Determinants of Temperature Development during Dental Implant Surgery
Abstract
1. Introduction
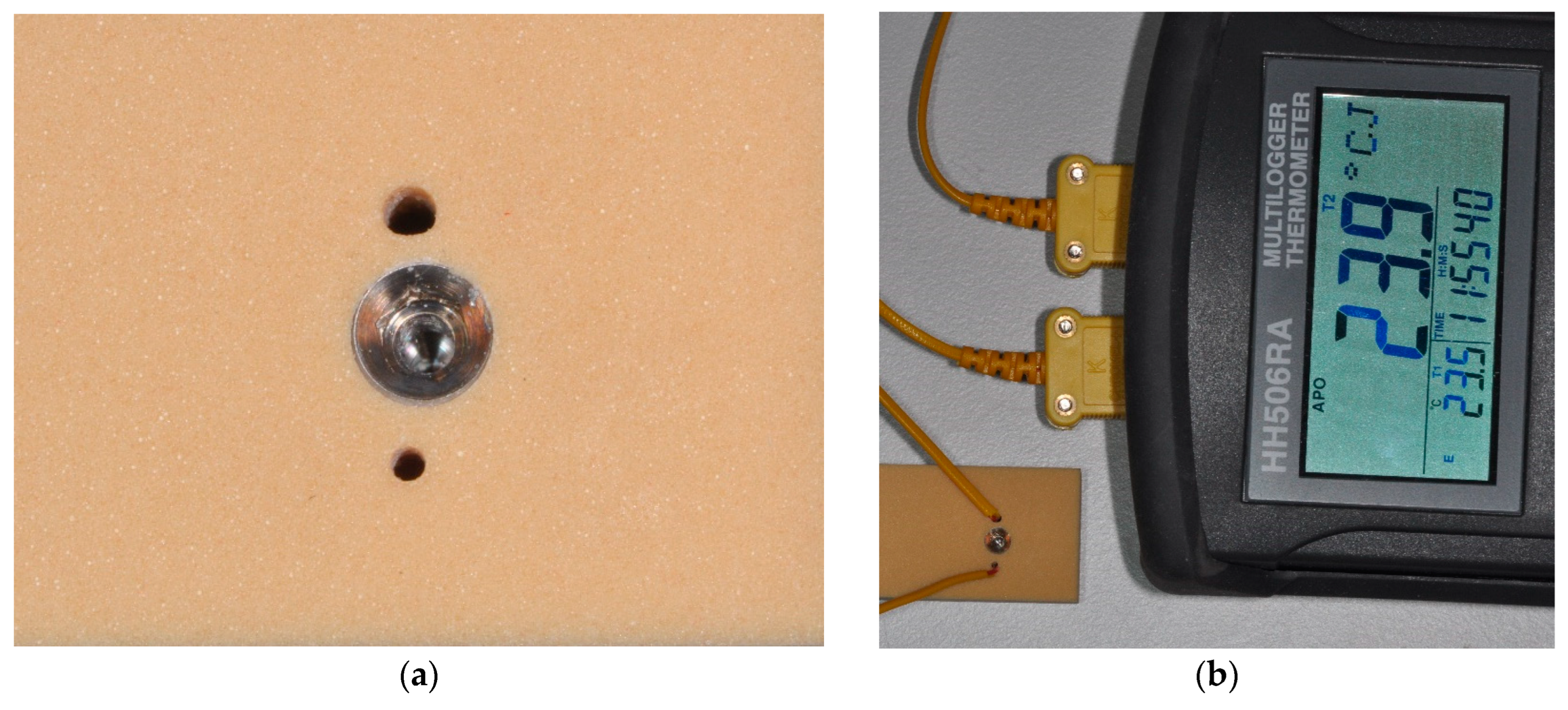
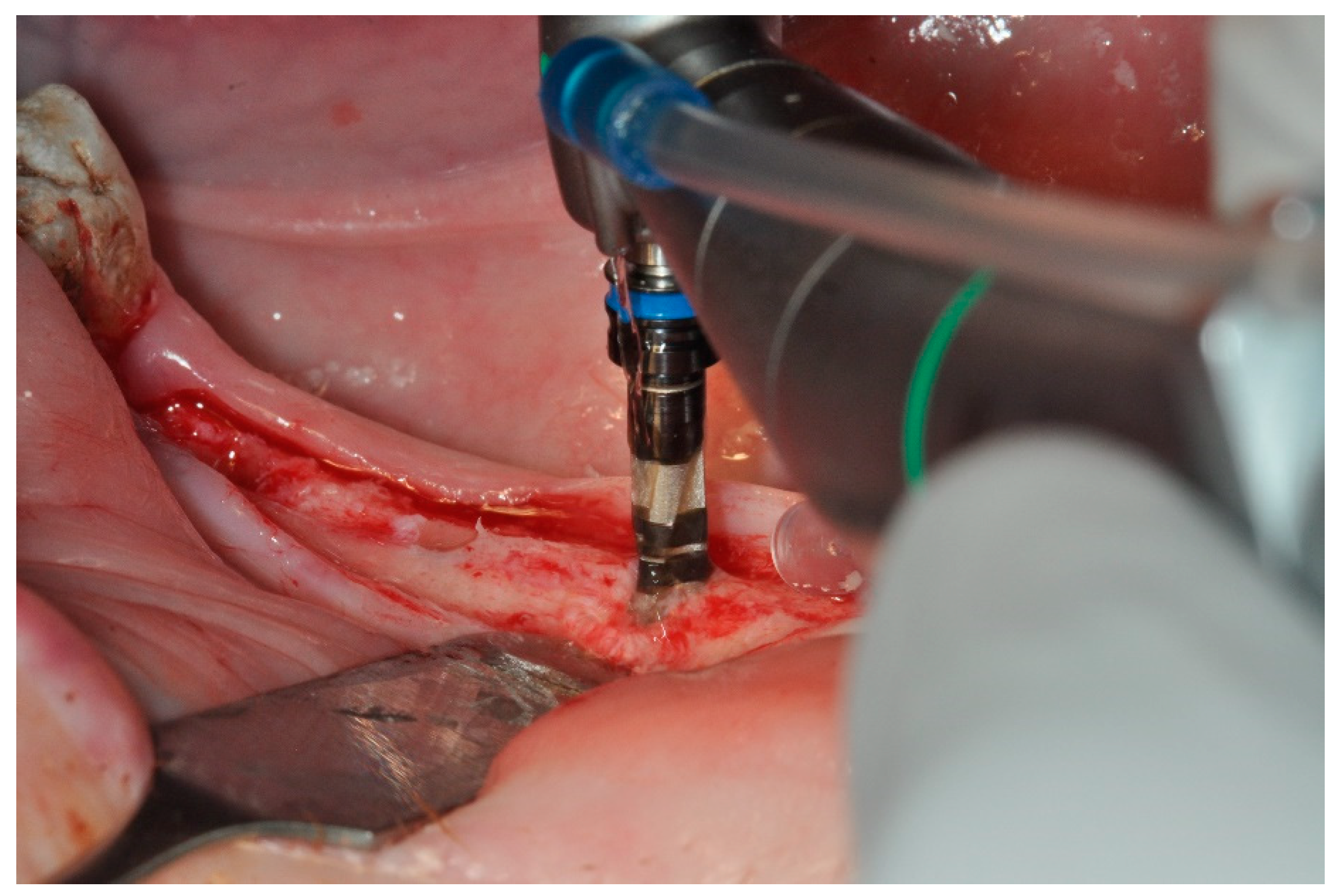
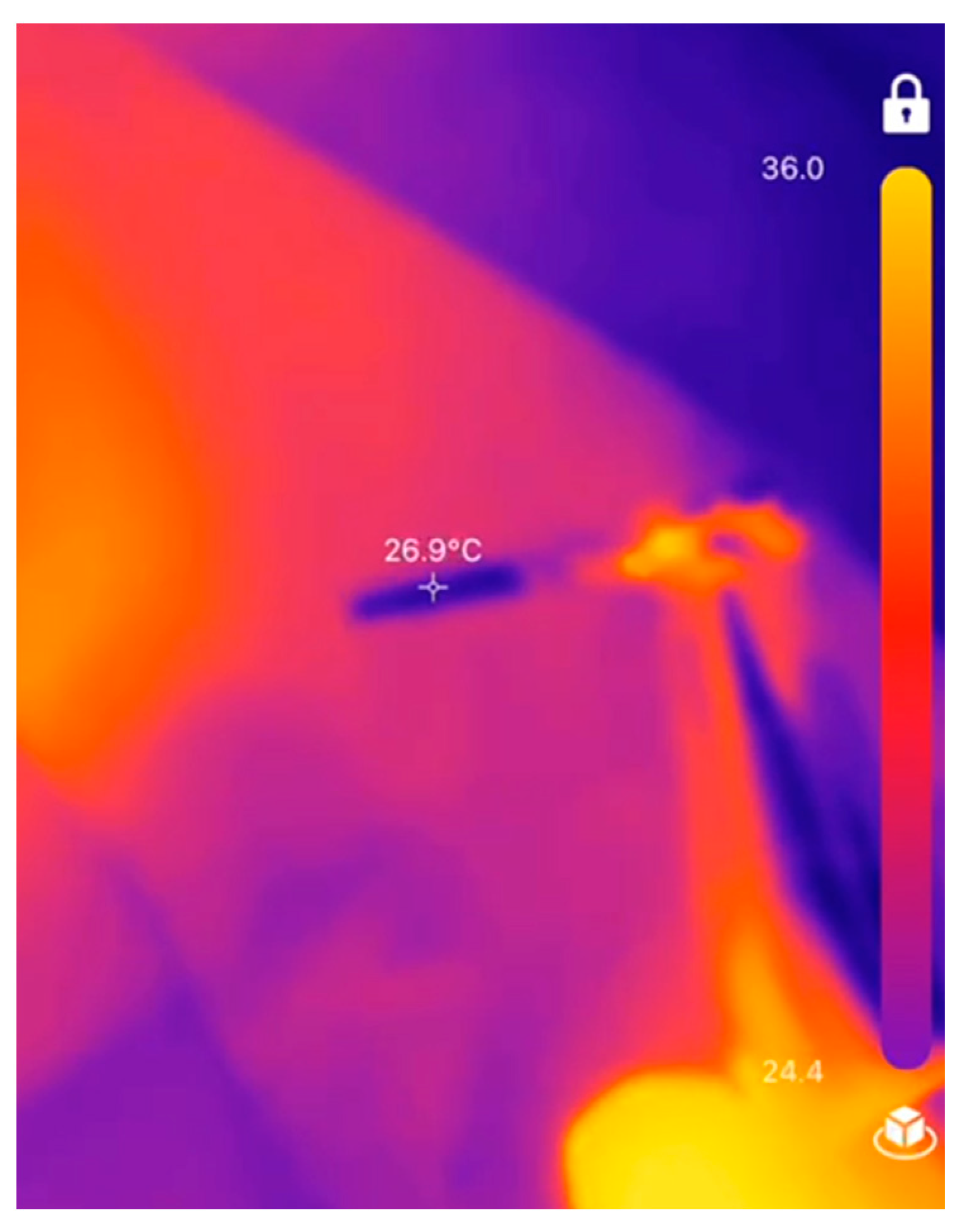
2. Materials and Methods
| DIFF = a + b * IR + res | DIFF: temperature change between start and end of drilling procedure |
| a: Intercept | |
| b: Slope | |
| IR: temperature measured with IR camera | |
| res: regression residuals |
| DIFFminipig = a + b * IRminipig | DIFFminipig: estimated temperature change between start and end of drilling procedure |
| a: Intercept | |
| b: Slope | |
| IRminipig: temperature measured with IR camera |
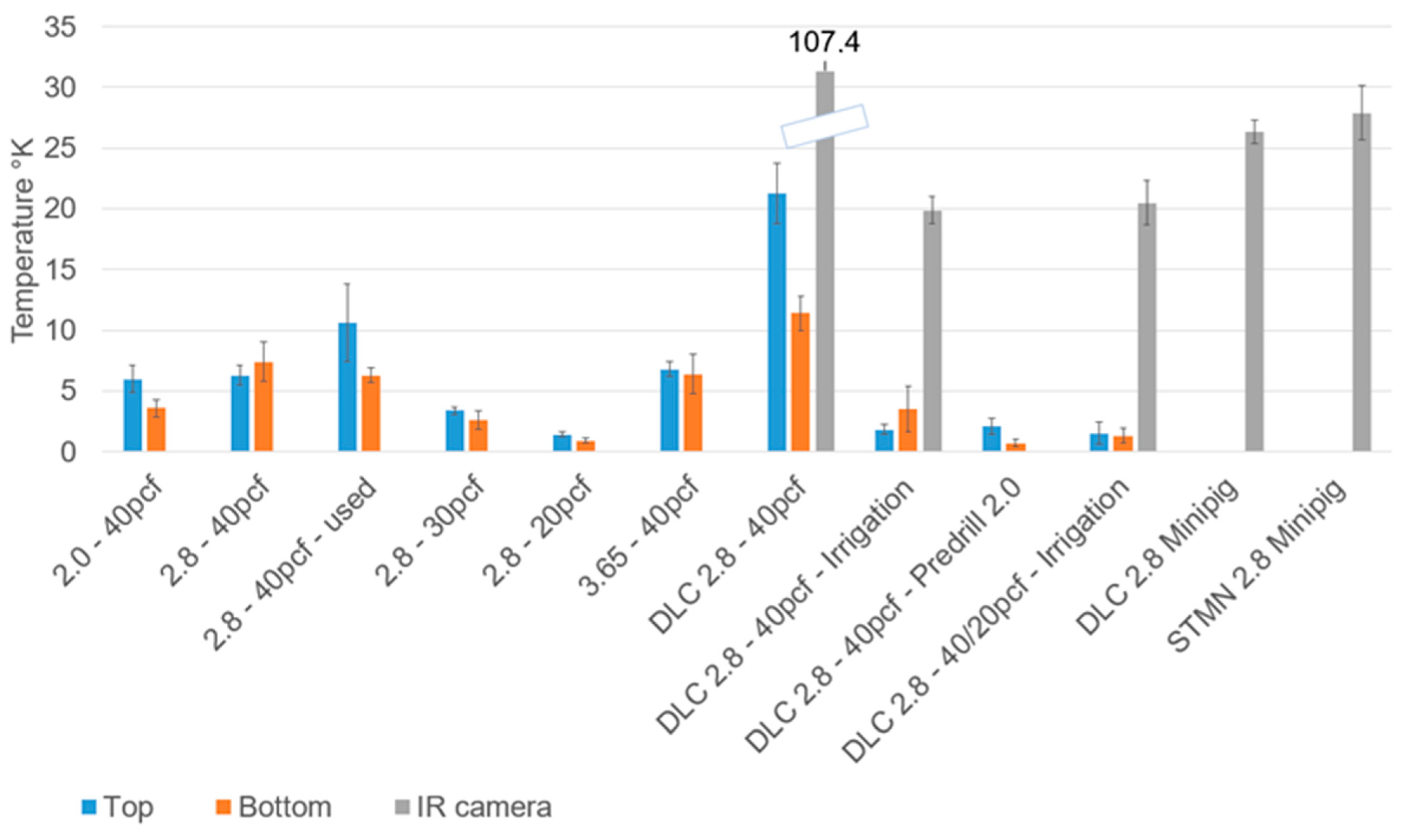
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implants 1986, 1, 11–25. [Google Scholar] [PubMed]
- Buch, R.S.; Weibrich, G.; Wagner, W. Criteria of success in implantology. Mund. Kiefer Gesichtschir. 2003, 7, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Roos, J.; Sennerby, L.; Lekholm, U.; Jemt, T.; Gröndahl, K.; Albrektsson, T. A qualitative and quantitative method for evaluating implant success: A 5-year retrospective analysis of the Brånemark implant. Int. J. Oral Maxillofac. Implants 1997, 12, 504–514. [Google Scholar]
- Albrektsson, T.; Chrcanovic, B.; Östman, P.O.; Sennerby, L. Initial and long-term crestal bone responses to modern dental implants. Periodontology 2017, 73, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Heuzeroth, R.; Pippenger, B.E.; Sandgren, R.; Bellón, B.; Kühl, S. Thermal exposure of implant osteotomies and its impact on osseointegration-A preclinical in vivo study. Clin. Oral Implants Res. 2021, 32, 672–683. [Google Scholar] [CrossRef] [PubMed]
- Stocchero, M.; Jinno, Y.; Toia, M.; Ahmad, M.; Papia, E.; Yamaguchi, S.; Becktor, J.P. Intraosseous Temperature Change during Installation of Dental Implants with Two Different Surfaces and Different Drilling Protocols: An In Vivo Study in Sheep. J. Clin. Med. 2019, 8, 1198. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.K.; Chowdhary, R. Heat generated by dental implant drills during osteotomy-a review: Heat generated by dental implant drills. J. Indian Prosthodont. Soc. 2014, 14, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Aghvami, M.; Brunski, J.B.; Serdar Tulu, U.; Chen, C.H.; Helms, J.A. A Thermal and Biological Analysis of Bone Drilling. J. Biomech. Eng. 2018, 140, 1010101–1010108. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Coyac, B.R.; Arioka, M.; Leahy, B.; Tulu, U.S.; Aghvami, M.; Holst, S.; Hoffmann, W.; Quarry, A.; Bahat, O.; et al. A Novel Osteotomy Preparation Technique to Preserve Implant Site Viability and Enhance Osteogenesis. J. Clin. Med. 2019, 8, 170. [Google Scholar] [CrossRef]
- Ikar, M.; Grobecker-Karl, T.; Karl, M.; Steiner, C. Mechanical stress during implant surgery and its effects on marginal bone: A literature review. Quintessence Int. 2020, 51, 142–150. [Google Scholar]
- Ozcan, M.; Salimov, F.; Temmerman, A.; Turer, O.U.; Alkaya, B.; Haytac, M.C. The Evaluation of Different Osteotomy Drilling Speed Protocols on Cortical Bone Temperature, Implant Stability and Bone Healing: An Experimental Study in an Animal Model. J. Oral Implantol. 2022, 48, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Raj, R.; Manju, V.; Kumar-Gopal, V.; Eswar, M. Analysis of factors determining thermal changes at osteotomy site in dental implant placement—An in-vitro study. J. Clin. Exp. Dent. 2021, 13, e234–e239. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, A.R.; Albrektsson, T.; Albrektsson, B. Heat caused by drilling cortical bone: Temperature measured in vivo in patients and animals. Acta Orthop. Scand. 1984, 55, 629–631. [Google Scholar] [CrossRef] [PubMed]
- Yamaba, T.; Suganami, T.; Ikebe, K.; Sogo, M.; Maeda, Y.; Wada, M. The Evaluation of the Heat Generated by the Implant Osteotomy Preparation Using a Modified Method of the Measuring Temperature. Int. J. Oral Maxillofac. Implants 2015, 30, 820–826. [Google Scholar] [CrossRef] [PubMed]
- Katic, Z.; Jukic, T.; Stubljar, D. Effects of Osteotomy Lengths on the Temperature Rise of the Crestal Bone During Implant Site Preparation. Implant. Dent. 2018, 27, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Bettach, R.; Cayron, B.; Boukhris, G.; Dedavid, B.A.; Frutos, J.C.P. Development of a New Drill Design to Improve the Temperature Control during the Osteotomy for Dental Implants: A Comparative In Vitro Analysis. Biology 2020, 9, 208. [Google Scholar] [CrossRef] [PubMed]
- Orgev, A.; Gonzaga, L.; Martin, W.; Morton, D.; Lin, W.S. Addition of an irrigation channel to a surgical template to facilitate cooling during implant osteotomy. J. Prosthet. Dent. 2021, 126, 164–166. [Google Scholar] [CrossRef] [PubMed]
- Soldatos, N.; Nelson-Rabe, L.; Palanker, N.; Angelov, N.; Romanos, G.; Weltman, R. Temperature Changes during Implant Osteotomy Preparations in Fresh Human Cadaver Tibiae, Comparing Straight with Tapered Drills. Materials 2022, 15, 2369. [Google Scholar] [CrossRef] [PubMed]
- Karaca, F.; Aksakal, B.; Kom, M. Influence of orthopaedic drilling parameters on temperature and histopathology of bovine tibia: An in vitro study. Med. Eng. Phys. 2011, 33, 1221–1227. [Google Scholar] [CrossRef]
- Tur, D.; Giannis, K.; Unger, E.; Mittlböck, M.; Rausch-Fan, X.; Strbac, G.D. Thermal effects of various drill materials during implant site preparation-Ceramic vs. stainless steel drills: A comparative in vitro study in a standardised bovine bone model. Clin. Oral Implants Res. 2021, 32, 154–166. [Google Scholar] [CrossRef]
- Strbac, G.D.; Giannis, K.; Unger, E.; Mittlböck, M.; Vasak, C.; Watzek, G.; Zechner, W. Drilling- and withdrawing-related thermal changes during implant site osteotomies. Clin. Implant. Dent. Relat. Res. 2015, 17, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Abboud, M.; Rugova, S.; Orentlicher, G. Immediate Loading: Are Implant. Surface and Thread Design More Important Than Osteotomy Preparation? Compend. Contin. Educ. Dent. 2020, 41, 384–386. [Google Scholar] [PubMed]
- Bernabeu-Mira, J.C.; Soto-Peñaloza, D.; Peñarrocha-Diago, M.; Camacho-Alonso, F.; Rivas-Ballester, R.; Peñarrocha-Oltra, D. Low-speed drilling without irrigation versus conventional drilling for dental implant osteotomy preparation: A systematic review. Clin. Oral Investig. 2021, 25, 4251–4267. [Google Scholar] [CrossRef] [PubMed]
- Roy, R.K.; Lee, K.R. Biomedical applications of diamond-like carbon coatings: A review. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 83, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Batista Mendes, G.C.; Padovan, L.E.; Ribeiro-Júnior, P.D.; Sartori, E.M.; Valgas, L.; Claudino, M. Influence of implant drill materials on wear, deformation, and roughness after repeated drilling and sterilization. Implant. Dent. 2014, 23, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Akaike, S.; Hayakawa, T.; Kobayashi, D.; Aono, Y.; Hirata, A.; Hiratsuka, M.; Nakamura, Y. Reduction in static friction by deposition of a homogeneous diamond-like carbon (DLC) coating on orthodontic brackets. Dent. Mater. J. 2015, 34, 888–895. [Google Scholar] [CrossRef]
- Raghavendra, S.; Wood, M.C.; Taylor, T.D. Early wound healing around endosseous implants: A review of the literature. Int. J. Oral Maxillofac. Implants 2005, 20, 425–431. [Google Scholar] [PubMed]
- Khayat, P.G.; Arnal, H.M.; Tourbah, B.I.; Sennerby, L. Clinical outcome of dental implants placed with high insertion torques (up to 176 Ncm). Clin. Implant. Dent. Relat. Res. 2013, 15, 227–233. [Google Scholar] [CrossRef]
- Frisardi, G.; Barone, S.; Razionale, A.V.; Paoli, A.; Frisardi, F.; Tullio, A.; Lumbau, A.; Chessa, G. Biomechanics of the press-fit phenomenon in dental implantology: An image-based finite element analysis. Head. Face Med. 2012, 8, 18. [Google Scholar] [CrossRef]
- Guan, H.; van Staden, R.C.; Johnson, N.W.; Loo, Y.C. Dynamic modelling and simulation of dental implant insertion process—A finite element study. Finite Elem. Anal. Des. 2011, 47, 886–897. [Google Scholar] [CrossRef]
- Flanagan, D. Heat generated during seating of dental implant fixtures. J. Oral Implantol. 2014, 40, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Bartold, P.M.; Kuliwaba, J.S.; Lee, V.; Shah, S.; Marino, V.; Fazzalari, N.L. Influence of surface roughness and shape on microdamage of the osseous surface adjacent to titanium dental implants. Clin. Oral Implants Res. 2011, 22, 613–618. [Google Scholar] [CrossRef]
- Tabassum, A.; Meijer, G.J.; Walboomers, X.F.; Jansen, J.A. Biological limits of the undersized surgical technique: A study in goats. Clin. Oral Implants Res. 2011, 22, 129–134. [Google Scholar] [CrossRef]
- Coelho, P.G.; Marin, C.; Teixeira, H.S.; Campos, F.E.; Gomes, J.B.; Guastaldi, F.; Anchieta, R.B.; Silveira, L.; Bonfante, E.A. Biomechanical evaluation of undersized drilling on implant biomechanical stability at early implantation times. J. Oral Maxillofac. Surg. 2013, 71, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Abrahamsson, I.; Lang, N.P.; Lindhe, J. De novo alveolar bone formation adjacent to endosseous implants. Clin. Oral Implants Res. 2003, 14, 251–262. [Google Scholar] [CrossRef]
- Parvini, P.; Trimpou, G.; Begic, A.; Cafferata, E.A.; Petsos, H.; Müller, K.M.; Schwarz, F.; Eickholz, P.; Obreja, K. Esthetic and clinical outcomes after immediate placement and restoration: Comparison of two implant systems in the anterior maxilla-A cross-sectional study. Clin. Implant. Dent. Relat. Res. 2023, 25, 252–260. [Google Scholar] [CrossRef]
- Fabbri, G.; Staas, T.; Urban, I. A Retrospective Observational Study Assessing the Clinical Outcomes of a Novel Implant System with Low-Speed Site Preparation Protocol and Tri-Oval Implant Geometry. J. Clin. Med. 2022, 11, 4859. [Google Scholar] [CrossRef]
- Hurtgen, A.; Seidel, L.; Manni, L.L.; Liegeois, L.; Lecloux, G.; Lambert, F. Clinical and radiographic assessment of circular versus triangular cross-section neck implants in the posterior maxilla: Five-year follow-up of a randomized controlled trial. Clin. Oral Implants Res. 2023, 34, 698–706. [Google Scholar] [CrossRef] [PubMed]
- Schulz, A.; Klär, V.; Grobecker-Karl, T.; Karl, M. Biomechanical rationale for a novel implant design reducing stress on buccal bone. Appl. Sci. 2023, 13, 666. [Google Scholar] [CrossRef]
- Klär, V.; Zimmerer, R.; Schulz, A.; Lethaus, B. Biomechanical performance of a novel implant design in simulated extraction sites and sinuslift procedures. Appl. Sci. 2023, 13, 7541. [Google Scholar] [CrossRef]
- Parvizi, S.; Cameron, A.; Tadakamadla, S.; Figueredo, C.M.S.; Reher, P. A Novel Irrigation System to Reduce Heat Generation during Guided Implantology: An In Vitro Study. J. Clin. Med. 2023, 12, 3944. [Google Scholar] [CrossRef]
- Kuster, M.; Mukaddam, K.; Zitzmann, N.U.; Filippi, A.; Kühl, S. Influence of a Novel Drill Design on Heat Generation During Conventional and Guided Implant Osteotomy. Int. J. Oral Maxillofac. Implants 2021, 36, e31–e41. [Google Scholar] [CrossRef]
- Strbac, G.D.; Unger, E.; Donner, R.; Bijak, M.; Watzek, G.; Zechner, W. Thermal effects of a combined irrigation method during implant site drilling: A standardized in vitro study using a bovine rib model. Clin. Oral Implants Res. 2014, 25, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, R.A.; Albrektsson, T. The effect of heat on bone regeneration: An experimental study in the rabbit using the bone growth chamber. J. Oral Maxillofac. Surg. 1984, 42, 705–711. [Google Scholar] [CrossRef]
- Pérez-Pevida, E.; Brizuela-Velasco, A.; Chávarri-Prado, D.; Diéguez-Pereira, M.; Jiménez-Garrudo, A.; Montalbán-Vadillo, O.; Viteri-Agustín, I.; Estrada-Martínez, A.; Santamaría-Arrieta, G. Influence of time on primary stability of dental implants placed with osteotomes due to the elastic properties of peri-implant bone. J. Dent. Sci. 2019, 14, 358–364. [Google Scholar] [CrossRef]
- Wang, R.; Eppell, S.J.; Nguyen, C.; Morris, N. Relative Contribution of Trabecular and Cortical Bone to Primary Implant Stability: An In Vitro Model Study. J. Oral Implantol. 2016, 42, 145–152. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Arosio, P.; Gastaldi, G.; Gherlone, E. The insertion torque-depth curve integral as a measure of implant primary stability: An in vitro study on polyurethane foam blocks. J. Prosthet. Dent. 2018, 120, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Sierra-Rebolledo, A.; Allais-Leon, M.; Maurette-O’Brien, P.; Gay-Escoda, C. Primary Apical Stability of Tapered Implants Through Reduction of Final Drilling Dimensions in Different Bone Density Models: A Biomechanical Study. Implant. Dent. 2016, 25, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Elias, C.N.; Rocha, F.A.; Nascimento, A.L.; Coelho, P.G. Influence of implant shape, surface morphology, surgical technique and bone quality on the primary stability of dental implants. J. Mech. Behav. Biomed. Mater. 2012, 16, 169–180. [Google Scholar] [CrossRef]
- Ueno, D.; Nakamura, K.; Kojima, K.; Toyoshima, T.; Tanaka, H.; Ueda, K.; Koyano, K.; Kodama, T. A stepwise under-prepared osteotomy technique improves primary stability in shallow-placed implants: A preliminary study for simultaneous vertical ridge augmentation. Odontology 2018, 106, 187–193. [Google Scholar] [CrossRef]
- Lamazza, L.; Lollobrigida, M.; Vozza, I.; Palmieri, L.; Stacchi, C.; Lombardi, T.; De Biase, A. Piezoelectric Implant Site Preparation: Influence of Handpiece Movements on Temperature Elevation. Materials 2020, 13, 4072. [Google Scholar] [CrossRef] [PubMed]
| Drill | Bone | Irrigation | IR Camera |
|---|---|---|---|
| 2.0 | 40 | - | - |
| 2.8 | 40 | - | - |
| 3.65 | 40 | - | - |
| 2.8–25 times used | 40 | - | - |
| 2.8 | 30 | - | - |
| 2.8 | 20 | - | - |
| DLC 2.8 | 40 | - | yes |
| DLC 2.8 | 40 | yes | yes |
| DLC 2.8—Predrill DLC 2.0 | 40 | - | - |
| DLC 2.8 | 20 and 40 (3 mm) | yes | yes |
| DLC 2.8 | Minipig | yes | yes |
| STMN 2.8 | Minipig | yes | yes |
| 2.8–40 pcf | 2.8–40 pcf–Used | 2.8–30 pcf | 2.8–20 pcf | 3.65–40 pcf | DLC 2.8–40 pcf | DLC 2.8–40 pcf–Irrigation | DLC 2.8–40 pcf–Predrill 2.0 | DLC 2.8–40/20 pcf–Irrigation | |
|---|---|---|---|---|---|---|---|---|---|
| (a) | |||||||||
| 2.0–40 pcf | 0.076 | 0.007 * | 0.652 | 0.018 * | 0.213 | 0.000 * | 1.000 | 0.007 * | 0.013 * |
| 2.8–40 pcf | 1.000 | 0.029 * | 0.022 * | 1.000 | 0.066 | 0.135 | 0.018 * | 0.016 * | |
| 2.8–40 pcf–Used | 0.004 * | 0.000 * | 1.000 | 0.013 * | 0.357 | 0.000 * | 0.000 * | ||
| 2.8–30 pcf | 0.135 | 0.071 | 0.000 * | 1.000 | 0.071 | 0.267 | |||
| 2.8–20 pcf | 0.035 * | 0.004 * | 0.429 | 0.652 | 1.000 | ||||
| 3.65–40 pcf | 0.024 * | 0.359 | 0.029 * | 0.029 * | |||||
| DLC 2.8–40 pcf | 0.004* | 0.000 * | 0.000 * | ||||||
| DLC 2.8–40 pcf–Irrigation | 0.359 | 0.591 | |||||||
| DLC 2.8–40 pcf–Predrill 2.0 | 0.652 | ||||||||
| (b) | |||||||||
| 2.0–40 pcf | 1.000 | 1.000 | 0.016 * | 0.011 * | 1.000 | 0.006 * | 0.451 | 0.006 * | 0.004 * |
| 2.8–40 pcf | 1.000 | 0.004 * | 0.004 * | 1.000 | 0.009 * | 0.321 | 0.000 * | 0.000 * | |
| 2.8–40 pcf–Used | 0.068 | 0.046 * | 0.472 | 1.000 | 0.068 | 0.044 * | 0.046 * | ||
| 2.8–30 pcf | 0.000 * | 0.198 | 0.004 * | 1.000 | 0.000 * | 0.011 * | |||
| 2.8–20 pcf | 0.044 * | 0.004 * | 0.759 | 0.029 * | 1.000 | ||||
| 3.65–40 pcf | 0.018 * | 0.198 | 0.000 * | 0.000 * | |||||
| DLC 2.8–40 pcf | 0.000 * | 0.000 * | 0.000 * | ||||||
| DLC 2.8–40 pcf–Irrigation | 0.032 * | 1.000 | |||||||
| DLC 2.8–40 pcf–Predrill 2.0 | 0.808 | ||||||||
| Straumann | DLC | |||
|---|---|---|---|---|
| MEAN | SD | MEAN | SD | |
| Top | 3.418 | 0.5061 | 3.071 | 0.2161 |
| Bottom | 3.202 | 0.2302 | 3.045 | 0.0983 |
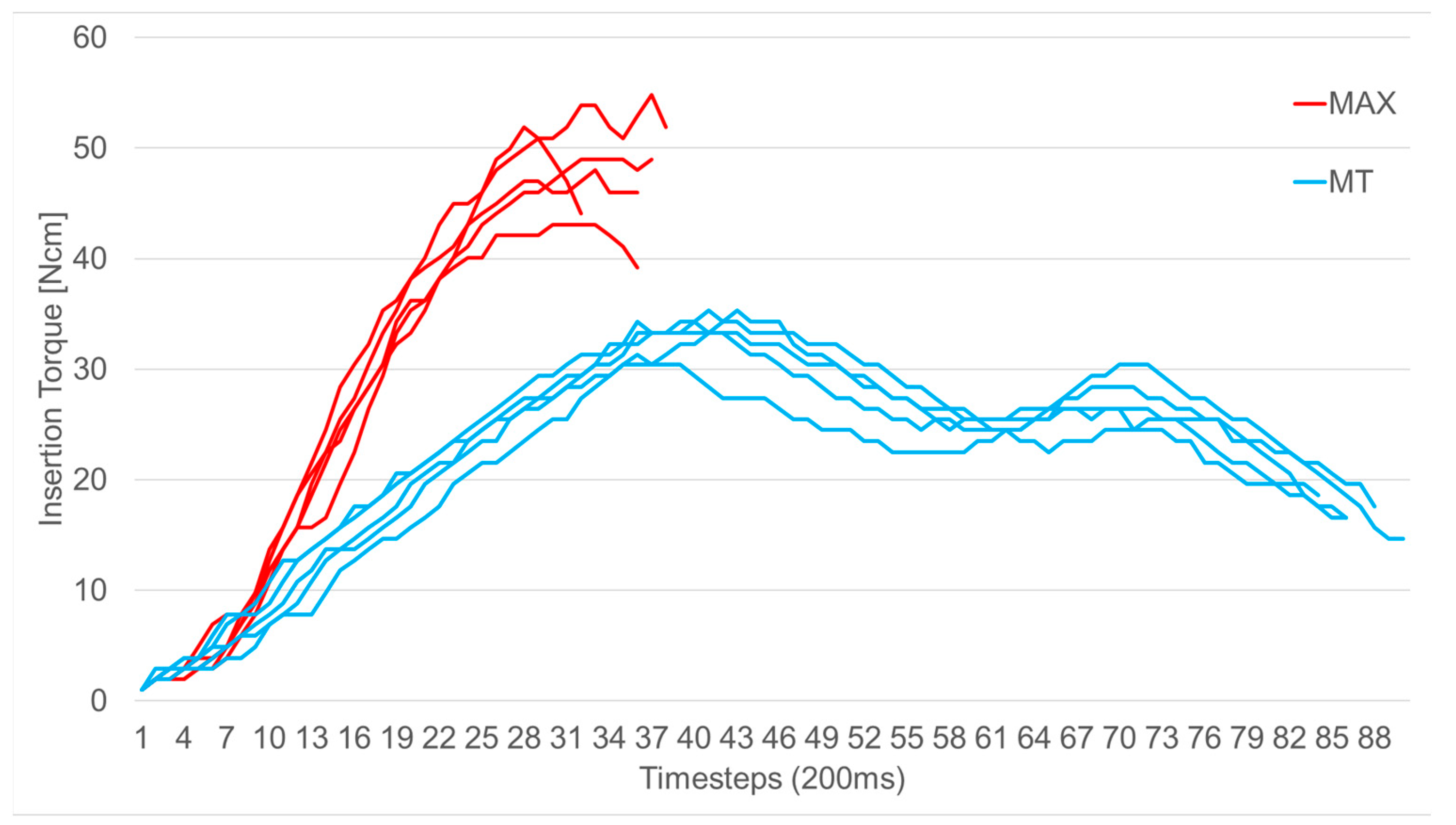
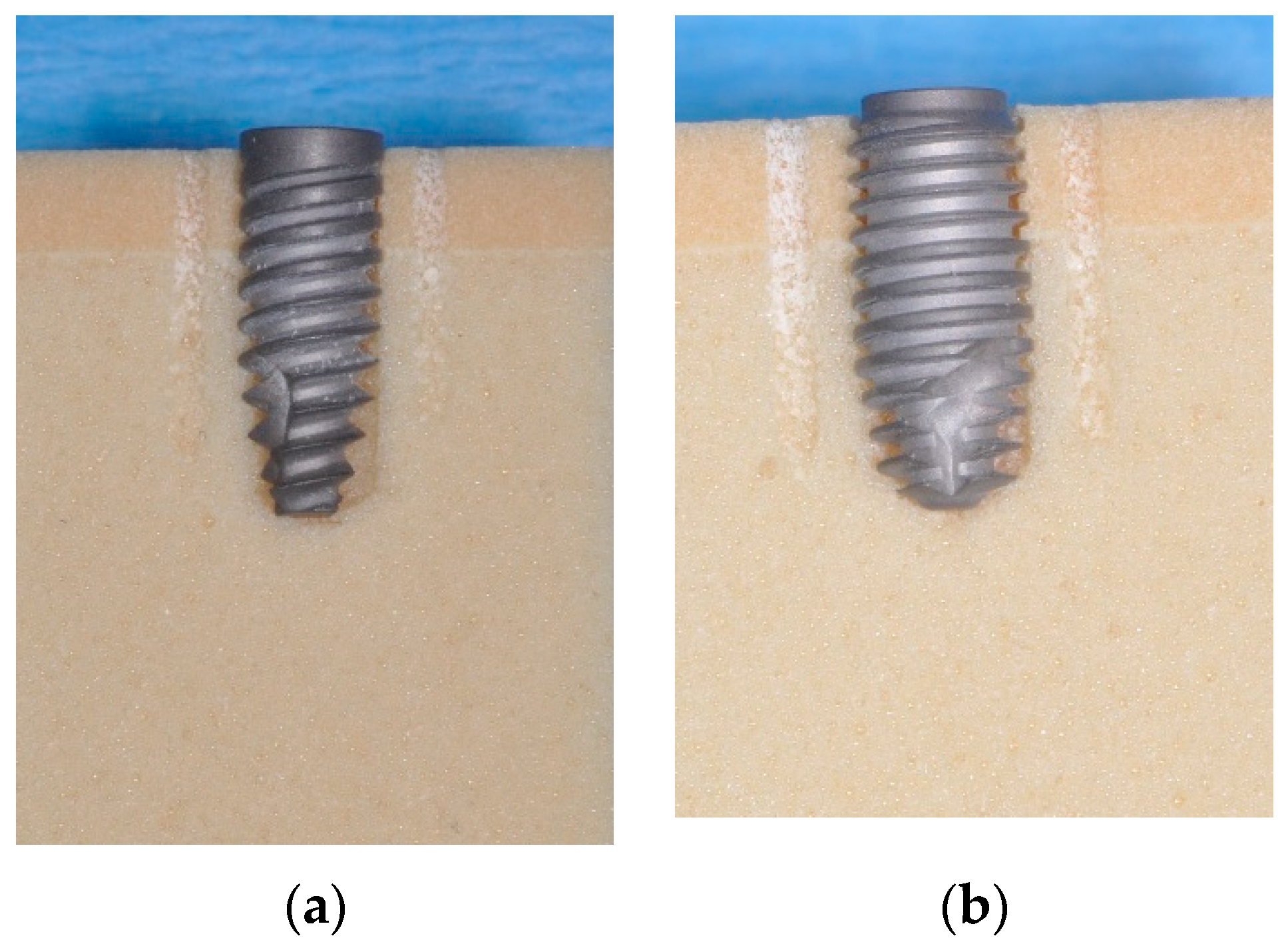
| MAX Implant | MT Implant | Comparison MAX vs. MT | |||
|---|---|---|---|---|---|
| MEAN | SD | MEAN | SD | p-Value | |
| Temperature top | 3.80 | 0.65 | 7.58 | 0.64 | <0.01 * |
| Temperature bottom | 4.48 | 1.92 | 7.50 | 0.16 | 0.02 * |
| Torque | 49.36 | 4.39 | 33.90 | 1.52 | <0.01 * |
| Osstell | 71.50 | 7.57 | 68.40 | 2.75 | 0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sekura, K.; Erbel, C.; Karl, M.; Grobecker-Karl, T. Determinants of Temperature Development during Dental Implant Surgery. Prosthesis 2024, 6, 657-669. https://doi.org/10.3390/prosthesis6030046
Sekura K, Erbel C, Karl M, Grobecker-Karl T. Determinants of Temperature Development during Dental Implant Surgery. Prosthesis. 2024; 6(3):657-669. https://doi.org/10.3390/prosthesis6030046
Chicago/Turabian StyleSekura, Kirsten, Carolin Erbel, Matthias Karl, and Tanja Grobecker-Karl. 2024. "Determinants of Temperature Development during Dental Implant Surgery" Prosthesis 6, no. 3: 657-669. https://doi.org/10.3390/prosthesis6030046
APA StyleSekura, K., Erbel, C., Karl, M., & Grobecker-Karl, T. (2024). Determinants of Temperature Development during Dental Implant Surgery. Prosthesis, 6(3), 657-669. https://doi.org/10.3390/prosthesis6030046







