Evolving 3D-Printing Strategies for Structural and Cosmetic Components in Upper Limb Prosthesis
Abstract
:1. Introduction
1.1. Prosthesis Classifications
1.2. Reported Limitations
1.3. Manufacturing Techniques
1.4. Aesthetic Design Considerations
2. Background
2.1. Device Development
2.2. Clinical Investigation
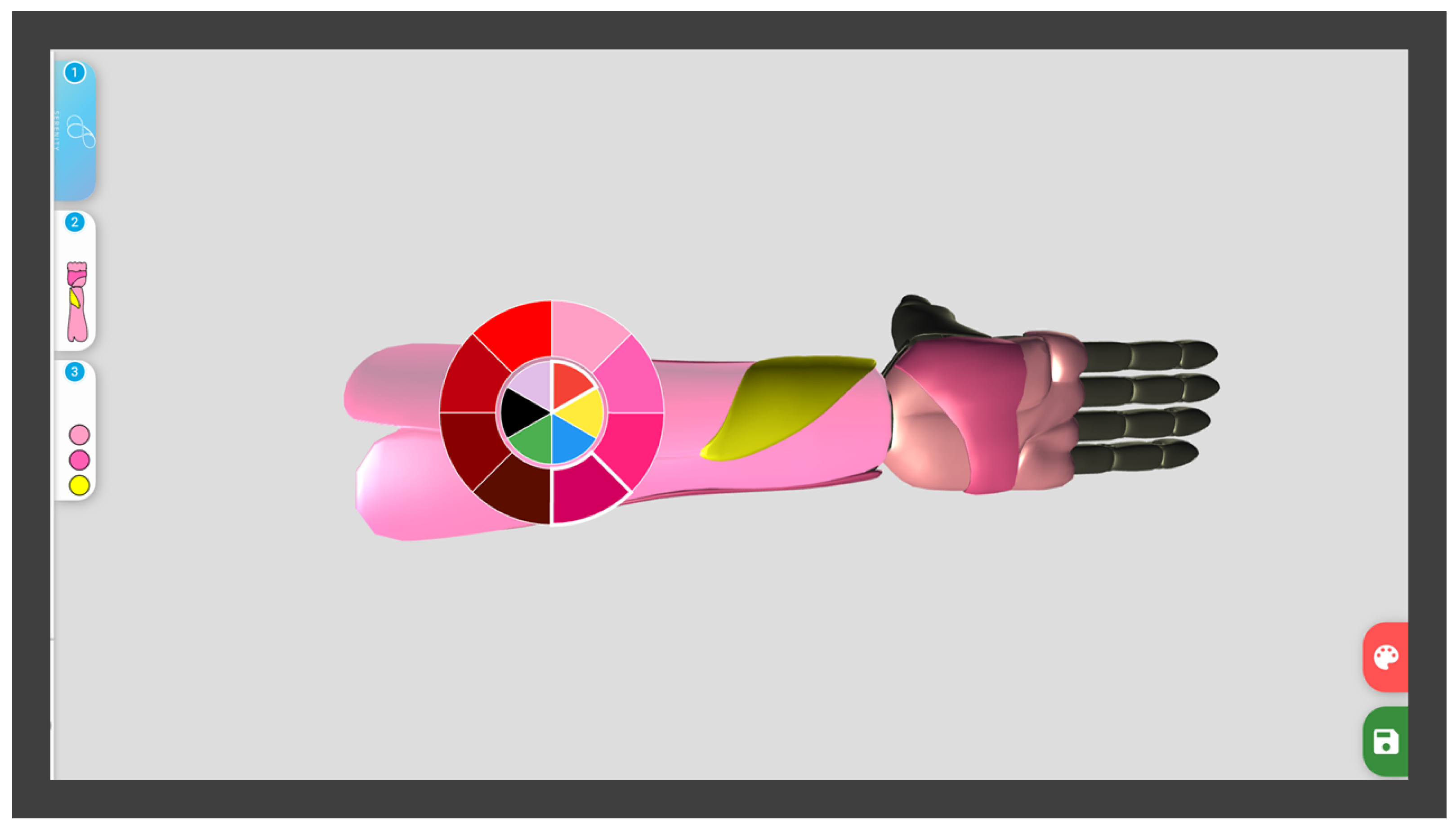
2.3. Aesthetic Design
3. Methods for Implementing Additive Manufacturing
3.1. Direct Part Manufacturing
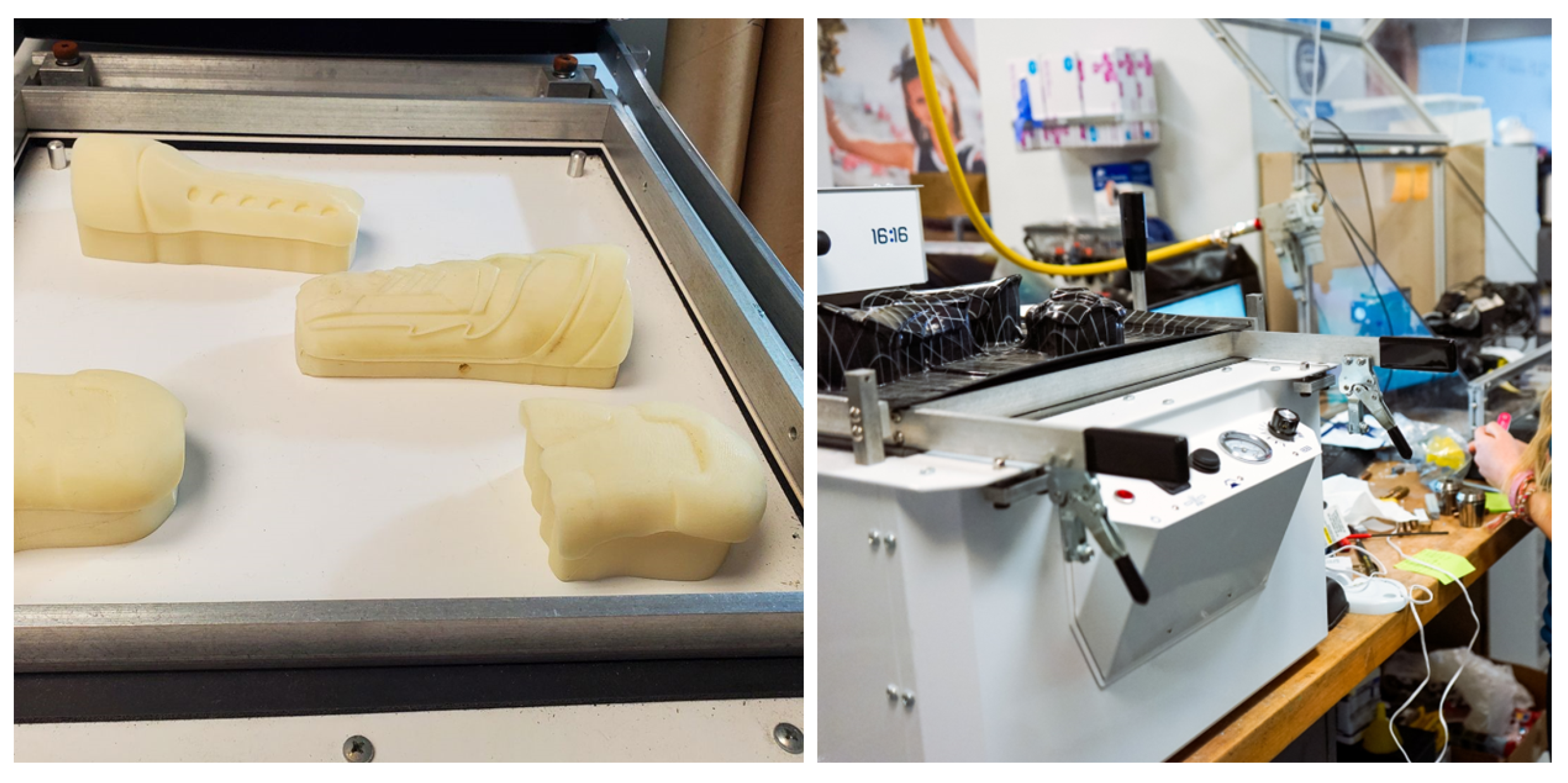
3.2. Thermoforming via Additive Manufacturing Positive Die
3.3. Overmolding via Additive Manufacturing Moulds
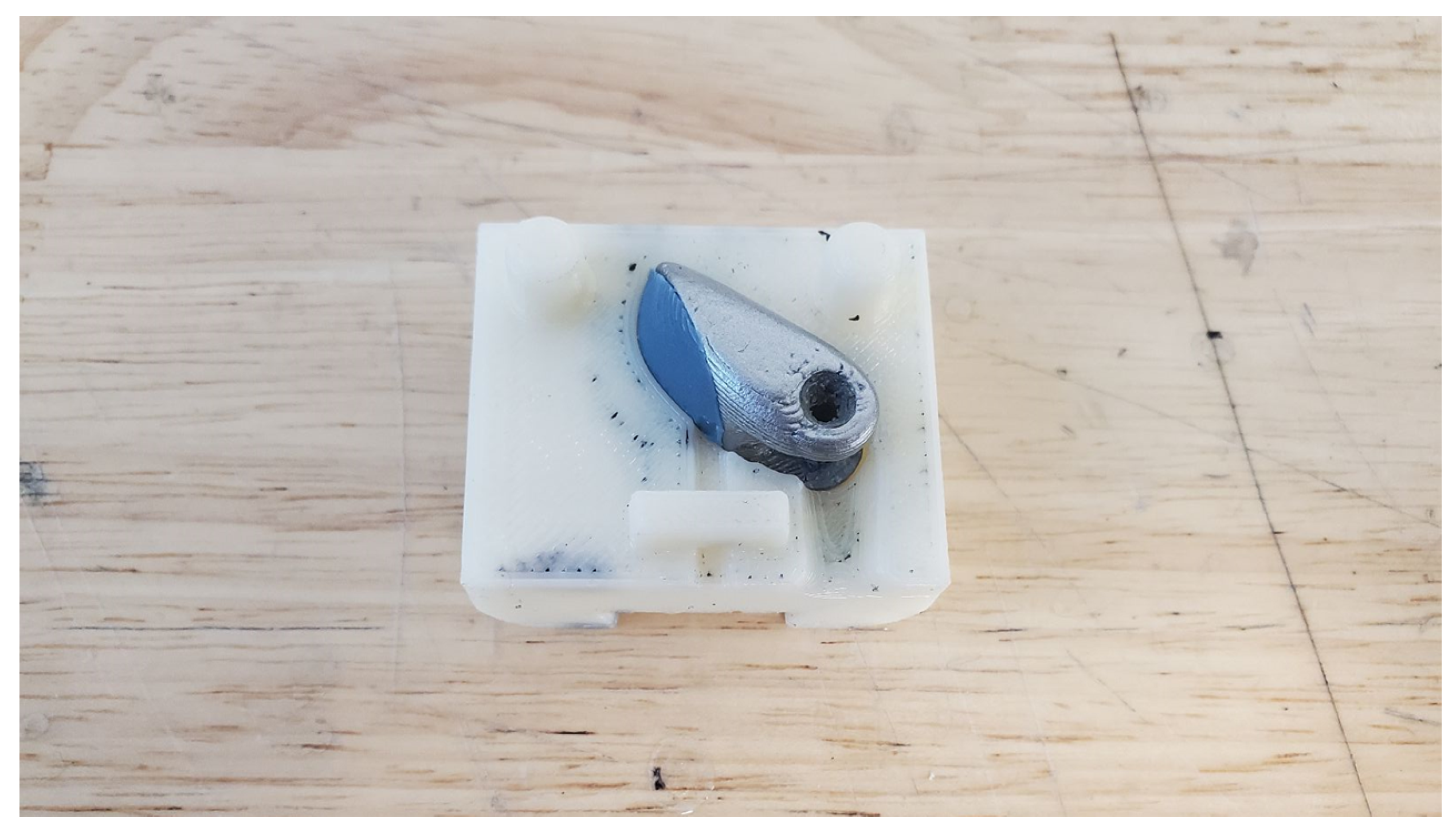
3.4. Injection Molding Prototyping via Additive Manufacturing
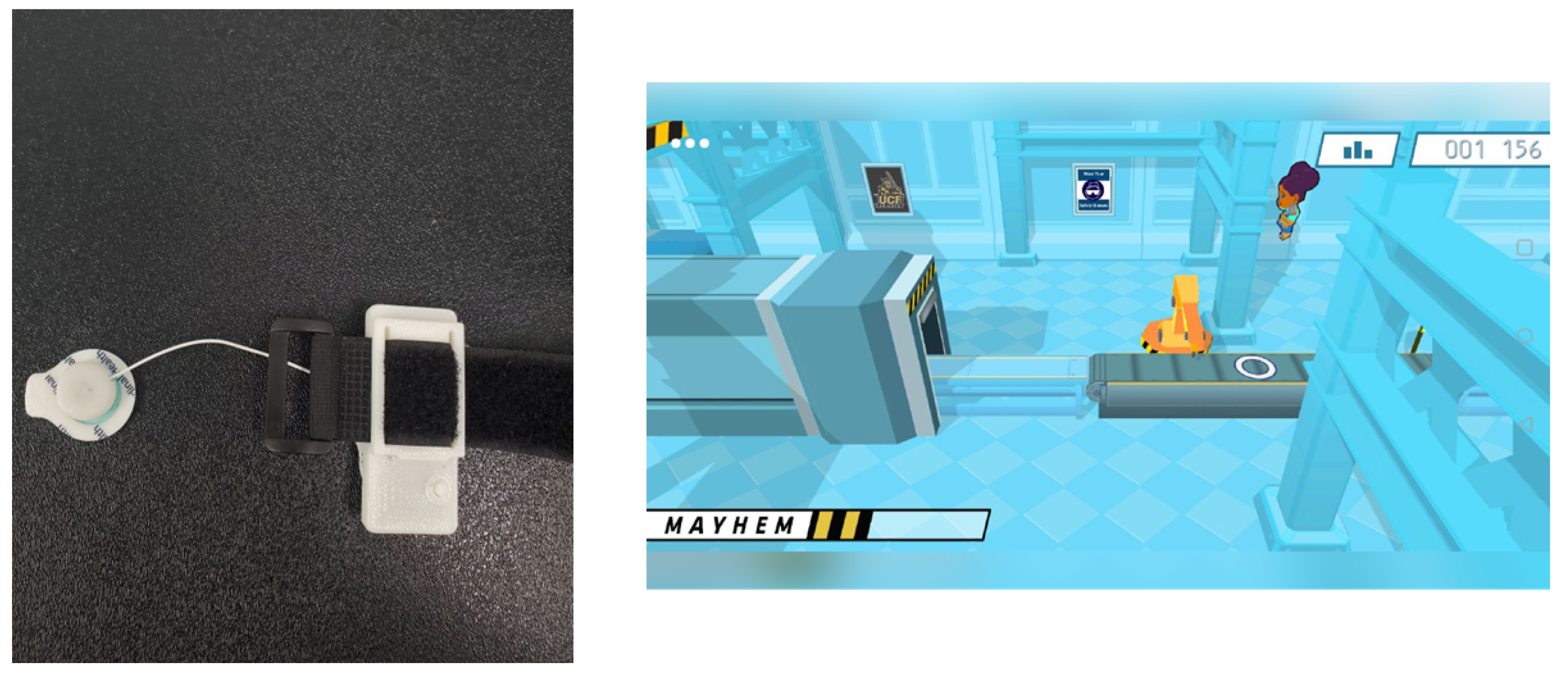
3.5. Accessories and Additional Components
4. Results
4.1. Direct Part Manufacturing Outcomes for Implementing Aesthetic Design
4.2. Thermoforming Outcomes for Reduced Manufacturing Time, and Increased Durability
4.3. Overmolding Outcomes for Improved Grip
4.4. Manufacturing Accessories
4.5. Overall Weight Reduction from All Methods
5. Conclusions and Recommendations
- Prostheses are a regulated device in many countries, and clinical research often requires medical institution involvement. Patient feedback is critical to continuing the improvement of the device. Novel manufacturing methods may result in different regulatory considerations, and researchers should work closely with their institution’s compliance teams.
- The customization opportunities when using an additive manufacturing approach enable extensive aesthetic expression. Incorporating the device’s user in the aesthetic choices, referred to as a variation of participatory visual design labeled ’cooperative expression’ [19], may provide increased affinity to the device.
- Additive manufacturing is an effective tool for prototyping, and in certain use cases, but components must be mechanically designed to use traditional fasteners and to integrate into multi-part assemblies. These fasteners may include binding posts, screws, anchors, and hinges. The integration points between additive parts and traditionally manufactured components may lead to stress concentrations, and optimization for printing orientation, parameters, and applied loading conditions must be taken into account with additional caution.
- Parts manufactured by additive manufacturing may be susceptible to cyclical loading failure or part degradation over time [48], making points of integration, for example, for mechanical joints, of high priority for additional robustness.
- Additive manufacturing for the creation of positive molding, to be used with thermoforming, can allow for increased manufacturing production rates and increased part robustness. FDM-produced positive molds for thermoforming applications may be limited to 50 production pulls before cosmetic detail could be lost. The improvement in surface finish and flexibility provides excellent properties for final cosmetic parts that require aesthetic treatments.
- Cosmetic components for prosthesis are a segment of prosthesis limb manufacturing that is primed for involvement from additive manufacturing. The resulting devices may hold promise to reduce overall cost and device weight, while also being capable of producing complex visual features that would not be cost effectively manufacturable in low production volumes through other methods.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AM | Additive Manufacturing |
| ABS | Acrylonitrile Butadiene Styrene |
| CAD | Computer-aided Design |
| EMG | Electromyography |
| LSR | Liquid Silicone Rubber |
| PLA | Polylactic Acid |
References
- Biddiss, E.A.; Chau, T.T. Upper limb prosthesis use and abandonment: A survey of the last 25 years. Prosthetics Orthot. Int. 2007, 31, 236–257. [Google Scholar] [CrossRef]
- Salminger, S.; Stino, H.; Pichler, L.H.; Gstoettner, C.; Sturma, A.; Mayer, J.A.; Szivak, M.; Aszmann, O.C. Current rates of prosthetic usage in upper-limb amputees—Have innovations had an impact on device acceptance? Disabil. Rehabil. 2020, 44, 3708–3713. [Google Scholar] [CrossRef]
- Østlie, K.; Lesjø, I.M.; Franklin, R.J.; Garfelt, B.; Skjeldal, O.H.; Magnus, P. Prosthesis rejection in acquired major upper-limb amputees: A population-based survey. Disabil. Rehabil. Assist. Technol. 2012, 7, 294–303. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, M.A. Innovation and improvement of body-powered arm prostheses: A first step. Clin. Prosthetics Orthot. 1985, 9, 13–16. [Google Scholar]
- Gallagher, P.; Maclachlan, M. Adjustment to an Artificial Limb: A Qualitative Perspective. J. Health Psychol. 2001, 6, 85–100. [Google Scholar] [CrossRef]
- Murray, C.D. The Social Meanings of Prosthesis Use. J. Health Psychol. 2005, 10, 425–441. [Google Scholar] [CrossRef]
- Blom, J. The aesthetics of prosthetic greaves: Co-design for expressing personal identity. Making Futures 2018, 5, 18. [Google Scholar]
- Sansoni, S.; Wodehouse, A.J.; Buis, A. The aesthetics of prosthetic design: From theory to practice. In DS 77: Proceedings of the DESIGN 2014 13th International Design Conference, Cavtat, Coratia, 19–22 May 2014; pp. 975–984. [Google Scholar]
- Hall, M.L.; Orzada, B.T. Expressive prostheses: Meaning and significance. Fash. Pract. 2013, 5, 9–32. [Google Scholar] [CrossRef]
- Nagaraja, V.H.; da Ponte Lopes, J.; Bergmann, J.H.M. Reimagining prosthetic control: A novel body-powered prosthetic system for simultaneous control and actuation. Prosthesis 2022, 4, 394–413. [Google Scholar] [CrossRef]
- Carey, S.; Lura, D.; Highsmith, M. Differences in myoelectric and body-powered upper-limb prostheses: Systematic literature review. J. Rehabil. Res. Dev. 2015, 52, 247–262. [Google Scholar] [CrossRef]
- Wagner, L.V.; Bagley, A.M.; James, M.A. Reasons for prosthetic rejection by children with unilateral congenital transverse forearm total deficiency. JPO J. Prosthetics Orthot. 2007, 19, 51–54. [Google Scholar] [CrossRef]
- Uellendahl, J. Myoelectric versus body-powered upper-limb prostheses: A clinical perspective. JPO J. Prosthetics Orthot. 2017, 29, P25. [Google Scholar] [CrossRef]
- Biddiss, E.; Chau, T. Upper-limb prosthetics: Critical factors in device abandonment. Am. J. Phys. Med. Rehabil. 2007, 86, 977–987. [Google Scholar] [CrossRef]
- Childress, D.S. Powered Limb Prostheses: Their clinical significance. IEEE Trans. Biomed. Eng. 1973, BME-20, 200–207. [Google Scholar] [CrossRef]
- Childress, D.S. Historical aspects of powered limb prostheses. Clin. Prosthetics Orthot. 1985, 9, 2–13. [Google Scholar]
- Geethanjali, P. Myoelectric control of Prosthetic Hands: State-of-the-art review. Med Devices Evid. Res. 2016, 9, 247–255. [Google Scholar] [CrossRef]
- Manero, A.; Sparkman, J.; Dombrowski, M.; Buyssens, R.; Smith, P. Developing and training multi-gestural prosthetic arms. In Proceedings of the Virtual, Augmented And Mixed Reality: Interaction, Navigation, Visualization, Embodiment, and Simulation: 10th International Conference, VAMR 2018, Held as Part of HCI International 2018, Las Vegas, NV, USA, 15–20 July 2018; 2018; pp. 427–437. [Google Scholar] [CrossRef]
- Manero, A.; Smith, P.; Sparkman, J.; Dombrowski, M.; Courbin, D.; Kester, A.; Womack, I.; Chi, A. Implementation of 3D Printing Technology in the Field of Prosthetics: Past, Present, and Future. Int. J. Environ. Res. Public Health 2019, 16, 1641. [Google Scholar] [CrossRef]
- Parker, P.; Englehart, K.; Hudgins, B. Myoelectric signal processing for control of powered limb prostheses. J. Electromyogr. Kinesiol. 2006, 16, 541–548. [Google Scholar] [CrossRef]
- Scotland, T.; Galway, H. A long-term review of children with congenital and acquired upper limb deficiency. J. Bone Jt. Surgery Br. Vol. 1983, 65, 346–349. [Google Scholar] [CrossRef]
- Murray, C.D. Being like everybody else: The personal meanings of being a prosthesis user. Disabil. Rehabil. 2009, 31, 573–581. [Google Scholar] [CrossRef]
- Mori, M. Bukimi no tani [the uncanny valley]. Energy 1970, 7, 33–35. [Google Scholar]
- Bartneck, C.; Kanda, T.; Ishiguro, H.; Hagita, N. Is the uncanny valley an uncanny cliff? In Proceedings of the RO-MAN 2007—The 16th IEEE International Symposium on Robot and Human Interactive Communication, Jeju, Republic of Korea, 26–29 August 2007; pp. 368–373. [Google Scholar]
- Sansoni, S.; Wodehouse, A.; McFadyen, A.K.; Buis, A. The aesthetic appeal of prosthetic limbs and the uncanny valley: The role of personal characteristics in attraction. Int. J. Des. 2015, 9, 67–81. [Google Scholar]
- Złotowski, J.A.; Sumioka, H.; Nishio, S.; Glas, D.F.; Bartneck, C.; Ishiguro, H. Persistence of the uncanny valley: The influence of repeated interactions and a robot’s attitude on its perception. Front. Psychol. 2015, 6, 883. [Google Scholar] [CrossRef]
- Smail, L.C.; Neal, C.; Wilkins, C.; Packham, T.L. Comfort and function remain key factors in upper limb prosthetic abandonment: Findings of a scoping review. Disabil. Rehabil. Assist. Technol. 2021, 16, 821–830. [Google Scholar] [CrossRef]
- Burton, L.; Melkumova-Reynolds, J. “My Leg is a Giant Stiletto Heel”: Fashioning the ProsthetisedBody. Fash. Theory 2019, 23, 195–218. [Google Scholar] [CrossRef]
- Maria Moreira Soares, J.; Pedro Farinha Nunes da Costa, J.; Ângelo, P.; Mendes, M. Expanded Boundaries: Art and Non-human Essence as Playful Inspirations for Children’s Prosthetics. In Proceedings of the Fifteenth International Conference on Tangible, Embedded, and Embodied Interaction, Salzburg, Austria, 14–17 February 2021; pp. 1–8. [Google Scholar]
- Zhou, W.; Lin, J.; Balint, D.S.; Dean, T.A. Clarification of the effect of temperature and strain rate on workpiece deformation behaviour in metal forming processes. Int. J. Mach. Tools Manuf. 2021, 171, 103815. [Google Scholar] [CrossRef]
- Wang, B. The future of manufacturing: A new perspective. Engineering 2018, 4, 722–728. [Google Scholar] [CrossRef]
- Hällgren, S.; Pejryd, L.; Ekengren, J. (Re) Design for additive manufacturing. Procedia Cirp 2016, 50, 246–251. [Google Scholar] [CrossRef]
- Gebler, M.; Schoot Uiterkamp, A.J.M.; Visser, C. A global sustainability perspective on 3D printing technologies. Energy Policy 2014, 74, 158–167. [Google Scholar] [CrossRef]
- Seol, K.S.; Zhao, P.; Shin, B.C.; Zhang, S.U. Infill print parameters for mechanical properties of 3D printed PLA parts. J. Korean Soc. Manuf. Process Eng. 2018, 17, 9–16. [Google Scholar] [CrossRef]
- Joska, Z.; Andrés, L.; Dražan, T.; Maňas, K.; Pokornỳ, Z.; Sedlák, J. Influence of the shape of the filling on the mechanical properties of samples made by 3D printing. Manuf. Technol. 2021, 21, 199–205. [Google Scholar] [CrossRef]
- Herbert, N.; Simpson, D.; Spence, W.D.; Ion, W. A preliminary investigation into the development of 3-D printing of prosthetic sockets. J. Rehabil. Res. Dev. 2005, 42, 141. [Google Scholar] [CrossRef]
- Ventola, C.L. Medical Applications for 3D Printing: Current and Projected Uses. P T A Peer-Rev. J. Formul. Manag. 2014, 39, 704–711. [Google Scholar]
- Wang, Y.; Tan, Q.; Pu, F.; Boone, D.; Zhang, M. A review of the application of additive manufacturing in prosthetic and orthotic clinics from a biomechanical perspective. Engineering 2020, 6, 1258–1266. [Google Scholar] [CrossRef]
- Korpela, M.; Riikonen, N.; Piili, H.; Salminen, A.; Nyrhilä, O. Additive manufacturing—Past, present, and the future. In Technical, Economic and Societal Effects of Manufacturing 4.0: Automation, Adaption and Manufacturing in Finland and Beyond; Palgrave Macmillan: Lappeenranta, Finland, 2020; pp. 17–41. [Google Scholar]
- Livingstone, R.W.; Bone, J.; Field, D.A. Beginning power mobility: An exploration of factors associated with child use of early power mobility devices and parent device preference. J. Rehabil. Assist. Technol. Eng. 2020, 7, 205566832092604. [Google Scholar] [CrossRef]
- Day, S. Using rapid prototyping in prosthetics: Design considerations. In Rapid Prototyping of Biomaterials; Woodhead Publishing: Sawston, UK, 2020; pp. 325–338. [Google Scholar] [CrossRef]
- Chimento, J.; Jason Highsmith, M.; Crane, N. 3D printed tooling for thermoforming of Medical Devices. Rapid Prototyp. J. 2011, 17, 387–392. [Google Scholar] [CrossRef]
- Junk, S.; Sämann-Sun, J.; Niederhofer, M. Application of 3D printing for the rapid tooling of thermoforming moulds. In Proceedings of the 36th International MATADOR Conference, Manchester, UK, 14–16 July 2010; pp. 369–372. [Google Scholar]
- Gajdoš, I.; Maňková, I.; Jachowicz, T.; Tor-Swiatek, A. Application of rapid tooling approach in process of thermoforming mold production. In Proceedings of the 8th International Engineering Symposium At Bánki, Budapest, Hungary, 7–10 November 2016. [Google Scholar]
- Wattanasiri, P.; Tangpornprasert, P.; Virulsri, C. Design of multi-grip patterns prosthetic hand with single actuator. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1188–1198. [Google Scholar] [CrossRef]
- Boros, R.; Rajamani, P.K.; Kovács, J. Combination of 3D printing and injection molding: Overmolding and overprinting. Express Polym. Lett. 2019, 13, 889–897. [Google Scholar] [CrossRef]
- Smith, P.A.; Dombrowski, M.; Buyssens, R.; Barclay, P. The impact of a custom electromyograph (EMG) controller on player enjoyment of games designed to teach the use of Prosthetic Arms. Comput. Games J. 2018, 7, 131–147. [Google Scholar] [CrossRef]
- Priya, M.S.; Naresh, K.; Jayaganthan, R.; Velmurugan, R. A comparative study between in-house 3D printed and injection molded ABS and PLA polymers for low-frequency applications. Mater. Res. Express 2019, 6, 085345. [Google Scholar] [CrossRef]


| Assembly | Composition & Manufacturing Method | Weight (g) | Reduction |
|---|---|---|---|
| Cosmesis | FDM 3D printed ABS shell, magnets, with paint | 119 | |
| Thermoformed ABS shell, magnets, with paint | 80 | 33% | |
| Battery Core | FDM 3D printed ABS, battery and circuitry, with paint | 177 | |
| Injection moulded ABS, battery and circuitry, with paint | 169 | 5% | |
| Hand | FDM 3D printed ABS, DC motors, metalic gears and supports, circuitry, with paint | 200 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manero, A.; Sparkman, J.; Dombrowski, M.; Smith, P.; Senthil, P.; Smith, S.; Rivera, V.; Chi, A. Evolving 3D-Printing Strategies for Structural and Cosmetic Components in Upper Limb Prosthesis. Prosthesis 2023, 5, 167-181. https://doi.org/10.3390/prosthesis5010013
Manero A, Sparkman J, Dombrowski M, Smith P, Senthil P, Smith S, Rivera V, Chi A. Evolving 3D-Printing Strategies for Structural and Cosmetic Components in Upper Limb Prosthesis. Prosthesis. 2023; 5(1):167-181. https://doi.org/10.3390/prosthesis5010013
Chicago/Turabian StyleManero, Albert, John Sparkman, Matt Dombrowski, Peter Smith, Pavan Senthil, Spencer Smith, Viviana Rivera, and Albert Chi. 2023. "Evolving 3D-Printing Strategies for Structural and Cosmetic Components in Upper Limb Prosthesis" Prosthesis 5, no. 1: 167-181. https://doi.org/10.3390/prosthesis5010013
APA StyleManero, A., Sparkman, J., Dombrowski, M., Smith, P., Senthil, P., Smith, S., Rivera, V., & Chi, A. (2023). Evolving 3D-Printing Strategies for Structural and Cosmetic Components in Upper Limb Prosthesis. Prosthesis, 5(1), 167-181. https://doi.org/10.3390/prosthesis5010013





