1. Introduction
Acute anterior poliomyelitis (AAP), which has caused widespread morbidity and mortality in children during multiple epidemics in the last century, has become a rare condition in most Western countries thanks to a widespread policy of immunization. Nevertheless, a relatively large number of patients are still affected by deformities following this disease. Recently [
1], it has been estimated that there are at least 15 to 20 million polio survivors worldwide, and up to 30 to 40% of these could develop some form of post-polio syndrome (PPS), a progressive muscular weakness that may occur later in life. Data on the number of individuals living with orthopedics poliomyelitis sequelae in some occidental countries have been reported in the literature. In the USA, Jordan et al. [
2] have estimated that 650,000 patients are affected by deformities following this disease, whereas there are 120,000 in the UK [
3] and 70,000 in Italy [
4]. The sequelae of AAP knee deformities over time cause degenerative alterations of the joints, which can be treated by joint replacement.
Total knee arthroplasty with unconstrained or semi-constrained prostheses has resulted in good pain relief, but concerns have been raised regarding the recurrence of knee instability [
2,
5,
6]. The issue of whether to use constrained implants during knee arthroplasty in patients with AAP is still debated and concerns have been expressed due to increased stress transfer to the bone–implant interface and subsequent potential loosening of more constrained implants [
7,
8,
9]. The aim of our study was to evaluate the long-term results of a consecutive series of third-generation rotating hinge total knee arthroplasties (RHKs) in patients affected by poliomyelitis.
2. Materials and Methods
Between January 2000 and October 2021, 21 consecutive TKAs were performed in 20 patients affected by knee osteoarthritis following poliomyelitis, by the same senior orthopedic surgeons (TD) at three different institutions (Rizzoli Orthopedic Institute (Bologna, Italy), Santa Maria alle Scotte Hospital (Siena, Italy), and Maggiore C. A. Pizzardi Hospital Bologna, Italy). Four different types of implant were used: two constrained condylar implants (NexGen LCCK, Zimmer Biomet, Warsaw, IN, USA) one posterior stabilized implant ((NexGen LPS) (Zimmer Biomet, Warsaw, IN, USA), one intracondylar rotating hinge implant (Endomodel, Waldemar Link, Hamburg, Germany) with a titanium niobium nitride (TiNbN) surface coating for documented nickel allergy, and seventeen NexGen rotating hinge knees (NexGen RHKs) (Zimmer Biomet, Warsaw, IN, USA). Patients that received an implant other than a Nex Gen RHK were excluded in order to have more homogenous series. A total of 17 knees (16 patients) were included, of which 12 (11 patients) completed a minimum follow-up of 10 years. Two patients were lost to follow-up, whereas two others have still not reached the minimum follow-up of 10 years. Finally, another patient developed a joint infection 4 months after the index procedure. Five of these patients, including the patient complicated by infection, have been previously reported in an earlier follow-up [
10].
Our study therefore consisted of eleven patients (12 knees): nine females and two males, with an average age at the time of surgery of 57.1 years (range 51 to 77 years); the average age at the time of last follow-up was instead 70.2 years (range 63 to 88 years).
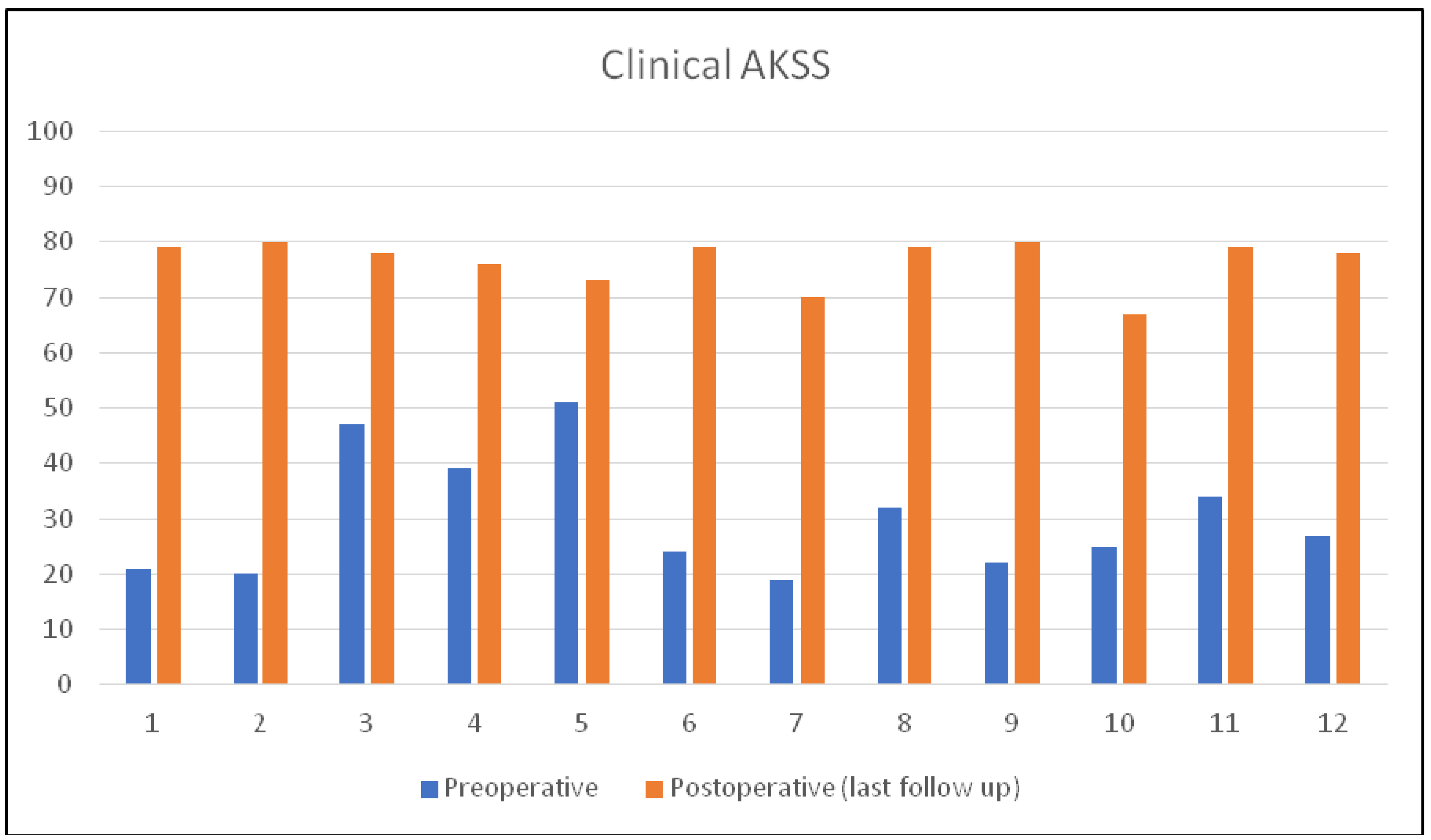
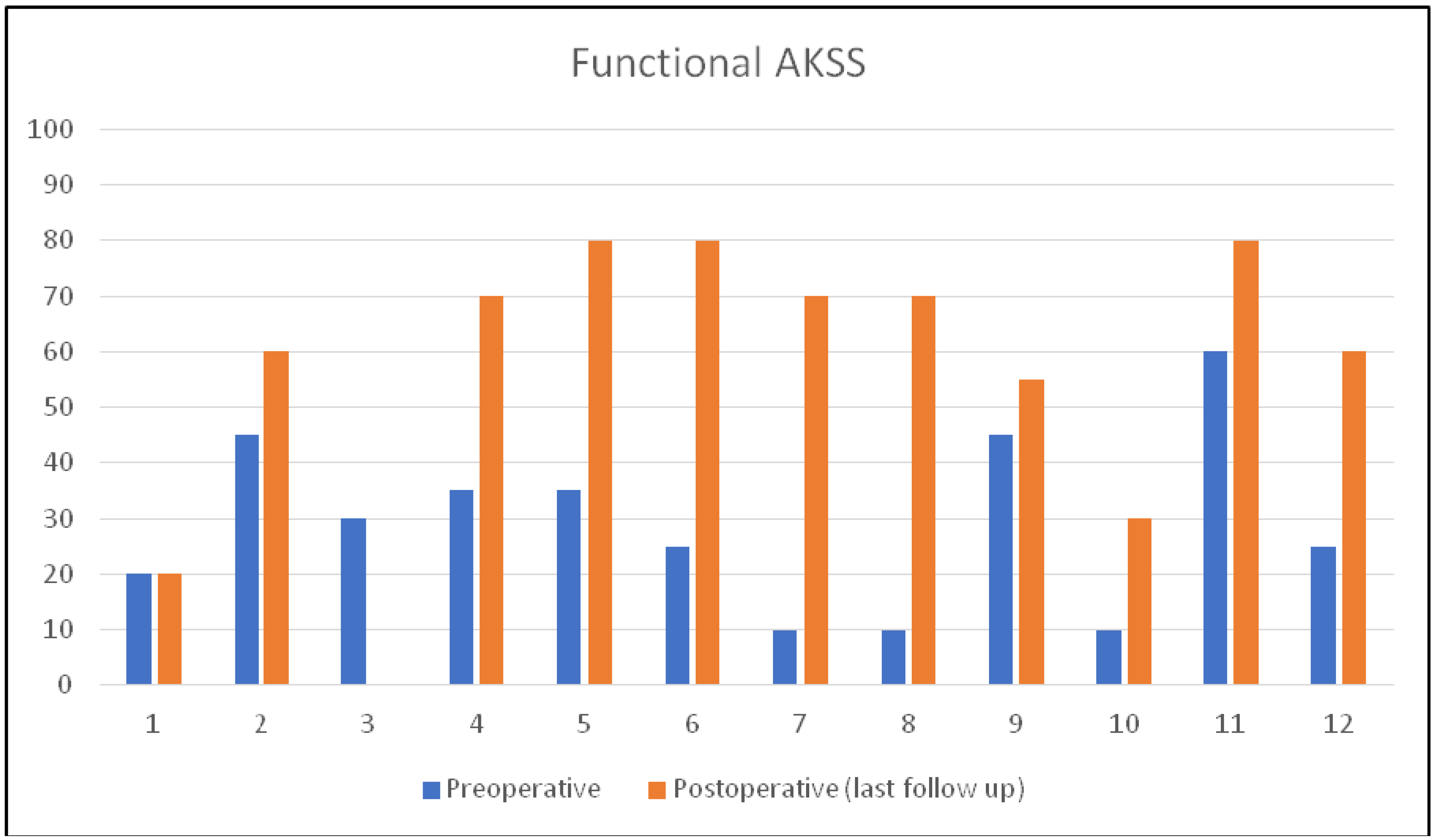
A preoperative clinical and functional assessment of each patient was performed using the American Knee Society Score (AKSS) [
11]. According to these parameters, an excellent score is defined as over 85, good between 70 and 84, fair between 60 and 69, and below 60 is considered poor. The preoperative clinical score in our series ranged from 21 to 51 with a mean of 30; the average functional score was 27.2 (range 10–60).
The quadriceps strength was assessed according to the Medical Research Council (MRC) scale [
12]: 0/5, no contraction—paralysis; 1/5, slight contraction; 2/5, contraction without gravity; 3/5, contraction against gravity; 4/5, contraction against minimum resistance; and 5/5, normal contraction. At the preoperative clinical evaluation, four patients achieved an MRC score of 0/5 for quadriceps muscle strength. In one patient, quadriceps strength was 1/5, in three cases it was 2/5, and in a further three cases it was 3/5; in no patient was the strength value inferior to 4/5 or normal.
An X-ray assessment was performed preoperatively and at last follow-up with a full weight-bearing panoramic view. Alignment on an antero-posterior view (hip–knee angle, HKA) and on a lateral view (procurvatum and recurvatum) was evaluated. The patellar height was measured according to the Insall–Salvati index [
13]. Particular attention was paid to checking for knee articular and extraarticular deformities. The diameter of the femoral and tibial intramedullary canals is often narrow in these patients [
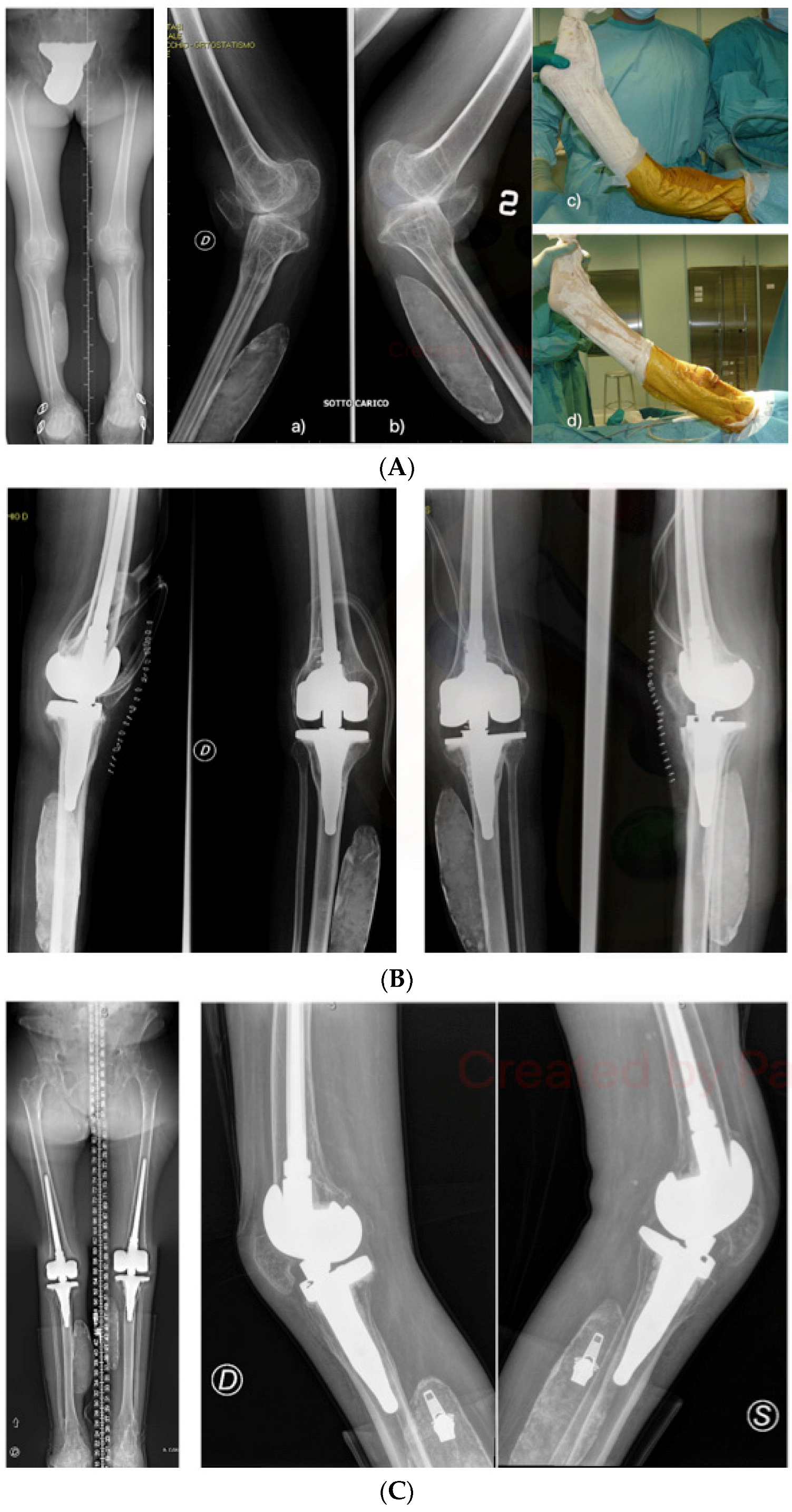
14] and was also evaluated on the preoperative X-rays. Preoperative radiographic evaluation revealed the following deformities: in 7 cases in the preoperative AP view, a varus deformity between 5 and 23 degrees was detected, while 5 patients had a valgus angulation between 4 and 13 degrees. On the lateral view, in 9 cases a recurvatum was present, with a mean value of 27.2° (range 5–60°) (
Table 1). In 11 cases, the patella was preoperatively “baja” according to the Insall–Salvati index (<0.8) [
13], while in one case it was “alta” (
Table 1). The patella was substituted in only two cases, both with a cementless trabecular implant.
In all patients, a standard medial parapatellar approach was performed. In all patients of the series, the release of the collateral ligaments was effectuated to reduce stress on the rotating hinge mechanism.
The implant used was a RHK NexGen Zimmer
TM (Trademark of Zimmer-Biomet
TM) in all cases. It is designed to maintain centralized contact throughout ROM (from −3° of hyperextension to 120° of flexion), resulting in 95% condylar loading through the tibial condyles. Theoretically, this design reduces stress on the constraint and on the stem–bone interface, minimizing the risk of implant breakage or aseptic loosening. Due to the limited dimensions of poliomyelitis knee, a non-modular tibial component was used in all but one case. It is a monoblock implant with an overall tibial stem length of 75 mm, where the diameter of the distal portion of the stem has been tapered so that it can be used for patients that have a small-diameter IM canal. Actually, the most distal centimeter of the stem is 9 mm in diameter, significantly smaller than the diameter of the modular version of the rotating hinge knee base plate (14.7 mm). A bowed femoral stem was used in 8 cases, while offset stems were used in 3 cases. In only one case the deformity following a previous supracondylar osteotomy of the femur made it necessary to implant a short (30 mm) straight femoral stem, which was completely cemented. If we excluded this case, both femoral and tibial components were cemented only around the metaphyseal portion [
15]. The diameter of the definitive stem was evaluated intraoperatively during reaming with hand drills, implanting stems with a diameter 1 mm smaller than the last reamer used. Particular attention was paid to allowing a slight hyperextension in order to preserve the patient’s ability to lock the knee in full extension during the loadbearing phase of the step [
10].
At the last follow-up X-ray assessment, any signs of aseptic loosening, osteolysis, and osteosclerosis were assessed according to the criteria defined by the Modern Knee Society radiographic evaluation system [
16].
The paired Wilcoxon signed rank test was then used to statistically compare preoperative AKSS to the last follow-up AKSS (threshold of significance: p-value < 0.05), to evaluate if RHK in polio patients guarantees a significant increase in clinical and functional score, even in the long-term.
3. Results
Of the fourteen patients included, two patients were lost to follow-up before they reach 10 years control, while for another patient the implant was removed due to infection four months after the index procedure and was submitted to knee fusion. Therefore, we had the possibility of evaluating twelve total knee arthroplasties in eleven patients (one patient underwent staged bilateral TKA). The mean follow-up was 154 months (min 120–max 216 months) (
Table 1).
Overall, there was a significant improvement in mean AKSS. At the last follow-up, the average AKSS clinical score improved from 30.08 points preoperatively (range 19–51) to 78.83 points (range 67–80) (
Figure 1), while the average AKSS function score improved from 29.17 (range 10–60) points to 56.25 points (range 0–80) (
Figure 2).
No patient reported an “excellent” outcome (>85 points) regarding the clinical AKSS, which evaluates the clinical profile with regard to pain intensity, total range of motion, flexion contractures, stability in the anteroposterior and mediolateral planes, and alignment. The outcome was “good” (70–84 points) in all cases, except one patient who scored 67 points due to limited knee range of motion.
The results of functional AKSS were less favorable, with no patient reporting an “excellent” outcome (>85 points) and only six patients reporting a “good” result (70–79 points). Two patients reported a “fair” outcome (69–60 points), whereas the remaining four patients had a “poor” score (<60 points). Among them, one patient developed post-polio syndrome (PPS) 13 years after surgery, at age 66; while not complaining of pain, nor were clinical or radiographic signs of instability recurrence or mobilization of the components observed, the patient lost her ambulatory autonomy due to important sthenic and muscular deficits of the limbs and trunk. At an intermediate follow-up in 2009, 3 years after surgery, she belonged to the “poor” score group with a functional score of 55 points.
The statistical analysis carried out with the paired Wilcoxon signed rank test compared the preoperative clinical and functional AKS scores to those observed at the last follow-up, highlighting a statistically significant increase for both (threshold of significance:
p-value < 0.05) (
Table 2).
We report only one intraoperative complication consisting of a femoral fracture at the tip of the stem which was stabilized with a plate and three cerclages. Knee active mobilization and toe touch weight bearing with crutches were granted immediately after surgery.
In one case, a missed and untreated transverse non-displaced traumatic fracture of the patella occurred three months after surgery for an accidental fall.
No cases of instability recurrence in recurvatum, implant failure, and revision were found over the long term.
The presence of peri-implant radiolucent lines proved to be sporadic at the last radiographic follow-up. According to the radiologic evaluation system described by Meneghini et al. [
16], they were found in one case at the anterior flange–bone interface of the femoral component (zone 1 on the latero-lateral view), in one case at the posterior femoral shield interface (zone 3P on the latero-lateral view), and in one case in zone 3 of the tibia on the antero-posterior view.
Radiosclerosis lines were frequently found around the stem extension, predominantly at the tip (areas 4 and 5) (
Table 3). In all cases, the radiolucent and sclerosis lines were partial, with a maximum width of 1 mm. In patients with intermediate radiographic follow-up, we did not observe any progression. Osteolysis was found in only one case, in tibial baseplate zone 2, both in antero-posterior and lateral views and with a maximum width of 4 mm (
Table 3).
4. Discussion
According to the prior literature and recent systematic reviews, TKA has provided predictable pain relief and functional improvement in polio patients with symptomatic knee arthritis and knee instability [
3,
7,
9,
10,
14]. However, the outcomes in these patients are worse than for the general population. Poor preoperative quadriceps function, instability, angular deformities, external rotation of the tibia, extraarticular deformities, and narrowness of the intramedullary canals are among the main features that make this surgery challenging [
9]. Short- and mid-term follow-up studies suggested that recurrent deformity remained a major problem, especially when less-constrained implants (cruciate retaining (CR), posterior-stabilized (PS), or constrained condylar knee (CCK)) are used [
5,
10,
17,
18]. The use of modern rotating hinge implants (RHKs) is recommended in the presence of less than antigravity quadriceps strength, finding several confirmations in the literature [
7,
9,
10,
17]. However, concerns exist regarding increased stress at the prosthesis–bone interface when an RHK implant is used. In our series, all but three patients had less than antigravity strength. That was the only criterion we used to address our implant choice independently of frontal or assial preoperative deformity. We have also to consider a possible functional decline caused by post-polio syndrome, which can negatively affect the choice of a less-constrained implant.
To compensate for the incompetence of the quadriceps muscle and avoid knee flexion collapse, the line of gravity must remain anterior to the knee. The upright position in the polio patient is, for this reason, guaranteed by a compensation mechanism that balances the load axis: the block in hyperextension of the knee (genu recurvatum) [
19]. Correcting this deformity completely during surgery may lead to loss of the compensatory mechanism and an unsatisfactory functional result [
6]. At the same time, however, maintaining knee hyperextension may result in increased stress on the soft tissues and on the implant, increasing the risk of recurrence of the deformity [
5,
6].
In the series reported in the present study, hyperextension was the most frequently encountered deformity in the preoperative phase: recurvatum was present in 9 cases out of 12 and in some patients it was found to be of an extreme degree (
Table 1;
Figure 3). In all cases, in order to preserve the functional compensation mechanism, a minimal postoperative residual knee hyperextension was guaranteed (about 3°, built-in in the Zimmer NexGen
TM implant design).
We have not reported any cases of mechanical failure at long-term follow-up, probably thanks to the use of third-generation RHK implants, which unload 95% of the femoral load on the tibial condyles. This preserves the structural integrity of the constraint and reduces stress transfer to the implant–bone interface [
20]. In constrained prostheses, the stems have the important function of increasing the bone–implant interface area, allowing forces to be distributed and relieving stress on the constraint [
21]. In our experience, we have used a hybrid cementation technique, placing the cement only in the metaphyseal area. In only one case, the deformity following a previous supracondylar osteotomy of the femur made it necessary to implant a short (30 mm) cemented straight femoral stem. At the final follow-up, we did not find any cases of aseptic loosening of the implant. The results are in agreement with what was previously reported by Sah et al. [
15], who reported long-term survival rates of hybrid cemented revision implants comparable to those of fully cemented stems. In radiographic controls, the sporadic radiolucent lines observed did not appear progressive and were not related to clinical symptoms or signs of implant loosening. To minimize the potential for tibial fracture, all but one patient was submitted to non-modular tibial implants. In this solution, the distal portion of the stem has been tapered, reducing the diameter to 9 mm instead of 14.7 mm. Therefore, the non-modular tibial component can be considered the preferred solution for patients with a small diameter of the tibial canal such as poliomyelitis. Although the results observed were inferior to those of standard knee replacement in the general population, the long-term outcome could be considered satisfactory. We observed a statistically significant improvement of more than 40 points for the clinical score (
p-value: 0.003) and of almost 25 points for the functional score (
p-value: 0.02).
The functional knee status of one patient started to decline 13 years after surgery; at the last follow-up (16 years), despite a painless and stable TKA, the patient’s functional score was 0. The etiology of this impressive deterioration, defined as “Post-polio Syndrome”, is not yet completely defined, but it raises a great interest in the scientific community. It is characterized by progressive muscle atrophy with asymmetrical distribution, pain, weakness, and easy fatigue, even in muscle groups not significantly affected by the disease in the acute phase and in the absence of other possible neurological or systemic triggers. The symptomatology is slowly worsening and determines progressive loss of functionality of the limbs up to the impairment of the activities of daily life. The actual cause of post-polio syndrome is not clear, but may be related to the effects of aging on nerve cells already affected by the virus [
14,
22,
23].
Our study has some limitations. The limited cohort makes the statistical analysis less reliable. Furthermore, the statistical analysis did not consider clinical and functional evaluation of a major postoperative complication because of a loss at follow-up. However, TKA in polio patients is a rare surgery, and in the literature there are no studies with more than 17 implants included. To the authors’ knowledge, there are currently no other works with a long-term follow-up on this topic.