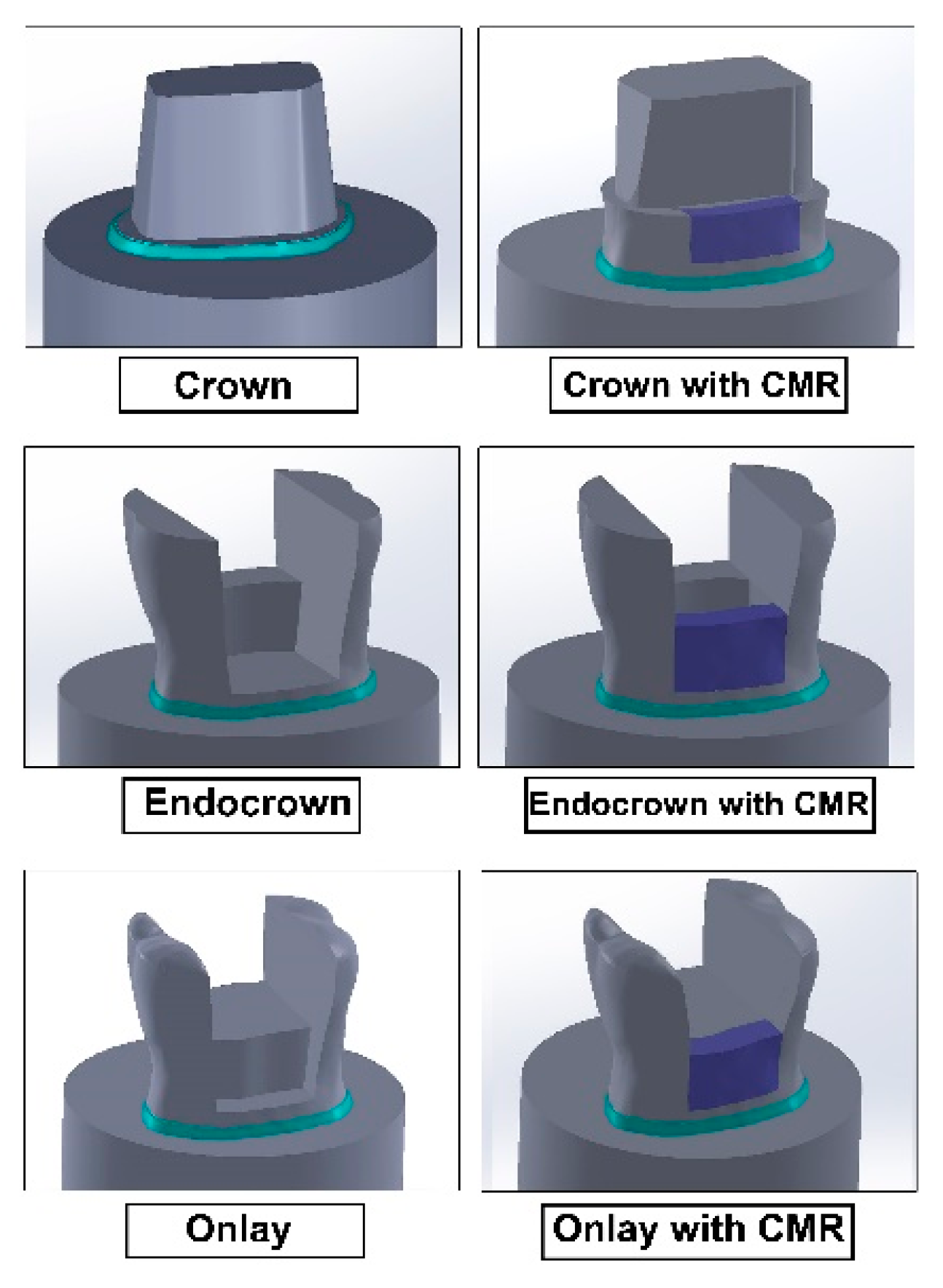
2. Materials and Methods
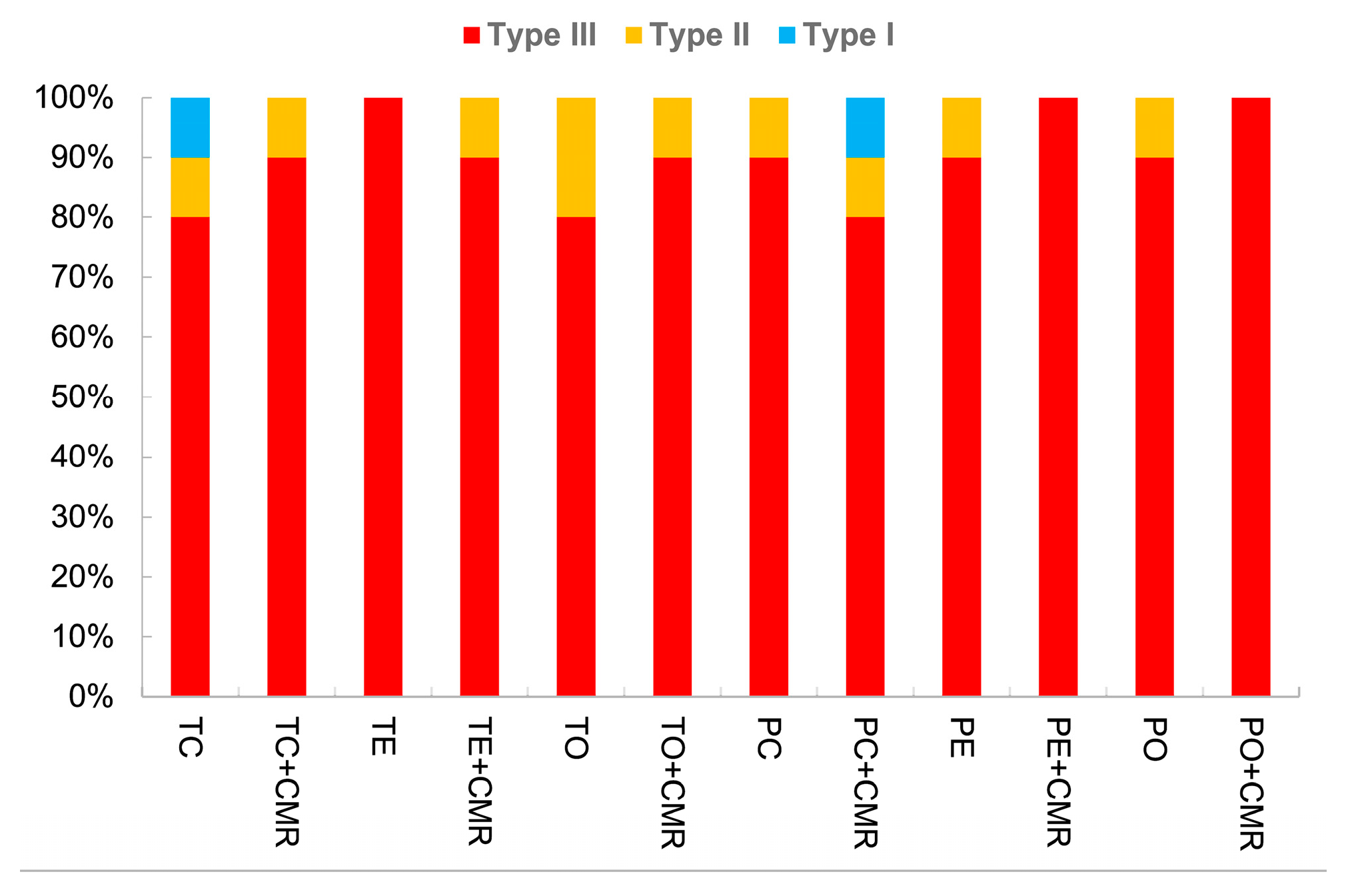
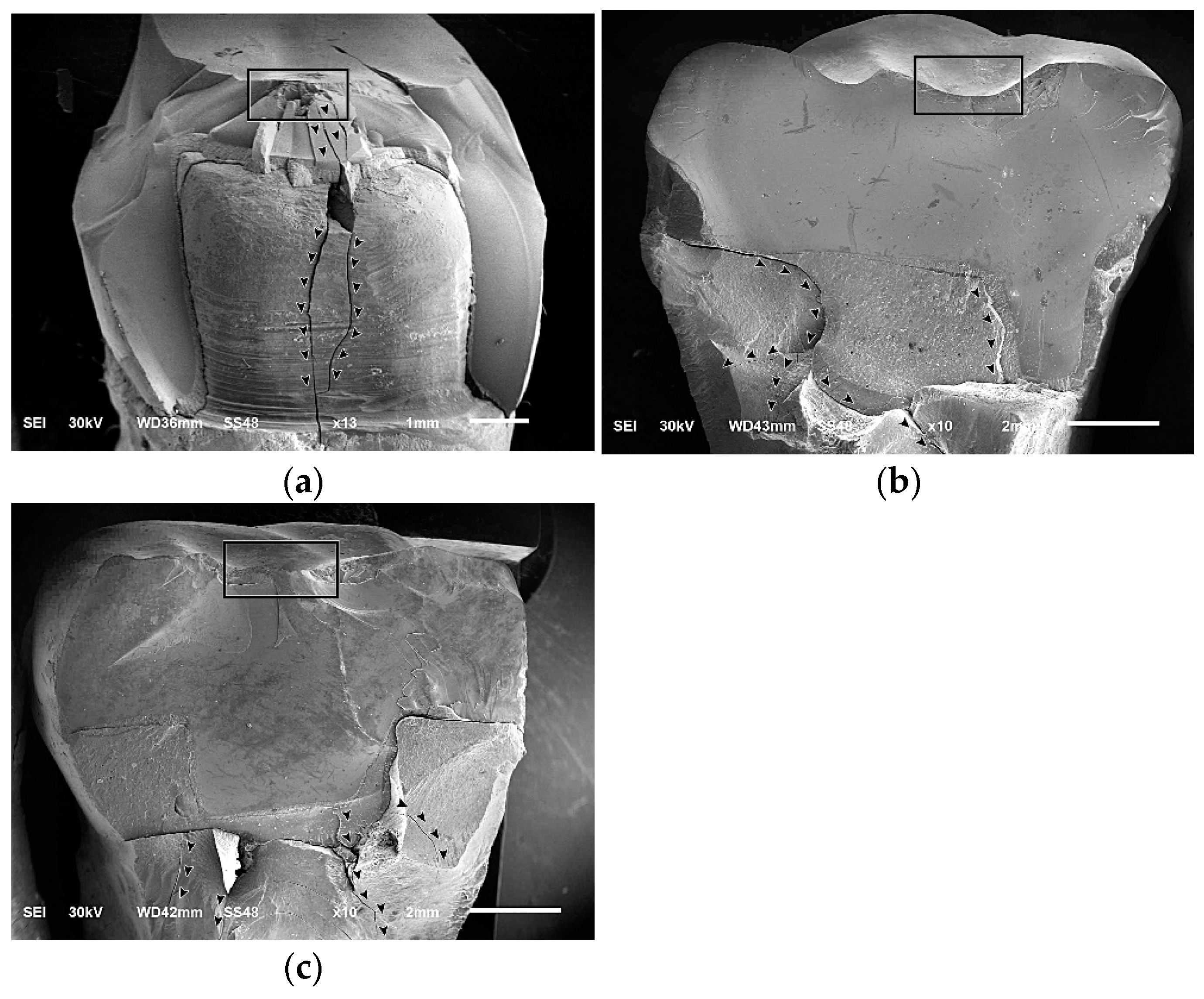
3. Results
4. Discussion
5. Conclusions
- (1)
- Margin location of the indirect restorations significantly affected the fracture resistance of the endodontically treated molars with an adverse effect of cervical margin relocation on the fracture resistance values in all study groups.
- (2)
- The material of the indirect restorations had no significant impact on the fracture resistance.
- (3)
- Crown restorations represented the best restorative option following endodontic treatment in terms of fracture resistance.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mugri, M.H.; Sayed, M.E.; Nedumgottil, B.M.; Bhandi, S.; Raj, A.T.; Testarelli, L.; Khurshid, Z.; Jain, S.; Patil, S. Treatment Prognosis of Restored Teeth with Crown Lengthening vs. Deep Margin Elevation: A Systematic Review. Materials 2021, 14, 6733. [Google Scholar] [CrossRef] [PubMed]
- Aldakheel, M.; Aldosary, K.; Alnafissah, S.; Alaamer, R.; Alqahtani, A.; Almuhtab, N. Deep margin elevation: Current concepts and clinical considerations: A review. Medicina 2022, 58, 1482. [Google Scholar] [CrossRef]
- Eggmann, F.; Ayub, J.M.; Conejo, J.; Blatz, M.B. Deep margin elevation-Present status and future directions. J. Esthet. Restor. Dent. 2023, 35, 26–47. [Google Scholar] [CrossRef]
- Bresser, R.A.; Naves, L.Z.; van der Made, S.A.M.; Cune, M.S.; Gresnigt, M.M.M. Deep margin elevation. A case report study. Int. J. Esthet. Dent. 2023, 18, 142–160. [Google Scholar]
- Geo, T.D.; Gupta, S.; Gupta, S.G.; Rana, K.S. Is Deep margin elevation a reliable tool for cervical margin relocation?—A comparative review. J. Oral. Biol. Craniofacial Res. 2024, 14, 360–361. [Google Scholar] [CrossRef]
- Dietschi, D.; Spreafico, R. Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract. Periodontics Aesthet. Dent. 1998, 10, 47–56. [Google Scholar] [PubMed]
- Magne, P. M-i-M for DME: Matrix-in-a-matrix technique for deep margin elevation. J. Prosthet. Dent. 2023, 130, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Samartzi, T.K.; Papalexopoulos, D.; Ntovas, P.; Rahiotis, C.; Blatz, M.B. Deep Margin Elevation: A Literature Review. Dent. J. 2022, 10, 48. [Google Scholar] [CrossRef]
- Bresser, R.A.; Carvalho, M.A.; Naves, L.Z.; Melma, H.; Cune, M.S.; Gresnigt, M.M.M. Biomechanical behavior of molars restored with direct and indirect restorations in combination with deep margin elevation. J. Mech. Behav. Biomed. Mater. 2024, 152, 106459. [Google Scholar] [CrossRef]
- Ilgenstein, I.; Zitzmann, N.U.; Bühler, J.; Wegehaupt, F.J.; Attin, T.; Weiger, R.; Krastl, G. Influence of proximal box elevation on the marginal quality and fracture behavior of root-filled molars restored with CAD/CAM ceramic or composite onlays. Clin. Oral. Investig. 2015, 19, 1021–1028. [Google Scholar] [CrossRef]
- Bresser, R.A.; van de Geer, L.; Gerdolle, D.; Schepke, U.; Cune, M.S.; Gresnigt, M.M.M. Influence of deep margin elevation and preparation design on the fracture strength of indirectly restored molars. J. Mech. Behav. Biomed. Mater. 2020, 110, 103950. [Google Scholar] [CrossRef] [PubMed]
- Grubbs, T.D.; Vargas, M.; Kolker, J.; Teixeira, E.C. Efficacy of direct restorative materials in proximal box elevation on the margin quality and fracture resistance of molars restored with CAD/CAM onlays. Oper. Dent. 2020, 45, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Li, H.; Cong, Q.; Zhang, Z.; Du, A.; Wang, Y. Effect of proximal box elevation on fracture resistance and microleakage of premolars restored with ceramic endocrowns. PLoS ONE 2021, 16, e0252269. [Google Scholar] [CrossRef]
- Mannocci, F.; Bitter, K.; Sauro, S.; Ferrari, P.; Austin, R.; Bhuva, B. Present status and future directions: The restoration of root filled teeth. Int. Endod. J. 2022, 55, 1059–1084. [Google Scholar] [CrossRef]
- Atalay, C.; Yazici, A.R.; Horuztepe, A.; Nagas, E.; Ertan, A.; Ozgunaltay, G. Fracture resistance of endodontically treated teeth restored with bulk fill, bulk fill flowable, fiber-reinforced, and conventional resin composite. Oper. Dent. 2016, 41, E131–E140. [Google Scholar] [CrossRef]
- Abdelfattah, R.A.; Nawar, N.N.; Kataia, E.M.; Saber, S.M. How loss of tooth structure impacts the biomechanical behavior of a single-rooted maxillary premolar: FEA. Odontology 2024, 112, 279–286. [Google Scholar] [CrossRef]
- Selvaraj, H.; Krithikadatta, J. Fracture Resistance of Endodontically Treated Teeth Restored With Short Fiber Reinforced Composite and a Low Viscosity Bulk Fill Composite in Class II Mesial-Occlusal-Distal Access Cavities: An Ex-Vivo Study. Cureus 2023, 15, e42798. [Google Scholar] [CrossRef]
- Frankenberger, R.; Zeilinger, I.; Krech, M.; Mörig, G.; Naumann, M.; Braun, A.; Krämer, N.; Roggendorf, M.J. Stability of endodontically treated teeth with differently invasive restorations: Adhesive vs. non-adhesive cusp stabilization. Dent. Mater. 2015, 31, 1312–1320. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Maksoud, H.B.; Eid, B.M.; Hamdy, M.; Abdelaal, H.M. Optimizing fracture resistance of endodontically treated maxillary premolars restored with preheated thermos-viscous composite post-thermocycling, a comparative study. Part I. BMC Oral. Health 2024, 24, 295. [Google Scholar] [CrossRef]
- Jurado, C.A.; El-Gendy, T.; Hyer, J.; Tsujimoto, A. Color stability of fully- and pre-crystalized chair-side CAD-CAM lithium disilicate restorations after required and additional sintering processes. J. Adv. Prosthodont. 2022, 14, 56–62. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, D.; Ding, H.; Chen, Q.; Meng, X. Fatigue behavior of endodontically treated maxillary premolars with MOD defects under different minimally invasive restorations. Clin. Oral. Investig. 2022, 26, 197–206. [Google Scholar] [CrossRef]
- Comba, A.; Baldi, A.; Carossa, M.; Michelotto Tempesta, R.; Garino, E.; Llubani, X.; Rozzi, D.; Mikonis, J.; Paolone, G.; Scotti, N. Post-fatigue fracture resistance of lithium disilicate and polymer-infiltrated ceramic network indirect restorations over endodontically-treated molars with different preparation designs: An in-vitro study. Polymers 2022, 14, 5084. [Google Scholar] [CrossRef] [PubMed]
- Veselinova, M.; Diamantopoulou, S.; Paximada, C.; Papazoglou, E. In-vitro comparison of fracture strength of endocrowns and overlays in endodontically treated teeth manufactured with monolithic lithium disilicate and zirconia. J. Funct. Biomater. 2023, 14, 422. [Google Scholar] [CrossRef]
- Yu, W.; Guo, K.; Zhang, B.; Weng, W. Fracture resistance of endodontically treated premolars restored with lithium disilicate CAD/CAM crowns or onlays and luted with two luting agents. Dent. Mater. J. 2014, 33, 349–354. [Google Scholar] [CrossRef]
- Morimoto, S.; Rebello de Sampaio, F.B.; Braga, M.M.; Sesma, N.; Özcan, M. Survival rate of resin and ceramic inlays, onlays, and overlays: A systematic review and meta-analysis. J. Dent. Res. 2016, 95, 985–994. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Fan, J.; Wang, L.; Xu, B.; Wang, L.; Chai, L. Onlays/partial crowns versus full crowns in restoring posterior teeth: A systematic review and meta-analysis. Head. Face Med. 2022, 18, 36. [Google Scholar] [CrossRef]
- Govare, N.; Contrepois, M. Endocrowns: A systematic review. J. Prosthet. Dent. 2020, 123, 411–418.e9. [Google Scholar] [CrossRef]
- Taha, D.; Spintzyk, S.; Sabet, A.; Wahsh, M.; Salah, T. Assessment of marginal adaptation and fracture resistance of endocrown restorations utilizing different machinable blocks subjected to thermomechanical aging. J. Esthet. Restor. Dent. 2018, 30, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Kassis, C.; Khoury, P.; Mehanna, C.Z.; Baba, N.Z.; Bou Chebel, F.; Daou, M.; Hardan, L. Effect of inlays, onlays and endocrown cavity design preparation on fracture resistance and fracture mode of endodontically treated teeth: An in vitro study. J. Prosthodont. 2021, 30, 625–631. [Google Scholar] [CrossRef]
- Sağlam, G.; Cengiz, S.; Karacaer, Ö. Marginal adaptation and fracture strength of endocrowns manufactured with different restorative materials: SEM and mechanical evaluation. Microsc. Res. Tech. 2021, 84, 284–290. [Google Scholar] [CrossRef]
- Lubauer, J.; Belli, R.; Peterlik, H.; Hurle, K.; Lohbauer, U. Grasping the lithium hype: Insights into modern dental lithium silicate glass-ceramics. Dent. Mater. 2022, 38, 318–332. [Google Scholar] [CrossRef] [PubMed]
- Al-Johani, H.; Haider, J.; Silikas, N.; Satterthwaite, J. Effect of surface treatments on optical, topographical and mechanical properties of CAD/CAM reinforced lithium silicate glass ceramics. Dent. Mater. 2023, 39, 779–789. [Google Scholar] [CrossRef] [PubMed]
- Elsaka, S.E.; Elnaghy, A.M. Mechanical properties of zirconia reinforced lithium silicate glass-ceramic. Dent. Mater. 2016, 32, 908–914. [Google Scholar] [CrossRef]
- Hamza, T.A.; Sherif, R.M. Fracture resistance of monolithic glass-ceramics versus bilayered zirconia-based restorations. J. Prosthodont. 2019, 28, e259–e264. [Google Scholar] [CrossRef]
- Manziuc, M.; Kui, A.; Chisnoiu, A.; Labuneț, A.; Negucioiu, M.; Ispas, A.; Buduru, S. Zirconia-Reinforced Lithium Silicate Ceramic in Digital Dentistry: A Comprehensive Literature Review of Our Current Understanding. Medicina 2023, 59, 2135. [Google Scholar] [CrossRef]
- D’Addazio, G.; Santilli, M.; Rollo, M.L.; Cardelli, P.; Rexhepi, I.; Murmura, G.; Al-Haj Husain, N.; Sinjari, B.; Traini, T.; Özcan, M.; et al. Fracture resistance of zirconia-reinforced lithium silicate ceramic crowns cemented with conventional or adhesive systems: An in vitro study. Materials 2020, 13, 2012. [Google Scholar] [CrossRef]
- Marchesi, G.; Camurri Piloni, A.; Nicolin, V.; Turco, G.; Di Lenarda, R. Chairside CAD/CAM materials: Current trends of clinical uses. Biology 2021, 10, 1170. [Google Scholar] [CrossRef]
- Jurado, C.A.; Bora, P.V.; Azpiazu-Flores, F.X.; Cho, S.H.; Afrashtehfar, K.I. Effect of resin cement selection on fracture resistance of chairside CAD-CAM lithium disilicate crowns containing virgilite: A comparative in vitro study. J. Prosthet. Dent. 2023. [Google Scholar] [CrossRef]
- Mario, D.; Mario, A.; Allegra, C.; Andrea, B.; Giuseppe, T.; Milena, C.; Annalisa, M.; Lorenzo, B.; Lorenzo, L.M.; Nicola, S. The influence of indirect bonded restorations on clinical prognosis of endodontically treated teeth: A systematic review and meta-analysis. Dent. Mater. 2022, 38, e203–e219. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Ferrari Cagidiaco, E.; Pontoriero, D.I.K.; Ercoli, C.; Chochlidakis, K. Survival rates of endodontically treated posterior teeth restored with all-ceramic partial-coverage crowns: When systematic review fails. Int. J. Environ. Res. Public Health 2022, 19, 1971. [Google Scholar] [CrossRef]
- Frankenberger, R.; Winter, J.; Dudek, M.C.; Naumann, M.; Amend, S.; Braun, A.; Krämer, N.; Roggendorf, M.J. Post-fatigue fracture and marginal behavior of endodontically treated teeth: Partial crown vs. full crown vs. endocrown vs. fiber-reinforced resin composite. Materials 2021, 14, 7733. [Google Scholar] [CrossRef] [PubMed]
- Shams, A.; Elsherbini, M.; Elsherbiny, A.A.; Özcan, M.; Sakrana, A.A. Rehabilitation of severely-destructed endodontically treated premolar teeth with novel endocrown system: Biomechanical behavior assessment through 3D finite element and in vitro analyses. J. Mech. Behav. Biomed. Mater. 2022, 126, 105031. [Google Scholar] [CrossRef] [PubMed]
- Kasem, A.T.; Elsherbiny, A.A.; Abo-Madina, M.; Tribst, J.P.M.; Al-Zordk, W. Effect of different designs of minimally invasive cantilever resin-bonded fixed dental prostheses replacing mandibular premolar: Long-term fracture load and 3D finite element analysis. J. Prosthodont. 2023, 32, e41–e51. [Google Scholar] [CrossRef]
- Aleisa, K.; Alwazzan, K.; Al-Dwairi, Z.N.; Almoharib, H.; Alshabib, A.; Aleid, A.; Lynch, E. Retention of zirconium oxide copings using different types of luting agents. J. Dent. Sci. 2013, 8, 392–398. [Google Scholar] [CrossRef]
- Robaian, A.; Alqahtani, A.; Alanazi, K.; Alanazi, A.; Almalki, M.; Aljarad, A.; Albaijan, R.; Maawadh, A.; Sufyan, A.; Mirza, M.B. Different designs of deep marginal elevation and its influence on fracture resistance of teeth with monolith zirconia full-contour crowns. Medicina 2023, 59, 661. [Google Scholar] [CrossRef] [PubMed]
- Alahmari, N.M.; Adawi, H.A.; Moaleem, M.M.A.; Alqahtani, F.M.; Alshahrani, F.T.; Aldhelai, T.A. Effects of the cervical marginal relocation technique on the marginal adaptation of lithium disilicate cad/cam ceramic crowns on premolars. J. Contemp. Dent. Pract. 2021, 22, 900–906. [Google Scholar]
- Steiner, M.; Mitsias, M.E.; Ludwig, K.; Kern, M. In vitro evaluation of a mechanical testing chewing simulator. Dent. Mater. 2009, 25, 494–499. [Google Scholar] [CrossRef]



| Material | Brand Name | Composition | Manufacturer | Lot Number |
|---|---|---|---|---|
| Advanced lithium disilicate glass ceramic | CEREC Tessera | 90% Li2Si2O5, 5% Li3PO4, 5% Li0.5Al0.5Si2.5O6 | Dentsply Sirona, USA | 16013947 |
| Zirconia-reinforced lithium silicate glass ceramic | Celtra Press | 58% SiO2, 18.5% Li2O, 10.1% ZrO2, 5% P2O5, 1.9% Al2O3, 2% CeO2, 1% Tb4O7 | Dentsply Sirona, USA | 16003549 |
| Self-adhesive, self-curing composite resin cement | Multilink Speed | Dimethacrylates, ytterbium trifluoride, co-polymer, glass filler (base only), silicon dioxide, adhesive monomer, initiators, stabilizers and pigments | Ivoclar Vivadent, Liechtenstein | Z02THB |
| Light-curing nano-hybrid composite resin | Tetric N- Ceram | BisGMA, Bis-EMA, TEGDMA, barium glass, ytterbium difluoride | Ivoclar Vivadent, Liechtenstein | Z016VJ |
| Light-curing nano-hybrid Flowable composite resin | Tetric N-Flow | UDMA, bis-GMA, TEGDMA | Ivoclar Vivadent, Liechtenstein | ZL039J |
| Ceramic etchant | Bisco porcelain etchant | 9.5% Buffered hydrofluoric acid gel | Bisco Inc., USA | 2100008544 |
| Pre-hydrolyzed silane primer | Bisco porcelain primer | 3-propyl-2-Methyl-2-Propenoic Acid, ethanol, acetone | Bisco Inc., USA | 2200005217 |
| Tooth etchant | N-Etch Etching Gel | 37% phosphoric acid, thickeners and pigments | Ivoclar Vivadent, Liechtenstein | Z03H0Y |
| Single-component light-curing adhesive | Tetric N-bond universal | Ethanol, phosphonic acid acrylate, Bis-GMA, HEMA, UDMA, diphenyl (2,4,6- trimethylbenzoyl) phosphine oxide | Ivoclar Vivadent, Liechtenstein | Z03WDZ |
| Type | Failure Pattern | Description |
|---|---|---|
| I | Restorable | Fracture within the restoration |
| II | Restorable | Fracture of the restoration and tooth above the CEJ |
| III | Unrestorable (catastrophic) | Fracture of the restoration and tooth below the CEJ |
| Material | Margin Location | Design | Fracture Resistance Mean ± SD | Test of Significance |
|---|---|---|---|---|
| Cerec Tessera | Without CMR | Crown | 1805.39 ± 267.64 | F = 0.514 p = 0.604 |
| Endocrown | 1763.44 ± 212.04 | |||
| Onlay | 1703.18 ± 193.43 | |||
| With CMR | Crown | 1530.08 ± 243.12 b | F = 8.99 p = 0.001 * | |
| Endocrown | 1340.11 ± 216.74 a | |||
| Onlay | 1057.19 ± 203.42 ab | |||
| Celtra Press | Without CMR | Crown | 2136.57 ± 216.41 ab | F = 21.76 p = 0.001 * |
| Endocrown | 1584.28 ± 205.41 a | |||
| Onlay | 1566.19 ± 236.38 b | |||
| With CMR | Crown | 1866.24 ± 219.81 bc | F = 44.26 p = 0.001 * | |
| Endocrown | 1356.90 ± 225.99 ab | |||
| Onlay | 950.47 ± 208.12 ac |
| Restoration Type | Without CMR | With CMR | ||
|---|---|---|---|---|
| CEREC Tessera | Celtra Press | CEREC Tessera | Celtra Press | |
| Crown | 1805.38 ± 267.64 A | 2136.57 ± 216.41 B | 1530.08 ± 243.01 C | 1866.24 ± 219.81 A |
| Endocrown | 1763.44 ± 212.04 A | 1584.28 ± 205.41 A | 1340.11 ± 216.74 B | 1356.90 ± 225.99 B |
| Onlay | 1703.18 ± 193.43 A | 1566.19 ± 236.38 A | 1057.19 ± 203.42 B | 950.47 ± 208.12 B |
| Source | Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Margin location | 5,035,063.352 | 1 | 5,035,063.352 | 102.569 | 0.001 * |
| Restoration type | 5,426,067.054 | 2 | 2,713,033.527 | 55.267 | 0.001 * |
| Material | 56,881.263 | 1 | 56,881.263 | 1.159 | 0.284 |
| Margin location × restoration type | 747,598.643 | 2 | 373,799.321 | 7.615 | 0.001 * |
| Margin location × material | 44,541.353 | 1 | 44,541.353 | 0.907 | 0.343 |
| Restoration type × material | 1,270,879.707 | 2 | 635,439.854 | 12.944 | 0.001 * |
| Margin location × restoration type × material | 53,808.213 | 2 | 26,904.107 | 0.548 | 0.580 |
| Error | 5,301,687.200 | 108 | 49,089.696 | ||
| Total | 3.081 × 108 | 120 | |||
| Corrected Total | 1.794 × 107 | 119 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diaa, M.; Al-Zordk, W.; Ozcan, M.; Sakrana, A. Cervical Margin Relocation: Effect of Crown, Endocrown and Onlay Margin Location and Material Type on the Fracture Resistance of Endodontically Treated Molars. Prosthesis 2024, 6, 1106-1117. https://doi.org/10.3390/prosthesis6050080
Diaa M, Al-Zordk W, Ozcan M, Sakrana A. Cervical Margin Relocation: Effect of Crown, Endocrown and Onlay Margin Location and Material Type on the Fracture Resistance of Endodontically Treated Molars. Prosthesis. 2024; 6(5):1106-1117. https://doi.org/10.3390/prosthesis6050080
Chicago/Turabian StyleDiaa, Mohamed, Walid Al-Zordk, Mutlu Ozcan, and Amal Sakrana. 2024. "Cervical Margin Relocation: Effect of Crown, Endocrown and Onlay Margin Location and Material Type on the Fracture Resistance of Endodontically Treated Molars" Prosthesis 6, no. 5: 1106-1117. https://doi.org/10.3390/prosthesis6050080
APA StyleDiaa, M., Al-Zordk, W., Ozcan, M., & Sakrana, A. (2024). Cervical Margin Relocation: Effect of Crown, Endocrown and Onlay Margin Location and Material Type on the Fracture Resistance of Endodontically Treated Molars. Prosthesis, 6(5), 1106-1117. https://doi.org/10.3390/prosthesis6050080








