Marginal Bone Loss and Treatment Complications with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants—A Randomized Clinical Trial
Abstract
1. Introduction
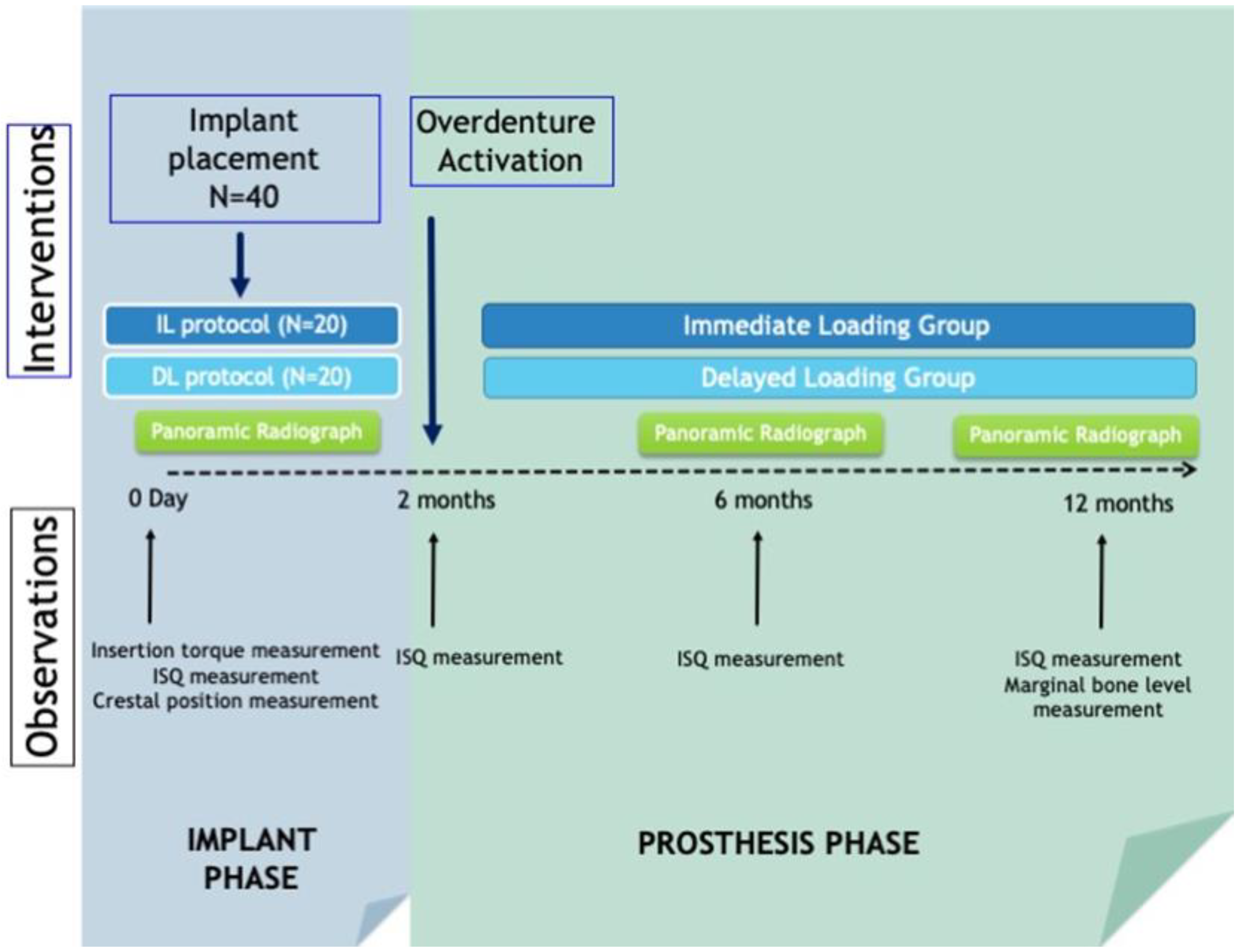
2. Materials and Methods
2.1. Surgical Protocol
2.2. Evaluation of Complications
2.3. Data Analysis
3. Results
3.1. Sample Description
3.2. Distribution and Characteristics of the Placed Implants
4. Discussion
4.1. Bone Loss Assessment
4.2. Implant Stability
4.3. Implant Failure
4.4. Complications
4.5. Limitations and Continuity
5. Conclusions
- There were no differences in marginal bone loss observed at one year in immediately loaded (0.40 ± 0.39 mm) versus conventionally loaded (0.44 ± 0.36 mm) implants placed for the retention of mandibular overdentures.
- There were no differences in primary and secondary stability of immediately loaded versus conventional implants; however, in the conventional loading group, stability increased significantly between the time of implant placement at both 6 and 12 months post-placement.
- The main predictive factor for implant failure as well as marginal bone loss is bone quality (β = 13.61; 95% CI: 1.3–25.8).
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schimmel, M.; Srinivasan, M.; Herrmann, F.; Müller, F. Loading Protocols for Implant-Supported Overdentures in the Edentulous Jaw: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2014, 29, 271–286. [Google Scholar] [CrossRef] [PubMed]
- Brånemark, P.I.; Hansson, B.O.; Adell, R.; Breine, U.; Lindström, J.; Hallén, O.; Ohman, A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand. J. Plast. Reconstr. Surg. Suppl. 1977, 16, 1–132. [Google Scholar]
- Feine, J.S.; Carlsson, G.E.; Awad, M.A.; Chehade, A.; Duncan, W.J.; Gizani, S.; Head, T.; Heydecke, G.; Lund, J.P.; MacEntee, M.; et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Gerodontology 2002, 19, 601–602. [Google Scholar]
- Thomason, J.M.; Feine, J.; Exley, C.; Moynihan, P.; Müller, F.; Naert, I.; Ellis, J.; Barclay, C.; Butterworth, C.; Scott, B.; et al. Mandibular two implant-supported overdentures as the first choice standard of care for edentulous patients—the York Consensus Statement. Br. Dent. J. 2009, 207, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Montero, J.; Dib, A.; Guadilla, Y.; Flores, J.; Pardal-Peláez, B. Functional and patient-centered treatment outcomes with man- dibular overdentures retained by two immediate or conven- tionally loaded implants. A randomized clinical trial. J. Clin. Med. 2021, 10, 3477. [Google Scholar] [CrossRef]
- Su, M.; Shi, B.; Zhu, Y.; Guo, Y.; Zhang, Y.; Xia, H.; Zhao, L. Comparison of implant success rates with different loading protocols: A meta-analysis. Int. J. Oral Maxillofac. Implant. 2014, 29, 344–352. [Google Scholar] [CrossRef]
- Adell, R.; Eriksson, B.; Lekholm, U.; Brånemark, P.I.; Jemt, T. Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int. J. Oral Maxillofac. Implant. 1990, 5, 347–359. [Google Scholar]
- Papaspyridakos, P.; Chen, C.-J.; Chuang, S.-K.; Weber, H.-P. Implant Loading Protocols for Edentulous Patients with Fixed Pros-theses: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2014, 29, 256–270. [Google Scholar] [CrossRef]
- Borges, T.D.F.; Mendes, A. Mandibular Overdentures with Immediate Loading: Satisfaction and Quality of Life. Int. J. Prosthodont. 2011, 24, 534–539. [Google Scholar]
- Weber, H.-P.; Morton, D.; Gallucci, G.O.; Roccuzzo, M.; Cordaro, L.; Grutter, L. Consensus statements and recommended clinical procedures regarding loading protocols. Int. J. Oral Maxillofac. Implant. 2009, 24, 180–183. [Google Scholar]
- Lekholm, U.; Zarb, G.A. Patient selection and preparation. In Tissue Integrated Prostheses: Osseointegration in Clinical Dentistry; Quintessence Publishing: Chicago, IL, USA, 1985; pp. 199–210. [Google Scholar]
- Jokstad, A.; Alkumru, H. Immediate function on the day of surgery compared with a delayed implant loading process in the mandible: A randomized clinical trial over 5 years. Clin. Oral Implant. Res. 2013, 25, 1325–1335. [Google Scholar] [CrossRef]
- Schincaglia, G.P.; Rubin, S.; Thacker, S.; Dhingra, A.; Trombelli, L.; Ioannidou, E. Marginal Bone Response Around Immediate- and Delayed-Loading Implants Supporting a Locator-Retained Mandibular Overdenture: A Randomized Controlled Study. Int. J. Oral Maxillofac. Implant. 2016, 31, 448–458. [Google Scholar] [CrossRef]
- Alfadda, S.A. A Randomized Controlled Clinical Trial of Edentulous Patients Treated with Immediately Loaded Implant-Supported Mandibular Fixed Prostheses. Clin. Implant. Dent. Relat. Res. 2013, 16, 806–816. [Google Scholar] [CrossRef]
- Romeo, E.; Chiapasco, M.; Lazza, A.; Casentini, P.; Ghisolfi, M.; Iorio, M.; Vogel, G. Implant-retained mandibular overdentures with ITI implants: A comparison of 2-year results between delayed and immediate loading. Clin. Oral Implant. Res. 2002, 13, 495–501. [Google Scholar] [CrossRef]
- Chiapasco, M.; Abati, S.; Romeo, E.; Vogel, G. Implant-retained mandibular overdentures with Brånemark System MKII implants: A prospective comparative study between delayed and immediate loading. Int. J. Oral Maxillofac. Implant. 2001, 16, 537–546. [Google Scholar]
- Schuster, A.J.; Marcello-Machado, R.M.; Bielemann, A.M.; da Rosa Possebon, A.P.; Chagas Júnior, O.L.; Faot, F. Immediate vs conventional loading of Facility-Equator system in mandibular overdenture wearers: 1-year RCT with clinical, biological, and functional evaluation. Clin. Implant. Dent. Relat. Res. 2020, 22, 270–280. [Google Scholar] [CrossRef]
- Elsyad, M.A.; Al-Mahdy, Y.F.; Fouad, M.M. Marginal bone loss adjacent to conventional and immediate loaded two implants supporting a ball-retained mandibular overdenture: A 3-year randomized clinical trial. Clin. Oral Implant. Res. 2011, 23, 496–503. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chen, C.J.; Singh, M.; Weber, H.P.; Gallucci, G.O. Success criteria in implant dentistry: A systematic review. J. Dent. Res. 2012, 91, 242–248. [Google Scholar] [CrossRef]
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implants 1986, 1, 11–25. [Google Scholar]
- Gallucci, G.O.; Doughtie, C.B.; Hwang, J.W.; Fiorellini, J.P.; Weber, H.-P. Five-year results of fixed implant-supported rehabilitations with distal cantilevers for the edentulous mandible. Clin. Oral Implant. Res. 2009, 20, 601–607. [Google Scholar] [CrossRef]
- Elsyad, M.A.; Elsaih, E.A.; Khairallah, A.S. Marginal bone resorption around immediate and delayed loaded implants supporting a locator-retained mandibular overdenture. A 1-year randomised controlled trial. J. Oral Rehabil. 2014, 41, 608–618. [Google Scholar] [CrossRef] [PubMed]
- Pardal-Peláez, B.; Flores-Fraile, J.; Pardal-Refoyo, J.L.; Montero, J. Implant loss and crestal bone loss in immediate versus delayed load in edentulous mandibles: A systematic review and meta-analysis. J. Prosthet. Dent. 2020, 125, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I.; Tumer, C. Early versus late loading of unsplinted TiUnite surface implants supporting mandibular overdentures: A 2-year report from a prospective study. J. Oral Rehabil. 2007, 34, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Cannizzaro, G.; Felice, P.; Soardi, E.; Ferri, V.; Leone, M.; Lazzarini, M.; Audino, S.; Esposito, M. Immediate loading of 2(all-on-2) versus 4 (all-on-4) implants placed with a flapless technique supporting mandibular cross-arch fixed prostheses: 1-year results from a pilot ran-domised controlled trial. Eur. J. Oral Implantol. 2013, 6, 121–131. [Google Scholar] [PubMed]
- Alfadda, S.A.; Chvartszaid, D.; Tulbah, H.I.; Finer, Y. Immediate versus conventional loading of mandibular implant-supported fixed prostheses in edentulous patients: 10-year report of a randomised controlled trial. Int. J. Oral Implantol. 2019, 12, 431–446. [Google Scholar]
- Mundt, T.; Passia, N.; Att, W.; Heydecke, G.; Freitag-Wolf, S.; Luthardt, R.G.; Kappel, S.; Konstantinidis, I.K.; Stiesch, M.; Wolfart, S.; et al. Pain and discomfort following immediate and delayed loading by overdentures in the single mandibular implant study (SMIS). Clin. Oral Investig. 2016, 21, 635–642. [Google Scholar] [CrossRef]
- García-Moreno, S.; González-Serrano, J.; López-Pintor, R.; Pardal-Peláez, B.; Hernández, G.; Martínez-González, J. Implant stability using piezoelectric bone surgery compared with conventional drilling: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2018, 47, 1453–1464. [Google Scholar] [CrossRef]
- La Escala ISQ-Osstell—Implant Stability. Available online: https://www.osstell.com/es/clinical-guidelines/the-isq-scale/ (accessed on 7 January 2023).
- Acham, S.; Rugani, P.; Truschnegg, A.; Wildburger, A.; Wegscheider, W.A.; Jakse, N. Immediate loading of four interforaminal im-plants supporting a locator-retained mandibular overdenture in the elderly. Results of a 3-year randomized, controlled, pro-spective clinical study. Clin. Implant. Dent. Relat. Res. 2017, 19, 895–900. [Google Scholar] [CrossRef]
- Medizintechnik Gulden. Periotest, el Instrumento de Medición Dental para la Implantología y la Odontología más Exigentes. Available online: http://www.med-gulden.com/downloads/03_spain/01_Informaci%F3ndeproducto/Proceso_de_producci%F3n.pdf (accessed on 7 January 2023).
- Kern, M.; Att, W.; Fritzer, E.; Kappel, S.; Luthardt, R.; Mundt, T.; Reissmann, D.; Rädel, M.; Stiesch, M.; Wolfart, S.; et al. Survival and Complications of Single Dental Implants in the Edentulous Mandible Following Immediate or Delayed Loading: A Randomized Controlled Clinical Trial. J. Dent. Res. 2017, 97, 163–170. [Google Scholar] [CrossRef]
- Atieh, M.A.; Baqain, Z.H.; Tawse-Smith, A.; Ma, S.; Almoselli, M.; Lin, L.; Alsabeeha, N.H.M. The influence of insertion torque values on the failure and complication rates of dental implants: A systematic review and meta-analysis. Clin. Implant. Dent. Relat. Res. 2021, 23, 341–360. [Google Scholar] [CrossRef]
- Merheb, J.; Graham, J.; Coucke, W.; Roberts, M.; Quirynen, M.; Jacobs, R.; Devlin, H. Prediction of Implant Loss and Marginal Bone Loss by Analysis of Dental Panoramic Radiographs. Int. J. Oral Maxillofac. Implant. 2015, 30, 372–377. [Google Scholar] [CrossRef]
- Barewal, R.M.; Stanford, C.; Weesner, T.C. A randomized controlled clinical trial comparing the effects of three loading protocols on dental implant stability. Int. J. Oral Maxillofac. Implant. 2012, 27, 945–956. [Google Scholar]
- Tawil, G.; Mawla, M.; Gottlow, J. Clinical and radiographic evaluation of the 5-mm diameter regular-platform Brånemark fixture: 2- to 5-year follow-up. Clin. Implant. Dent. Relat. Res. 2002, 4, 16–26. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bone Quality and Quantity and Dental Implant Failure: A Systematic Review and Meta-analysis. Int. J. Prosthodont. 2017, 30, 219–237. [Google Scholar] [CrossRef]
- Misch, C.E. Contemporary Implant Dentistry. Implant. Dent. 1999, 8, 90. [Google Scholar] [CrossRef]
- Tawse-Smith, A.; Payne, A.G.; Kumara, R.; Thomson, W.M. Early Loading of Unsplinted Implants Supporting Mandibular Overdentures Using a One-Stage Operative Procedure with Two Different Implant Systems: A 2-Year Report. Clin. Implant. Dent. Relat. Res. 2002, 4, 33–42. [Google Scholar] [CrossRef]
| Implant Size | All Patients (n = 20 Patients with 40 Implants) | Immediate Loading Group (n = 10 Patients with 20 Implants) | Conventional Loading Group (n = 10 Patients with 20 Implants) | |||
|---|---|---|---|---|---|---|
| Diameter | N | % | N | % | N | % |
| 3.3 mm | 7 | 17.5 | 3 | 15.0 | 4 | 20.0 |
| 3.75 mm | 23 | 57.5 | 13 | 65.0 | 10 | 50.0 |
| 4.2 mm | 10 | 25.0 | 4 | 20.0 | 6 | 30.0 |
| Length | N | % | N | % | N | % |
| 10 mm | 14 | 35.0 | 5 | 25.0 | 9 | 45.0 |
| 11.5 mm | 22 | 55.0 | 13 | 65.0 | 9 | 45.0 |
| 13 mm | 4 | 10.0 | 2 | 10.0 | 2 | 10.0 |
| Baseline | All Patients (n = 20 Patients with 40 Implants) | Immediate Loading Group (n = 10 Patients with 20 Implants) | Conventional Loading Group (n = 10 Patients with 20 Implants) | |||
|---|---|---|---|---|---|---|
| Implant insertion torque at different sites | Mean | SD | Mean | SD | Mean | SD |
| #33 | 62.9 | 14.4 | 64.5 | 13.8 | 61.2 | 15.5 |
| #43 | 64.0 | 13.0 | 65.9 | 11.9 | 62.0 | 14.4 |
| Average | 63.5 | 13.1 | 65.2 | 12.1 | 61.7 | 14.4 |
| Implant stability by ISQ | Mean | SD | Mean | SD | Mean | SD |
| #33 | 69.1 a | 7.3 | 69.2 a | 6.7 | 69.0 a | 8.1 |
| #43 | 71.7 a | 8.6 | 72.3 a | 10.3 | 71.0 a | 6.9 |
| Average | 70.4 a | 5.9 | 70.8 a | 6.8 | 70.0 a | 5.3 |
| Averaged Crestal position (aggregating mesial and distal sides of both implants) | N | % | N | % | N | % |
| Subcrestal | 6 a | 30.0 | 2 a | 20.0 | 4 a | 40.0 |
| Crestal | 7 a | 35.0 | 4 a | 40.0 a | 3 a | 30.0 |
| Supracrestal | 7 a | 35.0 | 4 a | 40.0 | 3 a | 30.0 |
| At 2 months of follow-up | ||||||
| Implant stability by ISQ | Mean | SD | Mean | SD | Mean | SD |
| #33 | 67.0 a | 10.3 | 66.9 a | 12.5 | 67.1 a | 8.3 |
| #43 | 72.8 a | 4.8 | 72.7 a | 6.2 | 72.9 a | 3.3 |
| Average | 69.9 a | 5.8 | 69.8 a | 7.2 | 70.0 a | 4.3 |
| Percentage of healthy gingival sites | 57.5 a | 46.7 | 65.0 a | 47.4 | 50.0 a | 47.1 |
| At 6 months of follow-up | ||||||
| Implant stability by ISQ | Mean | SD | Mean | SD | Mean | SD |
| #33 | 71.9 a | 4.3 | 73.0 a | 5.2 | 70.9 a | 3.0 |
| #43 | 72.9 a | 4.5 | 72.8 a | 5.8 | 72.9 a | 3.1 |
| Average | 72.8 b | 4.1 | 73.3 a | 5.2 | 72.3 b | 2.8 |
| Percentage of healthy gingival sites | 55.0 a | 45.6 | 60.0 a | 46.0 | 50.0 a | 47.1 |
| At 12 months of follow-up | ||||||
| Implant stability by ISQ | Mean | SD | Mean | SD | Mean | SD |
| #33 | 72.9 b | 6.0 | 71.4 a | 7.4 | 74.6 b | 3.9 |
| #43 | 73.7 b | 5.0 | 73.5 a | 5.2 | 73.8 a | 5.0 |
| Average | 73.5 b | 4.8 | 72.8 a | 5.7 | 74.2 b | 3.9 |
| Percentage of healthy gingival sites | 87.5 b | 22.2 | 100.0 b | 0.0 | 75.0 a | 26.4 |
| Averaged Crestal position (aggregating mesial and distal sides of both implants) | N | % | N | % | N | % |
| Subcrestal | 3 b | 15.0 | 2 a | 20.0 | 1 b | 10.0 |
| Crestal | 4 b | 20.0 | 2 a | 20.0 | 2 b | 20.0 |
| Supracrestal | 13 b | 65.0 | 6 a | 60.0 | 7 b | 70.0 |
| All Patients (n = 20 Patients with 40 Implants) | Immediate Loading Group (n = 10 Patients with 20 Implants) | Conventional Loading Group (n = 10 Patients with 20 Implants) | ||||
|---|---|---|---|---|---|---|
| Baseline Implant shoulder position (mm) | Mean | SD | Mean | SD | Mean | SD |
| #33 | −0.08 | 0.63 | 0.00 | 0.61 | −0.17 | 0.67 |
| #43 | −0.06 | 0.46 | −0.05 | 0.28 | −0.08 | 0.60 |
| All implants | −0.08 | 0.51 | −0.03 | 0.40 | −0.13 | 0.62 |
| Final Implant shoulder position (mm) | Mean | SD | Mean | SD | Mean | SD |
| #33 | 0.45 | 0.85 | 0.47 | 0.87 | 0.44 | 0.88 |
| #43 | 0.21 | 0.59 | 0.29 | 0.42 | 0.14 | 0.74 |
| All implants | 0.34 | 0.68 | 0.38 | 0.60 | 0.30 | 0.68 |
| Marginal Bone Loss (mm) | Mean | SD | Mean | SD | Mean | SD |
| #33 | 0.54 | 0.50 | 0.47 | 0.53 | 0.61 | 0.50 |
| #43 | 0.28 | 0.30 | 0.34 | 0.33 | 0.22 | 0.26 |
| All implants | 0.4 | 0.37 | 0.40 | 0.39 | 0.44 | 0.36 |
| CI 95% | CI 95% | CI 95% | ||||
| lower limit | upper limit | lower limit | upper limit | lower limit | upper limit | |
| Averaged Marginal Bone loss (mm) | 0.25 | 0.59 | 0.12 | 0.68 | 0.19 | 0.69 |
| Mean | SD | Mean | SD | Mean | SD | |
| Months of follow-up | 13.4 | 2.1 | 13.2 | 2.1 | 13.5 | 2.1 |
| Short-Term Complications | All Patients (n = 20) | Immediate Loading Group (n = 10) | Conventional Loading Group (n = 10) | |||
|---|---|---|---|---|---|---|
| Prevalence | N | % | N | % | N | % |
| Biological A | 10 | 50.0 | 4 | 40.0 | 6 | 60.0 |
| Mechanical B | 5 | 25.0 | 3 | 30.0 | 2 | 2.0 |
| None | 5 | 25.0 | 3 | 30.0 | 2 | 2.0 |
| Number of complications | Mean | SD | Mean | SD | Mean | SD |
| Average complications | 1.0 | 0.9 | 1.1 | 1.1 | 0.8 | 0.6 |
| Biological complications | 0.8 | 0.8 | 0.8 | 1.0 | 0.8 | 0.6 |
| Mechanical complications | 0.4 | 0.5 | 0.5 | 0.5 | 0.3 | 0.5 |
| Prevalence of complications | ||||||
| Type of complications | N | % | N | % | N | % |
| Uneventful treatment | 7 | 35.0 | 4 | 40.0 | 3 | 30.0 |
| Prosthetic complications | 13 | 65.0 | 6 | 60.0 | 7 | 70.0 |
| Minor C | 8 | 40.0 | 5 | 50.0 | 3 | 30.0 |
| Major D | 6 | 30.0 | 4 | 40.0 | 2 | 20.0 |
| Biological complications | 12 | 60.0 | 5 | 50.0 | 7 | 70.0 |
| Implant Failure | 4 | 20.0 | 2 | 20.0 | 2 | 20.0 |
| Mean | SD | Mean | SD | Mean | SD | |
| Failure Ratio(%) E | 11.2 | 25.9 | 8.3 | 18.0 | 14.0 | 32.7 |
| Event Rate Per 100 Yrs F | Mean | CI-95% | Mean | CI-95% | Mean | CI-95% |
| Total | 5.4 | 3.4–7.3 | 5.6 | 2.3–9.0 | 5.1 | 2.4–7.9 |
| Prosthetic | 1.9 | 0.8–3.0 | 2.2 | 0.5–4.0 | 1.5 | −0.2–3.2 |
| Biological | 3.5 | 1.9–5.2 | 3.4 | 0.5–6.3 | 3.6 | 1.4–5.9 |
| Implant failure | 1.1 | −0.1–2.3 | 0.8 | −0.5–2.1 | 1.4 | −0.9–3.7 |
| Dependent Predictors | β | Error | T | p-Value | Lower CI 95% | Upper CI 95% |
|---|---|---|---|---|---|---|
| Implant Failure a | ||||||
| Bone Quality | 13.61 | 12.7 | 2.4 | 0.03 | 1.3 | 25.8 |
| Prosthetic Complications b | ||||||
| Averaged insertion torque | 0.13 | 0.05 | 2.4 | 0.03 | 0.01 | 0.24 |
| Biological Complications c | ||||||
| Minor prosthetic complications | 1.11 | 0.4 | 2.4 | 0.04 | 0.1 | 2.0 |
| Marginal Bone Loss d | ||||||
| Bone Quality | −0.59 | 0.21 | −2.8 | 0.01 | −0.15 | −1.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pardal-Peláez, B.; Dib, A.; Guadilla, Y.; Flores-Fraile, J.; Quispe-López, N.; Montero, J. Marginal Bone Loss and Treatment Complications with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants—A Randomized Clinical Trial. Prosthesis 2023, 5, 295-309. https://doi.org/10.3390/prosthesis5010022
Pardal-Peláez B, Dib A, Guadilla Y, Flores-Fraile J, Quispe-López N, Montero J. Marginal Bone Loss and Treatment Complications with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants—A Randomized Clinical Trial. Prosthesis. 2023; 5(1):295-309. https://doi.org/10.3390/prosthesis5010022
Chicago/Turabian StylePardal-Peláez, Beatriz, Abraham Dib, Yasmina Guadilla, Javier Flores-Fraile, Norberto Quispe-López, and Javier Montero. 2023. "Marginal Bone Loss and Treatment Complications with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants—A Randomized Clinical Trial" Prosthesis 5, no. 1: 295-309. https://doi.org/10.3390/prosthesis5010022
APA StylePardal-Peláez, B., Dib, A., Guadilla, Y., Flores-Fraile, J., Quispe-López, N., & Montero, J. (2023). Marginal Bone Loss and Treatment Complications with Mandibular Overdentures Retained by Two Immediate or Conventionally Loaded Implants—A Randomized Clinical Trial. Prosthesis, 5(1), 295-309. https://doi.org/10.3390/prosthesis5010022










